Published online Jul 15, 2024. doi: 10.4239/wjd.v15.i7.1404
Revised: April 30, 2024
Accepted: May 17, 2024
Published online: July 15, 2024
Processing time: 130 Days and 17.4 Hours
Adiposity, synonymous with obesity, is prevalent among both children and adults with type 1 diabetes in China. Recent literature underscored the patho-physiological and socioeconomic factors associated with adiposity, and consistently highlighted its impact on cardiovascular, kidney, and metabolic diseases among Chinese individuals with type 1 diabetes. Addressing and managing adiposity in individuals with type 1 diabetes are complicated and entail comprehensive approaches including lifestyle modifications, cognitive-behavioral therapy, insulin dose titration, and other diabetes treatment medications. The condition calls for coordination among policymakers, researchers, clinicians, and patients.
Core Tip: Adiposity emerges as a significant health concern for individuals with type 1 diabetes in China as well as globally. Adiposity is associated with adverse health outcomes, including cardiovascular and kidney complications in people with type 1 diabetes. This article highlighted the approaches in addressing and managing adiposity in individuals with type 1 diabetes. The condition calls for coordination among policymakers, researchers, clinicians, and patients.
- Citation: Wu NW, Lyu XF, An ZM, Li SY. Adiposity in Chinese people with type 1 diabetes. World J Diabetes 2024; 15(7): 1404-1408
- URL: https://www.wjgnet.com/1948-9358/full/v15/i7/1404.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i7.1404
Obesity (adiposity) pandemic goes wildly in China as well as globally[1]. Adolescents and adults with overweight and obesity are facing elevated risks of metabolic diseases, cardiovascular diseases, kidney diseases, chronic pain, disability, and neoplasm[2]. Compared to type 2 diabetes, type 1 diabetes is less prevalent in China but more common among young people. Almost a quarter of individuals with type 1 diabetes were first diagnosed before the age of 14[3]. Adiposity does not directly involve in the pathogenesis or development of type 1 diabetes, which is characterized by beta-cell failure due to autoimmunity, viral infection, and other non-metabolic factors. Nevertheless, adiposity-associated impairment of the antioxidant defense system[4] and elevated proinflammatory cytokines may be associated with worsened immune response[5,6]. At individual level, adiposity means adverse health prognosis, including cardiovascular and kidney complications in people with type 1 diabetes[7-9].
In people with type 1 diabetes and poor glucose control, particularly those experiencing frequent episodes of ketoacidosis, fat mass, including visceral and subcutaneous fat, scarcely accumulates. Adiposity is less prevalent among individuals with type 1 diabetes receiving inadequate healthcare. In nations with advanced healthcare policies, individuals with type 1 diabetes, particularly at younger ages, anticipate minimal years of life lost or a lifespan comparable to those without type 1 diabetes[10]. However, in such circumstances, adiposity could pose a challenge. A recent study by Zeng et al[11] from China examined 101 individuals with type 1 diabetes spanning a wide range of ages. Among their participants, 19.8% exhibited overweight and obesity, while 15.8% were diagnosed with metabolic syndrome. Following the trend of Europe and North America, the adiposity emerges as a significant health concern for individuals with type 1 diabetes in China and other developing countries[12].
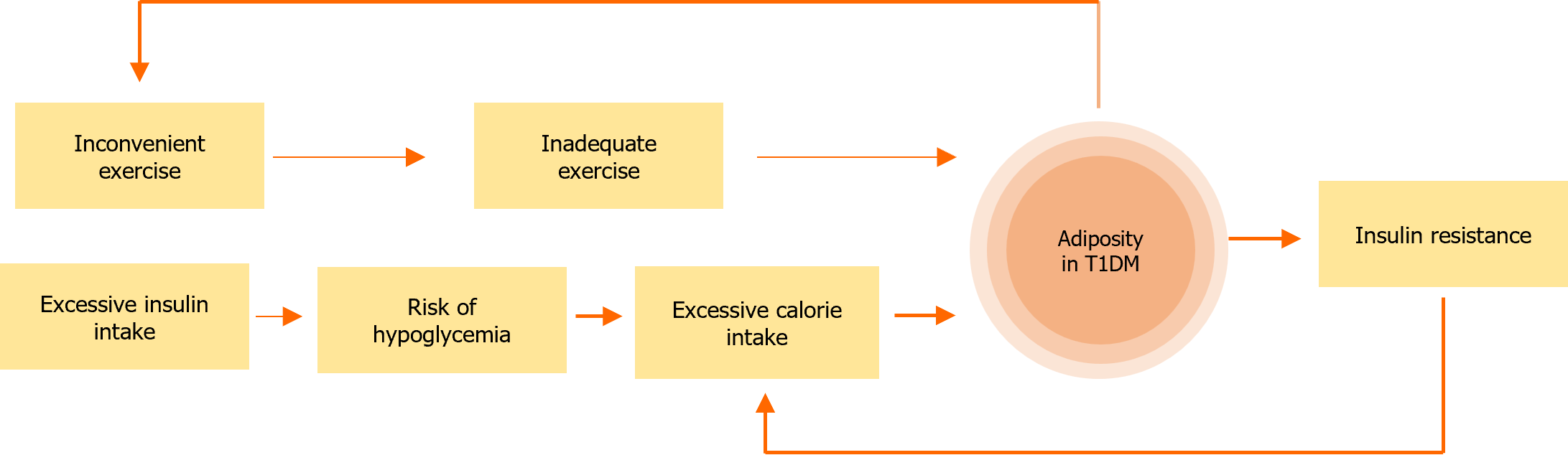
Multiple factors contribute to the excess body fat mass and elevated risks of health complications among individuals with type 1 diabetes. Insulin therapy is indispensable for individuals with type 1 diabetes for life sustain, as it facilitates the transfer of blood glucose into fat after the body consumption. However, excessive insulin dosing leads to the disproportionate storage of energy in body fat mass, along with the episodes of hypoglycemia. For individuals with type 1 diabetes and severely impaired beta-cell function, hypoglycemia appears unavoidable in the long term, particularly during stressful events necessitating insulin replacement. Food intake following hypoglycemic episodes exacerbates the accumulation of fat mass, especially in regions such as China where the glucagon injections is unavailable.
Lifestyle modifications associated with type 1 diabetes may contribute to adiposity in affected individuals. Engaging in moderate-to-high intensity exercise requests tailored diet and insulin dose adjustments among individuals with type 1 diabetes[13], highlighting the need for comprehensive education and healthcare support. At the population level, such complexities can dampen the overall exercise intensity, while the fear of hypoglycemia can drive up overall energy intake among individuals with type 1 diabetes. Both phenomena escalate the risk of obesity and associated health complications. Inadequate exercise can lead to diminished skeletal muscular mass, which is linked to type 2 diabetes and other adverse health outcomes[14]. Zeng et al's report[11] observed reduced muscular mass among Chinese individuals with type 1 diabetes and correlated it with metabolic syndrome.
In people with type 1 diabetes and adiposity, insulin resistance is common and is associated with increased insulin dosages, resulting in a phenotype akin to those with type 2 diabetes and poor beta-cell function needing lifelong insulin replacement. Patients in both scenarios require multiple injections of insulin for type 1 diabetes and oral medications for type 2 diabetes. The interactive effects and complexity of the two treatment challenge the quality of life improvement and the prevention of metabolic complications. Europe and North America approved metformin, sodium-glucose cotransporter 2 (SGLT2) inhibitors, and glucagon-likepeptide-1 (GLP-1) receptor agonists for the early use of type 1 diabetes. Clinicians must consider the combined therapy of two diseases in a single individual: insulin replacement for type 1 diabetes and bodyweight management for type 2 diabetes. Integrating both arms in one person challenges the intelligence of clinicians and patients.
The risk factors of adiposity in people with type 1 diabetes were outlined in Figure 1.
Lifestyle modifications are crucial yet highly challenging for individuals with type 1 diabetes and adiposity. Attitudinal barriers may arise, especially in China, where many individuals have experienced frequent episodes of ketoacidosis and lean body mass during their early years. Weight loss efforts may evoke memories of poor glucose control and fear of acute complications of type 1 diabetes, most of which could be unwarranted. Cognitive interviews and associated personalized interventions have proven beneficial[15], relying on long-term follow-up by qualified multidisciplinary teams, which may be scarce in developing countries like China. Cognitive-behavioral therapy (CBT) and motivational in-terviewing aid individuals with type 1 diabetes in addressing and modifying underlying psychological and behavioral factors contributing to adiposity[16,17]. While these interventions improve adherence and facilitate enduring lifestyle changes, they may be prohibitively expensive and unattainable for many individuals in developing countries. Recent advancements in web-based technology support remote CBT, thereby increasing accessibility for a wider population with type 1 diabetes[18].
Besides insulin, medications designed for type 2 diabetes are also cornerstones in managing people with type 1 diabetes and adiposity. Metformin stands as one of the first approved oral medications for type 1 diabetes and is widely employed, particularly in those with excessive fat mass accumulation[19]. The addition of metformin reduces insulin dose requirements, which are associated increases in appetite. Initial use of metformin may precipitate mild gastrointestinal adverse events such as abdominal pain and nausea, though most people tolerate these effects following dose titration over several weeks. SGLT2 inhibitors was previously debated due to the risk of ketoacidosis in individuals with type 1 diabetes[20,21]. However, most clinicians now prescribe SGLT2 inhibitors for individuals with type 1 diabetes and adiposity, particularly those experiencing fluctuating blood glucose levels. In individuals with type 1 diabetes receiving regular insulin therapy, SGLT2 inhibitors stabilize blood glucose levels by lowering the glucose threshold in the kidneys, which excrete excess glucose during elevated blood levels[22]. Nonetheless, in people who do not adhere to insulin therapy, SGLT2 inhibitors may pose risks. Long-term use of SGLT2 inhibitors may also increase the risk of genital infections, amputations, and urinary malignancies[23-25], albeit with a very low absolute incidence. GLP-1 receptor agonists are also suggested for individuals with type 1 diabetes and obesity[26], improving body weight management and enhancing cardiovascular and kidney outcomes in the target population. Tirzepatide, a recent GLP-1 and gastric inhibitory polypeptide receptor dual agonist, is now a new contender for its potential benefits in body weight loss among patients with type 1 diabetes.
A supportive environment fosters healthy lifestyle habits and medication adherence at the societal level. The stigma of type 2 diabetes affects individuals with type 1 diabetes due to limited public awareness of the distinction between the two diabetes types[27]. The environment encompasses family members, colleagues, friends, and their involvement in daily activities, event planning, and financial support. Unlike other diseases, the Chinese healthcare system does not encompass type 1 diabetes in primary healthcare services. Unlike other conditions, clinicians are unlikely to assign a diagnosis of type 2 diabetes to individuals with type 1 diabetes. Primary care physicians may not recognize the comorbidity of type 1 and type 2 diabetes. Such dilemma limits the access of people with type 1 diabetes to body weight control as one of the treatments for type 2 diabetes and metabolic syndrome unless comorbidities such as hypertension and cardiovascular diseases are present.
In summary, adiposity, synonymous with obesity, is prevalent among people with type 1 diabetes in China and may be attributed to numerous cardiovascular and kidney adverse outcomes. The prevention and management of adipose accumulation in individuals with type 1 diabetes pose challenges due to multiple pathophysiological and socioeconomic factors, calling for urgent action by policymakers, researchers, clinicians, and patients.
| 1. | Li J, Shi Q, Gao Q, Pan XF, Zhao L, He Y, Tian H, Zhu Z, Li S. Obesity pandemic in China: epidemiology, burden, challenges, and opportunities. Chin Med J (Engl). 2022;135:1328-1330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Pan XF, Wang L, Pan A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021;9:373-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 1024] [Article Influence: 204.8] [Reference Citation Analysis (14)] |
| 3. | Weng J, Zhou Z, Guo L, Zhu D, Ji L, Luo X, Mu Y, Jia W; T1D China Study Group. Incidence of type 1 diabetes in China, 2010-13: population based study. BMJ. 2018;360:j5295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 227] [Article Influence: 28.4] [Reference Citation Analysis (1)] |
| 4. | Grabia M, Socha K, Bossowski A, Markiewicz-Żukowska R. Metabolic Syndrome as a Factor of Impairment of Antioxidant Defense System in Youth with T1DM. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | El-Wakkad A, Hassan Nel-M, Sibaii H, El-Zayat SR. Proinflammatory, anti-inflammatory cytokines and adiponkines in students with central obesity. Cytokine. 2013;61:682-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Ellulu MS, Patimah I, Khaza'ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017;13:851-863. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 793] [Cited by in RCA: 1314] [Article Influence: 146.0] [Reference Citation Analysis (0)] |
| 7. | Heerspink HJ, Cherney DZ, Groop PH, Matthieu C, Rossing P, Tuttle KR, McGill JB. People with type 1 diabetes and chronic kidney disease urgently need new therapies: a call for action. Lancet Diabetes Endocrinol. 2023;11:536-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 8. | Al-Makhamreh HK, Toubasi AA, Al-Harasis LM, Albustanji FH, Al-Sayegh TN, Al-Harasis SM. Pericardial fat and cardiovascular diseases: A systematic review and meta-analysis. J Evid Based Med. 2023;16:178-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Fan Y, Lau ESH, Wu H, Yang A, Chow E, Kong APS, Ma RCW, Chan JCN, Luk AOY. Incident cardiovascular-kidney disease, diabetic ketoacidosis, hypoglycaemia and mortality in adult-onset type 1 diabetes: a population-based retrospective cohort study in Hong Kong. Lancet Reg Health West Pac. 2023;34:100730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Gregory GA, Robinson TIG, Linklater SE, Wang F, Colagiuri S, de Beaufort C, Donaghue KC; International Diabetes Federation Diabetes Atlas Type 1 Diabetes in Adults Special Interest Group, Magliano DJ, Maniam J, Orchard TJ, Rai P, Ogle GD. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: a modelling study. Lancet Diabetes Endocrinol. 2022;10:741-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 625] [Article Influence: 156.3] [Reference Citation Analysis (0)] |
| 11. | Zeng Q, Chen XJ, He YT, Ma ZM, Wu YX, Lin K. Body composition and metabolic syndrome in patients with type 1 diabetes. World J Diabetes. 2024;15:81-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (1)] |
| 12. | Zheng Y, Rostami Haji Abadi M, Gough J, Johnston JJD, Nour M, Kontulainen S. Higher Body Fat in Children and Adolescents With Type 1 Diabetes-A Systematic Review and Meta-Analysis. Front Pediatr. 2022;10:911061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Riddell MC, Gallen IW, Smart CE, Taplin CE, Adolfsson P, Lumb AN, Kowalski A, Rabasa-Lhoret R, McCrimmon RJ, Hume C, Annan F, Fournier PA, Graham C, Bode B, Galassetti P, Jones TW, Millán IS, Heise T, Peters AL, Petz A, Laffel LM. Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol. 2017;5:377-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 701] [Cited by in RCA: 592] [Article Influence: 65.8] [Reference Citation Analysis (0)] |
| 14. | Liu D, Li N, Zhou Y, Wang M, Song P, Yuan C, Shi Q, Chen H, Zhou K, Wang H, Li T, Pan XF, Tian H, Li S. Sex-specific associations between skeletal muscle mass and incident diabetes: A population-based cohort study. Diabetes Obes Metab. 2024;26:820-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 15. | Harrison A, Konstantara E, Zaremba N, Brown J, Allan J, Pillay D, Hopkins D, Treasure J, Ismail K, Stadler M. A cognitive behavioural model of the bidirectional relationship between disordered eating and diabetes self care in adult men with Type 1 diabetes mellitus. Diabet Med. 2024;41:e15287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 16. | Rechenberg K, Koerner R. Cognitive Behavioral Therapy in Adolescents with Type 1 Diabetes: An Integrative Review. J Pediatr Nurs. 2021;60:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Vilarrasa N, San Jose P, Rubio MÁ, Lecube A. Obesity in Patients with Type 1 Diabetes: Links, Risks and Management Challenges. Diabetes Metab Syndr Obes. 2021;14:2807-2827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 18. | Newby J, Robins L, Wilhelm K, Smith J, Fletcher T, Gillis I, Ma T, Finch A, Campbell L, Andrews G. Web-Based Cognitive Behavior Therapy for Depression in People With Diabetes Mellitus: A Randomized Controlled Trial. J Med Internet Res. 2017;19:e157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 76] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 19. | Frandsen CS, Dejgaard TF, Madsbad S. Non-insulin drugs to treat hyperglycaemia in type 1 diabetes mellitus. Lancet Diabetes Endocrinol. 2016;4:766-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 20. | Nakamura Y, Horie I, Kitamura T, Kusunoki Y, Nishida K, Yamamoto A, Hirota Y, Fukui T, Maeda Y, Minami M, Matsui T, Kawakami A, Abiru N. Glucagon secretion and its association with glycaemic control and ketogenesis during sodium-glucose cotransporter 2 inhibition by ipragliflozin in people with type 1 diabetes: Results from the multicentre, open-label, prospective study. Diabetes Obes Metab. 2024;26:1605-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 21. | Nan J, Wang D, Zhong R, Liu F, Luo J, Tang P, Song X, Zhang L. Sodium glucose cotransporter2 inhibitors for type 1 diabetes mellitus: A meta-analysis of randomized controlled trials. Prim Care Diabetes. 2024;18:17-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | Qu F, Shi Q, Wang Y, Shen Y, Zhou K, Pearson ER, Li S. Visit-to-visit glycated hemoglobin A1c variability in adults with type 2 diabetes: a systematic review and meta-analysis. Chin Med J (Engl). 2022;135:2294-2300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 23. | Shi Q, Nong K, Vandvik PO, Guyatt GH, Schnell O, Rydén L, Marx N, Brosius FC 3rd, Mustafa RA, Agarwal A, Zou X, Mao Y, Asadollahifar A, Chowdhury SR, Zhai C, Gupta S, Gao Y, Lima JP, Numata K, Qiao Z, Fan Q, Yang Q, Jin Y, Ge L, Zhu H, Yang F, Chen Z, Lu X, He S, Chen X, Lyu X, An X, Chen Y, Hao Q, Standl E, Siemieniuk R, Agoritsas T, Tian H, Li S. Benefits and harms of drug treatment for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2023;381:e074068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 141] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 24. | Shen Y, Shi Q, Zou X, Meng W, Tian H, Du L, Li S. Time-dependent risk of fracture in adults with type 2 diabetes receiving anti-diabetic drug: A one-stage network meta-analysis. Diabetes Metab Res Rev. 2024;40:e3780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 25. | Han Z, He Y, Li X, Li S, Ai J. Insights into the impact of sodium-glucose cotransporter 2 inhibition on urinary tract malignancy: A two-sample Mendelian randomization. Diabetes Obes Metab. 2024;26:1986-1989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 26. | Park J, Ntelis S, Yunasan E, Downton KD, Yip TC, Munir KM, Haq N. Glucagon-Like Peptide 1 Analogues as Adjunctive Therapy for Patients With Type 1 Diabetes: An Updated Systematic Review and Meta-analysis. J Clin Endocrinol Metab. 2023;109:279-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 48] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 27. | Speight J, Holmes-Truscott E, Garza M, Scibilia R, Wagner S, Kato A, Pedrero V, Deschênes S, Guzman SJ, Joiner KL, Liu S, Willaing I, Babbott KM, Cleal B, Dickinson JK, Halliday JA, Morrissey EC, Nefs G, O'Donnell S, Serlachius A, Winterdijk P, Alzubaidi H, Arifin B, Cambron-Kopco L, Santa Ana C, Davidsen E, de Groot M, de Wit M, Deroze P, Haack S, Holt RIG, Jensen W, Khunti K, Kragelund Nielsen K, Lathia T, Lee CJ, McNulty B, Naranjo D, Pearl RL, Prinjha S, Puhl RM, Sabidi A, Selvan C, Sethi J, Seyam M, Sturt J, Subramaniam M, Terkildsen Maindal H, Valentine V, Vallis M, Skinner TC. Bringing an end to diabetes stigma and discrimination: an international consensus statement on evidence and recommendations. Lancet Diabetes Endocrinol. 2024;12:61-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 73] [Article Influence: 36.5] [Reference Citation Analysis (0)] |