Published online Apr 15, 2024. doi: 10.4239/wjd.v15.i4.724
Peer-review started: October 8, 2023
First decision: December 6, 2023
Revised: December 20, 2023
Accepted: February 27, 2024
Article in press: February 27, 2024
Published online: April 15, 2024
Processing time: 186 Days and 14.5 Hours
Diabetic cardiomyopathy (DCM), which is a complication of diabetes, poses a great threat to public health. Recent studies have confirmed the role of NLRP3 (NOD-like receptor protein 3) activation in DCM development through the infla
To examine the therapeutic effects of teneligliptin on DCM in diabetic mice.
Streptozotocin was administered to induce diabetes in mice, followed by trea
Marked increases in cardiomyocyte area and cardiac hypertrophy indicator heart weight/tibia length reductions in fractional shortening, ejection fraction, and heart rate; increases in creatine kinase-MB (CK-MB), aspartate transaminase (AST), and lactate dehydrogenase (LDH) levels; and upregulated NADPH oxidase 4 were observed in diabetic mice, all of which were significantly reversed by tene
Overall, teneligliptin mitigated DCM by mitigating activation of the NLRP3 inflammasome.
Core Tip: Teneligliptin mitigated diabetic cardiomyopathy by mitigating the activation of NLRP3 (NOD-like receptor protein 3) inflammasome. Teneligliptin reversal markedly increased cardiomyocyte area and heart weight/tibia length, reduced fractional shortening, ejection fraction, and heart rate, increased creatine kinase-MB (CK-MB), aspartate transaminase (AST), and lactate dehydrogenase (LDH) levels, and upregulated NADPH oxidase 4 in streptozotocin-induced diabetic mice. Teneligliptin repressed activated NLRP3 inflammasome and increased CK-MB, AST, and LDH levels in glucose-stimulated cardiomyocytes, accompanied by an upregulation of phosphorylated-adenosine 5‘-monophosphate and activated protein kinase.
- Citation: Zhang GL, Liu Y, Liu YF, Huang XT, Tao Y, Chen ZH, Lai HL. Teneligliptin mitigates diabetic cardiomyopathy by inhibiting activation of the NLRP3 inflammasome. World J Diabetes 2024; 15(4): 724-734
- URL: https://www.wjgnet.com/1948-9358/full/v15/i4/724.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i4.724
With the rapid development of international society and the economy, living standards have improved qualitatively. However, the prevalence of diseases has greatly increased, and diabetes mellitus (DM) is common. According to the International Diabetes Federation, there are 8.75 million people with type 1 diabetes (T1D) worldwide, or 0.11% of the global population. 1.52 million (17.0%) patients were younger than 20 years of age, 5.56 million (64.0%) patients were between 20 and 59 years of age, and 1.67 million (19.9%) patients were 60 years of age or older. In 2022, there will be 530000 newly diagnosed cases of T1D in all age groups, of which 200000 will be under 20 years old[1], posing a threat to public health. As a complication of DM, diabetic cardiomyopathy (DCM) is a condition in which the heart has abnormal myocardial structure and function in the absence of coronary artery disease, severe valvular lesions, or other conventional cardiovascular factors. DCM is characterized by lipid accumulation in the heart, myocardial fibrosis, and an increased probability of myocardial cell death, leading to left ventricular remodeling, hypertrophy, and diastolic dysfunction, which, in turn, contributes to systolic dysfunction[2]. The pathophysiological mechanism of DCM is related to an abn
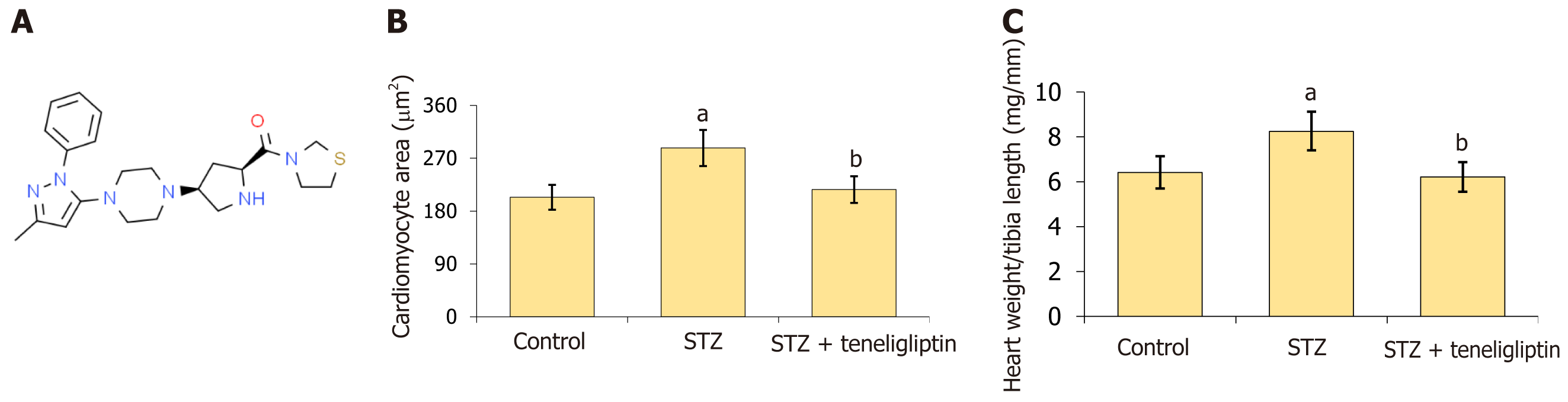
Teneligliptin (Figure 1A) is an oral hypoglycemic dipeptidyl peptidase-IV inhibitor developed by Mitsubishi Pharmaceutical Company in Japan that is mainly used to treat type II diabetes. By suppressing the inactivation of glucagon-like peptide in vivo by selectively inhibiting the activity of DPP-IV, teneligliptin promotes the production of insulin by islet cells and reduces the concentration of glucagon, thereby reducing blood glucose. Teneligliptin is well tolerated and has a low incidence of adverse reactions[7,8]. Recently, teneligliptin was shown to have a promising suppressive effect on infla
The streptozotocin (STZ) solution (S0130; Sigma-Aldrich, St Louis, MO, United States) was prepared with citric acid/sodium citrate buffer, and 55 mg/kg STZ was administered to C57BL/6 male mice by intraperitoneal injection for 5 consecutive days. One week later, blood was collected from the tail vein and fasting blood glucose levels were detected by a Roche blood glucose meter. The mouse model of DCM was considered successfully constructed if the fasting blood glucose level was higher than 16.7 mmol/L. The mice were divided into three groups: Vehicle, STZ, and teneligliptin (SML3077; Sigma-Aldrich). In the vehicle and STZ groups, normal mice and diabetic mice received oral doses of normal saline. In the teneligliptin group, diabetic mice were orally administered 30 mg/kg teneligliptin for 4 wk. This study was approved by the Ethics Committee of Jiangxi Provincial People's Hospital.
The mice were anesthetized by an intraperitoneal injection of sodium pentobarbital to maintain a heart rate of approximately 300 beats/min and then placed on a thermostatic heating plate connected to a high-resolution small animal ultrasonic apparatus (VisualSonics, Toronto, ON, Canada). The following parameters were recorded: End-systolic diameter (ESD) and end-systolic volume (ESV), end-diastolic diameter (EDD) and end-diastolic volume (EDV), and heart rate. Fractional shortening was calculated as (EDD-ESD)/EDD × 100%, and the ejection fraction was calculated as (EDV-ESV)/EDV × 100%.
The levels of creatine kinase-MB (CK-MB), aspartate transaminase (AST), lactate dehydrogenase (LDH), and interleukin (IL)-1β were detected by ELISA (R&D Systems, Minneapolis, MN, United States). The supernatant was collected and added to a 96-well plate and the standards were added. After incubation for 1.5 h, the conjugate solution was added to the wells, after which the plates were incubated for another 1.5 h. Next, tetramethylbenzidine solution (861510; Sigma-Aldrich) was added, followed by a 15 m of incubation. Finally, the stop solution was added to stop the reaction, after which the optical density was detected with a microplate reader (Molecular Devices, San Jose, CA, United States) at 450 nm.
The collected myocardium was rinsed with water for 2 h. After being dehydrated with different concentrations of ethanol, the tissues were dehydrated with xylene until transparent, embedded for 1 h and then sliced. After being heated, dewaxed, and hydrated, the sections were immersed in water and subsequently stained with hematoxylin aqueous reagent for 2–3 min. After being differentiated in hydrochloric acid ethanol, the sections were stained with the blue-returning reagent for several seconds. After being stained with eosin for 180 s, images were obtained using an inverted microscope (Nikon, Tokyo, Japan).
Total RNA was extracted from tissues or cells with TRIzol reagent, after which the RNA concentration was quantified with an ultraviolet spectrophotometer (Hach, Loveland CO, United States). RNA was transcribed to cDNA using a cDNA synthesis kit (SolelyBio, China). Subsequently, PCR was performed by using an SYBR Premix Ex TaqII kit (Takara, Shiga, Japan), and gene expression was determined by using the 2−ΔΔCt method.
Tissues or cells were lysed to extract total proteins, followed by quantification using the bicinchoninic acid assay method. The proteins were separated by 12% SDS-PAGE and subsequently transferred to PVDF membranes. After the membranes were blocked, primary antibodies against NADPH oxidase 4 (1:2000, 14347-1-AP; Proteintech, Rosemont, IL, United States), NLRP3 (1:2000, 14347-1-AP; Proteintech), caspase-1 (1:2000, 22915-1-AP; Proteintech), p-AMPK (1:1000, 4186; Cell Signaling Technology, Danvers, MA, United States), and β-actin (4970; Cell Signaling Technology) were used. Then, secondary antibodies (1:2000, 7074, 7076; Cell Signaling Technology) were added. The bands were visualized with en-hanced chemiluminescence solution for quantification.
Immature mice (0–2 d of age) were disinfected by immersion in 75% alcohol for 1–2 m. Then, a small incision was made under the sternum with sterilized ophthalmic scissors, after which the heart was collected and was placed in a Petri dish with precooled Hanks solution. The heart was then cut into 1 mm–3 mm pieces with scissors on an ultraclean table, followed by the addition of 7 mL of 0.1% type II collagenase. The rubber plug was blocked, the sealing membrane was added, and cells were then placed in a 37 °C incubator for 10 m until the cells naturally precipitated. The supernatant was discarded, and the digestion was terminated by gently mixing the solution approximately 60 times with a pipettor for 15 m. Then, the cell suspension was transferred to high glucose Dulbecco’s modified Eagle’s medium. The cell suspension obtained from each digestion was mixed until the tissue block was completely digested. The supernatant was discarded after being centrifuged at 1000 × rpm for 10 m, and an appropriate amount of complete medium was subsequently mixed with a 100 μm nylon screen and inoculated into the culture flask, which was subsequently cultured at 37 °C in a 5% carbon dioxide incubator. After 90 m, the supernatant was mostly purified, and the cardiomyocytes were transferred to another culture flask for further culture.
The data are presented as the mean ± SD and were analyzed using one-way analysis of variance with GraphPad Prism software 6.0 (La Jolla, CA, United States). P < 0.05 was considered to indicate a statistically significant difference.
WGA staining was used to detect myocardial hypertrophy. Cardiomyocyte area in STZ-treated mice increased from 203.6 μm2 to 287.5 μm2 and was markedly reduced to 216.7 μm2 by teneligliptin (Figure 1B). Moreover, the heart weight/tibia length in STZ-treated mice increased from 6.4 mg/mm to 8.3 mg/mm and was decreased to 6.2 mg/mm by teneligliptin (Figure 1C). Moreover, teneligliptin alleviated myocardial hypertrophy.
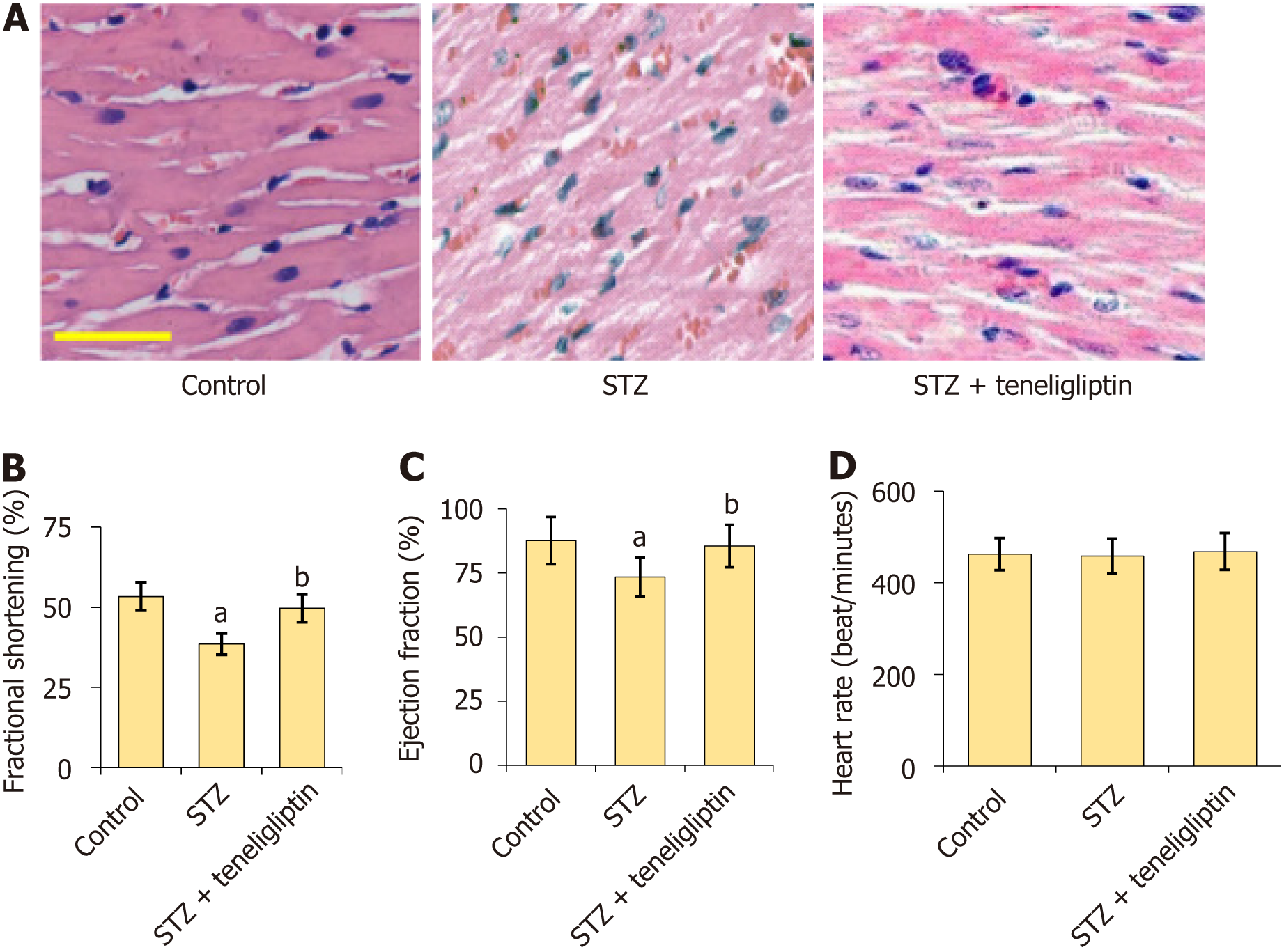
HE staining (Figure 2A) showed that myocardial cells in the vehicle group had a normal morphology, complete structure, dense and regular arrangement, and uniform distribution of nuclei. However, myocardial cells in diabetic mice were hypertrophic with a fuzzy structure, disordered arrangement, and some fiber breakage. The morphological structures of myocardial cells in the teneligliptin group were neat with relatively regular arrangements and improvements in hypertrophy and fiber breakage. The fractional shortening of diabetic mice decreased from 53.5% to 38.7% and was markedly increased to 49.6% by teneligliptin (Figure 2B). Furthermore, the ejection fractions in the vehicle, STZ, and teneligliptin groups were 87.6%, 73.5%, and 85.5%, respectively (Figure 2C). The heart rates of the diabetic mice decreased from 462.5 beats/min to 458.7 beats/minute and then increased to 468.3 beats/min in response to teneligliptin (Figure 2D). The heart function of diabetic mice was improved by teneligliptin.
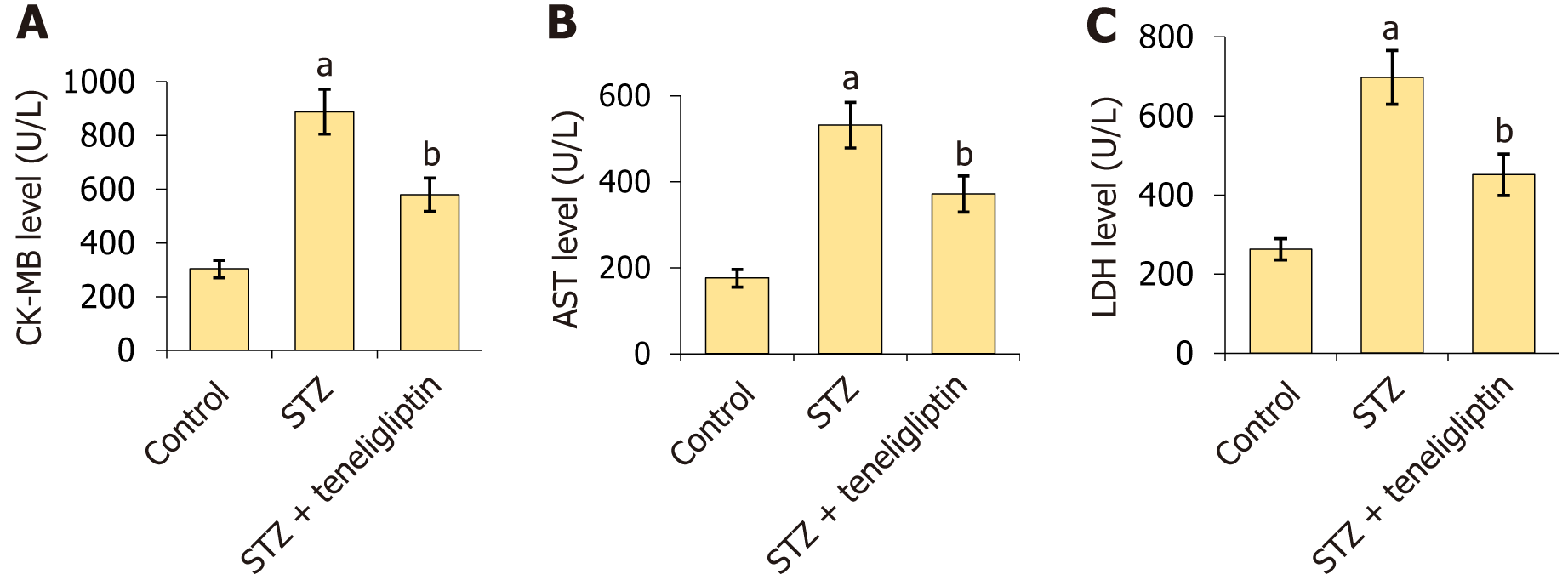
CK-MB levels in diabetic mice increased from 303.5 U/L to 888.8 U/L but were markedly reduced to 578.8 U/L by teneligliptin (Figure 3A). Moreover, AST levels in the vehicle, STZ, and teneligliptin groups were 176.3, 522.6, and 371.8 U/L, respectively (Figure 3B). LDH levels in diabetic mice increased from 262.7 U/L to 697.5 U/L and then decreased to 451.2 U/L in response to teneligliptin (Figure 3C).
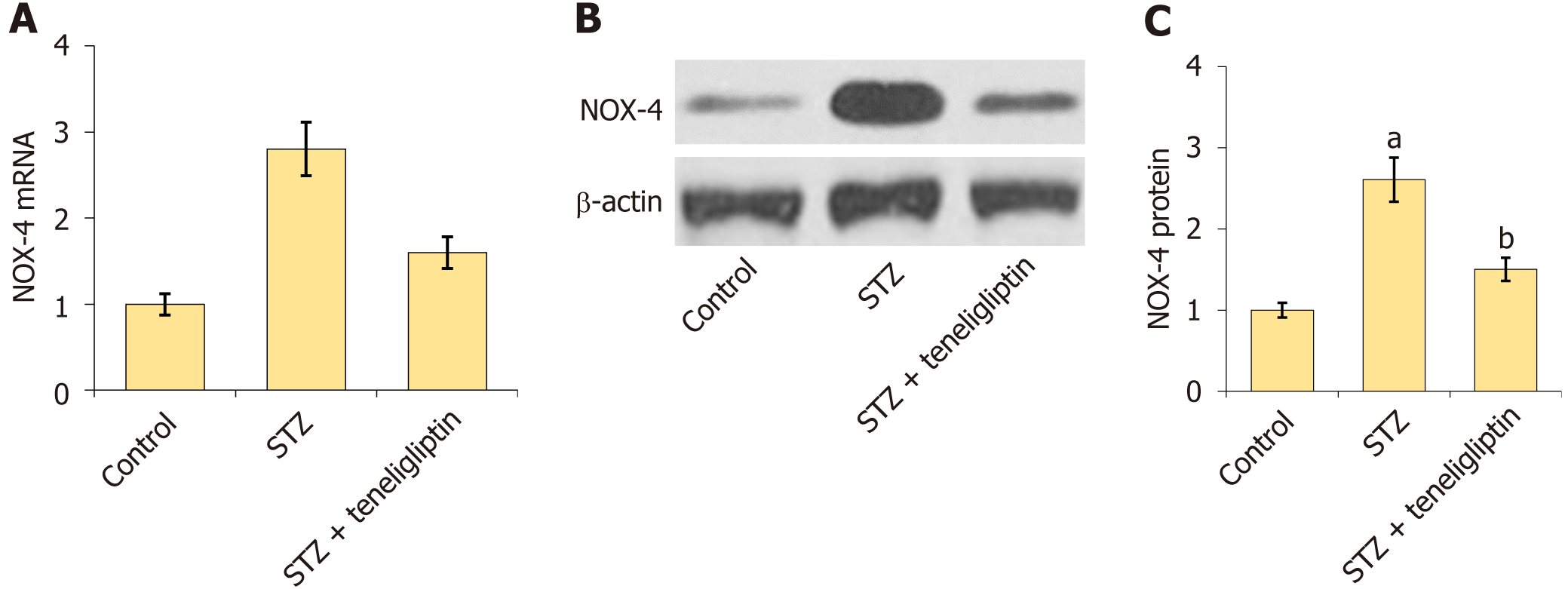
NOX4 is a critical pathological factor in DCM[12]. The increase in NOX4 levels in diabetic mice was markedly inhibited by teneligliptin (Figure 4).
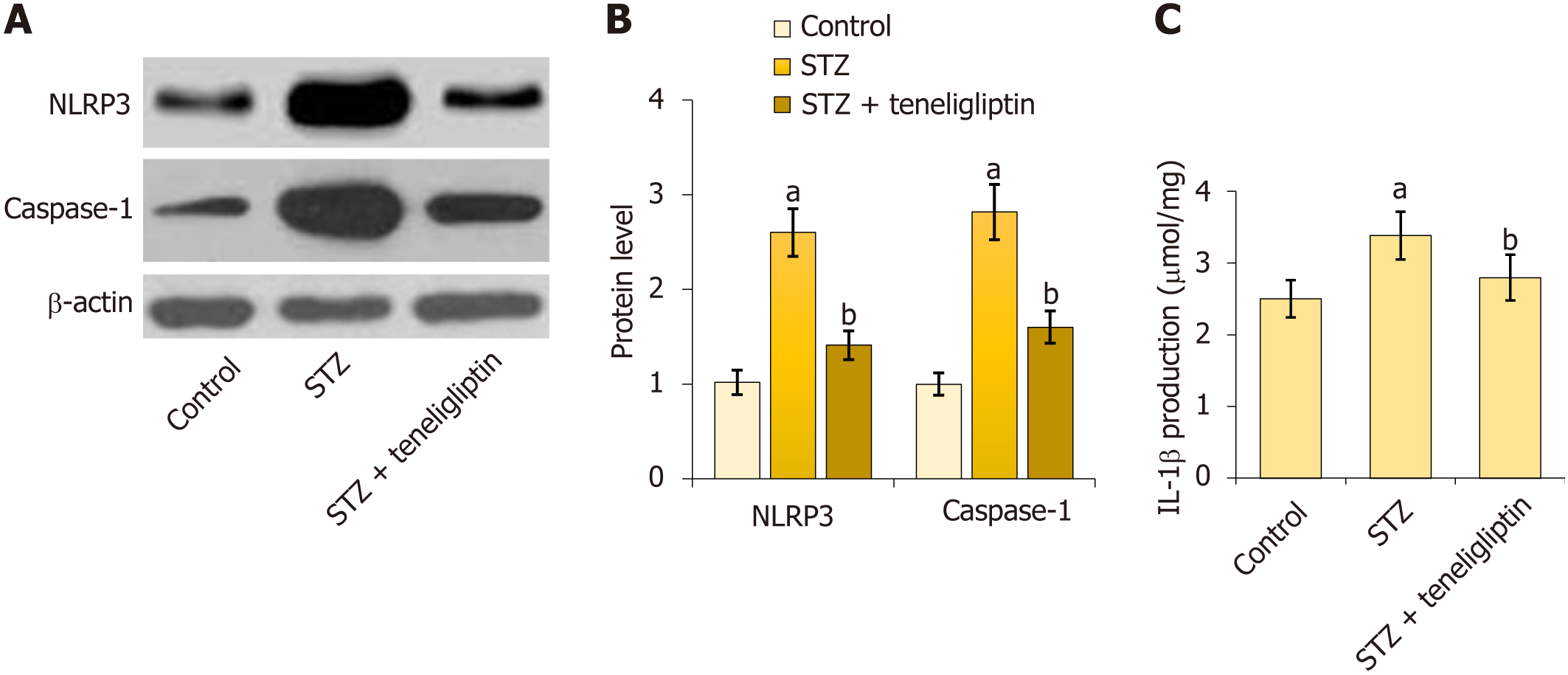
First, NLRP3 and caspase-1 were notably upregulated in diabetic mice but markedly decreased by teneligliptin (Figure 5A and B). Moreover, IL-1β levels in diabetic mice increased from 2.5 μmol/mg to 3.4 μmol/mg protein and then decreased to 2.8 μmol/mg protein in response to teneligliptin (Figure 5C). The suppressive effect of teneligliptin on the NLRP3 inflammasome in the heart was observed.
Primary mouse cardiomyocytes were extracted and treated with high glucose (30 mmol/L) with or without teneligliptin (2.5, 5 µM) for 24 h. NLRP3 and caspase-1 Levels in cardiomyocytes were markedly increased by 30 mmol/L glucose but were inhibited by 2.5 and 5 µM teneligliptin (Figure 6A). Moreover, IL-1β levels in the control, high glucose, 2.5 µM teneligliptin, and 5 µM teneligliptin groups were 1.5, 2.7, 2.1, and 1.8 μmol/mg protein, respectively (Figure 6B). CK-MB levels increased from 98.8 U/L to 288.5 U/L in 30 mmol/L glucose-treated cardiomyocytes and then decreased to 205.6 and 155.7 U/L in response to 2.5 and 5 µM teneligliptin, respectively. Furthermore, AST levels in the control, high glu
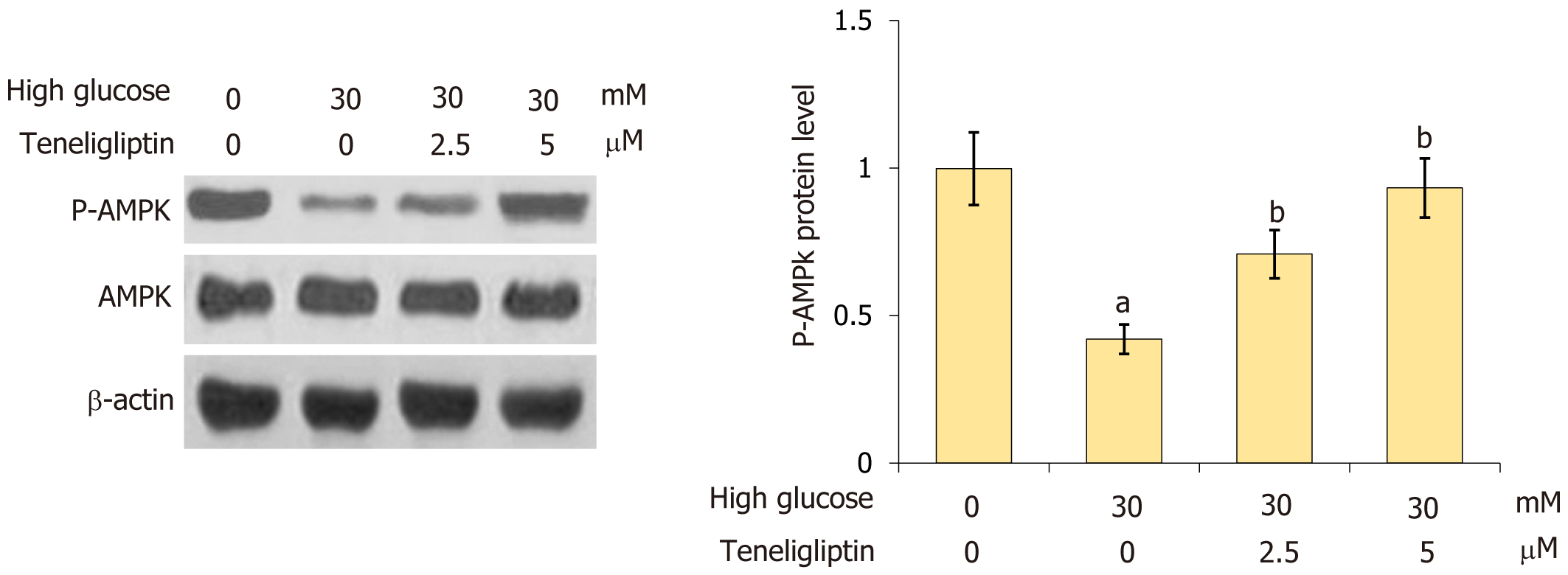
AMPK signaling reportedly regulates the NLRP3 inflammasome[13]. The decrease in p-AMPK in cardiomyocytes was reversed by 30 mmol/L glucose and this effect was markedly reversed by 2.5 and 5 µM teneligliptin (Figure 7), sug
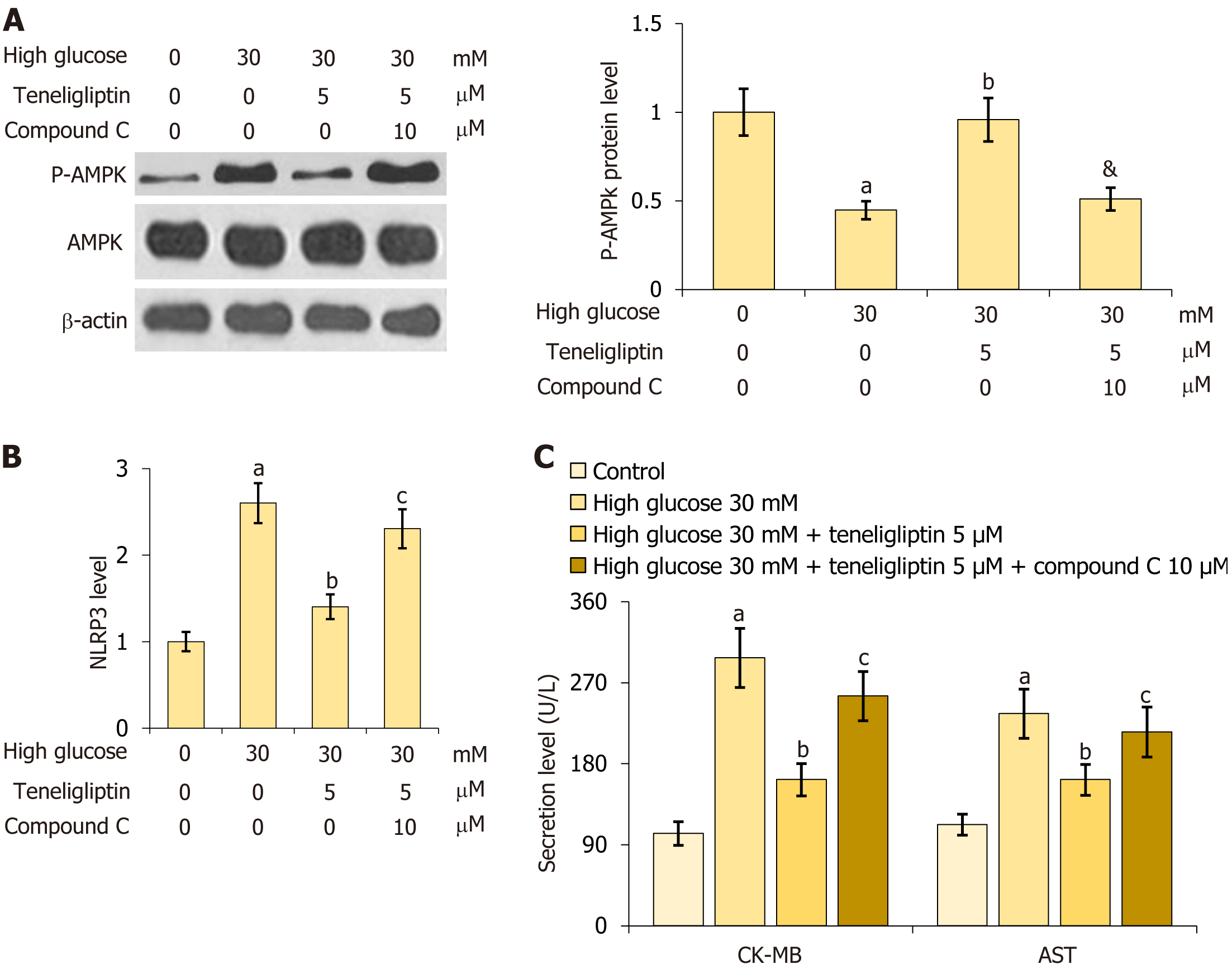
For verification, primary mouse cardiomyocytes were treated with high glucose (30 mmol/L) with or without teneligliptin (5 µM) and in the presence or absence of compound C (10 μM) for 24 h. First, the reduction in p-AMPK in 30 mmol/L glucose-treated cardiomyocytes was notably attenuated by teneligliptin, and this effect was reversed by compound C (Figure 8A). Furthermore, the increase in NLRP3 observed in 30 mmol/L glucose-treated cardiomyocytes was strongly reduced by teneligliptin but was elevated by compound C (Figure 8B). Moreover, CK-MB levels increased from 102.5 U/L to 297.6 U/L in 30 mmol/L glucose-treated cardiomyocytes and then greatly decreased to 162.3 U/L in response to teneligliptin. After the administration of compound C, CK-MB levels were reversed to 255.2 U/L. AST levels in the control, high glucose, teneligliptin, and teneligliptin+ compound C groups were 112.3, 235.6, 155.3, and 215.3 U/L, respectively (Figure 8C). The beneficial effects of teneligliptin on hyperglycaemia-induced cardiomyocytes were abolished by AMPK inhibition.
Studies have shown that NLRP3 is activated during DCM development through the inflammatory response and that teneligliptin exerts anti-inflammatory and protective effects in myocardial cells. In this study, we established an STZ-induced diabetes model and found that teneligliptin significantly inhibited cardiac hypertrophy and reduced fractional shortening and the ejection fraction induced by diabetes. Additionally, teneligliptin significantly reversed diabetes-induced increases in CK-MB, AST, and LDH. In addition, activation of the NLRP3 inflammasome and the increased release of IL-1β in diabetic mice were inhibited by teneligliptin, which was accompanied by the upregulation of p-AMPK. The same results were obtained in primary mouse cardiomyocytes treated with high glucose.
Teneligliptin is a low-cost oral hypoglycemic dipeptidyl peptidase-IV inhibitor that is used for diabetes treatment. Singh et al[14] searched 13 eligible studies containing data on 15720 subjects and showed similar efficacy (or better) and safety of teneligliptin compared with other DPP4Is. The average cost per tablet of teneligliptin (20 mg) was markedly lower than that of sitagliptin, vildagliptin, or other commonly used DPP4Is. Teneligliptin has various effects on both cardiovascular disease and other disorders. Teneligliptin can improve vascular endothelial function by improving flow-mediated vascular dilatation through divergent actions, including changes in circulating endothelial progenitor cells[15]. Teneligliptin-induced vasodilation occurs via the activation of protein kinase G, SERCA pumps and protein kinase G channels[16]. A systematic review of 13 randomized controlled trials that enrolled 2853 patients showed that teneligliptin was an effective and safe therapeutic option for patients with T2DM as a monotherapy and add-on therapy[17].
Teneligliptin has recently been reported to have anti-inflammatory and protective effects on myocardial cells, and DPP4 inhibitors have been reported to be associated with mitochondrial metabolism. Notably, teneligliptin enhances SIRT1 protein expression and activity through USP22, a ubiquitin-specific peptidase. Activated SIRT1 prevents hyper
NLRP3 is a NOD-like receptor sensor molecule[21] that belongs to the cytoplasmic NOD family of pattern recognition receptors. After being activated, NLRP3 undergoes self-oligomerization and assembles with ASC and the protease caspase-1 to form the NLRP3 inflammasome. This process results in the production of the active form of the caspase-1 p10/p20 splicer and induces the conversion of the proinflammatory cytokines IL-1β and IL-18 from their immature forms to their active forms, inducing an inflammatory response[22]. The NLRP3 inflammasome triggers a form of cell death known as pyroptosis. NLRP3 activation triggers the autocatalytic activation of caspase-1, which drives the cleavage of the gasdermin D protein to produce N'-segment protein fragments that bind to phospholipid proteins on the cell membrane, form holes, and release inflammatory factors. Subsequently, cells continue to expand until the membrane ruptures, which is the process of pyroptosis[23]. NLRP3 inhibition improves insulin sensitivity in obese mice, suggesting that NLRP3 may participate in metabolism-related diseases such as diabetes[24]. In addition, hyperglycemia reportedly activates NLRP3 inflammasome-mediated pyroptosis in myocardial cells, and knocking down NLRP3 in DCM rats reduces the inflammatory response in myocardial tissues, inhibits the occurrence of myocardial pyroptosis and myocardial interstitial fibrosis, and improves cardiac function[25,26]. These findings suggest that the NLRP3 inflammasome is involved in DCM development. In our study, DCM model mice were generated by STZ injection, and the results were verified by assessing myocardial hypertrophy, impaired heart function, and myocardial injury indicator production; these findings were consistent with previous studies[27,28]. Following the administration of teneligliptin, myocardial hypertrophy was alle
This study showed that teneligliptin improved cardiac function in DCM in vivo and in vitro and exerted its effect through NLRP3. One shortcoming of this study is that the direct effect of NLRP3 was not verified by knocking down or overexpressing NLRP3. In addition, the effect of teneligliptin on NLRP3-induced autophagy will be examined in future studies.
AMPK regulates NLRP3 inflammasome activation through multiple pathways, such as mitochondrial homeostasis, endoplasmic reticulum stress, autophagy, and SIRT1 activation. p-AMPK/AMPK is an important sensor molecule that regulates bioenergy homeostasis and reduces the activation of NF-κB to control the inflammatory response mediated by the NLRP3 inflammasome[31]. A previous study showed that autophagy was induced, mitochondrial ROS production was reduced, and IL-1β secretion was inhibited by mTOR inhibitors[32]. Autophagy is facilitated by AMPK through the activation of ULK or inhibition of the mTOR pathway. Furthermore, NLRP3 inflammasome activity is negatively regu
In summary, in this study, we established an STZ-induced diabetes model and found that teneligliptin significantly inhibited cardiac hypertrophy and reduced fractional shortening and the ejection fraction induced by diabetes. Through animal in vivo and cell in vitro experiments, we found that teneligliptin can improve DCM through NLRP3 pathway, which take to us that cell pyroptosis plays an important role in the improvement of DCM by treatment with teneligliptin. Future study should performed by NLPR3 knocking down and overexpressing to verified its direct effect, which is the main limitations of this study.
Overall, teneligliptin mitigated DCM by mitigating activation of the NLRP3 inflammasome, which suggests that in future clinical work, teneligliptin may treat diseases involving the NLRP3 pathway.
Diabetic cardiomyopathy (DCM), which is a complication of diabetes, poses a great threat to public health. Recent studies have confirmed the role of NLRP3 (NOD-like receptor protein 3) activation in DCM development through the inflammatory response. Teneligliptin is an oral hypoglycemic dipeptidyl peptidase-IV inhibitor used to treat diabetes. Teneligliptin has recently been reported to have anti-inflammatory and protective effects on myocardial cells.
This study examined the therapeutic effects of teneligliptin on DCM in diabetic mice.
Teneligliptin improves DCM by means of NLRP3, providing a new target for teneligliptin in the treatment of DCM.
Streptozotocin (STZ) was administered to induce diabetes in mice, followed by treatment with 30 mg/kg teneligliptin. Small animal ultrasonic apparatus was used to measure mice heart function, The levels of creatine kinase-MB (CK-MB), aspartate transaminase (AST), lactate dehydrogenase (LDH), and interleukin (IL)-1β were detected by ELISA, car
Marked increases in cardiomyocyte area and heart weight/tibia length; reductions in fractional shortening, ejection fraction, and heart rate; increases in CK-MB, AST, and LDH levels; and upregulated NADPH oxidase 4 were observed in diabetic mice, all of which were significantly reversed by teneligliptin. Moreover, NLRP3 inflammasome activation and increased release of IL-1β in diabetic mice were inhibited by teneligliptin. Primary mouse cardiomyocytes were treated with high glucose (30 mmol/L) with or without teneligliptin (2.5 or 5 µM) for 24 h. NLRP3 inflammasome activation and the increases in CK-MB, AST, and LDH levels in glucose-stimulated cardiomyocytes were markedly inhibited by teneligliptin, and AMP (p-adenosine 5‘-monophosphate)-p-AMPK (activated protein kinase) levels were increased. Furthermore, the beneficial effects of teneligliptin on hyperglycaemia-induced cardiomyocytes were abolished by the AMPK signaling inhibitor compound C.
Overall, teneligliptin mitigated DCM by mitigating activation of the NLRP3 inflammasome.
Our study suggests that in future clinical work, teneligliptin may treat diseases involving the NLRP3 pathway.
| 1. | Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Claude Mbanya J, Pavkov ME, Ramachandaran A, Wild SH, James S, Herman WH, Zhang P, Bommer C, Kuo S, Boyko EJ, Magliano DJ. Erratum to "IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045" [Diabetes Res. Clin. Pract. 183 (2022) 109119]. Diabetes Res Clin Pract. 2023;204:110945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 94] [Reference Citation Analysis (0)] |
| 2. | Japp AG, Gulati A, Cook SA, Cowie MR, Prasad SK. The Diagnosis and Evaluation of Dilated Cardiomyopathy. J Am Coll Cardiol. 2016;67:2996-3010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 370] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 3. | Tan Y, Zhang Z, Zheng C, Wintergerst KA, Keller BB, Cai L. Mechanisms of diabetic cardiomyopathy and potential therapeutic strategies: preclinical and clinical evidence. Nat Rev Cardiol. 2020;17:585-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 592] [Article Influence: 98.7] [Reference Citation Analysis (35)] |
| 4. | Zeng C, Duan F, Hu J, Luo B, Huang B, Lou X, Sun X, Li H, Zhang X, Yin S, Tan H. NLRP3 inflammasome-mediated pyroptosis contributes to the pathogenesis of non-ischemic dilated cardiomyopathy. Redox Biol. 2020;34:101523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 294] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 5. | Zheng Y, Xu L, Dong N, Li F. NLRP3 inflammasome: The rising star in cardiovascular diseases. Front Cardiovasc Med. 2022;9:927061. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 76] [Reference Citation Analysis (0)] |
| 6. | Zhang H, Chen X, Zong B, Yuan H, Wang Z, Wei Y, Wang X, Liu G, Zhang J, Li S, Cheng G, Wang Y, Ma Y. Gypenosides improve diabetic cardiomyopathy by inhibiting ROS-mediated NLRP3 inflammasome activation. J Cell Mol Med. 2018;22:4437-4448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 125] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 7. | Scott LJ. Teneligliptin: a review in type 2 diabetes. Clin Drug Investig. 2015;35:765-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Sharma SK, Panneerselvam A, Singh KP, Parmar G, Gadge P, Swami OC. Teneligliptin in management of type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2016;9:251-260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Liu X, Cao Y, Zhang Y, Sun B, Liang H. Teneligliptin inhibits lipopolysaccharide-induced cytotoxicity and inflammation in dental pulp cells. Int Immunopharmacol. 2019;73:57-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Sagara M, Suzuki K, Aoki C, Tanaka S, Taguchi I, Inoue T, Aso Y. Impact of teneligliptin on oxidative stress and endothelial function in type 2 diabetes patients with chronic kidney disease: a case-control study. Cardiovasc Diabetol. 2016;15:76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Peng W, Rao D, Zhang M, Shi Y, Wu J, Nie G, Xia Q. Teneligliptin prevents doxorubicin-induced inflammation and apoptosis in H9c2 cells. Arch Biochem Biophys. 2020;683:108238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Fan L, Xiao Q, Zhang L, Wang X, Huang Q, Li S, Zhao X, Li Z. CAPE-pNO(2) attenuates diabetic cardiomyopathy through the NOX4/NF-κB pathway in STZ-induced diabetic mice. Biomed Pharmacother. 2018;108:1640-1650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Yang F, Qin Y, Wang Y, Meng S, Xian H, Che H, Lv J, Li Y, Yu Y, Bai Y, Wang L. Metformin Inhibits the NLRP3 Inflammasome via AMPK/mTOR-dependent Effects in Diabetic Cardiomyopathy. Int J Biol Sci. 2019;15:1010-1019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 279] [Cited by in RCA: 372] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 14. | Singh H, Arora E, Narula S, Singla M, Otaal A, Sharma J. Finding the most cost-effective option from commonly used Dipeptidyl peptidase-4 inhibitors in India: a systematic study. Expert Rev Endocrinol Metab. 2023;18:347-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Akashi N, Umemoto T, Yamada H, Fujiwara T, Yamamoto K, Taniguchi Y, Sakakura K, Wada H, Momomura SI, Fujita H. Teneligliptin, a DPP-4 Inhibitor, Improves Vascular Endothelial Function via Divergent Actions Including Changes in Circulating Endothelial Progenitor Cells. Diabetes Metab Syndr Obes. 2023;16:1043-1054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 16. | Li H, An JR, Park M, Choi J, Heo R, Kang M, Mun SY, Zhuang W, Seo MS, Han ET, Han JH, Chun W, Park WS. The antidiabetic drug teneligliptin induces vasodilation via activation of PKG, Kv channels, and SERCA pumps in aortic smooth muscle. Eur J Pharmacol. 2022;935:175305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 17. | Pelluri R, Kongara S, Nagasubramanian VR, Mahadevan S, Chimakurthy J. Systematic review and meta-analysis of teneligliptin for treatment of type 2 diabetes. J Endocrinol Invest. 2023;46:855-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Elumalai S, Karunakaran U, Moon JS, Won KC. High glucose-induced PRDX3 acetylation contributes to glucotoxicity in pancreatic β-cells: Prevention by Teneligliptin. Free Radic Biol Med. 2020;160:618-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Zhang Z, Jin X, Yang C, Li Y. Teneligliptin protects against hypoxia/reoxygenation-induced endothelial cell injury. Biomed Pharmacother. 2019;109:468-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Enoki Y, Watanabe H, Arake R, Fujimura R, Ishiodori K, Imafuku T, Nishida K, Sugimoto R, Nagao S, Miyamura S, Ishima Y, Tanaka M, Matsushita K, Komaba H, Fukagawa M, Otagiri M, Maruyama T. Potential therapeutic interventions for chronic kidney disease-associated sarcopenia via indoxyl sulfate-induced mitochondrial dysfunction. J Cachexia Sarcopenia Muscle. 2017;8:735-747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 126] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 21. | Inoue M, Shinohara ML. The role of interferon-β in the treatment of multiple sclerosis and experimental autoimmune encephalomyelitis - in the perspective of inflammasomes. Immunology. 2013;139:11-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19:477-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1426] [Cited by in RCA: 3537] [Article Influence: 589.5] [Reference Citation Analysis (0)] |
| 23. | Mangan MSJ, Olhava EJ, Roush WR, Seidel HM, Glick GD, Latz E. Targeting the NLRP3 inflammasome in inflammatory diseases. Nat Rev Drug Discov. 2018;17:688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 372] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 24. | Shao BZ, Xu ZQ, Han BZ, Su DF, Liu C. NLRP3 inflammasome and its inhibitors: a review. Front Pharmacol. 2015;6:262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 399] [Cited by in RCA: 670] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 25. | Luo B, Huang F, Liu Y, Liang Y, Wei Z, Ke H, Zeng Z, Huang W, He Y. NLRP3 Inflammasome as a Molecular Marker in Diabetic Cardiomyopathy. Front Physiol. 2017;8:519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 173] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 26. | Frangogiannis NG. The Extracellular Matrix in Ischemic and Nonischemic Heart Failure. Circ Res. 2019;125:117-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 395] [Article Influence: 56.4] [Reference Citation Analysis (0)] |
| 27. | Tong M, Saito T, Zhai P, Oka SI, Mizushima W, Nakamura M, Ikeda S, Shirakabe A, Sadoshima J. Mitophagy Is Essential for Maintaining Cardiac Function During High Fat Diet-Induced Diabetic Cardiomyopathy. Circ Res. 2019;124:1360-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 399] [Article Influence: 66.5] [Reference Citation Analysis (0)] |
| 28. | Arow M, Waldman M, Yadin D, Nudelman V, Shainberg A, Abraham NG, Freimark D, Kornowski R, Aravot D, Hochhauser E, Arad M. Sodium-glucose cotransporter 2 inhibitor Dapagliflozin attenuates diabetic cardiomyopathy. Cardiovasc Diabetol. 2020;19:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 166] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 29. | Song S, Ding Y, Dai GL, Zhang Y, Xu MT, Shen JR, Chen TT, Chen Y, Meng GL. Sirtuin 3 deficiency exacerbates diabetic cardiomyopathy via necroptosis enhancement and NLRP3 activation. Acta Pharmacol Sin. 2021;42:230-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 162] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 30. | Shi C, Wu L, Li L. LncRNA-MALAT 1 regulates cardiomyocyte scorching in diabetic cardiomyopathy by targeting NLRP3. Cell Mol Biol (Noisy-le-grand). 2022;67:213-219. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 31. | Cordero MD, Williams MR, Ryffel B. AMP-Activated Protein Kinase Regulation of the NLRP3 Inflammasome during Aging. Trends Endocrinol Metab. 2018;29:8-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 123] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 32. | Chen-Scarabelli C, Agrawal PR, Saravolatz L, Abuniat C, Scarabelli G, Stephanou A, Loomba L, Narula J, Scarabelli TM, Knight R. The role and modulation of autophagy in experimental models of myocardial ischemia-reperfusion injury. J Geriatr Cardiol. 2014;11:338-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 33. | Dong Y, Chen H, Gao J, Liu Y, Li J, Wang J. Molecular machinery and interplay of apoptosis and autophagy in coronary heart disease. J Mol Cell Cardiol. 2019;136:27-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 323] [Article Influence: 46.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pappachan JM, United Kingdom; Soriano-Ursúa MA, Mexico S-Editor: Lin C L-Editor: Filipodia P-Editor: Zhang YL