Published online Apr 15, 2024. doi: 10.4239/wjd.v15.i4.638
Peer-review started: December 19, 2023
First decision: January 9, 2024
Revised: January 29, 2024
Accepted: February 27, 2024
Article in press: February 27, 2024
Published online: April 15, 2024
Processing time: 114 Days and 23.6 Hours
Age is a significant risk factor of diabetes mellitus (DM). With the develop of population aging, the incidence of DM remains increasing. Understanding the epidemiology of DM among elderly individuals in a certain area contributes to the DM interventions for the local elderly individuals with high risk of DM.
To explore the prevalence of DM among elderly individuals in the Lugu com
A total of 4816 elderly people who came to the community for physical exami
DM was diagnosed in 32.70% of the 4816 elderly people. The BMI of the DM group (25.16 ± 3.35) was greater than that of the non-DM group (24.61 ± 3.78). The WHR was 0.90 ± 0.04 in the non-DM group and 0.90 ± 0.03 in the DM group, with no significant difference. The left SBP and SBP in the DM group were 137.9 mmHg ± 11.92 mmHg and 69.95 mmHg ± 7.75 mmHg, respectively, while they were 126.6 mmHg ± 12.44 mmHg and 71.15 mmHg ± 12.55 mmHg, respectively, in the non-DM group. These findings indicate higher SBP and lower DBP in DM patients than in those without DM. In the DM group, 1274 patients were dia
Older adults in the Lugu community are at a greater risk of DM. In elderly individuals, DM is closely related to high BMI and HT, CHD, and CKD. Physical examinations should be actively carried out for elderly people to determine their BMI, SBP, DBP, and other signs, and sufficient attention should be given to abnormalities in the above signs before further diagnosis.
Core Tip: Age is a significant risk factor of diabetes mellitus (DM). An investigation focusing on the prevalence and risk factors of DM among elderly individuals is necessary. A total of 4816 elderly people who came to the community for physical examination were retrospectively analyzed in this study. older adults in the Lugu community are at high risk of DM, a disease highly correlated with high body mass index (BMI) and hypertension, coronary heart disease and chronic kidney disease in the elderly population. Therefore, physical examinations should be actively carried out for elderly individuals in the Lugu community to determine their demographic indices, such as BMI, systolic pressure, and diastolic pressure. Moreover, adequate attention should be given to those with abnormal signs, and blood glucose levels should be further determined.
- Citation: Zhao LZ, Li WM, Ma Y. Prevalence and risk factors of diabetes mellitus among elderly patients in the Lugu community. World J Diabetes 2024; 15(4): 638-644
- URL: https://www.wjgnet.com/1948-9358/full/v15/i4/638.htm
- DOI: https://dx.doi.org/10.4239/wjd.v15.i4.638
Type 2 diabetes mellitus (T2DM) is a multifactorial chronic metabolic disorder characterized by hyperglycemia and insulin resistance[1]. The pathogenesis of this type of DM mainly involves: (1) The lack of insulin secreted by pancreatic cells in vivo; and (2) the inability of insulin-sensitive tissues to respond to insulin[2]. In recent years, the number of people with DM has shown a significant upward trend, especially in Asia[3]. China has one of the highest prevalence rates of DM in Asia, and it faces an enormous burden of DM[4], with approximately 11% of the population affected by the disease[5]. In addition to causing problems such as metabolic disorders caused by their own diseases, DM may also increase the risk of patients suffering from retinopathy[6], stroke[7], nephropathy[8], cardiovascular diseases[9] and other diseases.
The aging population and changing lifestyles have made DM more common among older adults[10]. Currently, elderly individuals, especially those aged 60-79 years, have a high incidence of DM, with nearly 50% of patients being aged ≥ 65 years[11]. DM is associated with a high risk of metabolic disorders in elderly individuals, which may increase mortality and reduce quality of life in older adults[12]. It is argued that DM increases the risk of hypoglycemia in older adults, which can lead to cognitive impairment, cardiovascular disease and even death[13]. Therefore, it is necessary to consider the glycemic indices of the elderly population, focusing on elderly individuals who may have DM or have been dia
The purpose of this study was to explore the prevalence of DM among elderly individuals in the Lugu community and analyze the related risk factors. A total of 4816 older adults who came to the community for physical examination were included, and clinical signs such as body mass index (BMI), waist-to-hip ratio (WHR), and systolic blood pressure (SBP) and diastolic blood pressure (DBP) were collected to diagnose hypertension (HT) and DM. The findings of this study will help to understand the DM status of elderly individuals in the Lugu community and provide corresponding health mana
In this study, physical examination data were collected from 37562 people who had physical examinations in the Lugu community, among whom 4816 elderly people (aged ≥ 60 years) were analyzed retrospectively. The weight, height, waist circumference, hip circumference, DBP, SBP, fasting BG (FBG), BMI, and WHR of the elderly individuals were analyzed, as was the incidence of DM and its risk factors.
BP testing: The subjects had no strenuous exercise within 30 min before BP testing. Left SBP and DBP were measured using a noninvasive automatic sphygmomanometer. Subjects who showed SBP was at least 140 mmHg and/or their DBP was at least 90 mmHg at each of the three non-same-day measurements was considered to be HT.
FBG detection: Venous blood was collected at 7:00-9:00 am in the morning after overnight fasting for 8-12 h. The blood sample was placed in a centrifuge tube containing heparin sodium (heparin sodium: blood = 1:9) and centrifuged at 3000 rpm for 10 min, after which the supernatant was carefully aspirated to obtain plasma samples. BG levels were measured by a BS-300 automatic biochemical analyzer. Patients with a FBG ≥ 7.0 mmol/L were further tested to determine whether they had DM.
BMI: The body weight (kg) and height (m) of the subjects were measured, and the BMI (BMI = weight/height2) was calculated.
WHR: Waist circumference (cm) and hip circumference (cm) were measured to calculate the WHR (WHR= waist circumference/hip circumference).
The data visualization process of this study was carried out with GraphPad 9.0, and the research data are displayed as pie charts and histograms. This study employed SPSS 22.0 software for statistical analysis. The data were tested for normality using the Shapiro-Wilk test, and the mean and variance were calculated for normally distributed data. Intergroup differences in BMI, WHR, SBP, and DBP were identified using an independent sample t test, and the number of hyper
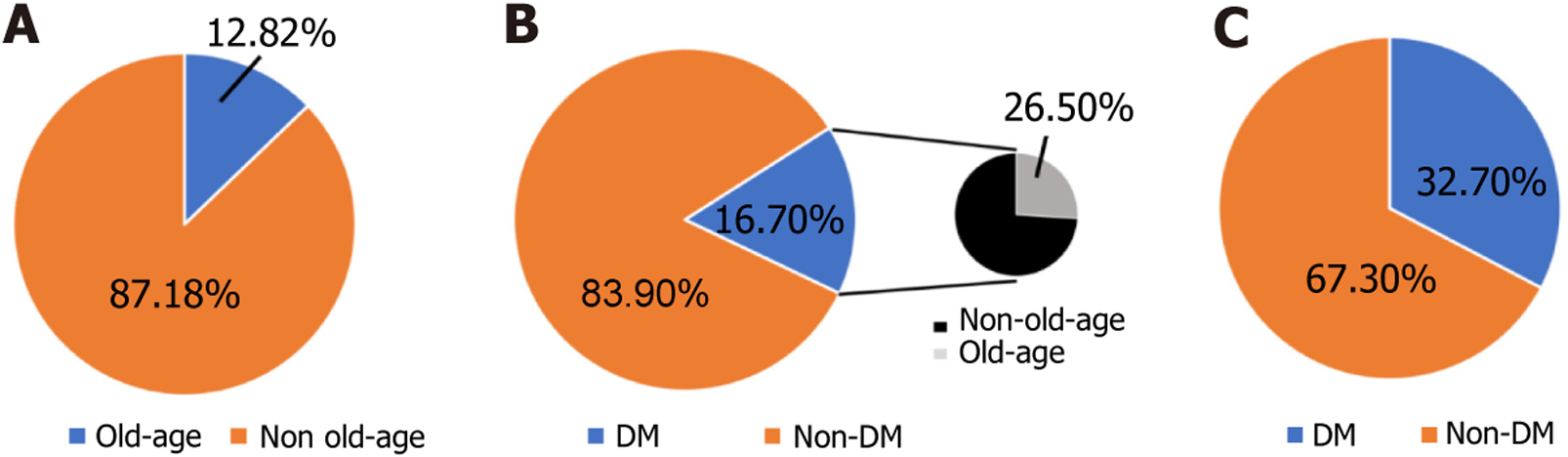
This study enrolled 37562 community physical examinees, including 4816 (12.82%) elderly people (Figure 1A). Of the 6046 (16.10%) confirmed cases of DM in the total physical examination population, 1575 (26.05%) were elderly DM patients (Figure 1B). Among the 4816 elderly people, 32.70% were diagnosed with DM (Figure 1C). The age of patients in the DM group ranged from 65-81 years, and that of patients in the non-DM group ranged from 67-82 years. Additionally, of the patients in the DM group, 1029 were females and 546 were males. There were 1667 females and 1574 males in the non-DM group. Accordingly, we speculate that DM is a common disease among elderly individuals in the Lugu com
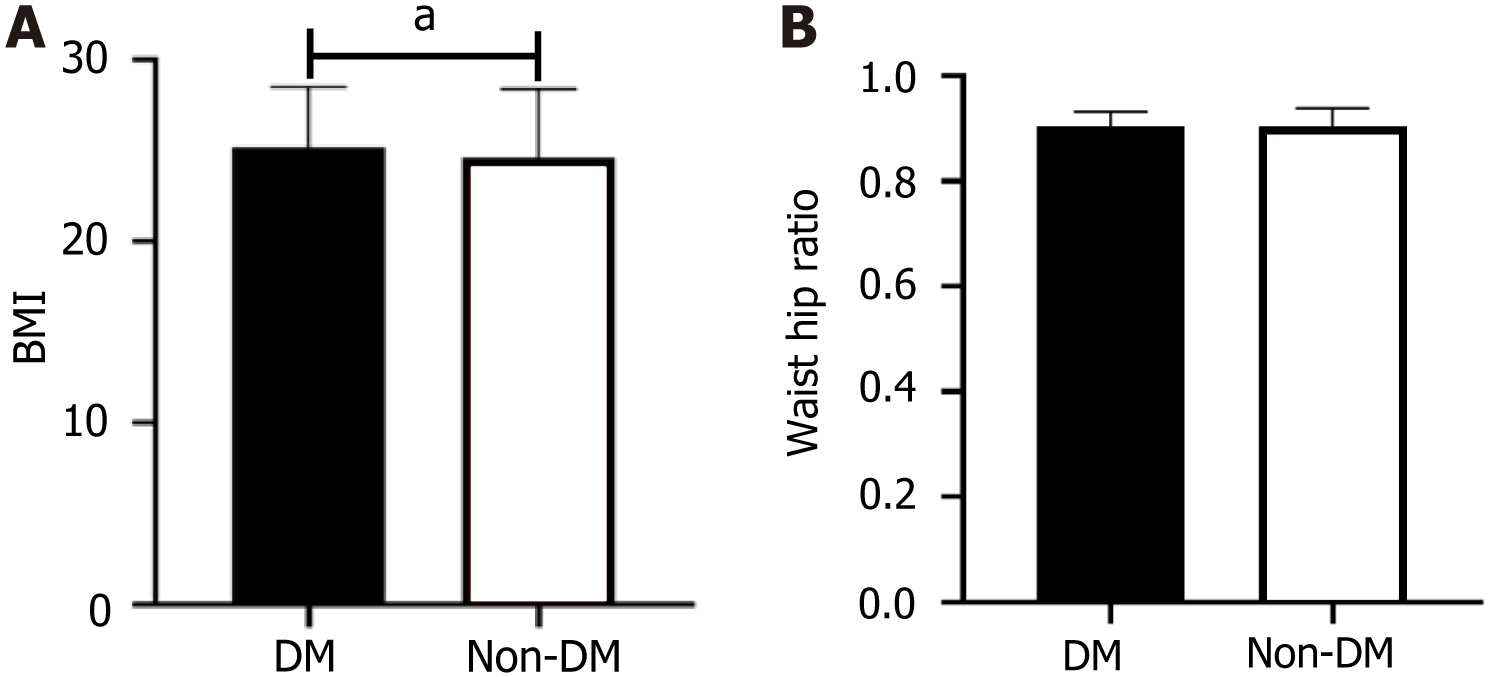
In this study, 4816 elderly people were divided into a DM group and a non-DM group according to their diagnosis of DM, and their BMI was determined. The results showed that the BMI of the individuals in the DM group was 25.16 ± 3.35, while that of the individuals in the non-DM group was 24.61 ± 3.78 (Figure 2A), and these two groups were signi
We also calculated the WHR of both groups and found that the WHR was 0.90 ± 0.04 in the non-DM group and 0.90 ± 0.03 in the DM group, with no significant difference (P > 0.05; Figure 2B). Overall, we believe that DM patients have a slightly greater risk of obesity than non-DM patients.
The SBP and DBP of the elderly individuals in the two groups were calculated, and the results are shown in Table 1. The left SBP and DBP in the DM group were 137.9 mmHg ± 11.92 mmHg and 69.95 mmHg ± 7.75 mmHg, respectively, while they were 126.6 mmHg ± 12.44 mmHg and 71.15 mmHg ± 12.55 mmHg, respectively, in the non-DM group. The above data revealed significantly greater SBP and lower DBP in the DM group than in the non-DM group.
| DM group (n = 1575) | Non-DM group (n = 3241) | t value | P value | |
| Systolic blood pressure (left side) | 137.90 ± 11.92 | 126.60 ± 12.44 | 4.779 | < 0.001 |
| Diastolic blood pressure (left side) | 69.95 ± 7.75 | 71.15 ± 12.55 | 3.475 | 0.005 |
In this study, we analyzed the relationship between HT and DM incidence. In the DM group, 1274 patients were confirmed to have HT, accounting for 80.89%. Among the 3241 non-DM patients, 1743 (53.78%) were hypertensive, and 1498 (46.22%) were nonhypertensive (Table 2). According to the statistical analysis, the number of hypertensive patients in the DM group was much greater than that in the non-DM group (P < 0.05). There were more patients with coronary heart disease (CHD) or CKD in the DM group than in the non-DM group (P < 0.05) (Table 2). Additionally, there were more patients who drank alcohol more frequently (≥ 3 times) in the DM group than in the non-DM group. Therefore, the results obtained in this study suggested that HT is related to DM among elderly individuals in the Lugu community.
| DM group (n = 1575) | Non-DM group (n = 3241) | χ2 value | P value | |
| 332.9 | < 0.001 | |||
| Hypertension | 1274 | 1743 | ||
| Nonhypertension | 301 | 1498 | ||
| 227.8 | < 0.001 | |||
| Coronary heart disease | 992 | 1291 | ||
| Noncoronary heart disease | 583 | 1950 | ||
| 182.4 | < 0.001 | |||
| Chronic kidney disease | 986 | 1357 | ||
| Non chronic kidney disease | 589 | 1884 | ||
| Alcohol consumption, frequency per week | 641.1 | < 0.001 | ||
| < 1 time | 198 | 1569 | ||
| 1-2 times | 529 | 854 | ||
| ≥ 3 times | 848 | 818 |
The pathogenesis of DM is complicated and involves many factors. For elderly people, the pathophysiological changes caused by aging affect internal metabolic regulation, thus promoting the occurrence of DM; subsequently, aging and DM interact to further promote the progression of diabetic complications; this can also explain the ever-higher incidence of DM among elderly people[15]. A study of atherosclerosis risk based on 5791 older adults revealed that elderly individuals with pre-DM were at a lower risk of death, while those with long-term DM had a higher mortality rate[16], highlighting the importance of timely screening for DM among elderly individuals. In addition, DM is often asymptomatic, and identifying the presence of DM is often difficult until a blood sugar test is performed[17]. Hence, it is necessary to analyze the risk of DM according to other signs. This study included 4816 elderly people to analyze the prevalence of DM and associated risk factors and revealed that HT and high BMI were common in elderly diabetic patients.
The BMI of diabetic elderly individuals was found to be greater than that of nondiabetic elderly individuals. A person can be defined as underweight, normal weight, overweight or obese based on their BMI[18], with a higher BMI indicating a greater degree of fat accumulation. Older people often face the risk of obesity[19], which may further increase the risk of DM. Fat accumulation may be the pathological basis of DM. An obesity environment disrupts the dynamic balance of metabolism, which in turn causes fat accumulation and altered insulin secretion, leading to DM[20]. In contrast, weight loss is associated with improved glycemic control. For elderly individuals whose BMI is close to the warning value or who are already overweight, although they are not currently affected by DM, they should still be urged to control their diet and maintain good exercise habits to return their BMI to normal[21]. It is worth noting that the number of female diabetic patients in this study was higher than that of male patients, which may be related to the local dietary patterns, living habits, and health promotion. Therefore, it is necessary to expand the sample size in subsequent studies to verify the difference in the male-to-female ratio of diabetic patients.
We also noted that the incidence of HT in diabetic patients was greater than that in nondiabetic patients. HT and DM go hand in hand. On the one hand, insulin resistance leads to the destruction of vascular function, resulting in symptoms such as an increase in BP and vascular stiffness; on the other hand, arteriosclerosis and impaired vasodilation contribute to the progression of DM[22]. Research[23] has shown that HT can be an independent predictor of DM and that HT and DM have similar metabolic syndrome phenotypes. Over time, DM also interacts with HT, leading to microvascular and macrovascular lesions and increasing the risk of death[24]. Therefore, HT is an important symptom that cannot be ignored during the progression of DM. Older adults with abnormal BP, especially high BP, need attention before being diagnosed with DM. Additionally, we found that patients with DM have a high risk of CHD and CKD. High-frequency alcohol consumption seems to be related to the occurrence of DM in Lugu Lake.
Overall, we believe that older adults in the Lugu community are at high risk of DM, a disease highly correlated with high BMI and HT, CHD and CKD in the elderly population. Therefore, physical examinations should be actively carried out for elderly individuals in the Lugu community to determine their demographic indices, such as BMI, SBP, and DBP. Moreover, adequate attention should be given to those with abnormal signs, and BG levels should be further determined. The findings of this paper provide a valid scientific basis for the health management of elderly individuals in the Lugu community.
The pathogenesis of diabetes mellitus (DM) is complicated and involves many factors. For elderly people, the path
It is necessary to consider the glycemic indices of the elderly population, focusing on those who may have DM or have been diagnosed. Understanding the prevalence of DM among elderly people in a certain area and discussing the risk factors related to DM are conducive to carrying out targeted interventions for the local elderly population and developing effective blood glucose (BG) management strategies.
To explore the prevalence of DM among elderly people in the Lugu community and analyze the related risk factors to provide a valid scientific basis for the health management of elderly people.
A total of 4816 elderly people who came to the community for physical examination were retrospectively analyzed. The prevalence of DM among the elderly was calculated. The individuals were divided into a DM group and a non-DM group according to the diagnosis of DM to compare the differences blood pressure (DBP) in diastolic and systolic blood pressure (SBP), fasting BG (FBG), BMI, waist-to-hip ratio (WHR) and incidence of hypertension (HT), coronary heart disease, and chronic kidney disease (CKD).
DM was diagnosed in 32.70% of the 4816 elderly people. The BMI of the DM group (25.16 ± 3.35) was greater than that of the non-DM group (24.61 ± 3.78). The WHR was 0.90 ± 0.04 in the non-DM group and 0.90 ± 0.03 in the DM group, with no significant difference. The left SBP and SBP in the DM group were 137.9 mmHg ± 11.92 mmHg and 69.95 mmHg ± 7.75 mmHg, respectively, while they were 126.6 mmHg ± 12.44 mmHg and 71.15 mmHg ± 12.55 mmHg, respectively, in the non-DM group. These findings indicate higher SBP and lower DBP in DM patients than in those without DM. In the DM group, 1274 patients were diagnosed with HT, accounting for 80.89%. Among the 3241 non-DM patients, 1743 (53.78%) were hypertensive and 1498 (46.22%) were nonhypertensive. The DM group had more cases of HT than did the non-DM group. There were more patients with coronary heart disease or CKD in the DM group than in the non-DM group. There were more patients who drank alcohol more frequently (≥ 3 times) in the DM group than in the non-DM group.
Older adults in the Lugu community are at a higher risk of DM. In the elderly population, DM is closely related to high BMI and HT. Physical examinations should be actively carried out for elderly people to determine their BMI, SBP, DBP, and other signs, and sufficient attention should be given to abnormalities in the above signs before further diagnosis.
The findings of this paper provide a valid scientific basis for the health management of elderly individuals in the Lugu community.
| 1. | Peer N, Balakrishna Y, Durao S. Screening for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2020;5:CD005266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, Ostolaza H, Martín C. Pathophysiology of Type 2 Diabetes Mellitus. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 278] [Cited by in RCA: 1663] [Article Influence: 277.2] [Reference Citation Analysis (0)] |
| 3. | Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14:88-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2249] [Cited by in RCA: 3699] [Article Influence: 462.4] [Reference Citation Analysis (0)] |
| 4. | Sun J, Ji J, Wang Y, Gu HF. Association of the Haze and Diabetes in China. Curr Diabetes Rev. 2021;17:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Ma RCW. Epidemiology of diabetes and diabetic complications in China. Diabetologia. 2018;61:1249-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 377] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 6. | Li M, Wang Y, Liu Z, Tang X, Mu P, Tan Y, Wang J, Lin B, Deng J, Peng R, Zhang R, He Z, Li D, Zhang Y, Yang C, Li Y, Chen Y, Liu X. Females with Type 2 Diabetes Mellitus Are Prone to Diabetic Retinopathy: A Twelve-Province Cross-Sectional Study in China. J Diabetes Res. 2020;2020:5814296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | He C, Wang W, Chen Q, Shen Z, Pan E, Sun Z, Lou P, Zhang X. Factors associated with stroke among patients with type 2 diabetes mellitus in China: a propensity score matched study. Acta Diabetol. 2021;58:1513-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Faselis C, Katsimardou A, Imprialos K, Deligkaris P, Kallistratos M, Dimitriadis K. Microvascular Complications of Type 2 Diabetes Mellitus. Curr Vasc Pharmacol. 2020;18:117-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 337] [Article Influence: 56.2] [Reference Citation Analysis (0)] |
| 9. | Yun JS, Ko SH. Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes. Metabolism. 2021;123:154838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 174] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 10. | Strain WD, Hope SV, Green A, Kar P, Valabhji J, Sinclair AJ. Type 2 diabetes mellitus in older people: a brief statement of key principles of modern day management including the assessment of frailty. A national collaborative stakeholder initiative. Diabet Med. 2018;35:838-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 81] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 11. | Bellary S, Kyrou I, Brown JE, Bailey CJ. Type 2 diabetes mellitus in older adults: clinical considerations and management. Nat Rev Endocrinol. 2021;17:534-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 340] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 12. | Rodríguez-Pascual C, Rodriguez-Justo S, García-Villar E, Narro-Vidal M, Torrente-Carballido M, Paredes-Galan E. Quality of life, characteristics and metabolic control in diabetic geriatric patients. Maturitas. 2011;69:343-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Freeman J. Management of hypoglycemia in older adults with type 2 diabetes. Postgrad Med. 2019;131:241-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 79] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 14. | Sesti G, Antonelli Incalzi R, Bonora E, Consoli A, Giaccari A, Maggi S, Paolisso G, Purrello F, Vendemiale G, Ferrara N. Management of diabetes in older adults. Nutr Metab Cardiovasc Dis. 2018;28:206-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | LeRoith D, Biessels GJ, Braithwaite SS, Casanueva FF, Draznin B, Halter JB, Hirsch IB, McDonnell ME, Molitch ME, Murad MH, Sinclair AJ. Treatment of Diabetes in Older Adults: An Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2019;104:1520-1574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 345] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 16. | Tang O, Matsushita K, Coresh J, Sharrett AR, McEvoy JW, Windham BG, Ballantyne CM, Selvin E. Mortality Implications of Prediabetes and Diabetes in Older Adults. Diabetes Care. 2020;43:382-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 17. | Malone JI, Hansen BC. Does obesity cause type 2 diabetes mellitus (T2DM)? Pediatr Diabetes. 2019;20:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 235] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 18. | Weir CB, Jan A. BMI Classification Percentile And Cut Off Points. 2023 Jun 26. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 19. | Bales CW, Porter Starr KN. Obesity Interventions for Older Adults: Diet as a Determinant of Physical Function. Adv Nutr. 2018;9:151-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | La Sala L, Pontiroli AE. Prevention of Diabetes and Cardiovascular Disease in Obesity. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 21. | Aras M, Tchang BG, Pape J. Obesity and Diabetes. Nurs Clin North Am. 2021;56:527-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 22. | Jia G, Sowers JR. Hypertension in Diabetes: An Update of Basic Mechanisms and Clinical Disease. Hypertension. 2021;78:1197-1205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 244] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 23. | Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and Diabetes Mellitus: Coprediction and Time Trajectories. Hypertension. 2018;71:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 190] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 24. | Yildiz M, Esenboğa K, Oktay AA. Hypertension and diabetes mellitus: highlights of a complex relationship. Curr Opin Cardiol. 2020;35:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee JH, South Korea; Shapiro AMJ, Canada S-Editor: Chen YL L-Editor: A P-Editor: Zhang YL