INTRODUCTION
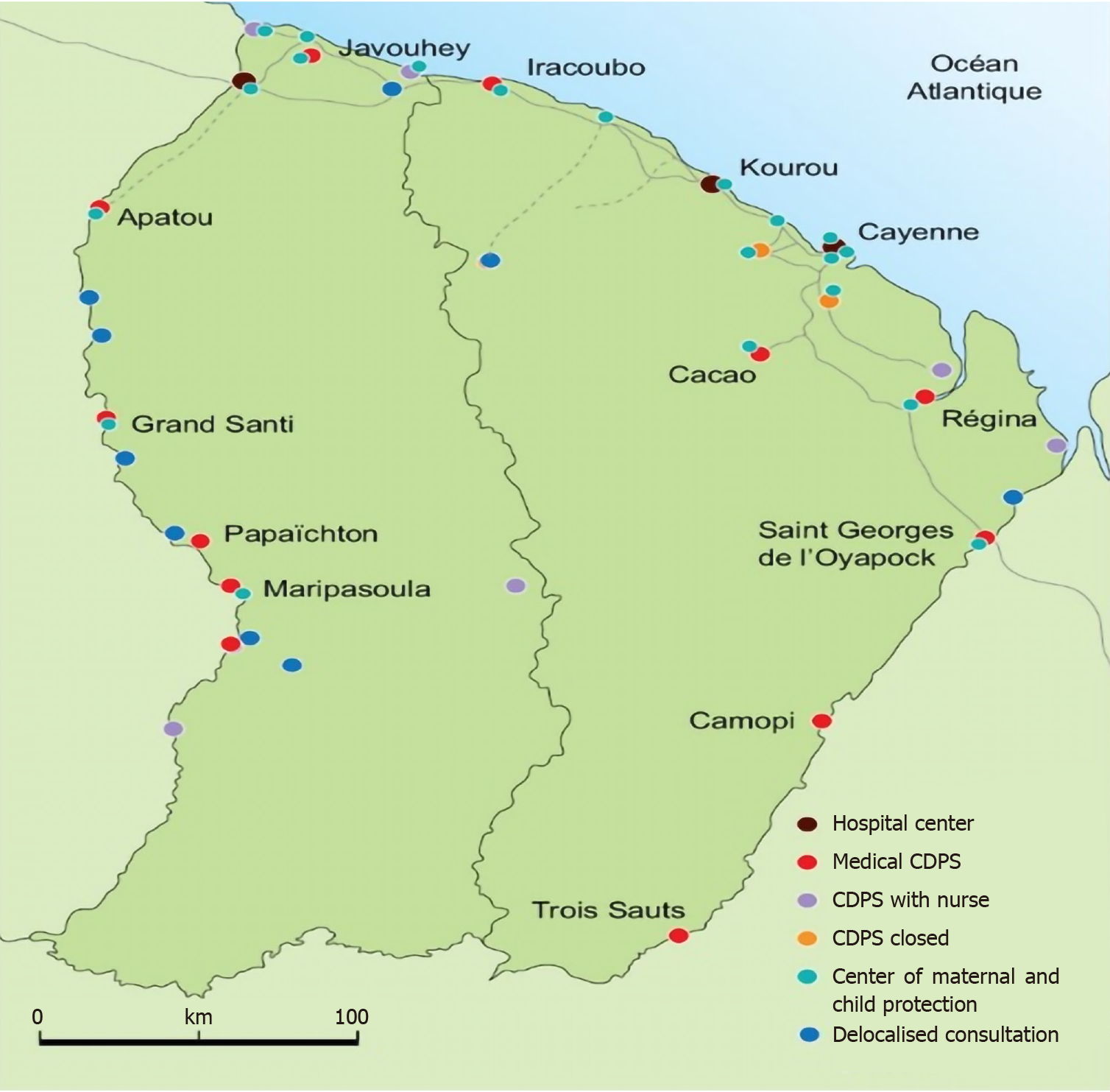
French Guiana, one of the largest French territories, extends over more than 83846 km[1]. It is divided into 22 municipalities and represents more than 15% of the surface of Mainland France. It is also the territory with the largest forest area and has some of the richest animal and plant biodiversity in the world[1,2]. Most of French Guiana's territory (over 90%) is made up of a vast tropical rainforest. French Guiana, located on the Guiana Shield, is bordered by several countries: Brazil, Suriname (Dutch Guiana), and it is very near Guyana (British Guiana). This closeness partly explains its multiculturality and cultural richness. The population is officially 296700 inhabitants and the birth rate is high compared to other French territories as it is 26%, and the population growth rate is 3.2%, which will double the population between 2007 and 2030[2]. There are regular waves of migration partly related to successive social crises in neighboring countries including Haiti (crises of 1978-1996, instability in 2018)[3] and natural disasters (earthquakes)[4]. Thus, based on a published study on social disparities in French Guiana, we note the precarious situation in the two main cities, a migrant population of about 40% in Cayenne and 58% in Saint-Laurent du Maroni[5]. The majority of the population is concentrated on the Atlantic Ocean coastline; the rest of the territory, mainly covered with Amazonian forest is very sparsely populated, notably by the Amerindian populations or Bushinenges. The under-developed road network, does not allow satisfactory access to all the territory and in particular serves only the coastal zone. The lack of road infrastructure partly explains the great difficulties in access to care and its unavailability to the most isolated populations who sometimes have to travel several days by road and canoes before arriving at one of the two main hospitals (the Cayenne Hospital or the Hospital of Saint Laurent du Maroni, still called Western French Guiana Healthcare Center). There is a significant poverty level, with more than 30% of the population in French Guiana vs 14% of the population in Mainland France, and the unemployment rate is 23% vs 10%[6]. Nonetheless, there are 18 Remote Prevention and Care Centers (CDPS) (community health centers) that provide care to the most isolated populations, and sometimes with great difficulties related to lack of medical and para-medical staff and logistics difficulties related to remoteness (Figure 1). It is also important to take into account the greater pre-cariousness of these populations, which have little financial means, and who do not have access to air or road transportation when they are available. They live sometimes in very slum-like housing, without water and without electricity, which would represent 20% according to the report of the IEOM (The Overseas Territories Issuing Institute) before 2014[7]. The different ethnic groups in the territory explain the linguistic and cultural diversity and the marked mixed heritage in French Guiana. There are more than twenty ethnic groups, including Creoles, Chinese, Hmongs, Amerindian who were the first inhabitants of French Guiana (Kalina, Lokono, Wayanas, Teko, Wayampis, and Palikurs), and the Bushinenge population. There are also many immigrants from Haiti, and Brazil, but also Guyana or Suriname[8]. Medical shortage (with a medical density 47% lower than in Mainland France)[9], adds to the geographical and cultural difficulties. In the field of endocrinology diabetology, there is only one hospital specialist in Cayenne and a general practitioner with knowledge on how to treat diabetes in Saint Laurent du Maroni, with these two institutions being 4 h away. There are two endocrinologists in the private sector for the entire territory, which is three times less than in Mainland France (endocrinologist density is 2.7 per 100000 inhabitants)[10].
Figure 1 Remote healthcare centers and hospitals in French Guiana.
DIABETES IN FRENCH GUIANA: THE STATE OF AFFAIRS
The prevalence of diabetes is about 8% in French Guiana, twice as much as in Mainland France. It is probably underestimated because the current figures come from health insurance data, which do not include patients without health insurance[11,12]. Furthermore, there are more people who are obese and overweight, and the PODIUM study conducted in several overseas territories reported 18% of obese people and 30% of overweight people in 2012[13]. According to the latest data from the report on the application of the health insurance financing laws of 2018, it is estimated that 35% of patients have complementary universal medical coverage, compared to 8% in Mainland France (CMU-C is free complementary health insurance[6], and is intended for persons with low resources permanently residing in France). The number of patients with State Medical Aid (AME is a program that allows undocumented foreigners to benefit from access to healthcare, and is awarded under conditions of stable residence for more than 3 months in the territory and based on economic resources) is around 16896. The latest figures from health insurance, assessing people without proper access to healthcare, amounted to 18% of the population in 2010.
For the poor and those who have been in an irregular situation for less than three months in the territory, urgent care may be provided (definition: Urgent care whose absence would be life-threatening or which could lead to serious and lasting compromise of the state of health of the individual or a child awaiting birth) exclusively in public or private health facilities either during in-patient or out-patient treatment, including the provision of medicines.
The International Diabetes Federation confirms this prevalence data with an estimate of 8.3%, placing French Guiana among the 10 regions of South America and Central America with the highest prevalence of diabetes in 2013, just below Brazil[14]. Amerindian and Afro-American populations are considered among the populations most at risk of developing diabetes[15].
French Guiana is often described as a young territory where infectious and tropical diseases represent the main public health issue. However, when looking at the leading causes of premature death, neurovascular pathologies are at the forefront. The epidemiologic transition from infectious diseases to chronic pathologies is already well underway. The increase in the incidence of diabetes is probably multifactorial; however, one of the major cause of diabetes in French Guiana is being overweight and obese, which concerns one in every two adults[16]. It has been shown that migrants, who are socially most vulnerable, have a delayed diagnosis of many infectious or chronic diseases, a higher rate of loss of vision, and increased mortality; the main studies published that have made this clear have been in the field of tropical diseases[17] or cancer, especially breast cancer[18].
THERAPEUTIC EDUCATION IN DIABETOLOGY (DIABETES SELF-MANAGEMENT EDUCATION) IN THE FRENCH AMAZON
The state of affairs regarding treatments, the complications of diabetes and its educational approach in French Guiana is difficult to report due to the lack of published data.
Therapeutic education is an essential part of the management of chronic pathologies, which allows the patient to understand their pathology and adhere more easily to follow-up and treatment[19]. It reduces micro and macrovascular com-plications[20].
New technologies such as tele-medicine and tele-consultation hosted by secure health data servers make it possible to monitor patients through the transmission of glycemic data instantly. Patient monitoring in tele-medicine allows a regular and adapted adjustment of anti-diabetic treatments or insulin therapy; however, only patients with access to a smartphone and a phone network will benefit from such monitoring. In French Guiana, the most isolated areas do not have telephone operator coverage or have very bad coverage and the most precarious do not have a smartphone or Internet subscription. A Norwegian study found a significant difference between the level of education, high income and use of phone apps[21].
An understanding of the territory and its cultural diversity make it difficult to set up homogeneous educational programs and these must be adapted according to the region and ethnic groups. At the level of the three remote health centers with the highest prevalence of diabetes, various educational programs have been set up. We have respectively 330 diabetics in the Oyapock (St Georges and Camopi), 106 in the higher Maroni (Maripassoula, Papaichton, Talhuen and Antecumpata), and 117 in the lower Maroni (Apatou and Grand Santi), who represent more than 20% of the reasons for consultation (from the 2017 remote health centers activity report) (Figure 2). Migrants are often in a precarious situation and have great difficulty in accessing healthcare, and are more exposed to chronic pathologies[5,22]. They often have a limited understanding of their disease, and their knowledge is often influenced by cultural beliefs, notably for chronic diseases. The therapeutic education that allows the patient to understand and accept their pathology and especially in the context of diabetes mellitus, remains very much utopic in populations who are culturally different, and the language barrier is often the first obstacle. Therapeutic education programs are carried out in association with cultural mediators who perform both the translation and the adaptation of the discourse according to each person's beliefs and culture. The example of the Grand Santi center, which is the only healthcare center on the French bank on 180 km of river between Apatou and Papaïchton, is an important one. The medical and paramedical team has put together a comic book and educational films translated into the Sranan Tongo language. Evaluation of the therapeutic education program is often difficult to carry out because of the understanding of the questions asked in the qualitative evaluation grid, but also regarding the evaluation plan of the biological criteria such as hemoglobin A1c (HbA1c), as the patients, due the access difficulties, are not all reevaluated within comparable intervals, and evaluations will only be performed if they have access to the health center.
Figure 2 Healthcare centers of Trois-Sauts and Camopi.
Thus, at Cayenne Hospital, as the single reference service, we have set up two therapeutic education structures, one in the endocrinology-diabetology department where two therapeutic education nurses offer workshops and individual interviews, sometimes with the help of a cultural mediator, and educational tools (films, audio and paper) translated into the most frequently spoken languages in French Guiana. Language is one of the first difficulties because of the many ethnic groups in the territory; the recruitment of a cultural mediator associated with translation and educational consultations is one of the main goals. Cultural mediators, most often from the patient community, foster reciprocal understanding and communication between patients and health professionals and enable the multicultural interface of two value systems. The second difficulty lies in the frequency of illiteracy, particularly in recent immigrant populations, which limits the use of educational tools such as cards or leaflets and forces us to work mainly on visual and auditory aids. A study conducted in an emergency department in Guyana, an English-speaking country bordering French Guiana, found that illiteracy was associated with high HbA1c and often in the context of previously undiagnosed diabetes and highlighted during the Emergency room consultation[23]. Given the problems of access to healthcare, we have also set up a mobile therapeutic education program in the city of Cayenne and its surroundings. It travels to different locations in Cayenne and its surroundings, and includes a coordinator, a therapeutic education nurse, a sports educator, a dietician, a psychologist and a part-time cultural mediator. This sector is reserved for outpatients, and general practitioners may register their patients on an electronic calendar via a website. The procedure is very simple and is the beginning of a three-month cycle, once the patient is included (after consent) in the sector to receive the benefit after an initial educational review. The unit is mobile and moves throughout 15 locations (pharmacies, houses, town hall, community halls, etc.) in Cayenne and surrounding areas to reach patients with difficulties in mobility. Nonetheless, the poorest patients often live in precarious homes. The income of these populations is often extremely low, and it is difficult for them to access public transportation. In a study by Valmy et al[24] conducted in one of the poor neighborhoods of Cayenne, 20% of patients earned less than 300 euros per month, 35.2% less than 500 euros and 55% less than 800 euros (the minimum net monthly wage is 1137 euros)[24]. Socially disadvantaged patients have a harder time achieving glycemic equilibrium. A study by Houle et al[25] showed that the significant effects of poverty and education on HbA1c were mediated by avoidance and depressive symptoms[25]. Depression and anxiety are often associated with diabetes[26,27], which amounts to more than 17% of diabetic patients according to the study by Wang et al[28], especially in low-income populations; they have a lower glycemic equilibrium and increased mortality and morbidity associated with diabetes[29]. Depression is often linked to discouragement and increases the risk of non-adherence[30]. Frequent psychological stress in these migrant populations is particularly related to the lack of a residence permit for them and their families, and they often renounce healthcare either for fear of encountering the police, or because access to care is complicated for them. This renouncing of healthcare was described in the study "Health Barometer 2014[31]", which was a telephone survey of more than 2000 people (excluding the poor, living in slums and without a phone), and highlighted that 12% of the surveyed population was giving up care because of access difficulties[32].
THERAPEUTIC MANAGEMENT IN THE FRENCH AMAZON
Complications of diabetes are more common in French Guiana. The REIN registry shows that almost 40% of dialysis patients in French Guiana are diabetic[33].
Data from the INDIA study show excess ischemic stroke mortality in the most vulnerable patients[34].
A balanced diet is one of the essential factors of glycemic balance. Nonetheless, in the same way as in therapeutic education, a low social level is an increased risk for non-compliance with hygiene and dietary measures and poor eating habits[33].
The shortage of specialists is one of the major problems in the care of diabetics, especially in Western French Guiana and in the most remote areas. When patients have a severe glycemic imbalance leading to acute complications, ketoacidosis or hyperosmolar coma, they are transported from the remote health centers by helicopter to the endocrinology department after a stay in the emergency department of Cayenne Hospital, or according to their residence location, at the multipurpose medical service of the Western Guiana Hospital. Unfortunately, after the acute phase, the imple-mentation of appropriate treatment such as insulin therapy for major insulinopenia or significant imbalance in HbA1c greater than 11% is often not possible. Indeed, insulin requires adherence and understanding the disease, except that, as reported in the previous chapter, therapeutic education is often poorly adapted to these people who, upon returning to their village, experience difficulties while using insulin pens or, if they cannot read, to adapt the right doses; it is important to take the cultural aspects into account because, based on the populations and their feelings about the chronic pathology, treatment adherence will be completely different[35]. Assistance by a home-based nurse when the patient returns home is often implemented when patients live in urban areas with access to the city's infrastructure, which is not the case for patients living in remote villages or those who do not have health insurance because they are in an irregular situation in the territory. The second pitfall is related to precarious housing without water or electricity, making it difficult to preserve insulin, and while we are a French territory, we are sometimes faced with the same problems as developing countries; thus, in certain areas insulin preservation is a challenge[36]. In isolated municipalities, treatments may not be delivered on a regular basis due to the absence of pharmacies. Thus, it is not uncommon to prescribe oral anti-diabetic medicine alone, far from national standards, to limit the risk of immediate recurrence of acute complications of hyperglycemia. In the case of patients who have received education about self-management, the handling and adaptation of insulin therapy, mixed basal bolus regimens are sometimes introduced, but then the risk of hypoglycemia is real because the patient is still in an isolated sector and very often their family has not received training on the detection of signs of hyper- or hypoglycemia, and the required actions.
The case of gestational diabetes again raises the question of the feasibility of applying French and European standard recommendations in the French Amazon[37,38]. Indeed, the territory has a very high birth rate of 26.2‰; more than 7200 babies were born in French Guiana in 2016 (including almost 5000 at Cayenne Hospital, the only level 3 maternity unit allowing the management of high-risk pregnancy as is the case of pregnancies in diabetic patients or gestational diabetes)[39,40]. Approximately 8% to 10% of gestational diabetes is reported according to data from a study conducted between 2018 and 2019 at the maternity section of the Cayenne Hospital, not yet published (6% in 2013, data from the perinatal network in French Guiana), probably corresponding to the increase in the prevalence of obesity in our territory. In the past, Bushinenges and Amerindians lived on crops and hunting; unfortunately, traditional activities gave way to a sedentary lifestyle and the westernization of these populations, responsible for an increase in the overweight population and gestational diabetes. On the other hand, since 2015 the peri-natal network of French Guiana decided to carry out (contrary to the national recommendations[41]) a systematic screening of all pregnant women with gestational diabetes with an oral glucose tolerance test administered with 75 g of glucose.
Faced with the increase in the prevalence of gestational diabetes, the difficulties of understanding the disease and its treatment, in 2006 the gynecology and obstetrical teams of the Western Guiana Hospital decided to introduce oral anti-diabetic medicine in the management of gestational diabetes, after observing several accidents due to the misuse of insulin, and the impossibility of having a nurse carry out follow-ups due to remoteness. It is indeed easier for a patient not knowing how to read or write to understand how they will take tablets compared to self-injection of insulin and dose adaptation.
The rationale that has reinforced this choice is the use of oral anti-diabetic medicine in other countries during pregnancy, especially in English-speaking countries where this choice has shown its safety for the fetus due to the absence of placental glyburide, and an insulin-like efficacy for normalizing blood glucose levels and a reduction in macrosomia compared with placebo and shown in the Nachum study[42]. The study by Song et al[43] also showed that there is no difference in efficacy between glyburide and insulin use, but a higher rate of hypoglycemia was observed in the sulfonylurea group[43].
A study conducted at the Western French Guiana Hospital demonstrated a normalization of the glycemic cycle with the use of glibenclamide (DAONIL®) alone or associated with metformin in 80% of gestational diabetes cases and some cases of type 2 diabetes[44]. Thus, in the case of an insufficient single drug regimen, often difficult to follow for our patients due to their precariousness, glibenclamide is used in progressive doses up to 20 mg/d. In the case of insufficient results, it is possible to add a treatment with metformin and, if necessary, insulin may be added to or substitute oral treatment. The teams on site confirmed that the patients exhibited good compliance with the oral treatment compared with the insulin treatment. When insulin treatment is necessary and possible, pumps may only be offered to a small number of our patients, mainly because of sometimes irregular follow-ups and difficulties in patient education. We also very often note the absence of a fundus examination (related to the significant shortage of ophthalmologists) in the two to three years preceding pregnancy for type 2 or type 1 diabetes, which makes insulin optimization difficult in early pregnancy. In fact, diabetic retinopathy can worsen during pregnancy and with rapid improvement in glycemic control[45]. In approximately 600 diabetic pregnancies and cases of gestational diabetes, only 2% to 3% of patients will benefit from an insulin pump. The development of tele-medicine and remote monitoring of blood glucose levels in patients with gestational diabetes is also under development in our territory; nonetheless, the language, the need to have a smartphone and to know how to read and write limits once more the follow-up of the most precarious patients. A recently published study shows that even if computers and internet access is provided to the poorest women, the difficulties of using these new technologies persist, and there is no difference in their overall glycemic balance but a better psycho-social satisfaction with diabetes management[46].
SCREENING PROGRAMS: THE EXAMPLE OF DIABSAT-FRENCH GUIANA
Faced with the health risk, a diabetes screening program and its complications under the management of the endocrinology department of the Cayenne Hospital and the multipurpose medical service of Saint Laurent, subsidized by the General Healthcare Department, the National Center for Space Studies and the Regional Health Agency was set up in the first quarter of 2017.
The DIABSAT-French Guiana program started at the end of 2016, inspired by that of the Midi-Pyrénées region[47], and it allows for the implementation of diagnostic tools and training of healthcare staff for the care of the most isolated diabetic patients in the territory. Thus, three REMOTE HEALTH CENTERS (St Georges, Maripasoula and Grand Santi) were equipped with a retinograph, pedometer platform, measurement of the Systolic Pressure Index and remote biological monitoring (HbA1c and micro-albuminuria). A team consisting of a therapeutic education nurse, a chiropodist, an orthoptist for retinographs, and a doctor carries out one visit per center per month. The main difficulties are the lack of regularity of the visits due to a lack of staff, and the high turnover of the staff of the centers making it difficult to train them to use the equipment installed. On the other hand, the lack of an ophthalmologist limits the number of retinographs that may be read, and they are uninterpretable in the case of some patients who have never had a fundus examination. Remote biological monitoring is also difficult due to the different organizational and financial issues involved.
It is necessary to have a good knowledge of the prevalence of diabetes and its complications, ethnic differences, the different types of diabetes and the healthcare obstacles, in order to adapt interventions to French Guiana to the regional and national authorities. Thus, we started a database, the Codiam (Amazon Diabetes Database), corresponding to a collection of data of diabetics monitored in remote prevention and care centers, Cayenne Hospital and Western French Guiana Hospital. The goal is to include at least 2000 diabetic patients and it will answer many of our questions.
CONCLUSION
The difficulties in access to healthcare related to the extent of the territory and the Amazon rainforest, the lack of road infrastructure and the cultural and linguistic diversity make French Guiana an extraordinary territory. This may be obvious given the precariousness of non-Francophone migrant populations for the most part, but there are also the ethnic and social differences of the native populations located in isolated municipalities; therefore, the therapeutic and educational management of diabetic patients in the French Amazon cannot be in line with French or European recommendations. It is necessary that French public authorities and learned societies become aware of the difficulties and peculiarities of this French territory located in the middle of the Amazon in order to set up more adapted and coherent healthcare organization.
ACKNOWLEDGEMENTS
We thank Dr. Brousse Paul for his help with data and pictures.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: Société Française de Diabetologie.
Specialty type: Endocrinology and metabolism
Country/Territory of origin: French Guiana
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rohani B S-Editor: Fan JR L-Editor: Webster JR P-Editor: Ma YJ