©The Author(s) 2015.
World J Diabetes. Mar 15, 2015; 6(2): 321-325
Published online Mar 15, 2015. doi: 10.4239/wjd.v6.i2.321
Published online Mar 15, 2015. doi: 10.4239/wjd.v6.i2.321
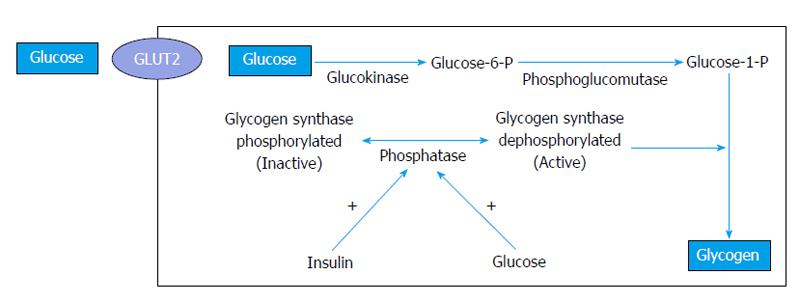
Figure 1 Pathogenesis of hepatic glycogenosis.
Glucose from the blood enters hepatocytes by facilitated diffusion independent of insulin and is converted into glycogen via glucose-6-phosphate. Glycogen synthesis depends on insulin and glucose (modified from Munns et al[12]). GLUT2: Glucose transporter 2.
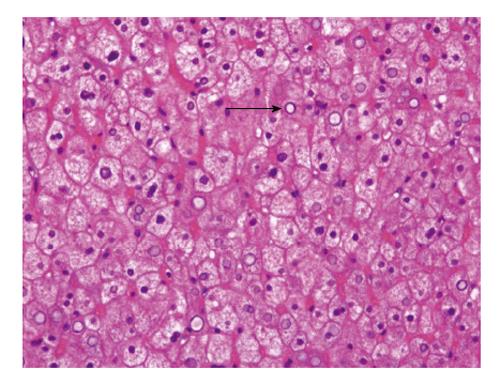
Figure 2 Liver biopsy, haematoxylin and eosin staining.
The hepatocytes are swollen with pale cytoplasm and accentuation of the cell membranes. Sinusoids appear compressed by the swollen hepatocytes. Glycogen nuclei are present (black arrow).
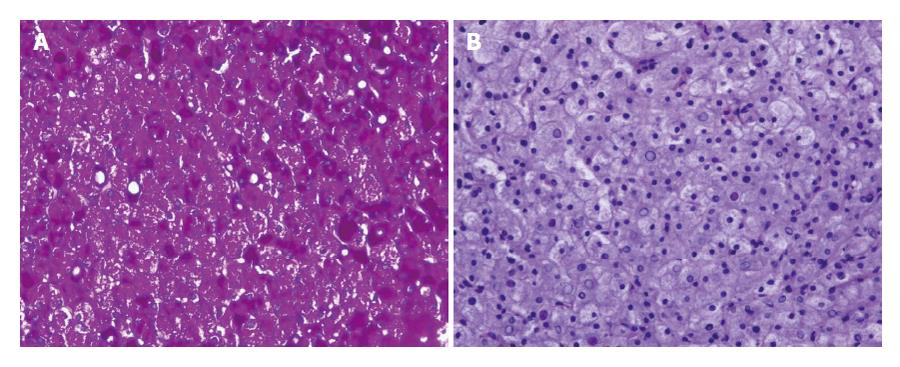
Figure 3 Liver biopsy, periodic acid-Schiff staining.
A: Periodic acid-Schiff (PAS) demonstrates abundant cytoplasmic deposits. An intense reaction is also found in the nucleus; B: The hepatocyte cytoplasm is not stained with PAS after diastase treatment confirming the present of glycogen.
- Citation: Julián MT, Alonso N, Ojanguren I, Pizarro E, Ballestar E, Puig-Domingo M. Hepatic glycogenosis: An underdiagnosed complication of diabetes mellitus? World J Diabetes 2015; 6(2): 321-325
- URL: https://www.wjgnet.com/1948-9358/full/v6/i2/321.htm
- DOI: https://dx.doi.org/10.4239/wjd.v6.i2.321