Published online Feb 15, 2014. doi: 10.4251/wjgo.v6.i2.52
Revised: December 22, 2013
Accepted: January 6, 2014
Published online: February 15, 2014
Processing time: 123 Days and 20.5 Hours
We report on a patient who remained cancer-free for an extended time after palliative radiotherapy (RT) and chemotherapy (nedaplatin plus 5-fluorouracil) treatment for stage IV (cT3N3M1) esophageal squamous cell carcinoma. Although multiple lymph nodes outside the RT field recurred, the local primary tumor within the RT field did not recur, even 17 mo after palliative RT of 30 Gy in 10 fractions. In this case, acute toxicity, such as myelosuppression or esophagitis, was not enhanced by increasing the fraction dose from 1.8-2.0 Gy to 3.0 Gy. Because 30 Gy in 10 fractions can be completed within a shorter time and is less expensive than 50.4 Gy in 28 fractions, we think that 30 Gy without oblique beams is a more favorable RT method for patients.
Core tip: The palliative therapy method has not been confirmed for metastatic esophageal cancer. This case report represents a patient who was cancer-free for an extended period of time after palliative chemoradiation of 30 Gy in 10 fractions. We think that 30 Gy without oblique beams is a more favorable radiotherapy method for patients.
- Citation: Yamashita H, Okuma K, Nomoto A, Yamashita M, Igaki H, Nakagawa K. Extended cancer-free survival after palliative chemoradiation for metastatic esophageal cancer. World J Gastrointest Oncol 2014; 6(2): 52-54
- URL: https://www.wjgnet.com/1948-5204/full/v6/i2/52.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v6.i2.52
Esophageal cancer, which has the highest incidence and mortality worldwide, is one of the most common malignant tumors in Japan. Japan is recognized as having one of the highest incidence rates of esophageal squamous cell carcinoma in the world.
Due to a lack of obvious early symptoms, patients are often diagnosed at advanced stages, and more than half of patients present with metastases[1]. The recurrence and metastasis rates of esophageal cancer after treatment have tended to increase in recent years. In 2007, Grünberger et al[2] confirmed that palliative chemotherapy can prolong the survival of stage IV esophageal cancer patients, relieve their symptoms and improve their quality of life. Esophageal squamous cell carcinoma is the most common histology in Japan, and its constituent ratio is different from that in Europe and America.
Most patients with esophageal cancer present with dysphagia, and more than half of the patients have inoperable disease at the time of presentation[3,4]. The primary aim of treatment in these patients is to relieve the dysphagia with minimal morbidity and mortality and thus improve their quality of life.
We present a case of extended cancer-free survival after palliative radiotherapy (RT) and chemotherapy in a stage IV esophageal squamous cell carcinoma patient.
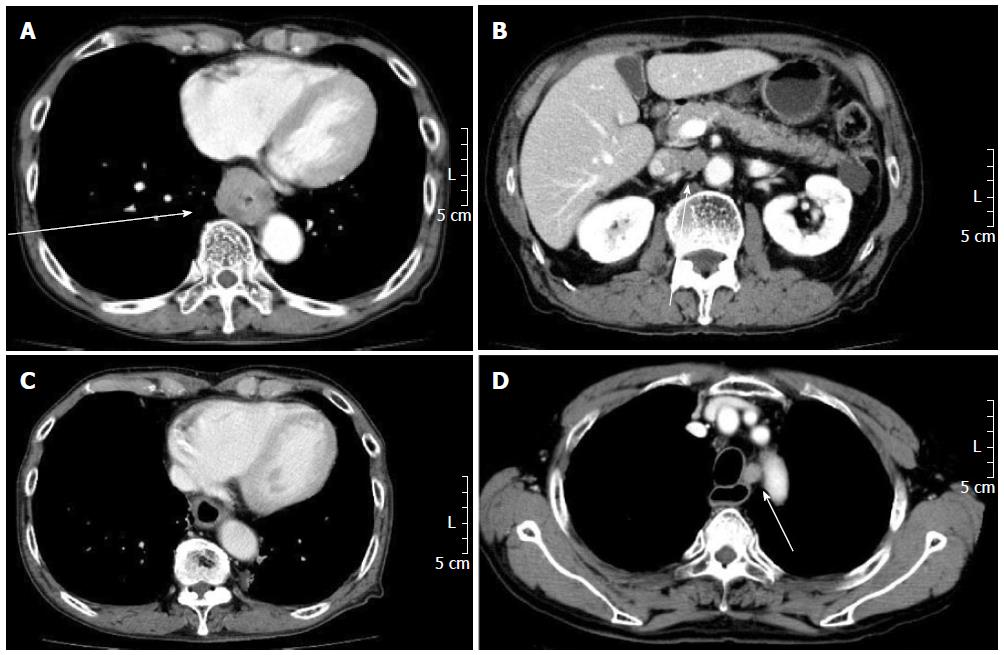
A 76-year-old Japanese man was referred to our hospital after a few months of dysphagia due to esophageal stenosis. A chest X-ray did not show any characteristic malignancy. A gastrofiberscopy and computed tomography (CT) scan showed a circumferential wall thickening and a 39 mm × 35 mm tumor on the lower thoracic esophagus (Figure 1A). A biopsy on December 13, 2011, revealed squamous cell carcinoma. Laboratory findings, including staining for tumor markers, such as p53, and squamous cell carcinoma, were all within the normal ranges, except for the cytokeratin 19 fragments (CYFRA), which were elevated at 4.3 ng/mL (normal 0-2.0 ng/mL, IRMA method). A chest/abdominal CT scan with enhancement on December 5, 2011, revealed multiple lymph node metastases, including the left supraclavicular, tracheal bifurcation, gastric cardia, and abdominal para-aortic lymph nodes (Figure 1B) (cT3N3 M1, c-Stage IV).
It was decided that our patient should undergo chemoradiation therapy (CRT). The patient received 30 Gy in 10 fractions of 3 Gy on the original tumor location using a 2-field technique of external beam irradiation from December 21, 2011, to January 10, 2012. The patient also received nedaplatin chemotherapy at a dose of 80 mg/m2 (day 1) plus 5-fluorouracil at 800 mg/m2 per day (days 1-4) starting on December 26, 2011.
A plain chest/abdominal CT scan on January 23, 2012, after a single cycle of chemotherapy, revealed a remarkable shrinkage of the mass in the lower esophagus and in all lymph nodes (Figure 1C). An enhanced chest/abdominal/pelvic CT scan on April 17, 2012 (after 4 cycles), August 20, 2012 (after 7 cycles), and October 16, 2012, revealed that the tumors continued to shrink. After 6 cycles of chemotherapy, the CYFRA levels had decreased to normal by June 15, 2012. One additional cycle of chemotherapy was added on July 17, 2012. After CRT, the patient had regular follow-up appointments every 3-4 mo.
After 8 completely asymptomatic months following chemotherapy and 14 mo after palliative RT, the tumor was found to have recurred during a regular follow-up appointment. A chest and abdominal enhanced CT scan on March 12, 2013, revealed that the metastatic tumor had spread to multiple lymph nodes, including the retro-esophageal, left para-tracheal (Figure 1D), supraclavicular, and bilateral hilum lymph nodes, but local recurrence was not observed. According to a cervical/chest/abdominal enhanced CT scan that was performed on June 11, 2013 (17 mo after palliative RT), local disease remained controlled.
More than 50% of patients with esophageal cancer are not amenable to surgical excision at the time of diagnosis, because of either advanced disease or the presence of comorbid conditions. For such patients, palliation of the symptoms is the mainstay of treatment[4].
According to the Radiation Therapy Oncology Group 94-05 trial[5], the standard radiation dose for patients with clinical stage T1 to T4, N0/1, M0 esophageal carcinoma that are selected for a nonsurgical approach and concurrent treatment with 5-FU and cisplatin chemotherapy is 50.4 Gy. Additionally, at our institution, 50.4 Gy in 28 fractions is selected as a curative method. In this case, 30 Gy in 10 fractions was selected as a palliative irradiation dose. Although multiple lymph nodes outside the RT field recurred, the local primary tumor within the RT field did not recur, even 17 mo after RT. In this case, acute toxicity, such as myelosuppression or esophagitis, was not enhanced by increasing the fraction dose from 1.8-2.0 Gy to 3.0 Gy. Because 30 Gy in 10 fractions was completed within a shorter time and was less expensive than 50.4 Gy in 28 fractions, we think that 30 Gy without oblique beam is a more favorable RT method for patients. Because control of the primary lesion of esophageal cancer is directly connected to the inability of the patient to ingest and the subsequent QOL deterioration, a total radiation dose of as much as 30 Gy, not 25 or 20 Gy, was used with palliative intent in our institution.
According to Matsumoto et al[5], docetaxel and nedaplatin combination chemotherapy with and without radiation therapy is well tolerated (2-year overall survival was 11.1%) and useful as a second-line chemotherapy for patients with relapsed or metastatic esophageal cancer.
A 76-year-old male was referred to our hospital with a few month history of dysphagia due to esophageal stenosis.
A gastrofiberscopy and computed tomography scan showed a circumferential wall thickening and a 39 mm × 35 mm tumor on the lower thoracic esophagus.
Esophageal leiomyoma, polyp, hemangioma, papilloma, lipoma, cyst.
Laboratory findings, including tumor markers like p53 and squamous cell carcinoma, were all within normal values, except for cytokeratin 19 fragments, which was raised at 4.3 ng/mL (normal 0-2.0 ng/mL, IRMA method).
A chest/abdominal computed tomography scan revealed multiple lymph node metastases such as left supraclavicular, tracheal bifurcation, gastric cardia, and abdominal para-aortic lymph node (cT3N3M1, c-Stage IV).
A biopsy revealed a squamous cell carcinoma.
The patient was treated with 30 Gy in 10 fractions of external beam irradiation and chemotherapy of nedaplatin plus 5-fluorouracil.
According to Matsumoto H, docetaxel and nedaplatin combination chemotherapy with and without radiation therapy is well tolerated and useful (2-year overall survival was 11.1%) as second-line chemotherapy for patients with relapsed or metastatic esophageal cancer.
The authors think that 30 Gy without oblique beams is a more favorable palliative radiotherapy method for patients with metastatic esophageal cancer.
This article applies a rare case who survived long time after palliative chemoradiation.
| 1. | Ishihara R, Tanaka H, Iishi H, Takeuchi Y, Higashino K, Uedo N, Tatsuta M, Yano M, Ishiguro S. Long-term outcome of esophageal mucosal squamous cell carcinoma without lymphovascular involvement after endoscopic resection. Cancer. 2008;112:2166-2172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 69] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 2. | Grünberger B, Raderer M, Schmidinger M, Hejna M. Palliative chemotherapy for recurrent and metastatic esophageal cancer. Anticancer Res. 2007;27:2705-2714. [PubMed] |
| 3. | Farrow DC, Vaughan TL. Determinants of survival following the diagnosis of esophageal adenocarcinoma (United States). Cancer Causes Control. 1996;7:322-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 84] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2651] [Cited by in RCA: 2604] [Article Influence: 104.2] [Reference Citation Analysis (1)] |
| 5. | Matsumoto H, Hirabayashi Y, Kubota H, Murakami H, Higashida M, Haruma K, Hiratsuka J, Nakamura M, Hirai T. A combined therapy with docetaxel and nedaplatin for relapsed and metastatic esophageal carcinoma. Anticancer Res. 2012;32:1827-1831. [PubMed] |
P- Reviewers: Chai J, Hsiao KCW S- Editor: Cui XM L- Editor: A E- Editor: Wang CH