Published online Dec 15, 2014. doi: 10.4251/wjgo.v6.i12.450
Revised: November 5, 2014
Accepted: November 17, 2014
Published online: December 15, 2014
Processing time: 168 Days and 3.7 Hours
While solid tumors are less commonly associated with meningeal involvement; lung, breast and melanoma are the ones most often reported. A few case reports have included gastric carcinoma but these are rare and most often associated with systemic disease at the time of diagnosis. Here we report a unique presentation of gastric carcinoma relapse with leptomeningeal carcinomatosis. An 81-year-old female was diagnosed with gastric cancer approximately one year before presentation. Following neoadjuvant chemotherapy, she had gastrectomy. Her periodic surveillance was stable. Thereafter she presented with a one week history of progressive fatigue lightheadedness, syncope. During hospitalization her mental status deteriorated. A repeat computed axial tomography scan of the head showed no changes to suggest an etiology. A lumbar puncture was performed and cerebral spinal fluid (CSF) cytopathology confirmed gastric signet cell adenocarcinoma. Encephalopathy was likely caused by increased intracranial pressure from communicating hydrocephalus. Leptomeningeal carcinomatosis is associated with short life expectancy. Therapeutic lumbar punctures and best supportive care or systemic therapy can be applied with guarded prognosis. Survival, however, may improve with cytologic negative conversion of the CSF if patient performance status allows treatment.
Core tip: Solid tumors rarely have leptomeningeal carcinomatosis. Gastric adenocarcinoma have been rarely reported with leptomeningeal involvement, and most of the reports have been documented in patients with Asian heritage, who have higher incidence of gastric adenocarcinoma. This leptomeningeal involvement is usually a late complication of disseminated and relapsed disease. In this case, however, we describe a patient with recurrence of gastric adenocarcinoma that presented with leptomenigeal carcinomatosis. We describe the presentation, the pertinent medical history of the patient, and the clinical outcome of the disease. We highlighted that leptomeningeal carcinomatosis can be a presentation of relapse, which is rare, and indicates a poor prognosis.
- Citation: Saad N, Alsibai A, Hadid TH. Carcinomatous meningitis due to gastric adenocarcinoma: A rare presentation of relapse. World J Gastrointest Oncol 2014; 6(12): 450-453
- URL: https://www.wjgnet.com/1948-5204/full/v6/i12/450.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v6.i12.450
Leptomeningeal carcinomatosis (LMC) is defined as the infiltration of the pia mater and the arachnoid membrane by malignant cells. LMC can be limited to the meninges but can also occur in association with paranchymal invasion of the central nervous system (CNS) with or without dissemination into the ventricles. LMC is an underestimated complication of malignancy. It is estimated to occur in 5%-8% of cancer patients[1]. However, the clinical diagnosis of LMC has been identified in 2%-4% of the patients who found to have LMD on autopsy[2].
The incidence of LMC varies by the primary site of malignancy. LMC occurs in 78% of hematologic malignancies if prophylactic treatment is not administered. It is less common in solid tumors, of which lung cancer (9%-25%), breast cancer (2%-5%), and melanoma (up to 23%) are the most common[3,4].
Gastric cancer complicated by LMC is very rare. It is estimated to occur in 0.16% of all cases of gastric cancer[5], of which 87% have disseminated disease[6]. We present a case of recurrence of gastric cancer manifested by LMC on presentation.
An 81-year-old woman was diagnosed with signet cell adenocarcinoma. Staging Positron emission tomography/computed tomography (CT) scan showed increased fluoro-D-glucose activity in the stomach and regional lymph nodes without distant metastasis. She was treated with neoadjuvant chemotherapy using Epirubicin, Oxaliplatin and Capecitabine for 6 cycles. This was followed by total gastrectomy with Roux-en-Y esophagojejunostomy. Pathologic staging showed pT2, N0 with negative margins and 23 negative lymph nodes. She received no adjuvant therapy, and active surveillance was initiated.
One year later, she presented with a one week history of progressive lightheadedness, rigors, generalized fatigue and an episode of syncope. Her review of systems was notable for drenching night sweats for about 3 mo.
On examination, she was afebrile, weak, alert and oriented to herself. Examination of the cranial nerves was normal, sensory and motor examination were normal without ataxia or nuchal rigidity.
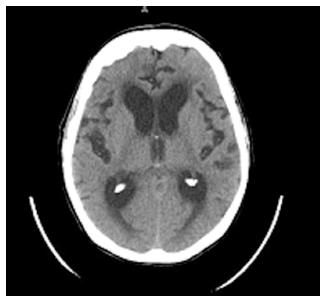
CT scan of the brain showed low attenuation changes of the left cerebellar hemisphere, likely sequela of remote vascular insult. There was prominence of the ventricular system, slightly out of proportion to the sulcal prominence which raised the possibility of normal pressure hydrocephalus (Figure 1).
Ten days prior to admission, a surveillance CT scan of the abdomen and the pelvis showed small amount of fluid within the abdomen and the pelvis, and nodules on the gastrectomy bed and the omentum which were stable compared with previous CT scan.
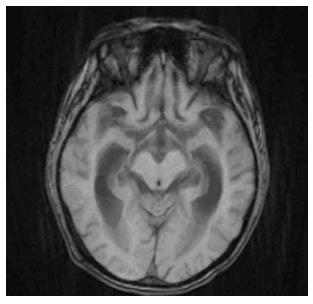
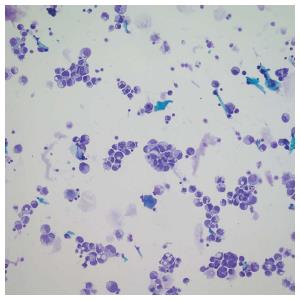
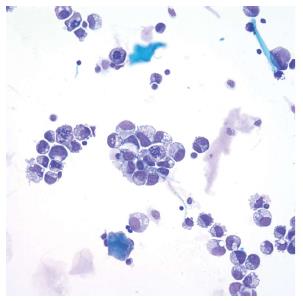
During the course of her hospital stay the patient was found to have pyuria and atrial fibrillation with rapid ventricular response. Rate control was instituted and she received empiric antibiotic therapy for urinary tract infection. Her blood cultures were negative and her urine cultures grew enterococci. While on therapy, she had progressive deterioration of her mental status and became non-verbal and unarousable. An enhanced magnetic resonance imaging of the brain with contrast showed no evidence of leptomeningeal enhancement (Figure 2). Electroencephalogram, vitamin B12, thyroxin stimulation hormone, folic acid and ammonia level were unrevealing. A diagnostic lumber puncture was performed revealing an opening pressure of 38 cm water. Cerebrospinal fluid (CSF) analysis showed WBC of 31 with 55% lymphocytes, 1% polymorphonuclear white cells, 36% atypical cells, protein of 120 mg/dL, and glucose of 85 mg/dL. Cytologic examination confirmed CSF involvement with adenocarcinoma with signet cell features (Figures 3 and 4). CSF microbiologic workup was negative. Best supportive care and therapeutic lumber punctures were applied to relieve the communicating hydrocephalus. The patient, however, continued to deteriorate and died shortly thereafter. Autopsy was refused by the family and there decision was respected.
In our case, we present a patient with signet cell gastric adenocarcinoma. This histologic subtype is the most among solid tumors to be complicated with LMC[7]. Among patients diagnosed with LMC in solid tumors, the most common encountered solid tumors are breast, lung, and melanoma[8]. However, In east Asian countries LMC due to gastric carcinoma is more common compared to other places due to higher incidence of this malignancy in that region[9]. Many cases of LMC have been reported in the contest of gastric cancer in advanced stage and poorly differentiated or signet-ring cell histology[10]. Although our patient did not have clinical or histological systemic dissemination at the time of leptomeningeal relapse, she had increased intraperitoneal fluid and nodularity at the gastrectomy bed and the omentum, which may reflect local recurrent disease which was interpreted as stable and left for monitoring. Our case is unique in that the patient presented with altered mental status secondary to LMC as the principle and first manifestation of Signet Cell Gastric Adenocarcinoma recurrence.
The increase in survival of patients with signet cell gastric adenocarcinoma with the discovery of newer therapeutic agents, and the poor penetration of these drugs into the CNS has led to an increase in the number of cases of LMC associated with gastric adenocarcinoma[11-13]. Prognosis of LMC is guarded, particularly in solid tumors. Treatment options are limited, including intrathecal therapy, systemic therapy and best supportive care.
Overall survival in cases of LMC is very short with median overall survival of 4-5 wk without treatment and 2-4 mo with treatment[7,14,15]. Our patient survived less than 2 wk from the time of diagnosis. One study noted that clearance of the CSF with intrathecal (IT) chemotherapy is independently associated with longer survival[6].
Radiotherapy has been tried for treatment; its role, however, remains controversial[16]. Systemic chemotherapy usually is given after IT chemotherapy in patients with good performance status. Due to the poor performance status of our patient, best supportive care was deemed appropriate.
We conclude that, despite LMC being a rare manifestation of recurrent gastric cancer, it should be considered in the differential diagnosis of a patient presenting with encephalopathy with prior history of gastric cancer. LMC may be the first sign of relapse in stomach cancer. LMC in the context of gastric cancer has poor prognosis[2]. Therapeutic options should be individualized based on the performance status of the affected patient. Further studies are needed to determine the risk factors for LMC in the contest of gastric cancer and to formulate an early diagnosis and more effective treatment.
An 81-year-old female with a history of gastric adenocarcinoma in remission, presented with a one week history of progressive fatigue, lightheadedness and syncope.
Encephalopathy.
Meningitis, encephalitis, metabolic encephalopathy, hydrocephalus.
Complete blood count, comprehensive metabolic panel, vitamin B12, thyroxin stimulation hormone, folic acid and ammonia level were normal.
Computed tomography scan of the brain showed prominence of the ventricular system, slightly out of proportion to the sulcal prominence, which raised the possibility of normal pressure hydrocephalus while enhanced magnetic resonance imaging of the brain with contrast showed no evidence of leptomeningeal enhancement.
Cerebral spinal fluid analysis showed atypical cells which were identified as adenocarcinomatous cells with signet cell features.
Best supportive care and therapeutic lumber punctures to relieve the communicating hydrocephalus were applied.
There are many case reports of leptomeningeal carcinomatosis in the contest of gastric adenomarcima, However this case was unique because the relapse of adenocarcinoma was manifested by acute encephalopathy.
Leptomeningeal carcinomatosis (LMC) is infiltration of the pia mater and the arachnoid membrane by malignant cells
LMC can be the first sign of relapse of gastric adenocarcinoma. LMC in the context of gastric cancer has poor prognosis
This is an interesting case report.
| 1. | Grossman SA, Krabak MJ. Leptomeningeal carcinomatosis. Cancer Treat Rev. 1999;25:103-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 385] [Cited by in RCA: 396] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 2. | Pentheroudakis G, Pavlidis N. Management of leptomeningeal malignancy. Expert Opin Pharmacother. 2005;6:1115-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Martins SJ, Azevedo CR, Chinen LT, Cruz MR, Peterlevitz MA, Gimenes DL. Meningeal carcinomatosis in solid tumors. Arq Neuropsiquiatr. 2011;69:973-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Slimane K, Andre F, Delaloge S, Dunant A, Perez A, Grenier J, Massard C, Spielmann M. Risk factors for brain relapse in patients with metastatic breast cancer. Ann Oncol. 2004;15:1640-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 125] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Kim M. Intracranial involvement by metastatic advanced gastric carcinoma. J Neurooncol. 1999;43:59-62. [PubMed] |
| 6. | Oh SY, Lee SJ, Lee J, Lee S, Kim SH, Kwon HC, Lee GW, Kang JH, Hwang IG, Jang JS. Gastric leptomeningeal carcinomatosis: multi-center retrospective analysis of 54 cases. World J Gastroenterol. 2009;15:5086-5090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Bruno MK, Raizer J. Leptomeningeal metastases from solid tumors (meningeal carcinomatosis). Cancer Treat Res. 2005;125:31-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 1982;49:759-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Lee JL, Kang YK, Kim TW, Chang HM, Lee GW, Ryu MH, Kim E, Oh SJ, Lee JH, Kim SB. Leptomeningeal carcinomatosis in gastric cancer. J Neurooncol. 2004;66:167-174. [PubMed] |
| 11. | Kosmas C, Malamos NA, Tsavaris NB, Stamataki M, Gregoriou A, Rokana S, Vartholomeou M, Antonopoulos MJ. Isolated leptomeningeal carcinomatosis (carcinomatous meningitis) after taxane-induced major remission in patients with advanced breast cancer. Oncology. 2002;63:6-15. [PubMed] |
| 12. | Bendell JC, Domchek SM, Burstein HJ, Harris L, Younger J, Kuter I, Bunnell C, Rue M, Gelman R, Winer E. Central nervous system metastases in women who receive trastuzumab-based therapy for metastatic breast carcinoma. Cancer. 2003;97:2972-2977. [PubMed] |
| 13. | Lin C, Turner S, Gurney H, Peduto A. Increased detections of leptomeningeal presentations in men with hormone refractory prostate cancer: an effect of improved systemic therapy? J Med Imaging Radiat Oncol. 2008;52:376-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | DeAngelis LM, Boutros D. Leptomeningeal metastasis. Cancer Invest. 2005;23:145-154. [PubMed] |
| 15. | Chowdhary S, Chamberlain M. Leptomeningeal metastases: current concepts and management guidelines. J Natl Compr Canc Netw. 2005;3:693-703. [PubMed] |
| 16. | Mehta M, Bradley K. Radiation therapy for leptomeningeal cancer, in Leptomeningeal Metastases. US: Springer 2005; 147-158. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
P- Reviewer: Mavrogiannaki AN, Mura B S- Editor: Ji FF L- Editor: A E- Editor: Wu HL