Published online Dec 15, 2023. doi: 10.4251/wjgo.v15.i12.2101
Peer-review started: September 21, 2023
First decision: October 9, 2023
Revised: October 26, 2023
Accepted: November 25, 2023
Article in press: November 25, 2023
Published online: December 15, 2023
Processing time: 83 Days and 19.6 Hours
Transversus abdominis plane block (TAPB) is a block of the abdominal afferent nerve fibers between the internal oblique muscle and the transverse abdominal muscle achieved with local anesthetics. It can effectively block the conduction of the anterior nerve of the abdominal wall and exert a good analgesic effect. However, the effect of combining the block with remimazolam on anesthesia in patients undergoing gastrointestinal tumor surgery is still unclear.
To examine the effects of combining TAPB with remimazolam on the stress response and postoperative recovery of gastrointestinal tumor surgery patients.
A retrospective analysis was conducted on the clinical data of 102 individuals diagnosed with gastrointestinal malignancies who underwent laparoscopic surgery under general anesthesia between April 2020 and June 2023. The patients were categorized into a control group (n = 51), receiving remimazolam for general anesthesia, and an observation group (n = 51), receiving TAPB combined with remimazolam for general anesthesia. A comparison was made between both groups in terms of hemodynamic parameters, stress markers, pain levels, recovery quality, analgesic effects, and adverse reactions during the perioperative period.
The observation group had significantly higher heart rates at time points 1 min after induction and upon leaving the operating room than the control group (P < 0.05). The mean arterial pressure at time point T1 in the observation group was significantly higher than that in the control group (P < 0.05). Five minutes after extubation, the levels of the hormones adrenaline and noradrenaline in the observation group were considerably lower than those in the control group (P < 0.05). At 12 h, 24 h, and 48 h following surgery, the visual analog scale scores of the observation group were considerably lower than those of the control group (P < 0.05). The observation group had shorter awakening and extubation times and lower Riker sedation-agitation scale scores than the control group (P < 0.05). The observation group exhibited considerably fewer effective pump presses, lower fentanyl dosages, and lower incidences of rescue analgesia within 24 h following surgery than the control group (P < 0.05).
The application effect of TAPB combined with remimazolam general anesthesia in anesthesia of patients undergoing gastrointestinal tumor surgery is good, which is helpful to promote faster recovery after operation.
Core Tip: Stress can lead to severe changes in hemodynamics during surgery and increase the risk of postoperative adverse events. In this study, the application value of transversus abdominis plane block (TAPB) combined with remimazolam general anesthesia in patients undergoing gastrointestinal tumor surgery was observed. The results showed that the application of TAPB combined with remimazolam general anesthesia had the advantages of stable anesthesia induction and small hemodynamic fluctuation, which was helpful to reduce the acute stress response of patients undergoing gastrointestinal tumor surgery and improve the quality of recovery.
- Citation: Liu J, Tian JM, Liu GZ, Sun JN, Gao PF, Zhang YQ, Yue XQ. Application of remimazolam transversus abdominis plane block in gastrointestinal tumor surgery. World J Gastrointest Oncol 2023; 15(12): 2101-2110
- URL: https://www.wjgnet.com/1948-5204/full/v15/i12/2101.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v15.i12.2101
The gastrointestinal tract includes the stomach, duodenum, jejunum, ileum, cecum, colon, and rectum. Gastrointestinal tumors are the most common digestive tract tumors worldwide. Based on statistical data[1], gastric cancer is the second most prominent cause of cancer death in China, following lung cancer. Recently, there has been a notable increase in the occurrence of colorectal cancer, resulting in its inclusion among the five most prevalent forms of cancer. Since most gastrointestinal tumor patients have subtle symptoms in the early stages of the disease and are usually diagnosed at an intermediate or advanced stage, timely surgical intervention is necessary to control disease progression[2] before distant metastasis. Due to its minimal invasiveness, reduced pain, and faster recovery, laparoscopic surgery has been widely used in treating gastrointestinal tumors. However, carbon dioxide (CO2) pneumoperitoneum is established during laparoscopic surgery, increasing intra-abdominal pressure. When the intra-abdominal pressure drops suddenly, it can lead to ischemia-reperfusion injury and a stress response, and the change in surgical position will also affect the body's homeostasis, causing severe postoperative pain and adversely affecting the patient's recovery[3]. Prior research has demonstrated that stress conditions can potentially augment the production and release of cortisol, epinephrine (E), norepinephrine (NE), and blood glucose in individuals. The drastic changes in hemodynamics can increase the risk of adverse events postoperatively, significantly affecting the effectiveness of surgical treatment and postoperative recovery[4]. Therefore, a reasonable anesthesia approach reduces stress responses during laparoscopic surgery and promotes faster postoperative recovery.
Transversus abdominis plane block (TAPB) provides regional anesthesia by effectively blocking the sensory nerve fibers within the abdominal cavity, explicitly targeting the area between the internal oblique and transverse abdominis muscles. It can effectively block the transmission of the anterior abdominal wall nerves, thus providing analgesic effects[5]. The relevant literature has shown that remimazolam can be safely and effectively used in outpatient gastrointestinal endoscopy and bronchoscopy. Its successful sedation rate is similar to that of propofol, but it is significantly safer. It can be used for anesthesia induction and maintenance[6]. There are few reports on the use of TAPB combined with remimazolam in laparoscopic surgery for the treatment of gastrointestinal tumors. The primary objective of this study was to examine the effects of the combination of TAPB and remimazolam for anesthesia on the stress responses and postoperative recovery of individuals undergoing gastrointestinal tumor surgery. The findings of this study can be used to establish a theoretical foundation for the prevention or reduction of stress responses in patients, as well as to provide evidence-based choices for clinical anesthesia.
Study subjects: Medical information from a cohort of 104 patients diagnosed with gastrointestinal malignancies and who underwent laparoscopic surgery under general anesthesia at our institution from April 2021 to June 2023 was retrospectively acquired. The criteria for inclusion are outlined below: Confirmed diagnosis of gastrointestinal tumors; being suitable for laparoscopic surgery; American Society of Anesthesiologists classification II-III; 18-65 years old; and complete medical records. Patients with incomplete case data were excluded. In this study, the clinical data of 104 patients with gastrointestinal tumors who underwent laparoscopic surgery under general anesthesia were reviewed, including 52 patients in the observation group and 52 patients in the control group. In the observation group, 1 patient without gastrointestinal tumors was excluded; in the control group, 1 patient was excluded due to missing intraoperative hemodynamic data. Finally, 51 patients in the observation group and 51 patients in the control group were included in the statistical analysis. All participants submitted informed consent forms, and the study methodology followed the Helsinki Declaration.
Preanesthetic preparation: All patients underwent relevant examinations preoperatively and were advised to fast for 6-8 h before surgery. Upon arrival to the operating room, peripheral intravenous access was established, and routine monitoring of the heart rate (HR), bispectral index (BIS), respiratory rate (RR), oxygen saturation, mean arterial pressure (MAP), and electrocardiography was commenced.
Anesthesia methods: Anesthesia Induction: The following drugs were sequentially administered intravenously for anesthesia induction: Remimazolam (0.2 mg/kg), cisatracurium (0.2-0.4 mg/kg), and sufentanil (0.4-0.6 μg/kg). After the BIS value fell below 60 and appropriate conditions for endotracheal intubation were ascertained, tracheal intubation was executed. Subsequently, the anesthetic device was attached to facilitate controlled respiration. The tidal volume was set at 8-10 mL/kg, the RR at 12-14 breaths per min, and the inspiratory-expiratory ratio at 1:2. During the surgery, respiratory parameters were adjusted to maintain the end-tidal carbon dioxide pressure-CO2 between 30-40 mmHg. In the observation group, bilateral TAPB was performed 5 min after anesthesia induction by the side entry method. A linear ultrasound probe guided the needle into the transversus abdominis plane. The ultrasonic probe was positioned at a right angle to the anterior axillary line, within the space bounded by the iliac crest and the costal edge on one side. The probe was then adjusted until the three distinct muscles of the transverse abdominal muscle group were discernible. When the needle tip reached the plane of the transverse fascia of the abdomen, it was drawn back to confirm that there was no blood or air. Ropivacaine (20 mL of 0.375%) was injected into the fascial sheath between the internal oblique and transverse abdominalis muscles to obtain spindle-shaped hypoechoic images. The same procedure was repeated on the other side to complete the bilateral TAPB. The control group received only remimazolam.
Anesthesia maintenance: Intravenous remimazolam 0.4-1.2 mg/kg/h was administered, while cisatracurium was injected at a rate of 0.1 mg/kg/h. On the other hand, sufentanil 6-12 μg/kg/h was provided intravenously. The dosage of anesthetic drugs was adjusted based on the patient’s BIS, MAP, and HR. The BIS value was maintained between 40-60. Atropine (0.3-0.5 mg) was administered if the patient’s HR dropped below 50 beats per min, and esmolol (0.5 mg/kg) was administered if the HR exceeded 100 beats per min. Drugs were readministered if necessary.
Flurbiprofen (50 mg) was administered for postoperative analgesia during skin closure, and all patients received patient-controlled intravenous analgesia (PCIA) after surgery. The PCIA scheme consisted of sufentanil 100 μg, flurbiprofen 200 mg, and ondansetron hydrochloride 32 mg, mixed in a total volume of 100 mL. The initial infusion rate was set at 2 mL/h, followed by a self-controlled infusion rate of 1.5 mL/h. The maximum self-controlled infusion rate allowed was 8 mL/h, with a lockout period of 20 min. After the surgical procedure, the individuals were sent to the postanesthesia care unit (PACU) for observation and recovery. Tracheal extubation was successfully performed in all patients, and they were then moved back to the ward.
(1) Hemodynamics comparison: MAP and HR were compared at different time points, including upon leaving the operating room (T3), immediately after tracheal intubation (T2), 1 min after induction (T1), and before anesthesia induction (T0); (2) Stress response: Blood samples were obtained from the radial artery of patients at two specific time points: 10 min before the introduction of anesthesia and 5 min following extubation. The concentrations of plasma NE and E were measured using an enzyme-linked immunosorbent assay; (3) Pain intensity: Pain intensity in both groups was evaluated at 4, 12, 24, and 48 h post surgery using the visual analog scale (VAS). The scores ranged from 0 to 10, with higher values denoting greater pain intensity; (4) Recovery quality: Recorded parameters included time to eye-opening, time to extubation, PACU stay duration, and Riker sedation-agitation score assessed at extubation. A Riker score ≥ 5 indicated agitation at extubation; and (5) Safety: The examiners monitored the number of successful activations of the Patient-Controlled Analgesia (PCA) pump, the amount of sufentanil administered, and the frequency of rescue analgesic administrations during the 24 h following the surgical procedure. The occurrence rates of vomiting, nausea, pruritus, and respiratory depression were compared between the two groups within 48 h after surgery.
We used SPSS 22.0 software to analyze the data. The measured information is presented as the mean ± SD, and we compared them using t tests. Count data are expressed as numbers or percentages and were compared using chi-square tests. The chi-square value was corrected if the theoretical frequency was ≤ 5 5 but ≥ 1. Fisher’s exact test was used if the theoretical frequency was < 1. A P value less than 0.05 is indicative of a statistically significant difference.
Between the observation and control groups, there was no statistically significant variation in sex, age, or any other baseline characteristics (P > 0.05, Table 1).
| Group | n | Sex (male/female, cases) | Age (yr, mean ± SD) | BMI (kg/m2, mean ± SD) | Surgical time, (min, mean ± SD) | ASA classification (I/II/III, cases) |
| Observation group | 51 | 33/18 | 49.58 ± 11.29 | 23.64 ± 1.54 | 216.15 ± 29.33 | 9/31/11 |
| Control group | 51 | 30/21 | 49.24 ± 11.58 | 23.28 ± 1.69 | 208.48 ± 31.67 | 12/33/6 |
| t/χ2 | 0.374 | 0.150 | 1.124 | 1.269 | 1.962 | |
| P value | 0.541 | 0.881 | 0.264 | 0.207 | 0.375 |
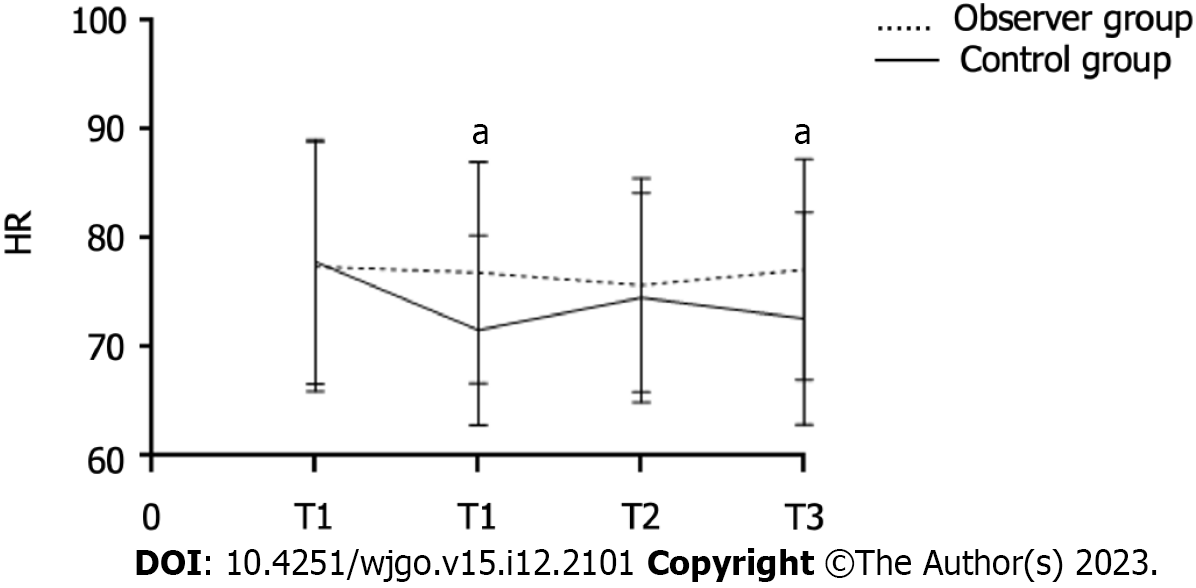
The two groups had no significant differences in HR at the T0 and T2 time points (P > 0.05). Nevertheless, the observation group displayed substantially higher HRs at the T1 and T3 time points than the control group (P > 0.05, Table 2, Figure 1).
| Group | n | T0 | T1 | T2 | T3 |
| Observation group | 51 | 77.37 ± 11.49 | 76.85 ± 10.18 | 75.69 ± 9.84 | 77.12 ± 10.15 |
| Control group | 51 | 77.84 ± 11.25 | 71.54 ± 8.74 | 74.55 ± 9.62 | 72.61 ± 9.78 |
| t/χ2 | 0.209 | 2.826 | 0.592 | 2.285 | |
| P value | 0.835 | 0.006 | 0.555 | 0.024 |
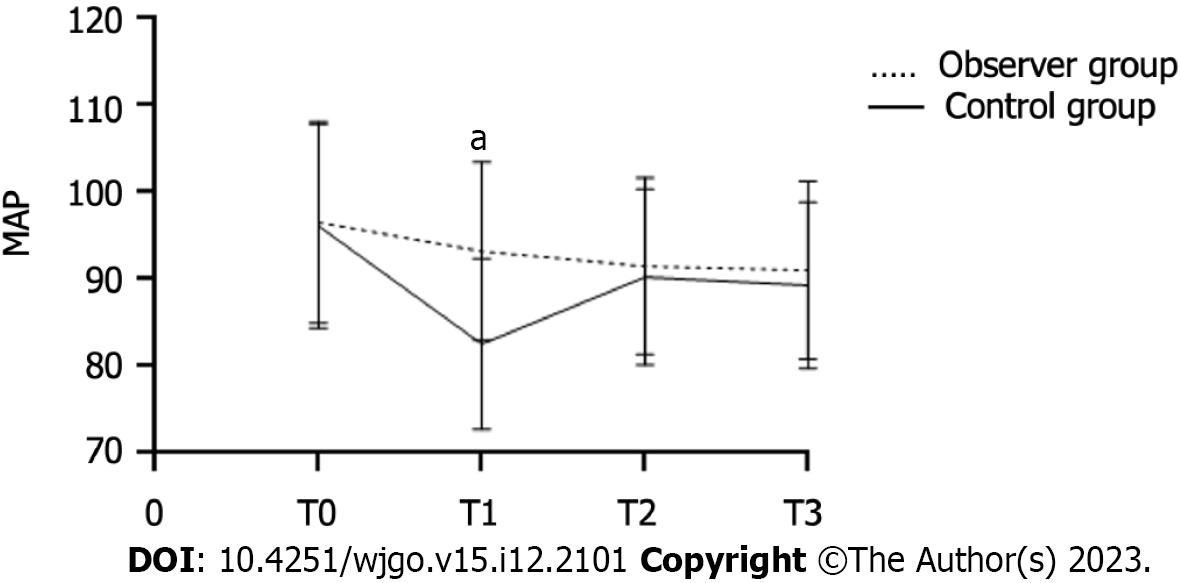
No statistically significant variation was observed in the MAP between the two categories at the T0, T2, and T3 time points (P > 0.05). Nevertheless, the MAP at the T1 time point exhibited a statistically significant elevation in the observation group compared to the control (P < 0.05, Table 3, Figure 2).
| Group | n | T0 | T1 | T2 | T3 |
| Observation group | 51 | 96.54 ± 11.59 | 93.18 ± 10.27 | 91.48 ± 10.18 | 91.02 ± 10.23 |
| Control group | 51 | 96.11 ± 11.74 | 82.54 ± 9.85 | 90.22 ± 10.09 | 89.25 ± 9.58 |
| t/χ2 | 0.259 | 3.834 | 0.628 | 0.902 | |
| P value | 0.796 | < 0.001 | 0.532 | 0.369 |
No statistically significant variations were observed in the levels of E and NE at 10 min prior to anesthesia induction between the two groups (P > 0.05). Nevertheless, the E and NE levels 5 min after extubation exhibited a notable decrease in the observation group compared to the control group (P < 0.05, Table 4).
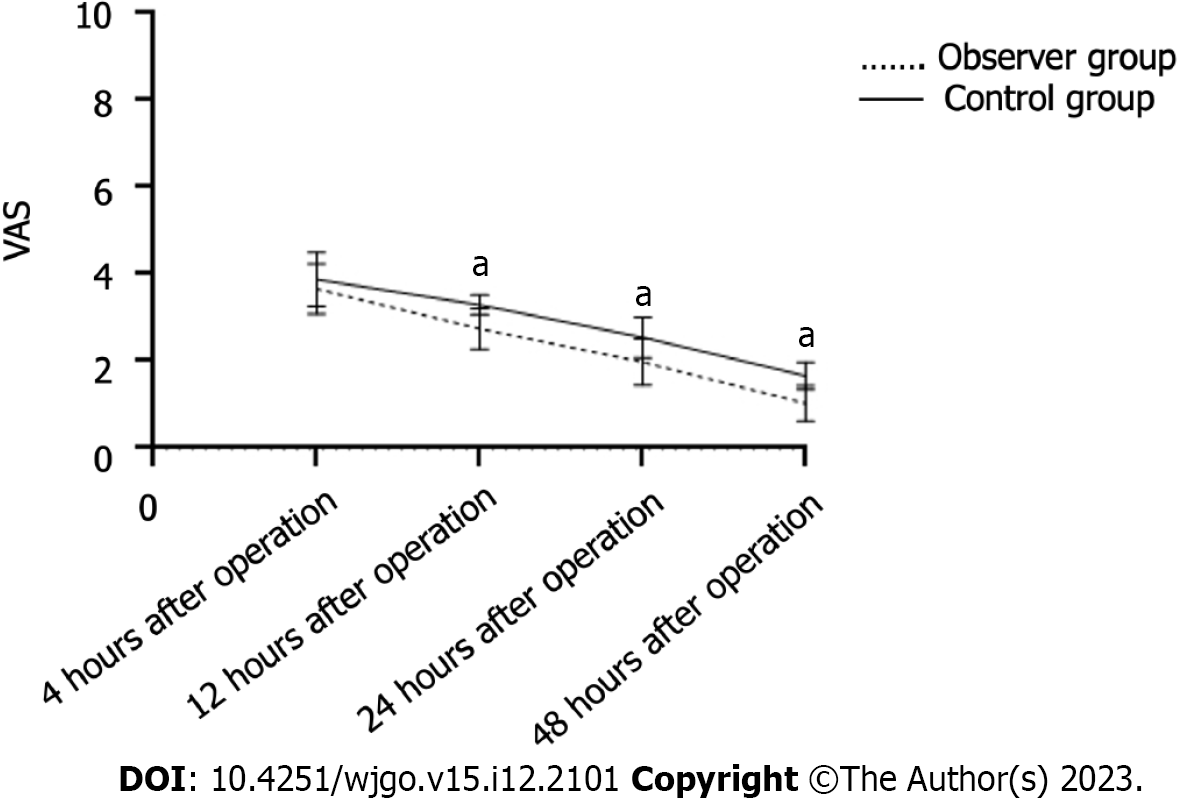
No statistically significant differences were observed in the VAS score between the two groups at the 4-h point following the surgical procedure (P > 0.05). Nevertheless, the VAS scores recorded at 12, 24, and 48 h post surgery showed a statistically significant decrease in the observation group (P < 0.05, Table 5, Figure 3).
| Group | n | 4 h following surgery | 12 h following surgery | 24 h following surgery | 48 h following surgery |
| Observation group | 51 | 3.65 ± 0.58 | 2.74 ± 0.47 | 1.97 ± 0.53 | 1.02 ± 0.41 |
| Control group | 51 | 3.87 ± 0.62 | 3.29 ± 0.23 | 2.54 ± 0.47 | 1.65 ± 0.32 |
| t/χ2 | 1.851 | 7.506 | 5.746 | 8.651 | |
| P value | 0.067 | < 0.001 | < 0.001 | < 0.001 |
There were no statistically significant differences in the duration of PACU stay between the two groups, as indicated by a P value greater than 0.05. The observation group exhibited a significantly shorter eye-opening and time to extubation time than the control group. Additionally, the observation group had a substantially lower Riker sedation-agitation score (P < 0.05, Table 6).
| Group | n | Time to eye-opening | Time to extubation | PACU stay duration | Riker sedation-agitation score (score) |
| Observation group | 51 | 18.12 ± 6.52 | 22.34 ± 8.31 | 37.54 ± 7.49 | 4.02 ± 1.33 |
| Control group | 51 | 23.25 ± 4.89 | 28.92 ± 6.54 | 38.12 ± 8.74 | 4.73 ± 0.82 |
| t/χ2 | 4.495 | 4.444 | 0.360 | 3.245 | |
| P value | < 0.001 | < 0.001 | 0.720 | 0.002 |
The observation group exhibited significantly lower effective PCA presses and sufentanil consumption within 24 h post surgery than the control group. Additionally, the observation group had a substantially lower number of cases requiring rescue analgesia (P < 0.05, Table 7).
| Group | n | Number of effective PCA presses within 24 h after surgery (mean ± SD) | Sufentanil consumption (μg, mean ± SD) | Number of rescue analgesia cases (cases) |
| Observation group | 51 | 3.52 ± 1.26 | 57.31 ± 5.82 | 3 |
| Control group | 51 | 6.11 ± 1.82 | 67.84 ± 4.37 | 13 |
| χ2 | 8.356 | 10.332 | 7.413 | |
| P value | < 0.001 | < 0.001 | 0.007 |
No statistically significant disparity was observed in the occurrence of postoperative nausea, vomiting, itching, or other unpleasant responses when comparing the two groups (P > 0.05, Table 8).
| Group | n | Nausea and vomiting | Skin itching | Respiratory depression | Hypotension |
| Observation group | 51 | 3 | 0 | 0 | 0 |
| Control group | 51 | 5 | 0 | 2 | 0 |
| χ2 | 0.543 | - | 2.040 | - | |
| P value | 0.461 | - | 0.153 | - |
As the proportion of aging adults increases, the incidence of gastrointestinal tumors has been increasing yearly. Although laparoscopic surgery can prolong the survival time of patients, factors such as CO2 pneumoperitoneum and positional changes during surgery can disturb the body’s homeostasis, leading to stress responses and causing severe postoperative pain that significantly affects surgical outcomes and postoperative recovery. Research has shown that administering various anesthetic medications during the perioperative phase substantially influences the stress reactions exhibited by patients under general anesthesia. Propofol is currently the most widely used intravenous anesthetic drug worldwide. However, it has apparent inhibitory effects on circulatory and respiratory functions, which can lead to hemodynamic fluctuations during surgery. Long-term use of propofol has drawbacks, such as drug residue, especially in patients with poor cardiovascular function or the elderly[7,8]. Remimazolam, a new type of benzodiazepine sedative-hypnotic drug, has the advantages of rapid metabolism, no residual effects, and minimal impact on respiration and circulation. It has been well applied in short and outpatient surgeries and is expected to be an anesthetic drug for reducing patient stress responses. Phase IIb/III trial results comparing propofol and remimazolam demonstrated that patients who received remimazolam had a lower incidence of adverse cardiovascular events such as bradycardia and hypotension than those who received propofol, confirming the safety and efficacy of remimazolam[9]. However, the analgesic and sedative effects of remimazolam alone are similar to those of propofol. Thus, additional anesthetics must be combined with remimazolam to improve the analgesic and soothing effects, further reduce the intraoperative stress response, and stabilize hemodynamics during the perioperative period.
The TAPB technique requires the administration of local anesthetics into the fascial gap across the transversus abdominis muscle and the internal oblique. This action effectively obstructs the abdominal wall nerves traversing this specific plane, hence inducing regional nerve block and analgesic effects on the anterior-lateral abdominal wall[10]. The TAPB technique blocks pain signal transmission by acting on the peripheral nerves and nerve fibers in the transversus abdominis plane, reducing postoperative pain perception. Moreover, TAPB can impede the transmission of nerve signals within the transversus abdominis plane, encompassing the intercostal nerves, inguinal nerves, and rectus abdominis nerves, consequently leading to the mitigation of pain postoperatively[11]. In recent years, with the continuous development of ultrasound-guided techniques, ultrasound-guided TAPB has been proven to effectively enhance the accuracy of needle insertion and enhance the analgesic and sedative effects of the blockade. Numerous studies have shown that TAPB can significantly alleviate postoperative pain and reduce opioid-related side effects, promoting postoperative recovery[12,13]. The present study investigated the use of TAPB combined with remimazolam in individuals undergoing laparoscopic surgery for gastrointestinal malignancies. The study’s findings indicate a statistically significant increase in HR at both T1 and T3 in the observation group compared to the control group. This suggests that the combination of TAPB and remimazolam is effective in maintaining stable hemodynamics during surgery while exerting fewer inhibitory effects on the circulatory system than remimazolam alone.
The hypothalamic-pituitary-adrenal axis is the primary mechanism mediating the acute stress response in the body. When sympathetic activation occurs during the perioperative period due to surgical trauma, fear and anxiety, or hypothermia, corticosteroid and catecholamine secretion, such as cortisol and E/NE, increases. The clinical manifestations include hemodynamic fluctuations, increased myocardial oxygen consumption, changes in RR and increased metabolic rates. In severe cases, internal environment disturbances, acid-base imbalances, and even arrhythmias can occur[14,15]. The outcomes of the present study demonstrated a significant decrease in E and NE levels 5 min following extubation in the observation group compared to the control group. This suggests that the combination of TAPB and remimazolam may be more effective in mitigating patient stress responses than remimazolam alone.
The Riker Sedation-Agitation Scale was proposed by Riker in 1999 and is mainly used to assess the level of agitation during the recovery phase in patients undergoing treatment under general anesthesia. It has higher reliability and authenticity in evaluating the awakening status of mechanically ventilated patients compared to the widely used Ramsay Sedation Scale[16,17]. The present study’s findings indicate that the time to eye opening and extubation was significantly shorter in the observation group than in the control group. The Riker sedation agitation score was notably lower in the observation group. Additionally, the VAS scores at 12, 24, and 48 h after surgery were significantly lower in the observation group, indicating that TAPB combined with remimazolam provides good analgesic and sedative effects, improves patient comfort during anesthesia recovery, and has a positive impact on improving the quality of recovery. In addition, compared to the control group, the observation group exhibited fewer PCA pump pushes and less sufentanil intake during the 24 h following surgery. The number of patients requiring rescue analgesia was considerably lower in the observation group, providing additional evidence to support the effective analgesic outcome of TAPB combined with remimazolam for postoperative pain control.
TAPB combined with remimazolam can improve the hemodynamic stability of patients undergoing gastrointestinal tumor surgery, reduce the stress response, and promote postoperative recovery. This study has limitations, that is, the sample size is limited and only focuses on patients undergoing gastrointestinal tumor surgery. In the future, the sample size will be expanded to analyze the potential benefits of the combination of TAPB and remimazolam.
Carbon dioxide pneumoperitoneum will be established in patients with gastrointestinal tumors during laparoscopic surgery, resulting in intra-abdominal hypertension, which is easy to cause stress response. At the same time, the change of posture will also aggravate the stress response, which will seriously affect the effect of surgical treatment and postoperative rehabilitation. Therefore, it is of great significance to adopt a reasonable anesthesia method to promote the postoperative recovery of patients. Transversus abdominis plane block (TAPB) can effectively block the conduction of the anterior nerve of the abdominal wall, resulting in analgesic effect. The success rate of remifentanil analgesia is similar to that of propofol, and the safety is significantly better than that of propofol. It can be used in the induction and maintenance of general anesthesia. The combination of TAPB and remimazolam and remimazolam can provide a basis for the anesthetic regimen to reduce the stress response of laparoscopic patients with gastrointestinal tumors.
The use of different anesthetics during the perioperative period of gastrointestinal tumors has an important impact on the stress response caused by general anesthesia. In the past, propofol was mostly used, but its obvious inhibition of circulatory and respiratory function can easily lead to intraoperative hemodynamic fluctuations. In addition, the change of intraoperative position can easily lead to stress response in patients, causing severe postoperative pain, which has a serious impact on the surgical effect and postoperative recovery. Remimazolam has the advantages of fast metabolism, no residue and little influence on respiration and circulation. However, the analgesic and sedative effects of simple application of remifentanil general anesthesia are similar to those of propofol. Therefore, it is necessary to combine the application of TAPB on the basis of remifentanil general anesthesia to improve the analgesic effect. It is expected to become an important anesthetic and analgesic scheme for laparoscopic surgery of gastrointestinal tumors in the future.
This study mainly discussed the effect of TAPB combined with remimazolam general anesthesia on stress response and postoperative recovery in patients undergoing gastrointestinal tumor surgery. The results showed that the application of TAPB combined with remimazolam general anesthesia in gastrointestinal tumor surgery had the advantages of stable anesthesia induction, small hemodynamic fluctuation, low incidence of cardiovascular events, fast postoperative recovery and less agitation. It is helpful to reduce acute stress response, improve the quality of recovery, and the level of analgesia and sedation can meet the needs of surgery. In the future, it can be used as an anesthesia and analgesia program for patients undergoing laparoscopic surgery for gastrointestinal tumors.
In this study, the clinical data of patients with gastrointestinal tumors who underwent laparoscopic surgery under general anesthesia were retrospectively analyzed. The patients were grouped according to different anesthesia schemes, and the hemodynamics, stress response and recovery quality of the observation group and the control group were compared. The data were analyzed by SPSS22.0 software to further clarify the application value of TAPB combined with remimazolam general anesthesia in patients undergoing gastrointestinal tumor surgery.
This study further clarified that TAPB combined with remimazolam general anesthesia can effectively alleviate the stress response of patients undergoing gastrointestinal tumor surgery. The level of analgesia and sedation is good, the intraoperative hemodynamic fluctuation is small, and the quality of recovery is good. However, this study is a retrospective analysis, and it is impossible to analyze the long-term effects of this anesthesia program and its application effect in other operations. In the future, the sample size will be further expanded to explore the application value of this anesthesia program.
The application of TAPB combined with remifentanil general anesthesia in gastrointestinal tumor surgery has the advantages of stable anesthesia induction, small hemodynamic fluctuations, low incidence of cardiovascular events, rapid postoperative recovery and less agitation. It is helpful to reduce acute stress response, improve the quality of recovery, and the level of analgesia and sedation can meet the needs of surgery.
In the future, the sample size will be expanded to explore the application value of TAPB combined with remifentanil general anesthesia in other types of laparoscopic surgery anesthesia.
| 1. | Gao K, Wu J. National trend of gastric cancer mortality in China (2003-2015): a population-based study. Cancer Commun (Lond). 2019;39:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 107] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 2. | Chen QY, Zhong Q, Liu ZY, Huang XB, Que SJ, Zheng WZ, Li P, Zheng CH, Huang CM. Advances in laparoscopic surgery for the treatment of advanced gastric cancer in China. Eur J Surg Oncol. 2020;46:e7-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W, Kim HI, Kim HH, Ryu SW, Hur H, Kim MC, Kong SH, Cho GS, Kim JJ, Park DJ, Ryu KW, Kim YW, Kim JW, Lee JH, Han SU; Korean Laparoendoscopic Gastrointestinal Surgery Study Group. Long-Term Outcomes of Laparoscopic Distal Gastrectomy for Locally Advanced Gastric Cancer: The KLASS-02-RCT Randomized Clinical Trial. J Clin Oncol. 2020;38:3304-3313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 295] [Article Influence: 49.2] [Reference Citation Analysis (1)] |
| 4. | Munteanu A, Munteanu D, Iancu M, Lupan I, Samasca G, Aldea C, Mocan T, Iancu C. Assessing immunological and surgical stress markers in patients undergoing digestive surgery for pancreatic, hepatic, and gastric tumors. Journal of B.U.ON: official journal of the Balkan Union of Oncology. 2018;23:1655. [DOI] [Full Text] |
| 5. | Peltrini R, Cantoni V, Green R, Greco PA, Calabria M, Bucci L, Corcione F. Efficacy of transversus abdominis plane (TAP) block in colorectal surgery: a systematic review and meta-analysis. Tech Coloproctol. 2020;24:787-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Dai G, Pei L, Duan F, Liao M, Zhang Y, Zhu M, Zhao Z, Zhang X. Safety and efficacy of remimazolam compared with propofol in induction of general anesthesia. Minerva Anestesiol. 2021;87:1073-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 7. | Tang S, Lu J, Xu C, Wei L, Mei S, Chen R, Meng QT. Feasibility and Safety of Remazolam versus Propofol When Inserting Laryngeal Masks Without Muscle Relaxants During Hysteroscopy. Drug Des Devel Ther. 2023;17:1313-1322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 8. | Liu G, Xiong Y. Analysis of Stress Response and Analgesic Effect of Remazolam Combined with Etomidate in Painless Gastroenteroscopy. Contrast Media Mol Imaging. 2022;2022:4863682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34:543-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 313] [Article Influence: 52.2] [Reference Citation Analysis (0)] |
| 10. | Tran DQ, Bravo D, Leurcharusmee P, Neal JM. Transversus Abdominis Plane Block: A Narrative Review. Anesthesiology. 2019;131:1166-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 135] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 11. | Kamel AAF, Amin OAI, Ibrahem MAM. Bilateral Ultrasound-Guided Erector Spinae Plane Block Versus Transversus Abdominis Plane Block on Postoperative Analgesia after Total Abdominal Hysterectomy. Pain Physician. 2020;23:375-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 12. | Liu KY, Lu YJ, Lin YC, Wei PL, Kang YN. Transversus abdominis plane block for laparoscopic colorectal surgery: A meta-analysis of randomised controlled trials. Int J Surg. 2022;104:106825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 13. | Emile SH, Elfeki H, Elbahrawy K, Sakr A, Shalaby M. Ultrasound-guided versus laparoscopic-guided subcostal transversus abdominis plane (TAP) block versus No TAP block in laparoscopic cholecystectomy; a randomized double-blind controlled trial. Int J Surg. 2022;101:106639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 14. | Aly A, Gouda J, Awadein A, Soliman HM, El-Fayoumi D. Serum cortisol and adrenocorticotrophic hormone (ACTH) in infants receiving topical and subconjunctival corticosteroids following cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2021;259:3159-3165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Milone M, Desiderio A, Velotti N, Manigrasso M, Vertaldi S, Bracale U, D'Ambra M, Servillo G, De Simone G, De Palma FDE, Perruolo G, Raciti GA, Miele C, Beguinot F, De Palma GD. Surgical stress and metabolic response after totally laparoscopic right colectomy. Sci Rep. 2021;11:9652. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Feng X, Zhao B, Wang Y. Effect Evaluation of Dexmedetomidine Intravenous Anesthesia on Postoperative Agitation in Patients with Craniocerebral Injury by Magnetic Resonance Imaging Based on Sparse Reconstruction Algorithm. Contrast Media Mol Imaging. 2022;2022:5161703. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 17. | Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation-Agitation Scale for adult critically ill patients. Crit Care Med. 1999;27:1325-1329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 617] [Cited by in RCA: 625] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Seeneevassen L, France; Vidal AF, Brazil S-Editor: Qu XL L-Editor: A P-Editor: Zhang XD