Published online Oct 15, 2023. doi: 10.4251/wjgo.v15.i10.1796
Peer-review started: May 31, 2023
First decision: June 26, 2023
Revised: July 7, 2023
Accepted: September 1, 2023
Article in press: September 1, 2023
Published online: October 15, 2023
Processing time: 131 Days and 15.2 Hours
In the United States, sorafenib monotherapy was approved in 2007 for first-line (1L) treatment of patients with unresectable hepatocellular carcinoma (uHCC). As other therapies have been approved in recent years for hepatocellular carcinoma treatment in later lines, it is essential to assess clinical effectiveness of older therapies in actual clinical practice to inform healthcare practitioners’ decisions for better patient care.
To assess patient characteristics/clinical effectiveness of 1L sorafenib in uHCC patients treated in United States academic and community practice settings.
A retrospective observational study was conducted among adult patients (≥ 18 years) in the United States initiating sorafenib monotherapy as 1L systemic therapy for uHCC with Eastern Cooperative Oncology Group status of 0 or 1 between January 2016 and December 2019 at City of Hope and Advent Health. Data were extracted by trained abstractionists from individual patients’ electronic health records and captured in electronic case report forms. Institutional Review Board approvals were obtained prior to study initiation. Data were captured from the time of sorafenib initiation until death or the end of follow-up. All data were de-identified prior to analyses. Clinical outcomes assessed included provider-reported best response, progression-free survival (PFS), and overall survival (OS). PFS and OS were estimated using Kaplan-Meier methods.
Among 134 uHCC patients treated with 1L sorafenib, majority were male (75%), and most were Caucasian (62%) or Asian (19%). Median patient age was 64 years. The most common etiologies of liver disease were hepatitis C (54%), alcohol-related liver disease (16%), and hepatitis B (11%). Most patients were reported to have Barcelona Clinic Liver Cancer stage B (19%) or stage C (70%) disease. Of 134 patients, 110 (82%) were reported to have discontinued treatment or died during follow-up. Primary reasons for sorafenib discontinuation were reported as progression (35%) and toxicity (30%). Best overall response was reported for 124 patients, of which 7.3% reported complete or partial response. Median time to treatment discontinuation was 2.3 mo. Overall, 103 patients (77%) had disease progression or died during sorafenib therapy. Median PFS was estimated to be 2.9 mo. At the end of follow-up, 82 patients (61%) were deceased. Median OS was 8.5 mo.
Newer therapeutic options that have reported higher PFS and OS in real-world clinical practice should be considered to enhance patient outcomes.
Core Tip: As treatment options evolve for hepatocellular carcinoma (HCC) it is important to assess and understand the clinical outcomes with older treatment options in diverse real-world clinical practice settings to inform clinical decision making and identify the right patient for the right drug. The current study aimed to assess the patient characteristics and clinical effectiveness of sorafenib as first-line therapy in unresectable HCC patients treated in both academic and community practice settings in the United States.
- Citation: Li D, Gruber SB, Iyer S, Gupta S, Tejani M. Real-world clinical effectiveness of sorafenib among patients with unresectable hepatocellular carcinoma at two centers in the United States. World J Gastrointest Oncol 2023; 15(10): 1796-1806
- URL: https://www.wjgnet.com/1948-5204/full/v15/i10/1796.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v15.i10.1796
Primary liver cancer is the sixth most commonly diagnosed cancer and the third leading cause of cancer death worldwide in 2020, with approximately 906000 new cases and 830000 deaths[1]. Hepatocellular carcinoma (HCC) is the most common type of liver cancer and accounts for approximately 75% of liver cancer cases in the United States[2]. Systemic treatments may benefit patients with advanced-stage HCC. Sorafenib was the first systemic drug approved by the United States Food and Drug Administration in 2007 and was considered standard of care until 2018[3].
Sorafenib was approved for the treatment of unresectable HCC (uHCC) after two phase III trials [Sorafenib HCC assessment randomized protocol (SHARP) and Asia-Pacific] demonstrated significant improvements in overall survival (OS)[4,5]. However, rapid advances during the last four years have led to the approval of other molecular targeted drugs and several immune checkpoint inhibitors[3] for first- or second/later-line use. In the first-line (1L) setting, lenvatinib was approved in July 2018 for the treatment of advanced uHCC patients[6]. Additional systemic treatment options are currently available and approved for use in sorafenib-treated patients (in second or later lines), including the tyrosine kinase inhibitors regorafenib and cabozantinib, the vascular endothelial growth factor receptor inhibitor ramucirumab, and the programmed cell death protein 1 inhibitor pembrolizumab[7-11].
Though previous retrospective and prospective real-world observational studies have evaluated clinical effectiveness of sorafenib[12-17], with the evolving landscape it is important to reassess clinical outcomes like OS in patients treated with 1L sorafenib, given there are many more options. Understanding OS with sorafenib becomes more critical given sorafenib is now a generic drug in the United States and progression-free survival (PFS)/OS are critical elements in assessing cost-benefit ratios of treatments, especially when comparing to novel branded therapeutic options. In our study we assess clinical outcomes of uHCC patients treated with 1L sorafenib at an academic cancer center and a community cancer practice.
A retrospective observational study was conducted among adult patients (≥ 18 years) in the United States who had initiated sorafenib monotherapy as 1L systemic therapy for uHCC with an Eastern Cooperative Oncology Group (ECOG) status of 0 or 1 between January 2016 and December 2019 at an academic cancer center (City of Hope) and a community cancer practice (Advent Health). City of Hope is an academic and National Cancer Institute-designated Comprehensive Cancer Center located in the state of California. Advent Health is a large regional community health system headquartered in Florida serving 5 million patients across 9 states (Colorado, Florida, Georgia, Illinois, Kansas, Kentucky, North Carolina, Texas, and Wisconsin). Patients were excluded if there was evidence of other malignant neoplasms within 3 years prior to initiation of sorafenib, liver transplant recorded at any point in their medical history, or if they had received sorafenib as part of a clinical trial. Each collaborating center had the study protocol reviewed and approved by their respective Institutional Review Board. All data transmitted from the data collaborators in support of the study were de-identified pursuant to Health Insurance Portability and Accountability Act Privacy Rule 164.514 (b) and (c).
Patient medical records were selected randomly in a three-part process as depicted in Figure 1. Each center used a database query to identify a superset of patients that contained all eligible patients (and likely some that were ineligible). Data were collected using a standard electronic case report form (eCRF) at both centers. Structured data were automatically collected from de-identified electronic medical records (EMR). Data explicitly stated in the EMR and not requiring any inference or clinical judgment were entered into the eCRF by expert oncology chart abstractionists trained on the study protocol at each center. Data abstracted by the abstractionists were reviewed by the study oncologist for completeness and quality assurance. Treating oncologists who were specifically trained on the study protocol also captured certain key data that were not expressly stated in the EMR but could be determined through clinical judgment from evidence in the patient EMR (including unstructured physician notes e.g., response, progression).
Sorafenib monotherapy initiated as 1L systemic therapy for uHCC between January 2016 and December 2019.
Data on these patients were captured from the time of sorafenib initiation until their death, lost to contact, or the end of follow-up.
Patient demographics and clinical history were extracted from the EMR. Demographics of interest included age at sorafenib initiation, sex, and race/ethnicity. Clinical history included liver disease etiology (hepatitis B, hepatitis C, alcohol-related, and nonalcoholic fatty liver disease), cirrhosis severity (Child-Pugh score), ECOG performance status, and Barcelona Clinic Liver Cancer (BCLC) stage. Patients’ treatment characteristics included receipt of treatments or procedures prior to and after sorafenib. Information about treatment with sorafenib start and end dates was ascertained. The reasons for discontinuation were captured at a category-level only (e.g., toxicity, progression, patient preference, death, not reported).
After baseline tumor assessment, subsequent assessments by the treating oncologist recorded the tumor response as progressive disease (PD), stable disease (SD), partial response (PR), complete response (CR), not evaluable. When these observations were stated explicitly in the patient medical record, they were captured by the abstractionists. When the tumor response was not explicitly stated by the treating oncologist in the EMR the abstractionist recorded that an assessment was done but tumor response was “not stated”. The reviewing oncologist recorded the patients’ best overall response (BOR) on sorafenib based on the treating oncologists’ explicitly stated assessment or, if that was not available, by applying their clinical judgment based on the evidence in the EMR. The physician-reported criteria used to evaluate best clinical response [e.g., Response Evaluation Criteria in Solid Tumors (RECIST) 1.1, modified (m) RECIST, or physician assessment, if no specific criteria were reported in patient charts] were collected. PFS was defined as time from sorafenib initiation to clinical progression or death during sorafenib treatment, and OS was defined as time from sorafenib initiation to death. For PFS, patients who did not progress during sorafenib treatment were censored at sorafenib treatment stop date; for OS, those who were still alive at the time of data collection were censored at the date of their last available medical record.
Our study did not involve formal hypothesis testing or comparative analyses and was primarily descriptive; therefore, the sample size was based on available resources rather than a formal statistical power calculation. Descriptive statistics were reported for patients’ demographic, clinical, and treatment characteristics as well as for physicians’ characteristics. Missing data were not extrapolated or estimated and were calculated as percentage of patients of the total that had a particular characteristic as missing or not reported. Clinical outcomes are reported for the overall cohort. Real-world BOR (rwBOR) was calculated as percentage of patients who had a real-world best response reported as partial or complete. Disease control rate (DCR) was calculated as percentage of patients who had a rwBOR of SD, PR, or CR. Time-to-event outcomes (i.e., PFS and OS) were estimated using the Kaplan-Meier method. PFS and OS between subgroups were compared using log-rank tests. A P value of P < 0.05 was considered statistically significant. The statistical methods of this study were reviewed by Shrividya Iyer from Eisai.
Patient demographics and clinical characteristics of the 134 patients who received 1L sorafenib are shown in Table 1 and Table 2, respectively. Patients’ median age was 64 years, and most patients were male (75%) and Caucasian (62%) or Asian (19%) (Table 1). Majority of the patients had either Child-Pugh class A cirrhosis (36%) or Child-Pugh class B cirrhosis (40%), with 9% showing more severe liver dysfunction with Child-Pugh class C cirrhosis. More than half (54%) of patients were diagnosed with hepatitis C and 11% with hepatitis B infection, whereas 16% of patients had alcohol-related liver disease and 8% had nonalcoholic fatty liver disease. Majority (70%) of patients were BCLC stage C, whereas 19% were BCLC stage B, and 9% BCLC stage A at initiation of 1L sorafenib (Table 2). Portal vein thrombosis was reported in 13% of patients.
| Characteristic | Overall (n = 134) | Advent Health (n = 62) | City of Hope (n = 72) |
| Age at diagnosis (yr) | |||
| Mean | 65 | 64 | 65 |
| Median (range) | 64 (33-90) | 63 (44-79) | 66 (33-90) |
| Sex, n (%) | |||
| Male | 101 (75) | 50 (81) | 51 (71) |
| Female | 33 (25) | 12 (19) | 21 (29) |
| BMI, n (%) | |||
| < 18.5 | 4 (3) | 4 (6) | - |
| 18.5-24.9 | 48 (36) | 20 (32) | 28 (39) |
| 25-29.9 | 38 (28) | 14 (23) | 24 (33) |
| ≥ 30 | 34 (25) | 21 (34) | 13 (18) |
| Not reported | 10 (8) | 3 (5) | 7 (10) |
| Race, n (%) | |||
| Asian | 25 (19) | 3 (5) | 22 (31) |
| African-American | 15 (11) | 11 (18) | 4 (6) |
| Native Hawaiian or other Pacific Islander | 1 (1) | - | 1 (1) |
| Caucasian | 83 (62) | 41 (66) | 42 (58) |
| Not reported | 10 (7) | 7 (11) | 3 (4) |
| Ethnicity, n (%) | |||
| Hispanic or Latino | 34 (25) | 16 (26) | 18 (25) |
| Non-Hispanic or Non-Latino | 94 (70) | 45 (73) | 49 (68) |
| Not reported | 6 (5) | 1 (1) | 5 (7) |
| Overall (n = 134) | Advent Health (n = 62)1 | City of Hope (n = 72) | |
| Child-Pugh class, n (%) | |||
| A | 48 (36) | 26 (42) | 22 (31) |
| B | 54 (40) | 25 (40) | 29 (40) |
| C | 12 (9) | 7 (11) | 5 (7) |
| Not reported | 20 (15) | 4 (6) | 16 (22) |
| BCLC stage, n (%) | |||
| 0 | 1 (1) | 1 (2) | - |
| A | 12 (9) | 2 (3) | 10 (14) |
| B | 25 (19) | 22 (35) | 3 (4) |
| C | 94 (70) | 36 (58) | 58 (81) |
| D | 1 (1) | - | 1 (1) |
| Not reported | 1 (1) | 1 (2) | 0 |
| ECOG, n (%) | |||
| 0 | 28 (21) | 10 (16) | 18 (25) |
| 1 | 103 (77) | 49 (79) | 54 (75) |
| Not reported | 3 (2) | 3 (5) | 0 |
| Etiology, n (%) | |||
| Hepatitis B | 15 (11) | 5 (8) | 10 (14) |
| Hepatitis C | 72 (54) | 35 (56) | 37 (51) |
| Alcohol-related liver disease | 21 (16) | 10 (16) | 11 (15) |
| Nonalcoholic fatty liver disease | 11 (8) | 4 (6) | 7 (10) |
| Not reported/none of the above | 15 (11) | 8 (13) | 7 (10) |
Of the 134 patients treated with 1L sorafenib, 110 were known to have discontinued treatment or died during the observation period. Median real-world time to treatment discontinuation (rwTTD) was 69 d (2.3 mo) from initiation of 1L sorafenib. Among patients with Child-Pugh class A cirrhosis, median rwTTD was 2.4 mo; among patients with Child-Pugh class B cirrhosis, median rwTTD was 1.9 mo, while patients with Child-Pugh class C cirrhosis had a median rwTTD of 1 mo.
Reason for discontinuation of 1L sorafenib was available for 102 patients. For majority of patients, sorafenib was discontinued due to progression (35%) and toxicity (30%). Death (5%), patient preference (3%), and hospice or palliative care (2%) were other reasons listed as a reason for discontinuation.
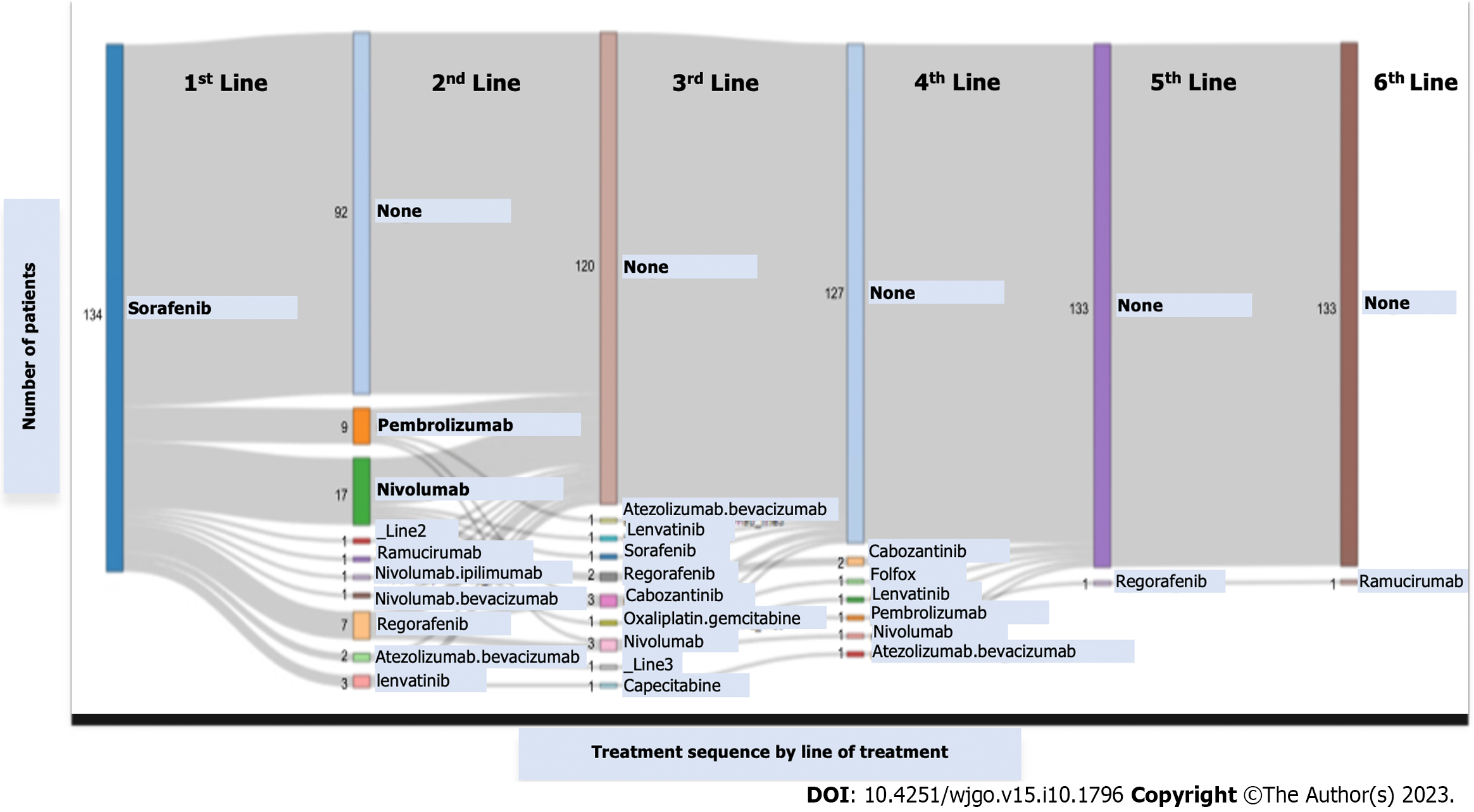
Majority of the patients (69%) received only one line of therapy. Of those who went on to receive subsequent lines of therapy, 17 (40%) received second-line nivolumab and 9 (21%) received second-line pembrolizumab. Figure 2 shows the therapeutic sequences observed.
Of the 134 patients that received 1L sorafenib, 124 patients had response information captured from the EMR. The response findings were based on the treating physicians’ assessment. Overall, 9 patients (7.3%) had best response reported as CR or PR on 1L sorafenib; 55 patients reported a best response as CR, PR, or SD with a DCR of 44.4%. BOR for subgroups are presented in Table 3.
| Cohort/subgroup | Best overall response, % (CR + PR) | N (PFS) | Median PFS (Q1, Q3), months | HR (95%CI) | N (OS) | Median OS (Q1, Q3), months | HR (95%CI) |
| Overall | 7.3 | 121 | 2.9 (1.5, 5.6) | 134 | 8.5 (3.6, 24.6) | ||
| Age group (yr) | |||||||
| < 651 | 7.7 | 61 | 3.5 (1.8, 7.1) | 69 | 8.5 (3.6, 23.4) | ||
| 65-75 | 9.8 | 42 | 2.3 (1, 10.3) | 1.40 (0.90-2.15) | 45 | 10.6 (4, 29.7) | 0.87 (0.53-1.44) |
| > 75 | 0 | 18 | 3.8 (1.5, 7.9) | 0.85 (0.48-1.52) | 18 | 6 (3.1, 31.6) | 1.09 (0.58-2.02) |
| Sex | |||||||
| Male1 | 7.4 | 91 | 2.8 (1.6, 5.4) | 92 | 7.1 (3.6, 21.8) | ||
| Female | 6.9 | 30 | 3.6 (1.3, 7.9) | 0.84 (0.53-1.32) | 31 | 14.2 (3.7, 30.3) | 0.68 (0.41-1.15) |
| Race | |||||||
| Asian1 | 12.0 | 25 | 3 (1.5, 5.4) | 25 | 10.6 (5.4, 23.4) | ||
| African-American | 7.7 | 12 | 4.5 (1.9, 6.7) | 0.90 (0.43-1.89) | 15 | 13.7 (1.8, 36.2) | 1.03 (0.47-2.27) |
| Native Hawaiian or other Pacific Islander | 0 | 1 | 2.8 (2.8, 2.8) | 1.37 (0.18-10.3) | 1 | 2.8 (2.8, 2.8) | 6.52 (0.82-51.7) |
| Caucasian | 6.4 | 77 | 2.6 (1.5, 6.4) | 0.89 (0.54-1.47) | 82 | 9.3 (4, 29.7) | 1.05 (0.59-1.84) |
| Child-Pugh Class | |||||||
| A1 | 9.1 | 43 | 3.1 (1.9, 5.4) | 47 | 10.6 (5.2, 24.6) | ||
| B | 10.2 | 50 | 2.6 (1.5, 5.6) | 1.23 (0.79-1.93) | 54 | 6.3 (2.8, 14.2) | 1.36 (0.84-2.19) |
| C | 0 | 11 | 1.4 (0.7, 2.5) | 3.27 (1.57-6.79)a | 12 | 3 (1.7, 4.2) | 4.49 (1.87-10.8)a |
| BCLC stage | |||||||
| 0 | 0 | 1 | 1 (1, 1) | NA | 1 | Not reached | NA |
| A1 | 9.1 | 10 | 10.8 (1, 14.8) | 12 | 23.4 (23.4, -) | ||
| B | 21.7 | 23 | 2.9 (1.5, 9.8) | 1.64 (0.68-3.96) | 24 | 9 (3.1, 22.6) | 4.67 (1.08-20.1) |
| C | 3.4 | 85 | 3 (1.6, 5.3) | 1.79 (0.80-3.98) | 93 | 7.1 (3.6, 24.6) | 4.35 (1.06-17.8) |
| D | 0 | 1 | 2.1 (2.1, 2.1) | NA | 1 | 5.4 (5.4, 5.4) | NA |
| ECOG | |||||||
| 01 | 12.5 | 25 | 5.1 (3, 10.5) | 27 | 29.1 (6, 30.3) | ||
| 1 | 6.2 | 94 | 2.4 (1.4, 5.2) | 1.70 (1.03-2.83)a | 102 | 6.3 (3.1, 14.2) | 2.02 (1.13-3.60) |
| Hepatitis B | |||||||
| No1 | 6.5 | 106 | 3 (1.5, 6) | 116 | 7.9 (3.6, 29.7) | ||
| Yes | 13.3 | 14 | 3 (1.9, 7.3) | 0.90 (0.48-1.70) | 15 | 9 (5.4, 21.8) | 1.31 (0.70-2.42) |
| Hepatitis C | |||||||
| No1 | 5.5 | 54 | 2.8 (1.5, 5.4) | 60 | 7.9 (5, 21.8) | ||
| Yes | 8.8 | 66 | 3 (1.5, 7.1) | 0.94 (0.63-1.39) | 71 | 9.3 (3.6, 29.1) | 0.85 (0.54-1.32) |
| Alcohol-related liver disease | |||||||
| No1 | 7.8 | 102 | 3 (1.5, 6.4) | 110 | 9 (3.7, 29.1) | ||
| Yes | 4.8 | 18 | 2.6 (2.1, 4.1) | 1.17 (0.68-2.00) | 21 | 7.1 (3.1, 13.4) | 1.46 (0.81-2.61) |
| Nonalcoholic fatty liver disease | |||||||
| No1 | 7.1 | 110 | 3 (1.6, 5.6) | 120 | 7.9 (3.7, 23.4) | ||
| Yes | 10.0 | 10 | 2.8 (1.4, 10.6) | 0.79 (0.38-1.63) | 11 | 10.6 (3.1, 29.7) | 0.71 (0.31-1.64) |
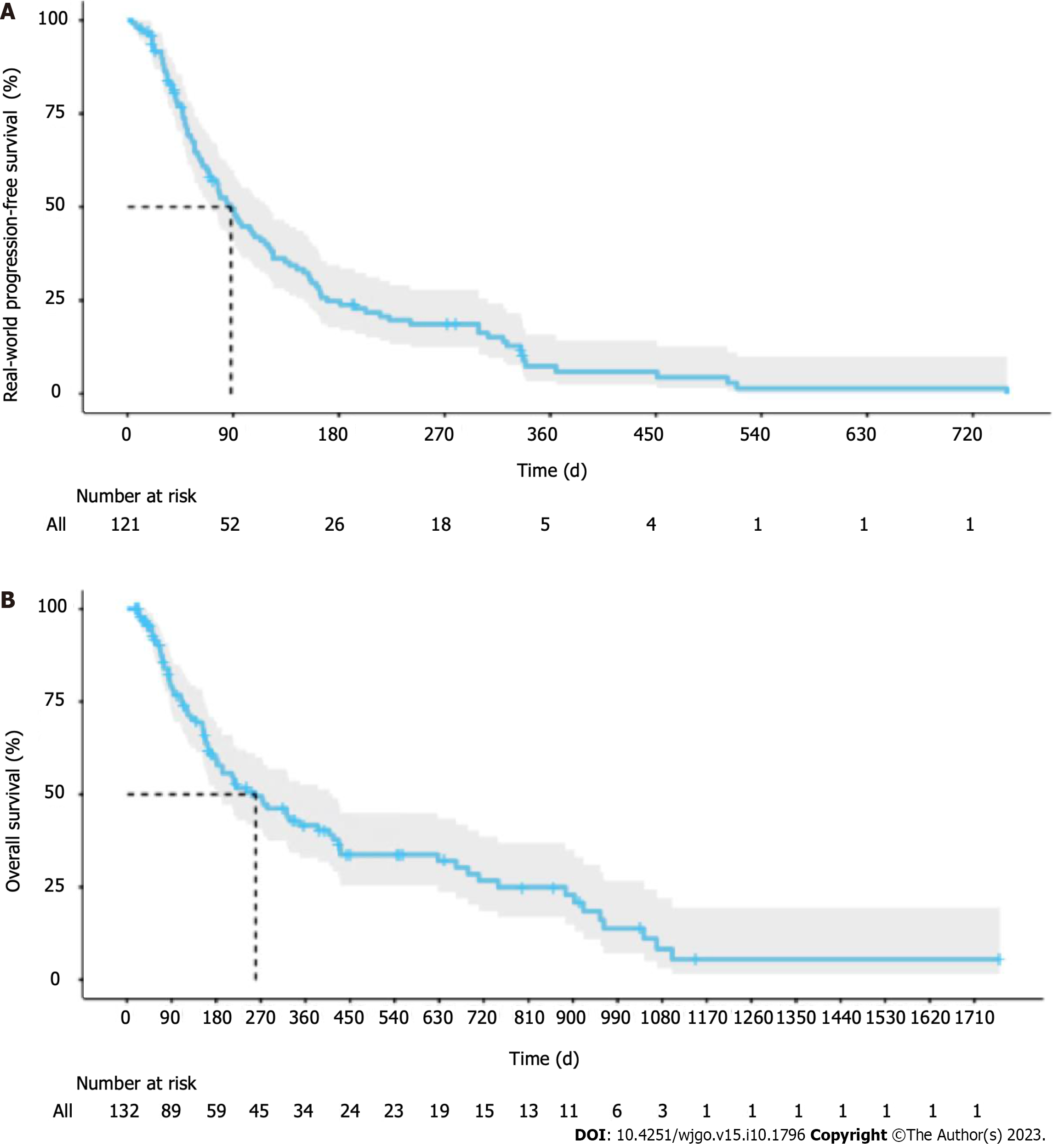
Overall, 103 of 134 patients had disease progression or died during sorafenib therapy. Median rwPFS was 88 d (2.9 mo) from initiation of 1L sorafenib (Figure 3A). Median rwPFS was estimated to be 3.1 mo among patients with Child-Pugh class A cirrhosis, 2.6 mo among patients with Child-Pugh class B cirrhosis, and 1.4 mo among patients with Child-Pugh class C cirrhosis. RwPFS was observed to be significantly lower in Child-Pugh C patients compared to Child-Pugh A patients [hazard ratio (HR) = 3.27, 95% confidence interval (CI): 1.57-6.79, P < 0.05] and in patients with an ECOG status of 1 compared to patients with an ECOG status of 0 (HR = 1.70, 95% CI: 1.03-2.83, P < 0.05) (Table 3).
At the end of the observation period, 82 patients (61%) were deceased. Median OS was 258 d (8.5 mo) from initiation of 1L sorafenib (Figure 3B). Median OS was 10.6 mo among patients with Child-Pugh class A cirrhosis, 6.3 mo among patients with Child-Pugh class B cirrhosis, and 3 mo among patients with Child-Pugh class C cirrhosis. Median OS was significantly lower in Child-Pugh C patients compared to Child-Pugh A patients (HR = 4.49, 95% CI: 1.87-10.8, P < 0.05). No statistically significant differences in OS were observed between other subgroups (Table 3).
Our retrospective real-world study evaluated clinical outcomes among a demographically and clinically diverse adult uHCC patient population treated at an academic cancer center and a community health care system, thus including uHCC patients treated with 1L sorafenib in diverse health care settings from multiple states in the United States.
The clinical outcomes observed in our study were similar to previously published real-world data studies as well as the sorafenib arm clinical outcomes in major clinical trials. The results of the SHARP study demonstrated the clinical effectiveness of sorafenib in the treatment of uHCC. Compared to the placebo group, the sorafenib treatment group had significantly prolonged median OS (10.7 vs 7.9 mo)[4,5]. In the Asia-Pacific study, patients treated with sorafenib had a longer median OS (6.4 vs 4.2 mo) and median time to progression (2.8 vs 1.4 mo) compared to placebo[5]. Notably, the patient population in our real-world study had Child-Pugh scores ranging from A to C, while the majority (> 95%) of patients in SHARP had Child-Pugh A scores[4].
In line with previous clinical and prospective real-world data studies, median PFS and median OS in patients treated with sorafenib in our study were shorter in Child-Pugh B patients compared with Child-Pugh A patients[13,14]. In a multi-center phase 2 trial, the median PFS (range) for the total patient population was 3.9 (0.1-35.3) mo; median PFS (range) for patients with Child-Pugh A or B cirrhosis was 4.3 (0.1-35.3) mo and 2.1 (0.3-27.3) mo, respectively (log-rank P < 0.001). In the multivariate analysis in the same trial, Child-Pugh B patients had a greater risk of disease progression or death compared to Child-Pugh A patients (HR 1.87, 95%CI: 1.41-2.48, P < 0.001)[14].
The global investigation of therapeutic decisions in HCC and of its treatment with sorafenib trial was a large prospective, observational cross-regional registry study undertaken to evaluate the real-life use, safety, and effectiveness of sorafenib in HCC patients; it included patients with baseline Child-Pugh B (21%) and C (2%) liver function[13]. Median OS was longer in Child-Pugh A patients (13.6 mo) than in Child-Pugh B patients (5.2 mo) and Child-Pugh C patients (2.6 mo)[13]. In a smaller retrospective real-world study of patients treated with sorafenib in Portugal (n = 36), median OS was reported to be 6.8 mo (95%CI: 3-10.6). Median OS differed according to Child-Pugh class [Child-Pugh A: 17.3 mo (95%CI: 5.3-29.4) vs Child-Pugh B: 3.2 mo (95%CI: 0.9-5.5); P = 0.001][17]. In the same study by Cardoso et al[17], two patients (6%) had PR, nine patients (25%) were classified as SD, and seven patients (19%) reported PD. Sixteen patients were also evaluated according to mRECIST criteria; one patient reached CR, four patients (11%) had PR, three patients (8%) had SD, and eight patients (22%) reported PD.
Our real-world study has a few limitations. Clinical data were entered directly into the eCRFs by data abstractionists based on medical records available at the time of data entry; therefore, the data are potentially subject to inadvertent entry, keying errors, or missing data. Review of the eCRFs by treating oncologists was enforced to minimize these errors. Frequency of scans in clinical practice might vary between patients and could be less frequent than commonly mandated in clinical trials. While published response criteria were provided as guidance in eCRFs, clinical responses were based on physician assessment and a criterion (if used) was asked to be reported. No safety data were collected. Our study may have also missed ascertainment of care received outside of the study clinics, and the convenience sample of United States-based centers likely limits the generalizability of our findings to other countries. Despite these limitations, our study provides useful information on the use and outcomes of sorafenib in real-world clinical practice in the United States.
To our knowledge, no other retrospective study has evaluated real-world outcomes of sorafenib in the United States combining data from an established academic cancer center and a multi-state community health care system. Real-world median PFS and OS of sorafenib in 1L uHCC were < 3 mo and < 9 mo, respectively. Newer therapeutic options that have reported higher PFS and OS in real-world clinical practice should be considered as 1L treatment choices to enhance uHCC patient outcomes.
Sorafenib has been approved for use in unresectable hepatocellular carcinoma (uHCC) patients for more than a decade. As other therapies have been approved in recent years for uHCC treatment in later lines, it is essential to assess clinical effectiveness of older therapies in actual clinical practice to inform healthcare practitioners’ decisions for better patient care.
Limited recent data on real-world clinical effectiveness of sorafenib in diverse clinical practice settings in the United States.
To assess clinical effectiveness of sorafenib as first-line (1L) therapy in uHCC patients treated in both academic and community practice settings in the United States.
In a retrospective observational study we assessed clinical outcomes including best response, progression-free survival (PFS), and overall survival (OS) among adult uHCC patients (≥ 18 years) in the United States initiating 1L sorafenib monotherapy at City of Hope (academic) and Advent Health (community practice) between January 2016 and December 2019.
Median time to treatment discontinuation was 2.3 mo. Overall, 103 patients (77%) had disease progression or died during sorafenib therapy. Median PFS was 2.9 mo and median OS was 8.5 mo.
Median PFS and OS of sorafenib in 1L uHCC were < 3 mo and < 9 mo, respectively.
Newer therapeutic options that have reported higher PFS and OS in real-world clinical practice should be considered to enhance patient outcomes.
We would like to acknowledge Christiana Crook, clinical research assistant at City of Hope, for providing editorial assistance, and Xiaoyu Xia, Ethan Truong, Kimber Slater, Yvette Estrada, Katherine Roth, Sidney Lindsey, and Joseph Bonner from City of Hope Center for Precision Medicine. The authors would like to acknowledge Samir Courdy and Srisairam Achuthan from City of Hope Center for Informatics for the utilization of the POSEIDON platform for data exploration, visualization, analysis, and discovery.
| 1. | World Health Organization. Globocan: The IARC Global Cancer Observatory. 2020. [cited 3 February 2022]. Available from: http://globocan.iarc.fr/old/FactSheets/cancers/Liver-new.asp. |
| 2. | Petrick JL, Kelly SP, Altekruse SF, McGlynn KA, Rosenberg PS. Future of Hepatocellular Carcinoma Incidence in the United States Forecast Through 2030. J Clin Oncol. 2016;34:1787-1794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 363] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 3. | Zhang H, Zhang W, Jiang L, Chen Y. Recent advances in systemic therapy for hepatocellular carcinoma. Biomark Res. 2022;10:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 157] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 4. | Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9016] [Cited by in RCA: 10530] [Article Influence: 585.0] [Reference Citation Analysis (9)] |
| 5. | Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3854] [Cited by in RCA: 4740] [Article Influence: 263.3] [Reference Citation Analysis (0)] |
| 6. | Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng AL. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4432] [Cited by in RCA: 4112] [Article Influence: 514.0] [Reference Citation Analysis (5)] |
| 7. | Foerster F, Galle PR. Comparison of the current international guidelines on the management of HCC. JHEP Rep. 2019;1:114-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, Gerolami R, Masi G, Ross PJ, Song T, Bronowicki JP, Ollivier-Hourmand I, Kudo M, Cheng AL, Llovet JM, Finn RS, LeBerre MA, Baumhauer A, Meinhardt G, Han G; RESORCE Investigators. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2160] [Cited by in RCA: 2843] [Article Influence: 315.9] [Reference Citation Analysis (1)] |
| 9. | Abou-Alfa GK, Meyer T, Cheng AL, El-Khoueiry AB, Rimassa L, Ryoo BY, Cicin I, Merle P, Chen Y, Park JW, Blanc JF, Bolondi L, Klümpen HJ, Chan SL, Zagonel V, Pressiani T, Ryu MH, Venook AP, Hessel C, Borgman-Hagey AE, Schwab G, Kelley RK. Cabozantinib in Patients with Advanced and Progressing Hepatocellular Carcinoma. N Engl J Med. 2018;379:54-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1630] [Cited by in RCA: 1862] [Article Influence: 232.8] [Reference Citation Analysis (1)] |
| 10. | Zhu AX, Kang YK, Yen CJ, Finn RS, Galle PR, Llovet JM, Assenat E, Brandi G, Pracht M, Lim HY, Rau KM, Motomura K, Ohno I, Merle P, Daniele B, Shin DB, Gerken G, Borg C, Hiriart JB, Okusaka T, Morimoto M, Hsu Y, Abada PB, Kudo M; REACH-2 study investigators. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20:282-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1027] [Cited by in RCA: 1315] [Article Influence: 187.9] [Reference Citation Analysis (1)] |
| 11. | Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY, Breder V, Edeline J, Chao Y, Ogasawara S, Yau T, Garrido M, Chan SL, Knox J, Daniele B, Ebbinghaus SW, Chen E, Siegel AB, Zhu AX, Cheng AL; KEYNOTE-240 investigators. Pembrolizumab As Second-Line Therapy in Patients With Advanced Hepatocellular Carcinoma in KEYNOTE-240: A Randomized, Double-Blind, Phase III Trial. J Clin Oncol. 2020;38:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1365] [Cited by in RCA: 1398] [Article Influence: 233.0] [Reference Citation Analysis (1)] |
| 12. | Jo M, Yasui K, Kirishima T, Shima T, Niimi T, Katayama T, Mori T, Funaki J, Sumida Y, Fujii H, Takami S, Kimura H, Mitsumoto Y, Minami M, Yamaguchi K, Yoshinami N, Mizuno M, Sendo R, Tanaka S, Shintani H, Kagawa K, Okanoue T, Itoh Y. Efficacy and safety of sorafenib in very elderly patients aged 80 years and older with advanced hepatocellular carcinoma. Hepatol Res. 2014;44:1329-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Marrero JA, Kudo M, Venook AP, Ye SL, Bronowicki JP, Chen XP, Dagher L, Furuse J, Geschwind JH, de Guevara LL, Papandreou C, Takayama T, Sanyal AJ, Yoon SK, Nakajima K, Lehr R, Heldner S, Lencioni R. Observational registry of sorafenib use in clinical practice across Child-Pugh subgroups: The GIDEON study. J Hepatol. 2016;65:1140-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 307] [Article Influence: 30.7] [Reference Citation Analysis (1)] |
| 14. | Pressiani T, Boni C, Rimassa L, Labianca R, Fagiuoli S, Salvagni S, Ferrari D, Cortesi E, Porta C, Mucciarini C, Latini L, Carnaghi C, Banzi M, Fanello S, De Giorgio M, Lutman FR, Torzilli G, Tommasini MA, Ceriani R, Covini G, Tronconi MC, Giordano L, Locopo N, Naimo S, Santoro A. Sorafenib in patients with Child-Pugh class A and B advanced hepatocellular carcinoma: a prospective feasibility analysis. Ann Oncol. 2013;24:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 128] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 15. | Wong H, Tang YF, Yao TJ, Chiu J, Leung R, Chan P, Cheung TT, Chan AC, Pang RW, Poon R, Fan ST, Yau T. The outcomes and safety of single-agent sorafenib in the treatment of elderly patients with advanced hepatocellular carcinoma (HCC). Oncologist. 2011;16:1721-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Morimoto M, Numata K, Kondo M, Hidaka H, Takada J, Shibuya A, Kobayashi S, Ohkawa S, Okuse C, Morita S, Taguri M, Tanaka K. Higher discontinuation and lower survival rates are likely in elderly Japanese patients with advanced hepatocellular carcinoma receiving sorafenib. Hepatol Res. 2011;41:296-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Cardoso H, Alves AM, Marques M, Vale AM, Pereira P, Macedo G. Hepatocellular Carcinoma Treatment With Sorafenib: Real-Life Evaluation of Prognostic Factors and a Practical Clue for Patient Management. GE Port J Gastroenterol. 2016;23:243-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li YW, China; Shomura M, Japan; Zhang XF, China S-Editor: Qu XL L-Editor: A P-Editor: Zhang XD