Published online Aug 15, 2022. doi: 10.4251/wjgo.v14.i8.1490
Peer-review started: March 28, 2022
First decision: May 11, 2022
Revised: May 23, 2022
Accepted: July 8, 2022
Article in press: July 8, 2022
Published online: August 15, 2022
Processing time: 135 Days and 5.2 Hours
The coronavirus disease 2019 (COVID-19) pandemic has caused detrimental effects on many aspects of healthcare practice. Screening programs for the commonest malignancies, namely colorectal cancer (CRC), breast cancer and cervical cancer have been discontinued or interrupted since the beginning of restriction measures aimed to limit transmission of the new coronavirus infection. Robust evidence exists in favour of the role of screening campaigns in reducing mortality from CRC. In fact, the majority of pre-malignant lesions of the colon and rectum can be diagnosed with colonoscopy and treated by endoscopic or surgical resection. Besides, colonoscopy screening allows the diagnosis of CRCs in their pre-clinical stage. Italy was one of the first European countries where a high level of COVID-19 infections and deaths was observed, and one of the first where lockdowns and strict measures were adopted to reduce the risk of COVID-19 diffusion among the population. A systematic review of the literature was performed, including the PubMed, Scopus, Web of Sciences, and Reference Citation Analysis databases, with the aim of critically evaluating the impact of the COVID-19 pandemic on CRC screening in Italy. We found that reduction of CRC screening activity surpassed 50% in most endoscopic units, with almost 600000 fewer CRC screening exams conducted in the first 5 mo of 2020 vs the same period of 2019. While the consequences of the discontinuation of endoscopy screening for the prognosis and mortality of CRC will be evident in the next few years, recent data confirm that CRC is currently treated at a more advanced stage than in the pre-COVID-19 era. Since delays in CRC prevention and early diagnosis may translate to increased CRC-specific mortality, world healthcare systems should adopt strategies to maintain the regularity of CRC screening during subsequent peaks of the COVID-19 pandemic, or future events that might hamper screening programs.
Core Tip: Screening is a key component of colorectal cancer control. As in the rest of the world, the coronavirus disease 2019 (COVID-19) emergency has interrupted the regular delivery of cancer screening services in Italy. As a consequence, significant delays in the diagnosis and treatment of malignant and pre-malignant lesions have occurred, with possible effects on disease prognosis. Screening activity has gradually resumed after the first wave of the pandemic. The healthcare system is called on to be prepared to prevent the potential suspension of new rounds of screening during the COVID-19 pandemic or future extraordinary events that might hamper screening programs.
- Citation: Fancellu A, Veneroni S, Santoru A, Meloni A, Sanna V, Ginesu GC, Deiana G, Paliogiannis P, Ninniri C, Perra T, Porcu A. How the COVID-19 pandemic has affected the colorectal cancer screening in Italy: A minireview. World J Gastrointest Oncol 2022; 14(8): 1490-1498
- URL: https://www.wjgnet.com/1948-5204/full/v14/i8/1490.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i8.1490
Colorectal cancer (CRC) is the third most commonly diagnosed cancer in males, the second in females, and the second leading cause of cancer death. Although incidence and mortality vary between countries, according to GLOBOCAN estimates, worldwide, the year 2020 saw 1.93 million new CRC cases diagnosed and 0.94 million deaths caused by CRC. The incidence of the disease is increasing in high-income countries, where it has traditionally been higher, as well as in middle- and low-income countries[1,2]. Robust evidence exists about the role of screening programs in reducing mortality from CRC. CRC screening includes a faecal occult blood test (FOBT) to detect blood in stool that may originate from a neoplastic or pre-neoplastic lesion, as well as colonoscopy. The latter allows either biopsy of early CRC or lesion removal at the time of the test.
In the last 2 years, population screening programs for the commonest cancers have been devastated by the spread of the coronavirus disease 2019 (COVID-19) pandemic[3-7]. In fact, screening has been deprioritized as healthcare resources have been reoriented toward treatment and prevention of the new coronavirus infection. Besides, many people have avoided hospitals and screening services for fear of contracting COVID-19.
Italy was one of the first countries in Europe to be affected by COVID-19, and measures taken to contain the spread of COVID-19 infection were more restrictive than those in other countries from the onset of the pandemic.
This review aims to critically evaluate the impact of the COVID-19 outbreak on CRC screening programs in Italy. We also discuss projected effects of delayed CRC diagnosis and treatment due to discontinuation of screening.
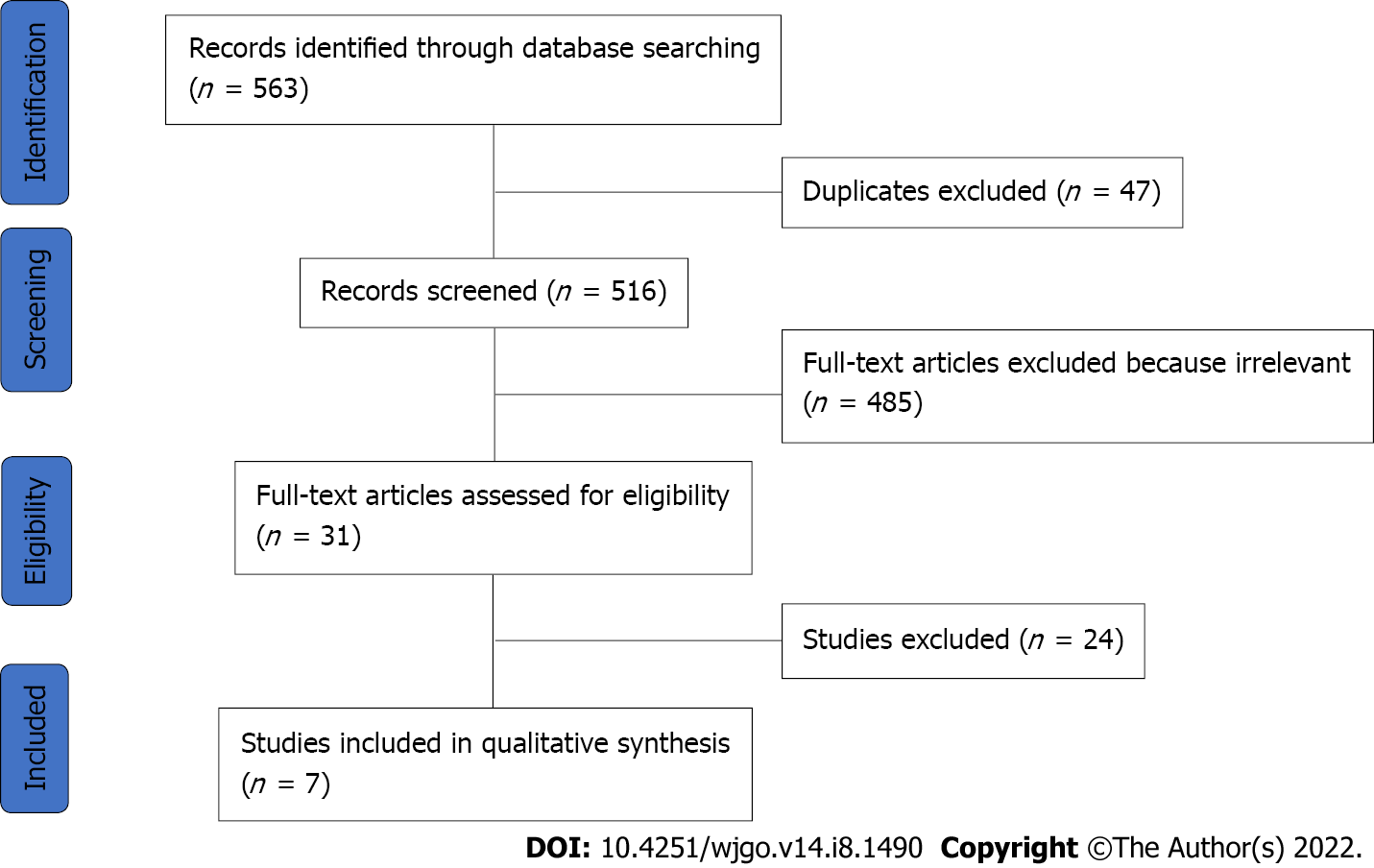
The present review focused on the literature covering the topic of CRC screening in Italy during the COVID-19 era. A systematic literature search using the PubMed, Scopus, Web of Science, and Reference Citation Analysis databases was conducted in February 2022. The following keywords were used and combined for the search: ‘colorectal’, ‘colon’, ‘rectal’, ‘cancer’, ‘carcinoma’, ‘malignancy’, ‘screening’, ‘screening program’, ‘COVID’, ‘COVID-19’, ‘SARS-CoV-2’, ‘coronavirus’, ‘Italy’ and ‘Italian’. Articles published in English from January 1, 2020 to January 31, 2022 were retrieved, screened and selected by two independent authors. Relevant data were extracted into a standardized data collection sheet by three authors. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses[8] guidelines were used to create a flowchart, which is shown in Figure 1.
The final inclusion criteria were observational retrospective studies, surveys or national and regional database-based studies that presented numerical analyses and comparisons of CRC screening results between the COVID-19 and pre-COVID-19 eras.
At the time of this review, a total of seven articles had been finally selected from a comprehensive number of 563 published studies[6,7,9-13]. The included articles are briefly summarized in Table 1. The outcomes were defined as percentages or overall proportions. Due to the nature of the work (minireview), no formal statistical analyses were conducted. Most of the studies (71%) focused their attention on the first semester of 2020, coinciding with the first COVID-19 burst in Italy[7,9,11-13]. The remaining two articles (29%) analysed a broader time frame of almost the entire year of 2020[6,10]. No articles were found concentrating on the 2021 situation, even though the pandemic was ongoing in its third and fourth waves. The studies ranged from single-unit experiences[7] to nation-wide surveys including all Italian regions[9] or evaluating more than 100 units across the country[12]. All of them focused on the reduction of endoscopic screening exams for CRC and the decrease in CRC new diagnoses in the analysed period with respect to the same temporal window in the previous years, namely 2018 and 2019.
| Ref. | Centers participating in the study | Time frame | Main conclusions |
| Armaroli et al[9] | 20 out of 21 regions involved | January-May 2020 vs January-May 2019 | (1) Cumulative delay of colorectal screening = 585.287 less exams (54.9%); (2) Esteemed delay of diagnosis of 3953 high-risk colonic adenomas and 611 colon cancer cases; and (3) Esteemed delay in diagnosis of 2.7 mo |
| Germana et al[10] | Veneto regional screening database | January-November 2020 vs same period in 2018-2019 | (1) 453877 people invited to undergo FOBT, within the regional colorectal cancer screening program, 115976 fewer than the previous two years (-20.4%), with an adherence rate that dropped from 65.2% to 54.2%; (2) Colonoscopies fell by 22.2% (67138 in 2020 ss. 86298 for the years 2018-2019); and (3) The reduction was of 13.1% for screening colonoscopies following a positive FOBT, and 24.9% for non-screening colonoscopies |
| Buscarini et al[6] | 49 units across Italy: 32 from the North (65.3%), 6 from the Center (12.2%), and 11 from the South (22.4%) | January-October 2020 vs same period in 2017, 2018 and 2019 | (1) CRC new diagnoses decreased by 11.9%; and (2) The 2019–2020 comparison showed fewer CRC diagnoses in the North (-13.7%), Center (-16.5%) and South (-4.1%) |
| Ferrara et al[11] | 7 Units in Northern-Central Italy | 11th-20th week of 2020 vs same period in 2018 and 2019 | Decrease of 46.6% of new colorectal cancer diagnosis with screening program (335 in 2018-2019 and only 178 in 2020) |
| De Vincentiis et al[7] | Single Unit audit | 11th-20th week of 2020 vs same period in 2018 and 2019 | CRC new diagnoses fell in 2020 by 62% compared with the average number in 2018 and 2019. CRC was identified as carrying a potentially important diagnostic delay |
| Maida et al[12] | 121 Units from 20 Italian regions | Survey between March 30, 2020 and April 7, 2020 | (1) 49 (46.7%) of 105 gastroenterology divisions had suspended their endoscopic screening program for colorectal cancer during the COVID-19 pandemic; (2) Overall, 10.7% Gastroenterology Divisions have been converted to Covid Units; and (3) Endoscopic procedures were limited to urgencies and oncology indications |
| Repici et al[13] | 41 EUs across Northern Italy | Survey between March 16, 2020 and March 21, 2020 | (1) 75%–99% reduction in activity in 28% of endoscopic units, a 50%–75% reduction in 9% of units, with only a single unit maintaining its workload unchanged; and (2) Most EUs limited their activity to urgent cases, including patients at high-risk of cancer |
According to the Italian Minister of Health, in the year 2020, about 43700 people were diagnosed with CRC (20282 women and 23420 men), and about 20000 died from the disease[14]. The 5-year survival rate for CRC in Italy is 65.3% in men and 65.3% in women[15]. CRC is one of the most preventable of all cancers, and regular screening is one of the most powerful preventive tools. Screening is the process of looking for cancer or precancerous lesions in people asymptomatic for the disease. The key usefulness of screening is that most CRCs develop following the so called ‘adenoma-carcinoma sequence’. Benign adenomatous polyps usually take several years to develop into CRC. With regular screening, most polyps can be detected and safely removed before they turn into forms of invasive carcinoma. Besides, screening can permit the diagnosis and treatment of early forms of CRC, thus increasing the possibility of a cure. The main aim of CRC screening is to decrease mortality from the disease[15-17]. There is evidence that the introduction of CRC screening programs in the early 2000s has substantially reduced mortality rates in European countries[18-21]. In Italy, CRC screening programs organized by the public health system cover the population of the entire country. In most regions, a FOBT by the immunochemical technique is offered every 2 years to all men and women aged 50–69 years, who are at the highest risk of developing the disease. In some regions, such as Piedmont, flexible sigmoidoscopy or FOBT are offered once in a time to people aged 58–69 years. The widespread use of FOBT in Italy has led to a progressive reduction in the incidence and mortality from CRC, the latter thanks to detection of CRC in its early stage. Data from 48 cancer registries from 17 Italian regions reported a reduction in the CRC incidence rate from 104.3 and 64.3 per 100.000 in the year 2003 to 89.9 and 58.4 per 100000 in 2014 in men and women, respectively. Besides, in the same time frame, mortality rates decreased from 41.1 to 39.2 per 100000 in men and from 24.6 to 23.1 per 100000 in women[15]. Data from randomized studies have demonstrated that both FOBT and flexible sigmoidoscopy have proven efficacy in reducing mortality from CRC by 22% and 28%, respectively[15,22]. In Italy, the most often used approach to CRC screening is to invite the target population by mail to undergo FOBT. Men and women with negative FOBT are recalled to repeat the test 2 years later. Those who do not respond to the first call are contacted by mail a second time within 6 mo. Patients with positive FOBT are contacted by phone to undergo a total or virtual colonoscopy (computed tomography colonography) in the case of incomplete colonoscopy[15]. When colonoscopy or sigmoidoscopy detects neoplasms, patients are directed to surgery or endoscopic surgery and enrolled in a follow-up program. Despite being a less tolerated and operator-dependent examination, colonoscopy leads to a complete exploration of the entire colorectal lumen and is much more sensitive than flexible sigmoidoscopy, based on indirect evidence and observational studies[23].
Italy was the first European nation to be affected by COVID-19. The first Italian cases of COVID-19 date back to January 30, 2020, when two tourists tested positive by nasopharyngeal COVID-19 Test in Rome. In February 2020, in the city of Codogno, located in the Northern region of Lombardy, a 38-year-old man was hospitalized for respiratory symptoms and tested positive; the day after, 60 cases of COVID in Codogno were diagnosed[24]. During this first COVID-19 wave, the Italian Healthcare Service was near collapse, registering in just 1 mo almost 40000 total cases and 3000 deaths (March 2020)[25]. From then onwards, Italy underwent three further pandemic waves, like most other countries in Europe. In that period, the development of vaccines contributed dramatically to proper management of the pandemic crisis[26]. As of March 14, 2022, 13402905 positive cases were registered in Italy, including 12242669 discharged and healed people, 156997 deaths and 1003239 active cases[27]. Italy ranks 9th in the world and 5th in Europe for the total number of cases, and 8th in the world and 3rd in Europe for the absolute number of deaths. Furthermore, Italy ranks 53rd in the world for total cases per capita and 25th for total deaths per capita[26].
The DECOR-19 DElayed CRC care during the COVID-19 Pandemic was a global perspective from an international survey, where the highest number of respondents (1051) were from Italy. Of note, endoscopic procedures for CRC were the diagnostic techniques most affected by the COVID-19 emergency (73.7% of respondents). CRC surgery was delayed in 58.3% of institutions. For 90% of respondents, the delay was 5–8 wk beyond the normal wait time and for the remaining 10%, more than 8 wk[28].
The Italian National Screening Observatory reported on the accumulated delay experienced by organized screening programs up to May 2020. In the first 5 mo of 2020 vs the same period of 2019, 585287 fewer CRC screening exams were conducted, accounting for a 54.9% decrease[9]. Based on these numbers, an estimated 1168 CRCs and 6667 advanced adenomas would have been missed in the period from January 2020 to September 2020[29].
A survey was conducted by the National Centre for Screening Monitoring on cervical, breast and CRC screening activities conducted in 2020. Screening tests for CRC decreased by 45.5% in 2020 compared with 2019, with an estimated 1299 CRC cases going undiagnosed. Interestingly, participation in CRC screening programs decreased by 20%[30].
In a study investigating the Cancer Diagnostic Delay in Northern and Central Italy During the 2020 lockdown, a comparison was made among the number of first pathologic diagnoses of malignancy made from weeks 11 to 20 (April and May) of 2018, 2019 and 2020 at seven pathology units serving secondary care hospitals in Northern-Central Italy. A consistent decrease of 46.6% in new CRC cases diagnosed by screening programs (335 in 2018–2019 and only 178 in 2020) was observed[11].
The number of people who responded to invitations for FOBT screening in the region of Veneto in 2020 was about 16000 less than in the previous 2 years, with an adherence rate that decreased from 65.2% to 54.2%. Colonoscopies fell by 22.2% (67138 in 2020 vs 86298 for the period 2018–2019); the rate reached its lowest in April (-70.4%). There was a 13.1% reduction in screening colonoscopies following a positive FOBT and a 24.9% reduction in non-screening colonoscopies (P < 0.001)[10].
In a national survey, CRC diagnoses decreased by 11.9% from 2019 to 2020. A comparison between 2019 and 2020 showed fewer CRC diagnoses in the North (-13.7%), Center (-16.5%) and South (-4.1%)[6]. The authors performed an audit to evaluate the impact of COVID-19 pandemic-related delays in the diagnosis of major cancers at a Pathology Unit of a Secondary Care Hospital Network in Italy[7]. Cancer diagnoses fell in 2020 by 39% compared with the average number recorded in 2018 and 2019, and CRC was the tumour type with the greatest decrease.
A multicentric study evaluated the impact of the 2019 outbreak on 41 Italian endoscopic units. In 27 (65.9%) units, endoscopists were relocated to other hospital departments. In 31 (75.6%) units, nurses were relocated to other hospital departments. Most endoscopy units limited their activity to urgent cases, also including patients at high risk of cancer. After the COVID-19 outbreak, 39 endoscopy units (95.1%) continued to perform urgent procedures, 39 (95.1%) continued inpatient procedures and 28 (68.3%) continued screening colonoscopies for CRC. In quantitative terms, this corresponded to a 75%–99% reduction in activity in 28% of endoscopic units and to a 50%–75% reduction in 9% of units, with only a single unit maintaining its workload unchanged. Finally, most EUs limited their activity to urgent cases, including patients at high risk of cancer[13]. Examining Gastroenterology Divisions in Italy, a national survey that analysed data between March and April 2020 underscored that 46.7% of gastroenterology divisions had suspended their endoscopic screening programs for CRC during the COVID-19 pandemic, 10.7% of Gastroenterology Divisions had been converted to COVID units, and endoscopic procedures had been limited to urgencies and oncology cases in 96.2% of units[12].
Similar data were reported from countries outside Italy. In South Australia, the total number of colonoscopies decreased by 51.1% from 2019 to 2020[31]. In the United Kingdom, endoscopic cancer detection was reduced by 58% overall and by 72% for CRC in particular during the period impacted by COVID (March–May 2020)[32]. In France, roughly 250000 fewer colonoscopy preparations were dispensed during the first 6 mo of the COVID-19 pandemic[33]. In Hong Kong of China, the mean number of lower endoscopies performed per week decreased by 51.0% after the beginning of the pandemic[34]. The number of obstructive CRCs in Japan has increased during the COVID-19 pandemic, as a possible consequence of CRC screening discontinuation[35].
This review demonstrates the remarkable impact of the pandemic on endoscopic services in Italy. Interruption and discontinuation of CRC screening inevitably translated into a substantial and concerning reduction in CRC detection. It is commonly believed that screening delays beyond 4–6 mo would significantly increase advanced CRC cases and, if lasting beyond 12 mo, mortality as well[15]. In patients with CRC, 3–10-year survival is lower if treatment is started > 90 d from diagnosis, and similar data are reported for other cancers[36]. The ideal timing of resection of colon cancer specifically has been estimated to be between 3 and 6 wk from diagnosis, which is unlikely to be achieved during the COVID-19 outbreak[37]. In a study where patients who underwent surgery for CRC in the pre-COVID-19 era (October 2019–February 2020) were compared to those who did so after the end of the second wave (January 2021–May 2021), an increase in T4 tumours with higher preoperative levels of CEA and CA 19-9 was observed. These tumours required more extensive lymph node dissection. The authors speculated that this finding could be attributed to the reduced number of colonoscopies performed during the lockdown, as well as to patients’ fears of potential infections in the hospital setting[37].
A survey by the Italian Federation of the Digestive Diseases Societies found that in gastroenterology units, 11.9% fewer CRC cases were diagnosed between January 1, 2020 and October 31, 2020, compared with the same period in 2019[6].
Surgical oncology services around the world suffered a remarkable reduction in activity, resulting in a doubling of waiting lists as a result of delays in the screening and diagnosis of CRC due to the restrictions imposed by the pandemic.
A study was designed to evaluate the effects of COVID-19-related delays in CRC screening in 20 hospitals of Northern Italy by comparing 1755 patients who underwent CRC surgery in 2019 vs 1481 in 2020. The results showed that CRC s in 2020 (compared to 2019) were more likely to be symptomatic [OR: 1.36 (95%CI: 1.09-1.69)], to be clinical stage T4 [OR: 1.38 (95%CI: 1.03-1.85)] and to have multiple liver metastases [OR: 2.21 (95%CI: 1.24-3.94)], although they were not more likely to be associated with surgical complications [OR: 0.79 (95%CI: 0.68-0.93)][38]. In particular, locally advanced disease, as well as the presence of CRC metastases to the liver, are definite prognostic factors in patients affected by CRC.
Another study evaluated the impact of the COVID-19 emergency on elective oncological surgical activity in 54 surgical units in Italy, including 11 colorectal units. Among the latter, 9 (82%) experienced a reduction of their surgical activity by 60%, with an expected prolongation of 5 wk between multidisciplinary meetings and surgery[39].
In the absence of proper catch-up campaigns aiming to recuperate those who missed their scheduled screening, the prognosis of patients with CRC could worsen. In fact, the long-term effects of the delay in CRC diagnosis due to interruption of screening activity could result in a rise in late-stage CRC cases and eventually in an undesirable loss of life years due to the lack of appropriate treatments for these patients[40].
Based on a procedural model using real-world data, in Italy a significant increase in deaths (12%) can be estimated at 5 years after a delay of longer than 12 mo in access to colonoscopy. In particular, in a study comparing baseline (0–3 mo), moderate (7–12 mo) and long (> 12 mo) delays, a significant increase in advanced CRC (from 26% to 29% and 33%, respectively, was seen. Thus, the authors have estimated a significant increase in the total number of deaths (12.0%) when moving from a 0–3-mo to a > 12-mo delay (P < 0.005) and a significant change in the mortality distribution by stage from baseline to > 12 mo (P < 0.001)[41,42].
The results of our review confirm that the COVID-19 emergency has caused detrimental effects on CRC screening programs in Italy, similarly to what occurred in other counties on all continents. In most hospitals and territorial healthcare services, a time-limited suspension of CRC screening services was observed. At the time of writing, the situation is different from that observed at the beginning of the COVID-19 crisis. Indeed, advances in the treatment of patients affected by COVID-19, as well as prevention with massive vaccine campaigns, has significantly decreased the growth in the total number cases and rates of hospitalization. As a consequence, screening activity has now resumed in many Italian regions. Nonetheless, sporadic COVID-19 outbreaks due to the diffusion of new variants of the virus continue to modify the activities of healthcare services, and the duration of the effects of the COVID-19 pandemic on social life and healthcare in general is difficult to predict. The delayed diagnoses of CRC cases attributable to screening discontinuation is expected to result in an increase in advanced cancer cases—and possibly deaths—in the coming years. It is of the utmost importance that healthcare services of countries around the world develop reliable policies to maintain standard CRC screening activity in the presence of new pandemic outbreaks or similar extraordinary events.
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 68628] [Article Influence: 13725.6] [Reference Citation Analysis (201)] |
| 2. | Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14:101174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 687] [Cited by in RCA: 1582] [Article Influence: 316.4] [Reference Citation Analysis (7)] |
| 3. | Alkatout I, Biebl M, Momenimovahed Z, Giovannucci E, Hadavandsiri F, Salehiniya H, Allahqoli L. Has COVID-19 Affected Cancer Screening Programs? Front Oncol. 2021;11:675038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 4. | Mayo M, Potugari B, Bzeih R, Scheidel C, Carrera C, Shellenberger RA. Cancer Screening During the COVID-19 Pandemic: A Systematic Review and Meta-analysis. Mayo Clin Proc Innov Qual Outcomes. 2021;5:1109-1117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 5. | Fancellu A, Sanna V, Rubino C, Ariu ML, Piredda C, Piana GQ, Cottu P, Spanu A, Cossu A, Deiana G, Porcu A. The COVID-19 Outbreak May Be Associated to a Reduced Level of Care for Breast Cancer. A Comparative Study with the Pre-COVID Era in an Italian Breast Unit. Healthcare (Basel). 2020;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Buscarini E, Benedetti A, Monica F, Pasquale L, Buttitta F, Cameletti M, Ferrari C, Ricciardiello L; FISMAD: the FISMAD-ALERT Survey Group. Changes in digestive cancer diagnosis during the SARS-CoV-2 pandemic in Italy: A nationwide survey. Dig Liver Dis. 2021;53:682-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | De Vincentiis L, Carr RA, Mariani MP, Ferrara G. Cancer diagnostic rates during the 2020 'lockdown', due to COVID-19 pandemic, compared with the 2018-2019: an audit study from cellular pathology. J Clin Pathol. 2021;74:187-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 106] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 8. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65-W94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3566] [Cited by in RCA: 4430] [Article Influence: 260.6] [Reference Citation Analysis (0)] |
| 9. | Armaroli P, Battagello J, Battisti F, Giubilato P, Mantellini P, Sassoli P. Rapporto sui ritardi accumulati alla fine di maggio 2020 dai programmi di screening Italiani e sulla velocità della ripartenza. Edizioni Cantagalli. 2020;1-8. [DOI] [Full Text] |
| 10. | Germana B, Bellio S, Barbiellini Amidei C, Capodaglio G, Avossa F, Narne E, Pitter G, Fedeli U, Zorzi M, Rosa–Rizzotto E, Pantalena M, Saia M; Colorectal Screening Units V. R.. PC.01.11 Impact of COVID-19 Pandemic on Colonoscopy and surgical interventions for Colorectal cancer in Veneto region. Dig Liver Dis. 2021;53:S92. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Ferrara G, De Vincentiis L, Ambrosini-Spaltro A, Barbareschi M, Bertolini V, Contato E, Crivelli F, Feyles E, Mariani MP, Morelli L, Orvieto E, Pacella E, Venturino E, Saragoni L. Cancer Diagnostic Delay in Northern and Central Italy During the 2020 Lockdown Due to the Coronavirus Disease 2019 Pandemic. Am J Clin Pathol. 2021;155:64-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 12. | Maida M, Sferrazza S, Savarino E, Ricciardiello L, Repici A, Morisco F, Furnari M, Fuccio L, Morreale GC, Vitello A, Burra P, Marchi S, Annibale B, Benedetti A, Alvaro D, Ianiro G; Italian Society of Gastroenterology (SIGE). Impact of the COVID-19 pandemic on Gastroenterology Divisions in Italy: A national survey. Dig Liver Dis. 2020;52:808-815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 13. | Repici A, Pace F, Gabbiadini R, Colombo M, Hassan C, Dinelli M; ITALIAN GI-COVID19 Working Group. Endoscopy Units and the Coronavirus Disease 2019 Outbreak: A Multicenter Experience From Italy. Gastroenterology. 2020;159:363-366.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 14. | I Numeri Del Cancro in Italia. Presentazione dei Gruppi di Lavoro. [cited 10 March 2022]. Available from: https://www.salute.gov.it/imgs/C_17_notizie_5681_0_file.pdf. |
| 15. | AIOM. Tumori Del Colon. [cited 10 March 2022]. Available from: https://www.aiom.it/Linee-guida-aiom-2021-tumori-del-colon/. |
| 16. | Schüz J, Espina C, Villain P, Herrero R, Leon ME, Minozzi S, Romieu I, Segnan N, Wardle J, Wiseman M, Belardelli F, Bettcher D, Cavalli F, Galea G, Lenoir G, Martin-Moreno JM, Nicula FA, Olsen JH, Patnick J, Primic-Zakelj M, Puska P, van Leeuwen FE, Wiestler O, Zatonski W; Working Groups of Scientific Experts. European Code against Cancer 4th Edition: 12 ways to reduce your cancer risk. Cancer Epidemiol. 2015;39 Suppl 1:S1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 181] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 17. | Lieberman D, Ladabaum U, Cruz-Correa M, Ginsburg C, Inadomi JM, Kim LS, Giardiello FM, Wender RC. Screening for Colorectal Cancer and Evolving Issues for Physicians and Patients: A Review. JAMA. 2016;316:2135-2145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 18. | Atkin WS, Cuzick J, Northover JM, Whynes DK. Prevention of colorectal cancer by once-only sigmoidoscopy. Lancet. 1993;341:736-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 240] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Regge D, Iussich G, Segnan N, Correale L, Hassan C, Arrigoni A, Asnaghi R, Bestagini P, Bulighin G, Cassinis MC, Ederle A, Ferraris A, Galatola G, Gallo T, Gandini G, Garretti L, Martina MC, Molinar D, Montemezzi S, Morra L, Motton M, Occhipinti P, Pinali L, Soardi GA, Senore C. Comparing CT colonography and flexible sigmoidoscopy: a randomised trial within a population-based screening program. Gut. 2017;66:1434-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D, Robertson DJ. Colorectal Cancer Screening: Recommendations for Physicians and Patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2017;112:1016-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 508] [Article Influence: 56.4] [Reference Citation Analysis (0)] |
| 21. | Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, Ederer F. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328:1365-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2183] [Cited by in RCA: 2187] [Article Influence: 66.3] [Reference Citation Analysis (1)] |
| 22. | Zorzi M, Dal Maso L, Francisci S, Buzzoni C, Rugge M, Guzzinati S; AIRTUM Working Group. Trends of colorectal cancer incidence and mortality rates from 2003 to 2014 in Italy. Tumori. 2019;105:417-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Holme Ø, Bretthauer M, Fretheim A, Odgaard-Jensen J, Hoff G. Flexible sigmoidoscopy vs faecal occult blood testing for colorectal cancer screening in asymptomatic individuals. Cochrane Database Syst Rev. 2013;CD009259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 24. | Indolfi C, Spaccarotella C. The Outbreak of COVID-19 in Italy: Fighting the Pandemic. JACC Case Rep. 2020;2:1414-1418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 25. | Armocida B, Formenti B, Ussai S, Palestra F, Missoni E. The Italian health system and the COVID-19 challenge. Lancet Public Health. 2020;5:e253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 297] [Cited by in RCA: 325] [Article Influence: 54.2] [Reference Citation Analysis (0)] |
| 26. | WHO. Tracking SARS-CoV-2 variants. [cited 10 March 2022]. Available from: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/. |
| 27. | Dipartimento della Protezione Civile. COVID-19 Italia-Monitoraggio della situazione. 2021; 45: 383-384 [cited 10 March 2022]. Available from: https://www.sciencedirect.com/science/article/pii/S0210569120301820?via%3Dihub#section-cited-by. |
| 28. | [cited 10 March 2022]. Available from: http://opendatadpc.maps.arcgis.com/apps/opsdashboard/index.html#/b0c68bce2cce478eaac82fe38d4138b1. |
| 29. | Santoro GA, Grossi U, Murad-Regadas S, Nunoo-Mensah JW, Mellgren A, Di Tanna GL, Gallo G, Tsang C, Wexner SD; DECOR-19 Collaborative Group. DElayed COloRectal cancer care during COVID-19 Pandemic (DECOR-19): Global perspective from an international survey. Surgery. 2021;169:796-807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 30. | Rapporto sui ritardi accumulati dai programmi di screening Italiani in seguito alla pandemia da Covid-19. Secondo rapporto al 30 Settembre 2020. [cited 31 March 2021]. Available from: https://www.osservatorionazionalescreening.it/sites/default/files/allegati/Rapporto%20ripartenza%20-%20settembre%202020_0.pdf. |
| 31. | Battisti F, Falini P, Gorini G, Sassoli de Bianchi P, Armaroli P, Giubilato P, Giorgi Rossi P, Zorzi M, Battagello J, Senore C, Zappa M, Mantellini P. Cancer screening programs in Italy during the COVID-19 pandemic: an update of a nationwide survey on activity volumes and delayed diagnoses. Ann Ist Super Sanita. 2022;58:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 32. | Wassie MM, Agaciak M, Cock C, Bampton P, Young GP, Symonds EL. The impact of coronavirus disease 2019 on surveillance colonoscopies in South Australia. JGH Open. 2021;5:486-492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Rutter MD, Brookes M, Lee TJ, Rogers P, Sharp L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut. 2021;70:537-543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 209] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 34. | Meyer A, Drouin J, Zureik M, Weill A, Dray-Spira R. Colonoscopy in France during the COVID-19 pandemic. Int J Colorectal Dis. 2021;36:1073-1075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 35. | Lui TKL, Leung K, Guo CG, Tsui VWM, Wu JT, Leung WK. Impacts of the Coronavirus 2019 Pandemic on Gastrointestinal Endoscopy Volume and Diagnosis of Gastric and Colorectal Cancers: A Population-Based Study. Gastroenterology. 2020;159:1164-1166.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 36. | Mizuno R, Ganeko R, Takeuchi G, Mimura K, Nakahara H, Hashimoto K, Hinami J, Shimomatsuya T, Kubota Y. The number of obstructive colorectal cancers in Japan has increased during the COVID-19 pandemic: A retrospective single-center cohort study. Ann Med Surg (Lond). 2020;60:675-679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 37. | Pellino G, Spinelli A. How Coronavirus Disease 2019 Outbreak Is Impacting Colorectal Cancer Patients in Italy: A Long Shadow Beyond Infection. Dis Colon Rectum. 2020;63:720-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 38. | Peltrini R, Imperatore N, Di Nuzzo MM, D'Ambra M, Bracale U, Corcione F. Effects of the first and second wave of the COVID-19 pandemic on patients with colorectal cancer: what has really changed in the outcomes? Br J Surg. 2021;108:e365-e366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Rottoli M, Pellino G, Spinelli A, Flacco ME, Manzoli L, Morino M, Pucciarelli S, Jovine E, Abu Hilal M, Rosati R, Ferrero A, Pietrabissa A, Guaglio M, de Manzini N, Pilati P, Cassinotti E, Pignata G, Goletti O, Opocher E, Danelli P, Sampietro G, Olmi S, Portolani N, Poggioli G; COVID-CRC Collaborative Group. Impact of COVID-19 on the oncological outcomes of colorectal cancer surgery in northern Italy in 2019 and 2020: multicentre comparative cohort study. BJS Open. 2022;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 40. | Torzilli G, Viganò L, Galvanin J, Castoro C, Quagliuolo V, Spinelli A, Zerbi A, Donadon M, Montorsi M; COVID-SURGE-ITA group. A Snapshot of Elective Oncological Surgery in Italy During COVID-19 Emergency: Pearls, Pitfalls, and Perspectives. Ann Surg. 2020;272:e112-e117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 41. | Kopel J, Ristic B, Brower GL, Goyal H. Global Impact of COVID-19 on Colorectal Cancer Screening: Current Insights and Future Directions. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 42. | Ricciardiello L, Ferrari C, Cameletti M, Gaianill F, Buttitta F, Bazzoli F, Luigi de'Angelis G, Malesci A, Laghi L. Impact of SARS-CoV-2 Pandemic on Colorectal Cancer Screening Delay: Effect on Stage Shift and Increased Mortality. Clin Gastroenterol Hepatol. 2021;19:1410-1417.e9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Delgado-Gallegos JL, Mexico; El Sayed S, Egypt; Osorno JF, Colombia S-Editor: Fan JR L-Editor: A P-Editor: Fan JR