Copyright
©The Author(s) 2022.
World J Gastrointest Oncol. Mar 15, 2022; 14(3): 690-702
Published online Mar 15, 2022. doi: 10.4251/wjgo.v14.i3.690
Published online Mar 15, 2022. doi: 10.4251/wjgo.v14.i3.690
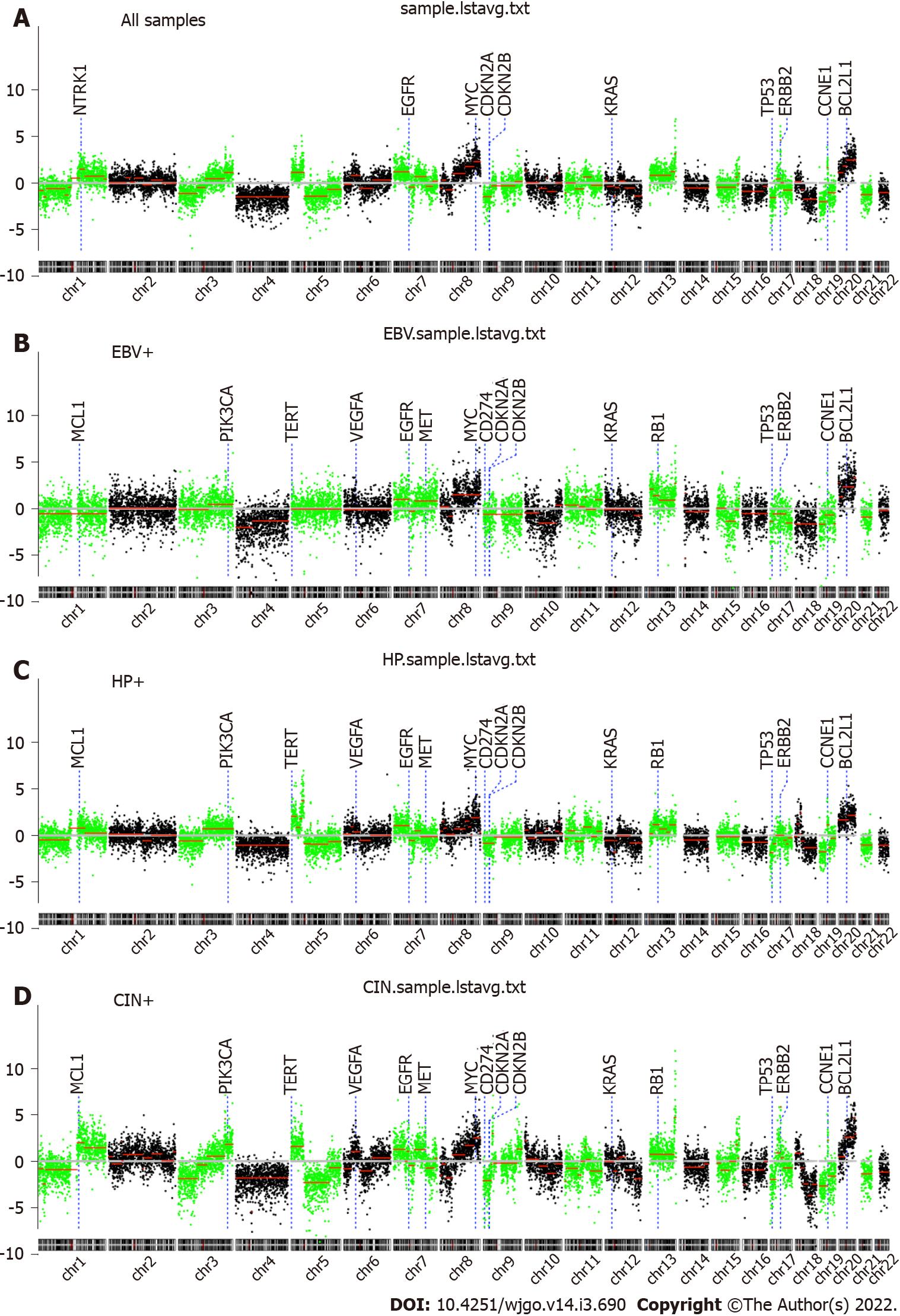
Figure 1 The chromosomal landscape.
A-D: The whole-genome overview for all (A), EBV-positive (B), Helicobacter pylori-positive (C), and chromosomal unstable (D) gastric cancers. Cancer-relevant genes are also indicated. CIN: Chromosomal instability; HP: Helicobacter pylori; EBV: Epstein-Barr virus.
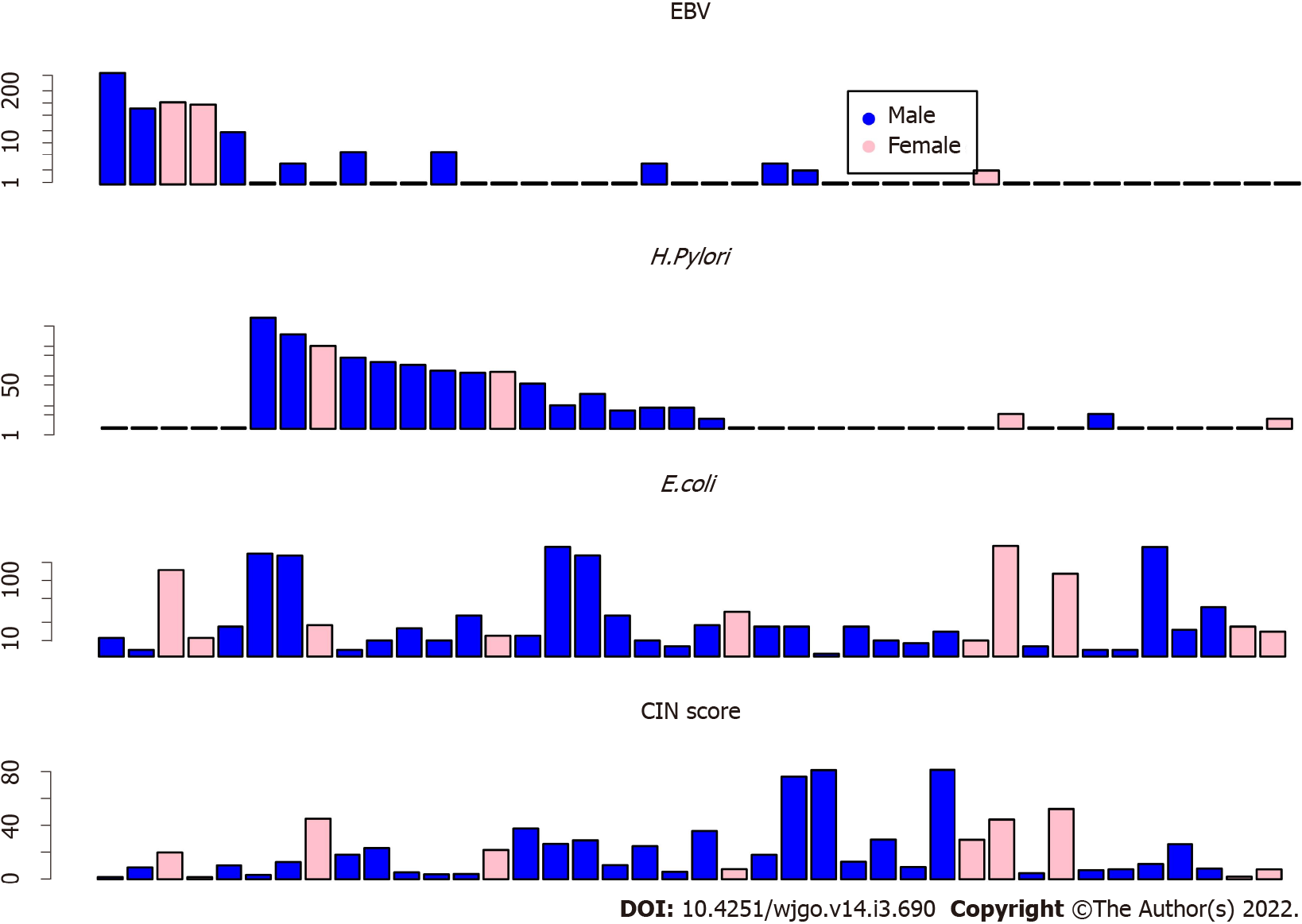
Figure 2 The bar plot of microbiome read counts and chromosomal instability scores.
Read counts of Epstein-Barr virus (top), Helicobacter pylori (second row), and Escherichia coli (third row) are shown in the bar plots. Chromosomal instability scores for each sample are shown at the bottom. CIN: Chromosomal instability; H. pylori: Helicobacter pylori; EBV: Epstein-Barr virus; E. coli: Escherichia coli.
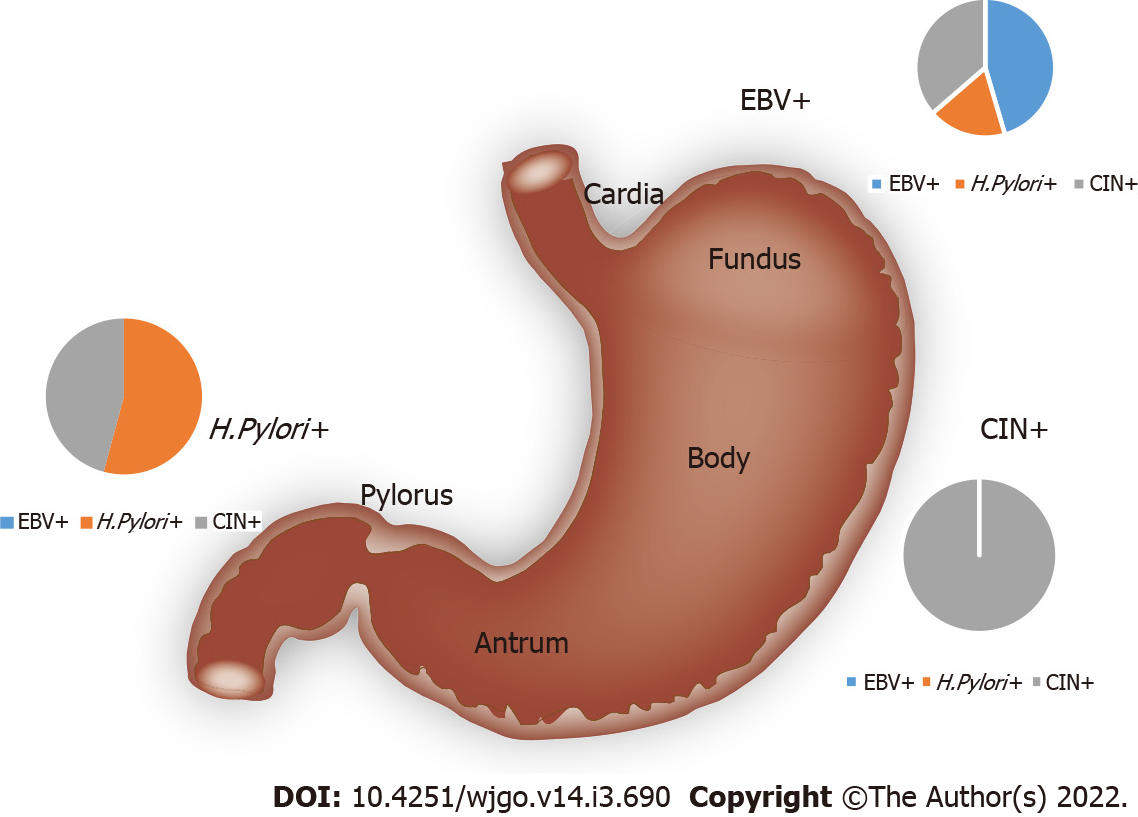
Figure 3 The gastric cancer subtypes.
Epstein-Barr virus enrichment is associated with tumors in the gastric cardia and fundus. Helicobacter pylori enrichment associated with tumors in the pylorus and antrum. Tumors with elevated genomic instability can be observed in any location. CIN: Chromosomal instability; H. pylori: Helicobacter pylori; EBV: Epstein-Barr virus.
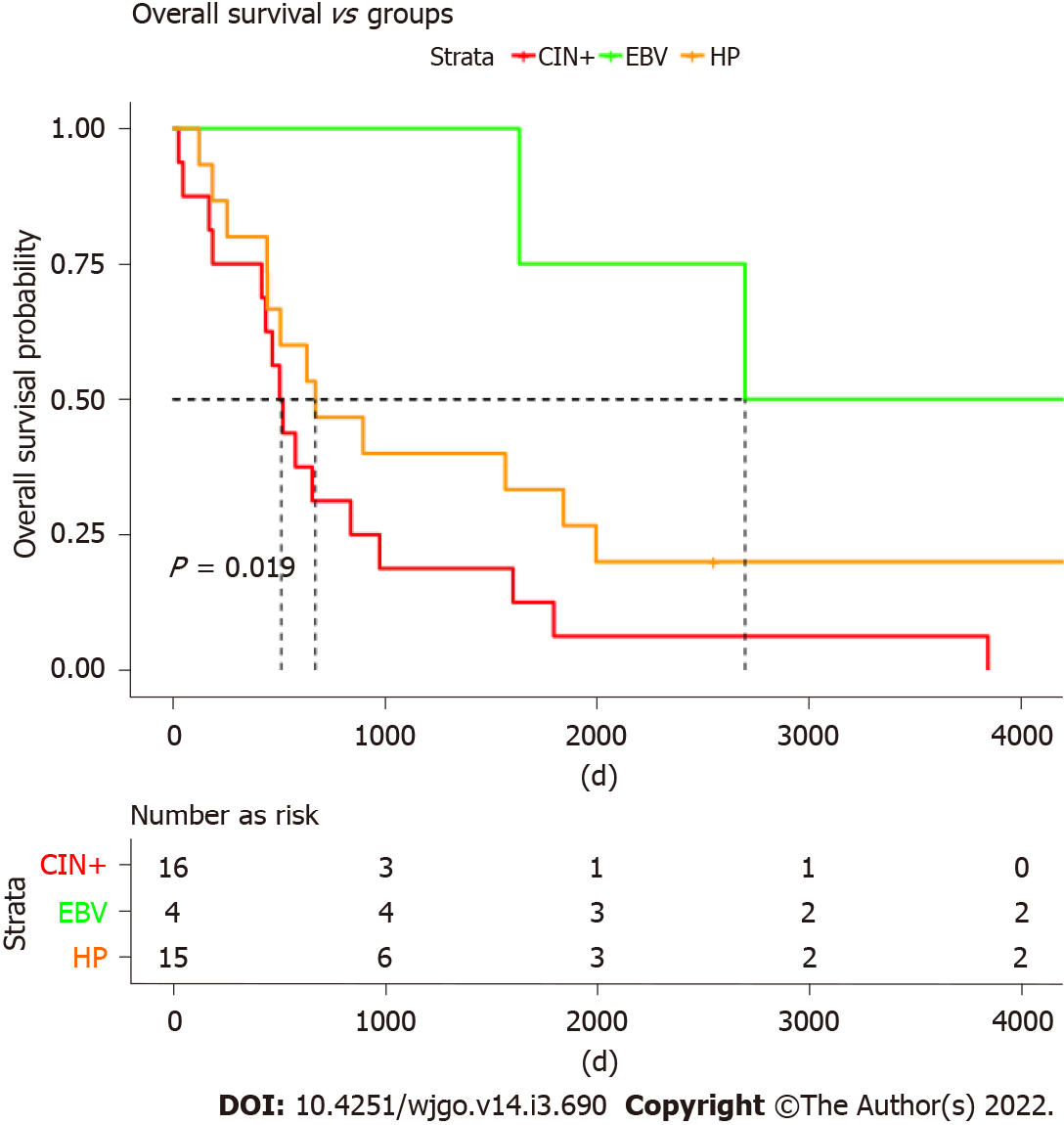
Figure 4 High chromosomal instability associated with worse overall survival.
Epstein-Barr virus-positive tumors present with the best overall survival; chromosomal instability (CIN)+ patients presented with the worst survival. Patients with Helicobacter pylori infections also showed worse survival as compared to Epstein-Barr virus ones but tended to be better than CIN+ patients. CIN: Chromosomal instability; HP: Helicobacter pylori; EBV: Epstein-Barr virus.
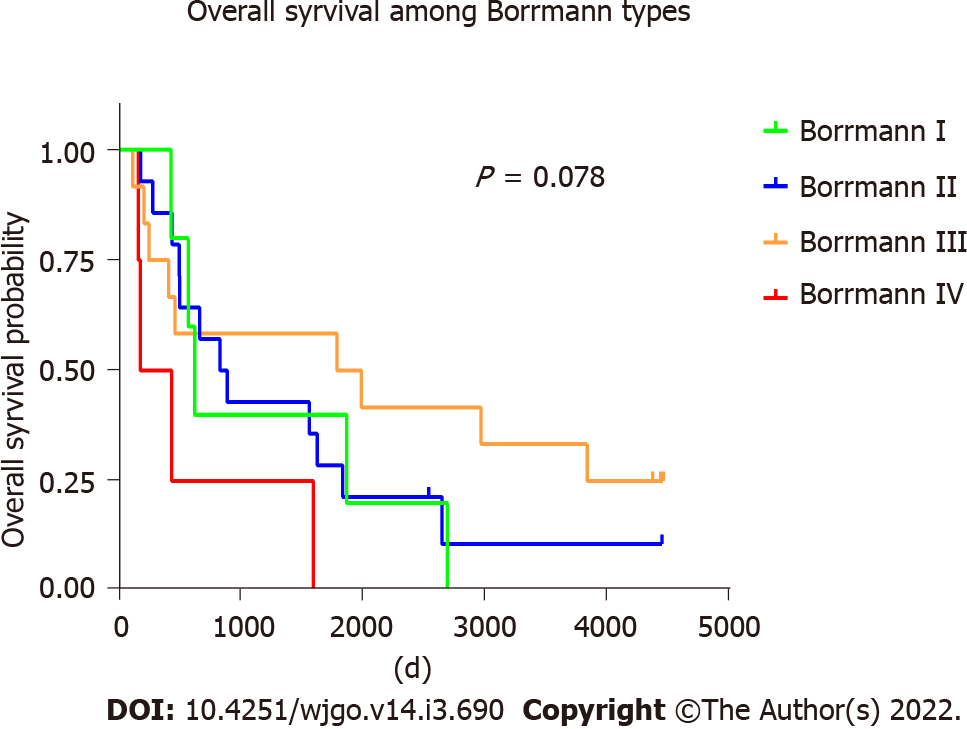
Figure 5 Overall survival among Borrman types of gastric cancer.
- Citation: Ye LP, Mao XL, Zhou XB, Wang Y, Xu SW, He SQ, Qian ZL, Zhang XG, Zhai LJ, Peng JB, Gu BB, Jin XX, Song YQ, Li SW. Cost-effective low-coverage whole-genome sequencing assay for the risk stratification of gastric cancer. World J Gastrointest Oncol 2022; 14(3): 690-702
- URL: https://www.wjgnet.com/1948-5204/full/v14/i3/690.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i3.690