©The Author(s) 2019.
World J Gastrointest Oncol. Nov 15, 2019; 11(11): 1054-1064
Published online Nov 15, 2019. doi: 10.4251/wjgo.v11.i11.1054
Published online Nov 15, 2019. doi: 10.4251/wjgo.v11.i11.1054
Figure 1 Endoscopic ultrasound of a muscularis propria tumor in the gastric fundus.
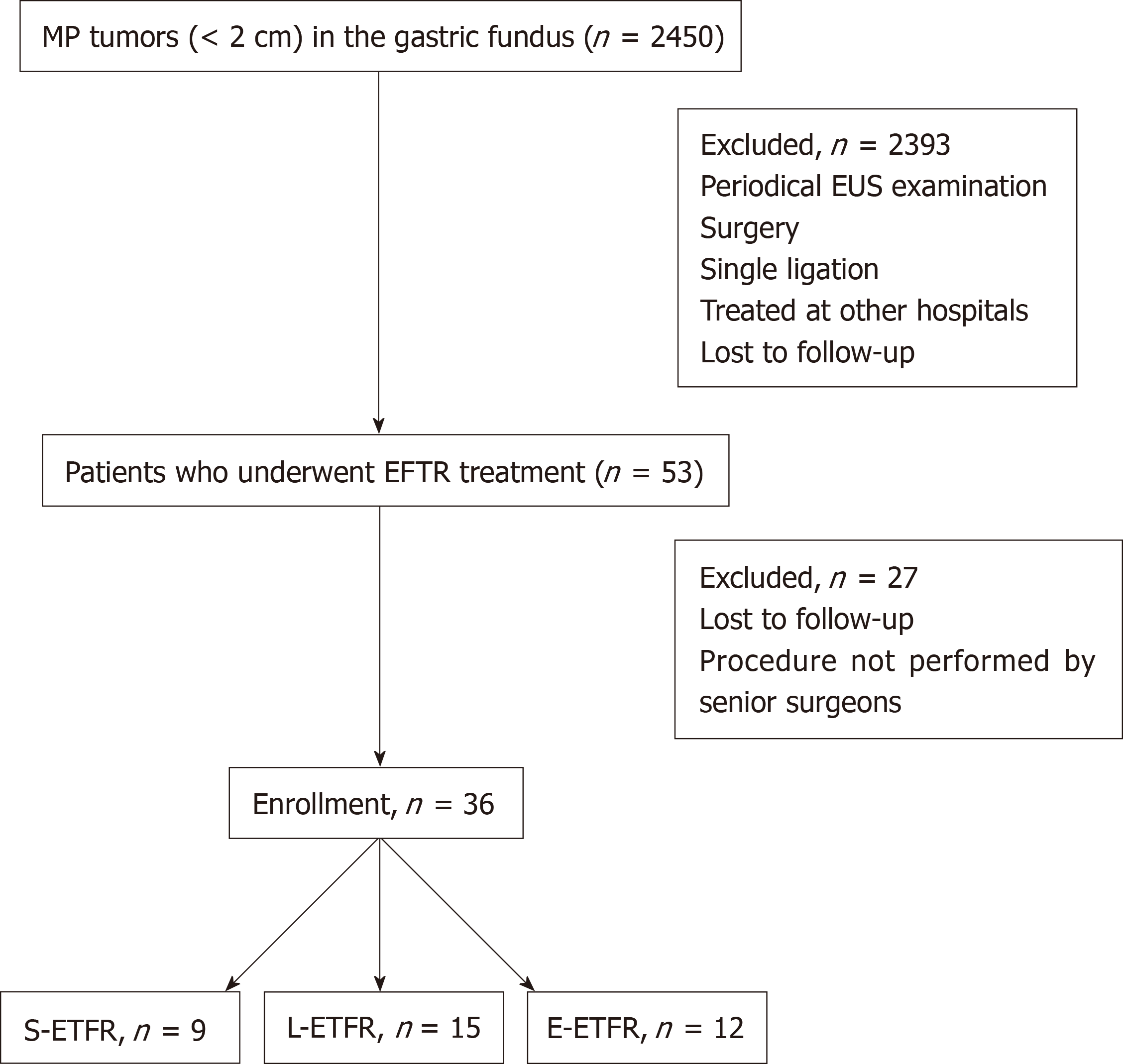
Figure 2 Flow diagram for screening and grouping of study subjects.
L-EFTR: Ligation-assisted endoscopic full-thickness resection; S-EFTR: Snare-assisted endoscopic full-thickness resection; E-EFTR: Endoscopic submucosal dissection-assisted endoscopic full-thickness resection; MP: Muscularis propria.
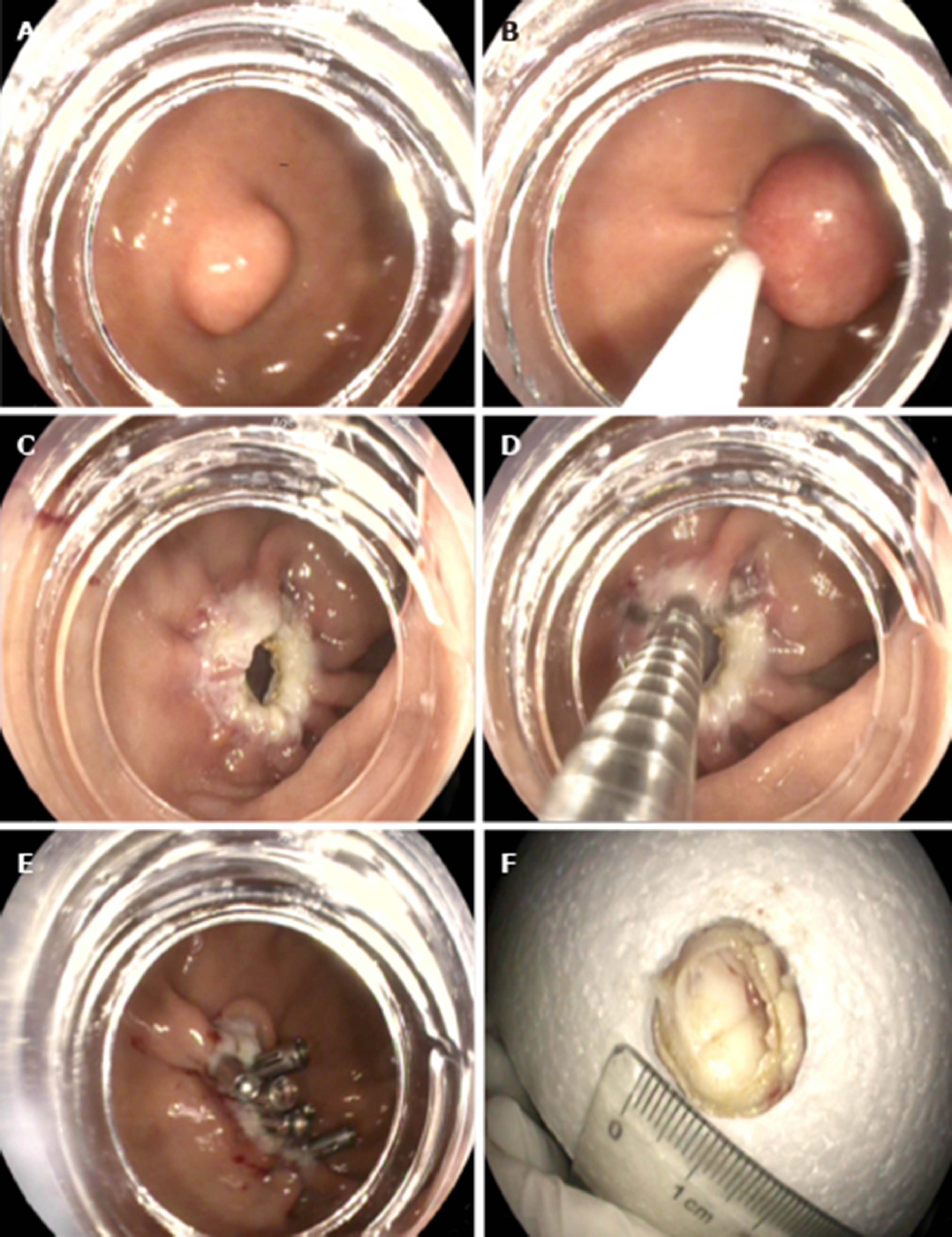
Figure 3 Snare-assisted endoscopic full-thickness resection.
A: Muscularis propria (MP) tumor in the gastric fundus; B: MP tumor grasped by a snare; C: A gastric wall defect during snare-assisted endoscopic full-thickness resection; D: Clip application during defect closure; E: Gastric wall defect closure using clips; F: The resected MP tumor.
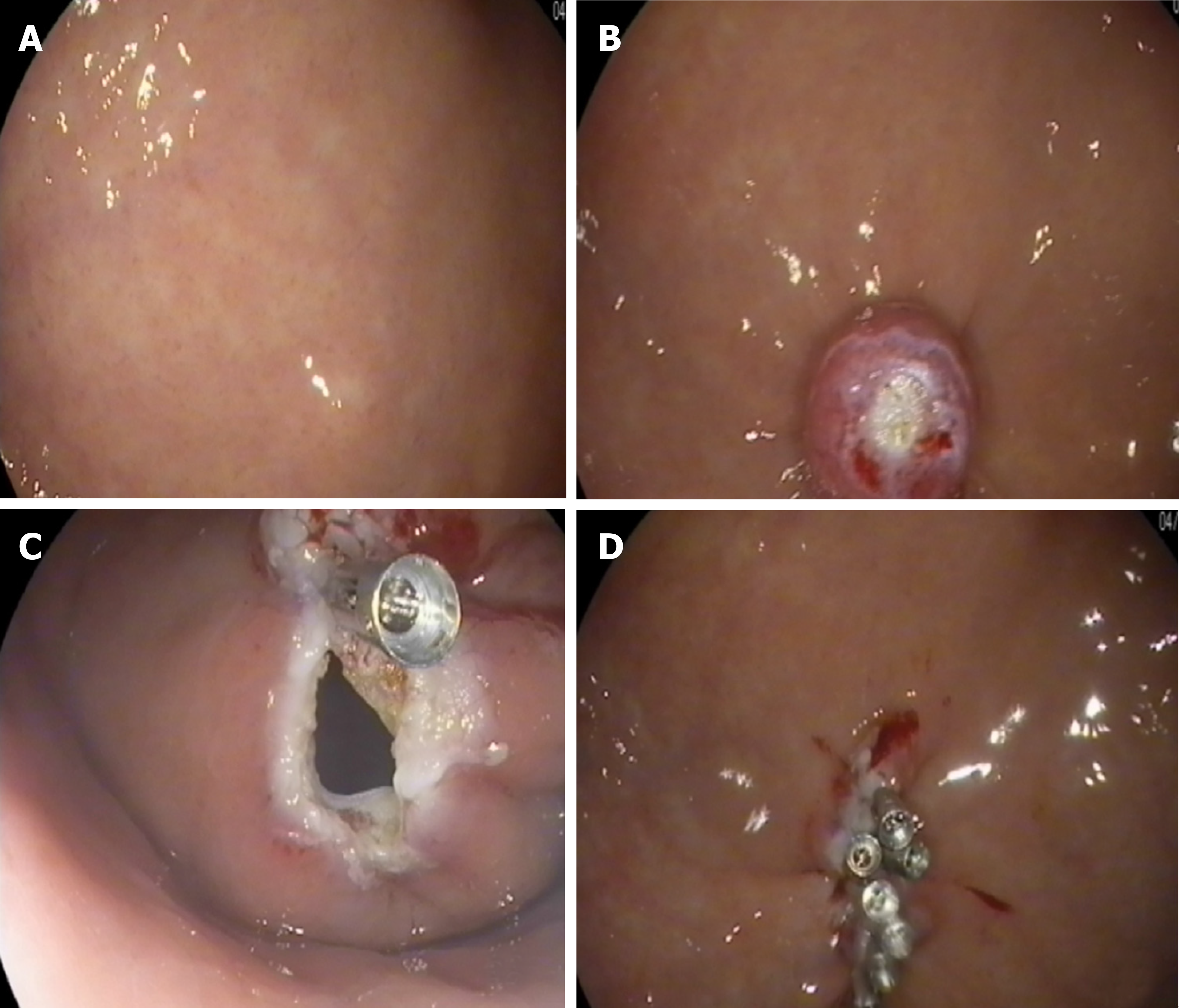
Figure 4 Ligation-assisted endoscopic full-thickness resection.
A: Muscularis propria (MP) tumor in the gastric fundus; B: MP tumor ligation by the band; C: A gastric wall defect during ligation-assisted endoscopic full-thickness resection; D: Gastric wall defect closure using clips.
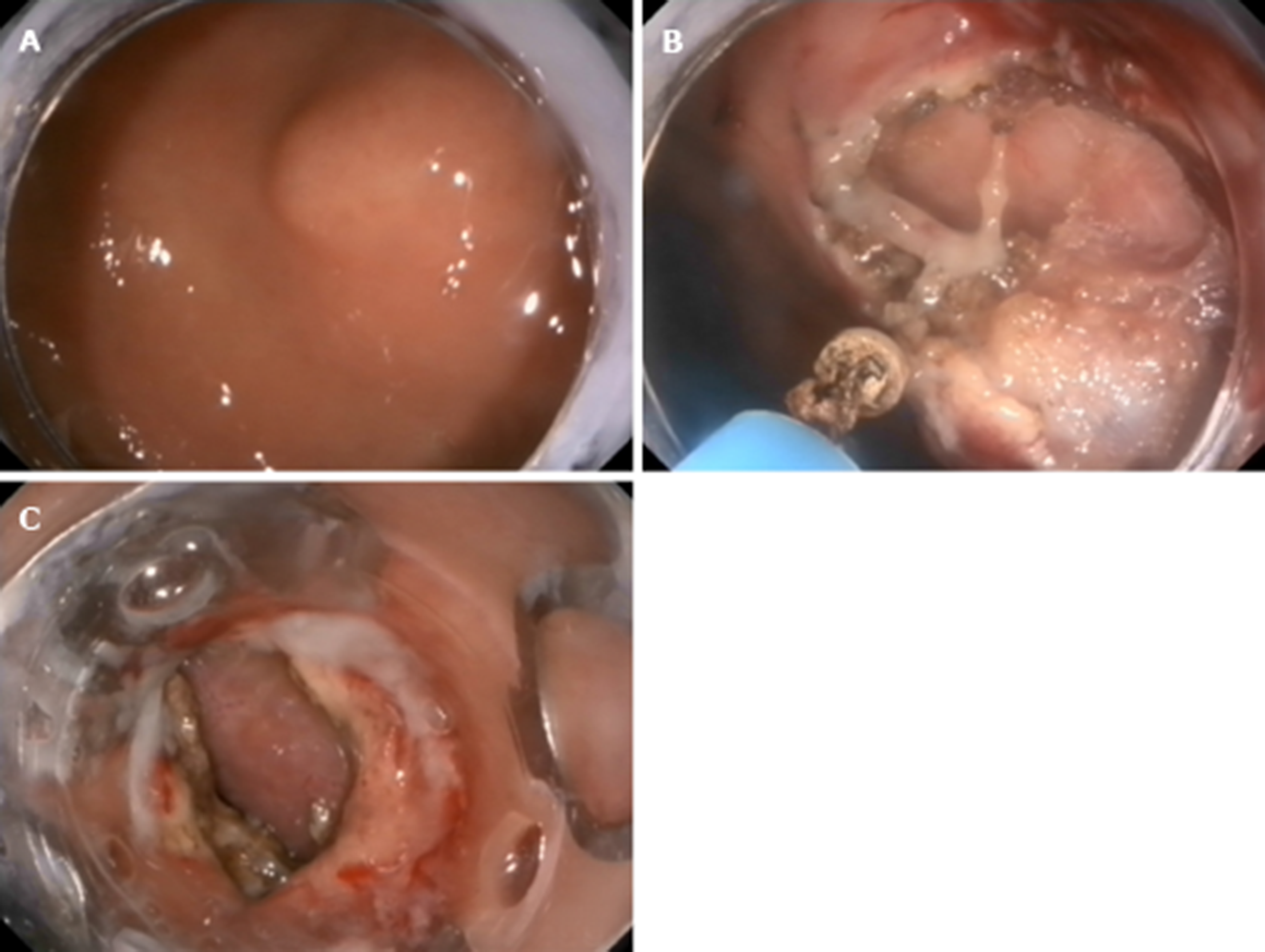
Figure 5 Endoscopic submucosal dissection-assisted endoscopic full-thickness resection.
A: Muscularis propria (MP) tumor in the gastric fundus; B: MP tumor resection using an IT knife; C: Application of the over-the-scope-clip device for gastric wall defect closure.
- Citation: Ge N, Hu JL, Yang F, Yang F, Sun SY. Endoscopic full-thickness resection for treating small tumors originating from the muscularis propria in the gastric fundus: An improvement in technique over 15 years. World J Gastrointest Oncol 2019; 11(11): 1054-1064
- URL: https://www.wjgnet.com/1948-5204/full/v11/i11/1054.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v11.i11.1054