Published online Nov 16, 2017. doi: 10.4253/wjge.v9.i11.552
Peer-review started: February 6, 2017
First decision: March 16, 2017
Revised: April 25, 2017
Accepted: July 22, 2017
Article in press: July 24, 2017
Published online: November 16, 2017
Processing time: 291 Days and 9.1 Hours
To perform a systematic review and meta-analysis to assess the safety of conscious sedation in patients with obstructive sleep apnea (OSA).
A comprehensive electronic search of MEDLINE and EMBASE was performed from inception until March 1, 2015. In an effort to include unpublished data, abstracts from prior gastroenterological society meetings as well as other reference sources were interrogated. After study selection, two authors utilizing a standardized data extraction form collected the data independently. Any disagreements between authors were resolved by consensus among four authors. The methodological quality was assessed using the Newcastle Ottawa tool for observational studies. The primary variables of interest included incidence of hypoxia, hypotension, tachycardia, and bradycardia. Continuous data were summarized as odds ratio (OR) and 95%CI and pooled using generic inverse variance under the random-effects model. Heterogeneity between pooled studies was assessed using the I2 statistic.
Initial search of MEDLINE and EMBASE identified 357 citations. A search of meeting abstracts did not yield any relevant citations. After systematic review and exclusion consensus meetings, seven studies met the a priori determined inclusion criteria. The overall methodological quality of included studies ranged from moderate to low. No significant differences between OSA patients and controls were identified among any of the study variables: Incidence of hypoxia (7 studies, 3005 patients; OR = 1.11; 95%CI: 0.73-1.11; P = 0.47; I2 = 0%), incidence of hypotension (4 studies, 2125 patients; OR = 1.10; 95%CI: 0.75-1.60; P = 0.63; I2 = 0%), incidence of tachycardia (3 studies, 2030 patients; OR = 0.94; 95%CI: 0.53-1.65; P = 0.28; I2 = 21%), and incidence of bradycardia (3 studies, 2030 patients; OR = 0.88; 95%CI: 0.63-1.22; P = 0.59; I2 = 0%).
OSA is not a significant risk factor for cardiopulmonary complications in patients undergoing endoscopic procedures with conscious sedation.
Core tip: Patients with obstructive sleep apnea (OSA) often receive monitored anesthesia care in lieu of conscious sedation due to a perceived elevated risk of complications. However, prior studies have failed to note any clinically significant variations in cardiopulmonary parameters in OSA patients when compared to controls during endoscopy but studies have been underpowered due to small sample sizes. The objective was to perform a systematic review and meta-analysis to assess the safety of conscious sedation in patients with OSA. This meta-analysis showed OSA is not a significant risk factor for cardiopulmonary complications in patients undergoing endoscopic procedures with conscious sedation.
- Citation: Andrade CM, Patel B, Vellanki M, Kumar A, Vidyarthi G. Safety of gastrointestinal endoscopy with conscious sedation in obstructive sleep apnea. World J Gastrointest Endosc 2017; 9(11): 552-557
- URL: https://www.wjgnet.com/1948-5190/full/v9/i11/552.htm
- DOI: https://dx.doi.org/10.4253/wjge.v9.i11.552
Obstructive sleep apnea (OSA) is an increasingly common disorder. Because of a presumed elevated risk, endoscopic evaluation in patients with OSA may be delayed, denied or achieved at a higher level of care resulting in substantial healthcare expenses. In the general population, adverse events during endoscopy are rare with an approximate adverse event rate of 0.1% and 0.2% for upper gastrointestinal and lower gastrointestinal procedures respectively[1-4]. Non-significant variations in cardiopulmonary parameters are usually noted during routine endoscopy and have been well studied[5-7]. Several published studies, including a recently reported prospective study evaluating the risk of cardiopulmonary complications in patients with OSA undergoing endoscopy with conscious sedation have not supported the need for extra precaution[8]. We recently published a prospective analysis in the veteran population undergoing upper and lower endoscopy which did not find any significant cardio-pulmonary variation in control and OSA patients[8].
Despite their comparable findings, these conclusions are limited by small sample sizes in conjunction with low adverse event rates. No systematic reviews or meta-analyses have been performed on this topic to date. The present study aims to systematically review the literature and perform a meta-analysis of all selected published and unpublished data meeting search criteria on patients with OSA undergoing endoscopic procedures.
A comprehensive electronic search of MEDLINE and EMBASE was performed from inception until March 1, 2015. A total of 119 MEDLINE references were identified using the following search strategy: (apnea) OR “sleep apnea”) OR sleep apnea) OR obstructive sleep apnea) OR “obstructive sleep apnea”) OR sleep disordered breathing) OR “sleep disordered breathing”) AND (sedation) OR conscious sedation) OR “conscious sedation”) OR moderate sedation) OR “moderate sedation”) AND endoscopy. A total of 238 EMBASE references were identified using the following strategy: Endoscopy AND (Apnea OR (sleep AND disordered AND breathing) OR “sleep disordered breathing” OR “obstructive sleep apnea” OR “sleep apnea” OR (sleep AND apnea) OR (obstructive AND sleep AND apnea) AND (Sedation OR “conscious sedation” OR (conscious AND sedation) OR “moderate sedation” OR (moderate AND sedation) AND human. Two authors evaluated the combined 357 candidate studies independently. Studies performed on patients with obstructive sleep apnea undergoing endoscopy with conscious sedation and at least one the following variables of interest were considered for inclusion: Incidence of hypoxia, hypotension, tachycardia, and bradycardia.
Two authors extracted all data independently utilizing a standardized data extraction form. Once the data was entered into a dataset, a random data check was performed for accuracy. All disagreements between authors were resolved by consensus with a third author. Data were collected on study and patient characteristics, OSA groups, use of conscious sedation and the incidences of hypoxia, hypotension, tachycardia, and bradycardia when available. The methodological quality was assessed using the Newcastle Ottawa tool for observational studies[9]. The primary variables of interest included incidence of hypoxia, hypotension, tachycardia, and bradycardia. The systematic review was performed and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[10].
Continuous data were summarized as odds ratio (OR) and 95%CI and pooled using generic inverse variance under the random-effects model. Heterogeneity between pooled studies was assessed using I2 statistic and categorized as low (< 30%), moderate (30%-50%), or high (> 50%)[11]. All analyses were performed using Review Manager 5.1 software[12].
The statistical methods of this study were performed and reviewed by a biomedical statistician, Ambuj Kumar, MD, MPH from Comparative Effectiveness Research, Morsani College of Medicine, University of South Florida, Tampa, FL, United States.
A comprehensive search of MEDLINE and EMBASE identified 357 eligible citations. In an effort to capture unpublished data, conference abstracts from the last 3 meetings (2013-2015) of the American College of Gastroenterology and Digestive Disease Week were also reviewed. No studies were identified to meet inclusion criteria. The following sites were also interrogated for possible study inclusion: ClinicalTrials.gov, Roche clinical trial protocol registry (http://www.roche-trials.com), Novartis clinical trials database (http://www.novctrd.com), Australian New Zealand Clinical Trials Registry (ANZCTR), and the metaRegister of Controlled Trials. No additional studies were identified for inclusion.
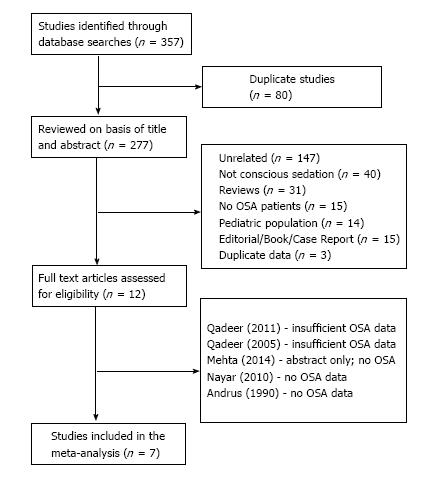
After systematic review and exclusion consensus meetings, seven studies met the a priori determined inclusion criteria (Figure 1). None of the references from the included studies yielded additional studies eligible for inclusion. The overall methodological quality of the included studies ranged from moderate to low as assessed by the Newcastle Ottawa tool for observational studies[9].
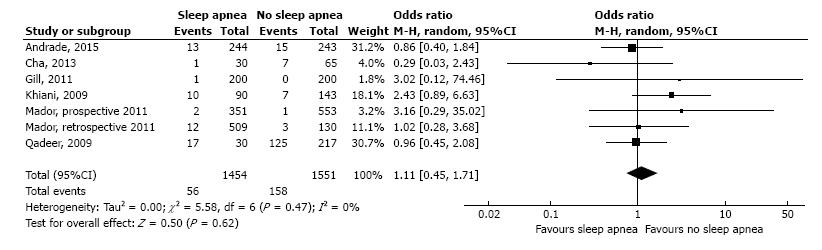
Seven studies identified for inclusion contained data on the incidence of hypoxia. A total of 3005 patients were included for analysis. No significant differences between OSA patients and controls were identified with regards to the incidence of hypoxia (OR = 1.11; 95%CI: 0.73-1.11; P = 0.47, Figure 2). The heterogeneity among the studies was low (I2 = 0%).
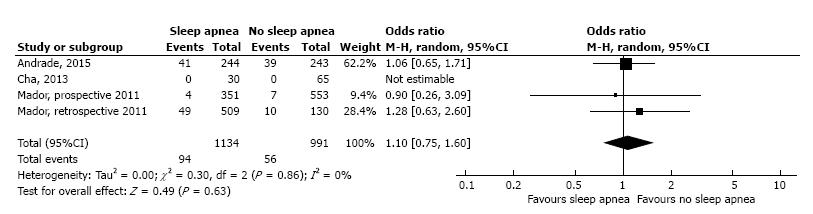
Four studies identified for inclusion contained data on the incidence of hypotension. A total of 2125 patients were included for analysis. No significant differences between OSA patients and controls were identified with regards to the incidence of hypotension (OR = 1.10; 95%CI: 0.75-1.60; P = 0.63, Figure 3). The heterogeneity among the studies was low (I2 = 0%).
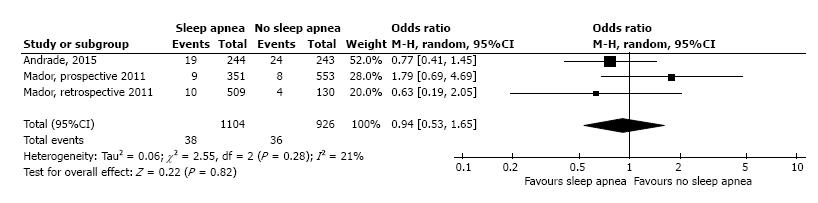
Three studies identified for inclusion contained data on the incidence of tachycardia. A total of 2030 patients were included for analysis. No significant differences between OSA patients and controls were identified with regards to the incidence of tachycardia (OR = 0.94; 95%CI: 0.53-1.65; P = 0.28, Figure 4). The heterogeneity among the studies was low (I2 = 21%).
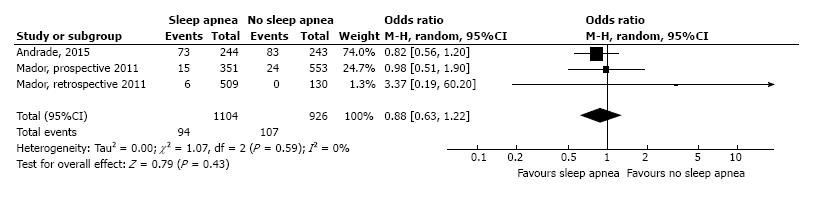
Three studies identified for inclusion contained data on the incidence of bradycardia. A total of 2030 patients were included for analysis. No significant differences between OSA patients and controls were identified with regards to the incidence of bradycardia (OR = 0.88; 95%CI: 0.63-1.22; P = 0.59, Figure 5). The heterogeneity among the studies was low (I2 = 0%).
OSA is a growing problem in the United States especially among the veteran population. Moderate to severe OSA is estimated to affect approximately 13% of men and 6% women between the ages of 30-70[13]. Per the ASGE sedation guidelines, patient with OSA are considered to be at a higher risk regarding sedation-related cardiopulmonary complications in relation to upper and lower endoscopy[14]. These patients are routinely recommended MAC anesthesia for endoscopic evaluation. Cardiopulmonary complications are the most feared unfavorable events among patients with OSA including episodes of tachycardia, bradycardia, hypotension, and hypoxia[5-7]. It is believed that OSA patients especially tend to have poor respiratory drive and effort which can be exacerbated by sedation[15,16]. Contrary to that belief, our meta-analysis and review does not show any significant difference in regards to hypoxia in OSA patients. It is also well studied that sedation tend to lower overall mean blood pressure. When looking at cardio-circulatory parameters including bradycardia, tachycardia and hypotension, our review failed to show any significant difference in regards to those parameters. Therefore, in patients undergoing endoscopy with conscious sedation, OSA does not seem to be a clinically important risk factor for unfavorable outcomes. In short, significant differences between OSA patients and controls were not identified among any of the study variables: Incidence of hypoxia, hypotension, tachycardia or bradycardia. This is in correlation with regards to the recent publication from our institution highlighting the cardiopulmonary parameters in the OSA and non-OSA patients[8]. OSA patients are perceived as high risk for endoscopy and are offered monitored anesthesia care routinely although this meta-analysis suggests otherwise. Moving forward, endoscopists should be cognizant that OSA does not predispose patients to higher risk compared to non OSA patients. In addition, using conscious sedation for OSA patients may reduce overall healthcare burden with cost saving measures as MAC anesthesia care has not necessarily shown any overall reduction in adverse events. A major limitation of the study includes the overall methodological quality of the included studies ranged from moderate to low. Further, for patients undergoing endoscopic procedures with conscious sedation, OSA does not appear to be a significant risk factor for cardiopulmonary complications. Future prospective studies must be conducted to evaluate the cost effectiveness and safety of endoscopy with MAC in the OSA population.
Patients with obstructive sleep apnea (OSA) often receive monitored anesthesia care in lieu of conscious sedation due to a perceived elevated risk of complications. However, prior studies have failed to note any clinically significant variations in cardiopulmonary parameters in OSA patients when compared to controls during endoscopy but studies have been underpowered due to small sample sizes. The authors aim was to perform a systematic review and meta-analysis to assess the safety of conscious sedation in patients with obstructive sleep apnea (OSA).
This meta-analysis has demonstrated that OSA does not appear to be a significant risk factor for cardiopulmonary complications in patients undergoing endoscopy. Future prospective studies are needed to look at both the safety and cost-effectiveness of endoscopy with MAC in the OSA population.
This meta-analysis showed OSA is not a significant risk factor for cardiopulmonary complications in patients undergoing endoscopic procedures with conscious sedation, which has typically been the standard of care. These results further open the consideration of endoscopy without MAC in patients with OSA but future prospective studies are needed to look at both the safety and cost-effectiveness of endoscopy with MAC in the OSA population.
These findings can be considered by endoscopists when performing endoscopy with MAC in the OSA population in assessing their risk for procedural cardiopulmonary complications.
Conscious sedation - The use of a sedative during a medical procedure that allows for a quick recovery; OSA - A sleep disorder that causes breathing to start and stop during sleep due to airway obstruction during sleep; Endoscopy - A procedure which uses an endoscope, or a long flexible tube with a camera to examine the upper GI tract.
The author gave a systematic review and meta-analysis about the safety of gastrointestinal endoscopy with conscious sedation in patients with OSA. The manuscript was concise and helpful for us to be cognizant that OSA does not appear to be a clinically significant risk factor for adverse outcomes in patients undergoing endoscopy with conscious sedation.
| 1. | Faigel DO, Baron TH, Goldstein JL, Hirota WK, Jacobson BC, Johanson JF, Leighton JA, Mallery JS, Peterson KA, Waring JP. Guidelines for the use of deep sedation and anesthesia for GI endoscopy. Gastrointest Endosc. 2002;56:613-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 129] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Rabeneck L, Paszat LF, Hilsden RJ, Saskin R, Leddin D, Grunfeld E, Wai E, Goldwasser M, Sutradhar R, Stukel TA. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology. 2008;135:1899-1906, 1906.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 359] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 3. | Anderson ML, Pasha TM, Leighton JA. Endoscopic perforation of the colon: lessons from a 10-year study. Am J Gastroenterol. 2000;95:3418-3422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 280] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Levin TR, Zhao W, Conell C, Seeff LC, Manninen DL, Shapiro JA, Schulman J. Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med. 2006;145:880-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 396] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 5. | Osinaike BB, Akere A, Olajumoke TO, Oyebamiji EO. Cardiorespiratory changes during upper gastrointestinal endoscopy. Afr Health Sci. 2007;7:115-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Hart R, Classen M. Complications of diagnostic gastrointestinal endoscopy. Endoscopy. 1990;22:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 142] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Agostoni M, Fanti L, Gemma M, Pasculli N, Beretta L, Testoni PA. Adverse events during monitored anesthesia care for GI endoscopy: an 8-year experience. Gastrointest Endosc. 2011;74:266-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 125] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Andrade CM, Patel B, Gill J, Amodeo D, Kulkarni P, Goldsmith S, Bachman B, Geerken R, Klein M, Anderson W. Safety of Gastrointestinal Endoscopy With Conscious Sedation in Patients With and Without Obstructive Sleep Apnea. J Clin Gastroenterol. 2016;50:198-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Wells G, Shea B, O’Connell J, Robertson J. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. 2011; Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. |
| 10. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9247] [Cited by in RCA: 8997] [Article Influence: 529.2] [Reference Citation Analysis (0)] |
| 11. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 26981] [Article Influence: 1124.2] [Reference Citation Analysis (0)] |
| 12. | Review Manager (RevMan) [Windows]. Version [5.1]. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration 2014; . |
| 13. | Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2961] [Cited by in RCA: 3204] [Article Influence: 246.5] [Reference Citation Analysis (0)] |
| 14. | Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy, Lichtenstein DR, Jagannath S, Baron TH, Anderson MA, Banerjee S, Dominitz JA, Fanelli RD, Gan SI, Harrison ME, Ikenberry SO, Shen B, Stewart L, Khan K, Vargo JJ. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008;68:815-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 280] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 15. | Arrowsmith JB, Gerstman BB, Fleischer DE, Benjamin SB. Results from the American Society for Gastrointestinal Endoscopy/U.S. Food and Drug Administration collaborative study on complication rates and drug use during gastrointestinal endoscopy. Gastrointest Endosc. 1991;37:421-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 321] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 16. | McCloy R, Nagengast F, Fried M, Rohde H, Froehlich F, Whitwam J. Conscious sedation for endoscopy. Eur J Gastroenterol Hepatol. 1996;8:1233-1240. [PubMed] |
| 17. | Cha JM, Jeun JW, Pack KM, Lee JI, Joo KR, Shin HP, Shin WC. Risk of sedation for diagnostic esophagogastroduodenoscopy in obstructive sleep apnea patients. World J Gastroenterol. 2013;19:4745-4751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Gill J, Vidyarthi G, Kulkarni P, Anderson W, Boyd W. Safety of conscious sedation in patients with sleep apnea in a veteran population. South Med J. 2011;104:185-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Khiani VS, Salah W, Maimone S, Cummings L, Chak A. Sedation during endoscopy for patients at risk of obstructive sleep apnea. Gastrointest Endosc. 2009;70:1116-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Mador MJ, Abo Khamis M, Nag N, Mreyoud A, Jallu S, Mehboob S. Does sleep apnea increase the risk of cardiorespiratory complications during endoscopy procedures? Sleep Breath. 2011;15:393-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Mador MJ, Nadler J, Mreyoud A, Khadka G, Gottumukkala VA, Abo-Khamis M, Mehboob S. Do patients at risk of sleep apnea have an increased risk of cardio-respiratory complications during endoscopy procedures? Sleep Breath. 2012;16:609-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Qadeer MA, Rocio Lopez A, Dumot JA, Vargo JJ. Risk factors for hypoxemia during ambulatory gastrointestinal endoscopy in ASA I-II patients. Dig Dis Sci. 2009;54:1035-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 88] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 23. | Qadeer MA, Vargo JJ, Khandwala F, Lopez R, Zuccaro G. Propofol versus traditional sedative agents for gastrointestinal endoscopy: a meta-analysis. Clin Gastroenterol Hepatol. 2005;3:1049-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 173] [Article Influence: 8.2] [Reference Citation Analysis (1)] |
| 24. | Mehta PP, Kochhar G, Kalra S, Maurer W, Tetzlaff J, Singh G, Lopez R, Sanaka MR, Vargo JJ. Can a validated sleep apnea scoring system predict cardiopulmonary events using propofol sedation for routine EGD or colonoscopy? A prospective cohort study. Gastrointest Endosc. 2014;79:436-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Nayar DS, Guthrie WG, Goodman A, Lee Y, Feuerman M, Scheinberg L, Gress FG. Comparison of propofol deep sedation versus moderate sedation during endosonography. Dig Dis Sci. 2010;55:2537-2544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lu IC, Yu B S- Editor: Gong ZM L- Editor: A E- Editor: Lu YJ