Published online Jul 10, 2015. doi: 10.4253/wjge.v7.i8.814
Peer-review started: August 26, 2014
First decision: November 27, 2014
Revised: April 15, 2015
Accepted: April 27, 2015
Article in press: April 29, 2015
Published online: July 10, 2015
Processing time: 322 Days and 22.4 Hours
The work of Muhe and Mouret in the late 1980s, paved the way for mainstream laparoscopic procedures and it rapidly became the mainstream method for many intra-abdominal procedures. Natural orifice transluminal surgery (NOTES) and Laparo-endoscopic single-site surgery (LESS) are very exciting new modalities in the field of minimally invasive surgery which work for further reducing the scars of standard laparoscopy and towards scarless surgery. However, according to objective assessment of the literatures, there is no clearly demonstrated benefit of NOTES (LESS), even cosmesis is poorly supported and had mixed results in the available data. NOTES (LESS) is far from the truly scarless surgery. Towards the Holy Grail, we have developed several techniques of creating nonvisible scar and named them as “Scar-hidden Endoscopic Surgery”. With the rapid development of science and technology, we believe that minimally invasive surgery over the next 2 decades will continue to bring remarkable change and realize truly scarless surgery even we may not be able to imagine what lies ahead.
Core tip: Natural orifice transluminal surgery (NOTES) and Laparo-endoscopic single-site surgery (LESS) are very exciting new modalities in the field of minimally invasive surgery which towards scarless surgery. However, according to objective assessment, NOTES (LESS) is far from the truly scarless surgery. Towards the Holy Grail, we have developed several techniques of creating nonvisible scar and named them as “Scar-hidden endoscopic surgery”. With the rapid development of science and technology, we believe that minimally invasive surgery over the next 2 decades will continue to bring remarkable change and realize truly scarless surgery.
- Citation: Hu H, Xu AA. Towards the Holy Grail: What can we do for truly scarless surgery? World J Gastrointest Endosc 2015; 7(8): 814-818
- URL: https://www.wjgnet.com/1948-5190/full/v7/i8/814.htm
- DOI: https://dx.doi.org/10.4253/wjge.v7.i8.814
The past thirty years has witnessed the infancy and rapid development of minimally invasive surgery (MIS). From the early multiple small incisions laparoscopic surgery to the single incision laparoscopic surgery nowadays, minimally invasive surgery has come a long way from its initial stage and scarless surgery has been the Holy Grail.
Phillipe Mouret performed the first laparoscopic cholecystectomy in 1987[1]. Since then, laparoscopic approach has been used to many disease processes and gradually become the mainstream procedure for many intra-abdominal surgeries. Compared with open procedures, laparoscopic surgery has shown to decrease postoperative morbidity, shorten hospitalization and convalescence, and improve cosmesis for many applications[2,3]. Therefore laparoscopic surgery has been a well-established and commonplace technique worldwide in the past century. However, there were still 3-6 small incisions post-operation, which not only cosmetically unappealing, but also increase the wound pain and potential wound morbidity, such as abdominal wall bleeding and hernia, and intra-abdominal organ damage[4].
The quest for scar reduction and the increasing recognition of patient’s satisfaction has led to the innovation of conventional laparoscopic surgery. In the last decade, natural orifice transluminal surgery (NOTES) and Laparo-endoscopic single-site surgery (LESS) have been considered as the most advanced representative “evolution” of minimally invasive surgery. NOTES was first descripted by Kalloo et al[5] in 2004 and developed towards the scarless surgery, but did not gain popularity due to a variety of reasons including difficulty in accessing anatomical sites, lack of appropriate devices and sterility. The lack of success of NOTES has prompted the interest in LESS which also aimed to “scarless” effect. Compared with NOTES, LESS offers an advantage to surgeons with its similar performance used in traditional laparoscopy. However, LESS is also more technically difficult than traditional laparoscopic surgery, due to the challenges included loss of triangulation, external an internal conflict[6]. What’s more is that while laparoscopic literature sought to demonstrate superiority of the technique over that of open surgery, the publications on LESS generally seem to seek to demonstrate equivalence with laparoscopy, with the major focus being on cosmesis[7]. LESS still has far a long way to go before becomes the mainstream approach for truly scarless surgery as it remains an evolving technique.
With the rapid development of science and technology, scarless surgery has been the Holy Grail of MIS. However, what’s MIS? Indeed, the term “minimally invasive surgery” has often been bastardized to imply a specific access strategy such as laparoscopy, robotic surgery or endoscopy, but the true definition of minimally invasive surgery may have been created by Sir William Osler over a century ago when he said that, “Diseases that harm call for treatments that harm less”. More specifically, minimally invasive surgery should meet the following factors. The first and foremost factor is curing the pathology[8]. When approach and technique are considered, the most important question that mandates answer is will the pathology be appropriately treated with the absolute best safety profile possible. Secondary to surgical efficacy is decrease blood loss, postoperative pain, postoperative complications, surgical time (not by itself an absolute goal), convalescence and length of hospital stay. Thirdly, and the least important are surgical cosmesis and cost-effectiveness ratios. Based on the above, when define the truly scarless surgery, not only do these procedures should provide equivalent outcomes to traditional laparoscopic surgery, but also offer significant benefits as quicker recovery, shorter hospital stays, less scarring, less pain, lower morbidity and less surgical time (not an absolute goal).
Towards to the scarless surgery, NOTES and LESS have been developed and aimed to reducing the incisions of conventional laparoscopy. Surgeon’s interest was focused on reducing or eliminating the incisions caused by the procedure. The hope is that reduced access points will ultimately decrease pain, morbidity, convalescence, and improve cosmesis. However, according to objective assessment of the literature which compared current standard laparoscopic techniques with NOTES (LESS), there is no clearly demonstrated benefit of NOTES (LESS), even cosmesis is poorly supported and had mixed results in the available data[9,10]. In patient polls, surgical success, risk, pain, convalescence and cost all ranked higher than cosmesis. NOTES and LESS were far from the truly scarless surgery.
As already mentioned, scarless surgery has been the Holy Grail of minimally invasive surgery. However, as it is difficult, if not impossible, to achieve truly scarless in current days, several techniques of creating nonvisible scar have been developed, which we named as “Scar-hidden endoscopic surgery (SHES)”. SHES include 2 broad categories of those techniques performed by obtaining new access to peritoneal cavity and those by hiding scar in the anterior abdominal wall.
The use of first category was represented by NOTES. In its purest form, NOTES does not use any transabdominal ports therefore decreased pain and eliminated the abdominal wound morbidity. However, NOTES was hampered by difficulty in accessing anatomical sites, lack of appropriate devices and sterility, thus far been successfully performed in patients and not a truly scarless surgery.
The limitations of NOTES led to the concept of LESS which also produced nonvisible scar as it hidden easily in umbilical plica. However, LESS is also more technically difficult than traditional laparoscopic surgery, due to the inherent challenges. As techniques mentioned above were fraught with problems, we attempted other approaches.
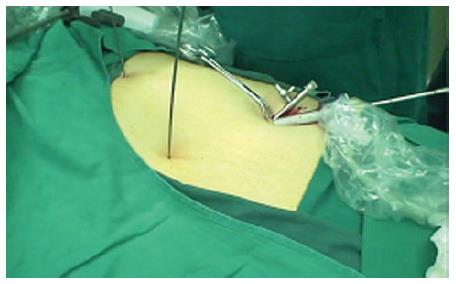
Surgical technique: A10-mm trocar was placed through an umbilical incision. After establishment of a pneumo-peritoneum, a 5-mm 30° laparoscope was introduced through the trocar. Two 5-mm suprapubic trocars were placed near the right and left ends of the superior margin of suprapubic hair under the guidance of the laparoscope. The laparoscope was then moved to the left side trocar. The instruments were introduced through the umbilical and the right side ports (Figure 1).
Advantages: Our research indicated that, compared with LESS, this approach characterized by no visible scar, a shorter operation time, minimal bleeding, etc., but longer instruments should be used[11].
The surgical technique and advantages of this approach were the same as described in approach above. What’s different is that the two 5-mm trocars were placed near the right and left ends of the tattoo or previous operation scar.
Surgical technique: A 15-mm incision was made at the right side of the umbilicus; a 10-mm trocar for the optic unit and another 5-mm trocar for the grasper were inserted side by side into the incision; a 5-mm trocar for instruments (ultrasonic scalpel, grasper, electrosurgical hook knife and hem-o-lok clips) was placed 20 mm inferior to the xiphoid (Figure 4).
Advantages: In our opinion, the transxiphoid-umbilical laparoscopic approach for laparoscopic cholecystectomy is as comfortable as the conventional techniques for laparoscopic cholecystectomy and allows the use of normal laparoscopic instruments. It has an advantage over conventional three-port laparoscopic cholecystectomy in both postoperative pain and, more importantly, cosmetic outcome, without a significant learning curve or increase in operative time. It offers a realistic better approach to conventional LC for chronic benign gallbladder disease.
Approach 4: Reduce the size of incision.
According to a previous study of us, the Optimized two-trocar LESS technique (a 2-mm trocar inserted for a grasper in the right upper abdomen) was found to be faster and less painful than the LESS approach and the 2-mm incision was almost nonvisible post-operation[12]. Under the guidance of this technique, we proposed another novel SHES as described below.
Surgical technique: A 15-mm incision was made at the right side of the umbilicus; a 10-mm trocar for the optic unit and another 5-mm trocar for an ultrasonic scalpel or clips were inserted side by side into the incision. Under laparoscopy, a 2-mm needle-shape grasper was placed direct through the abdominal wall in the midclavicular line 20 mm inferior to the costal margin, and electrocautery placed 20 mm inferior toxiphoid (Figure 5).
Advantages: Using the 2-mm needle-shape instruments, the new technique has following advantages: (1) The 2-mm grasper and electrocautery are at the normal location as the same as the traditional laparoscopic surgery. It helps to regain manipulate triangulation which not only enable performing sufficient traction of the gallbladder but also allow good mobilization of the gallbladder in order to dissect the calot’s triangle safely; (2) compared with LESS, the novel SHES was performed more feasibly and safely, with significantly shorter operation time and higher satisfactory score. Cosmesis, safety, and economy were balanced better in this new technique; and (3) the scars of the new technique were hidden in the natural folds of the skin around the navel and were too small to affect cosmesis when the 2-mm puncture hole on the upper abdomen healing. Compared with conventional laparoscopic surgery, it produced better cosmetic results while the operative time was almost equal according to our data[13].
According to the above analysis, NOTES or LESS is far from the truly scarless surgery as there were no longer follow-up, controlled and randomized studies which supported the touted benefits. There is no doubt that NOTES or LESS will be spurred on by rapid advances in technology and better instrumentation. However, when offering conventional vs investigational treatment options for patients, surgeons should be honest and balanced the safety and efficacy in their decision making.
In a word, what we believe is that, with the rapid development of science and technology, such as the use of da Vinci Surgical System, minimally invasive surgery in the nearly future will continue to bring remarkable changes and realize the truly scarless surgery.
| 2. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2325] [Article Influence: 110.7] [Reference Citation Analysis (0)] |
| 3. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1712] [Article Influence: 81.5] [Reference Citation Analysis (0)] |
| 4. | Kim SJ, Choi BJ, Lee SC. Overview of single-port laparoscopic surgery for colorectal cancers: past, present, and the future. World J Gastroenterol. 2014;20:997-1004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1037] [Cited by in RCA: 912] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 6. | Zhu JF, Hu H, Ma YZ, Xu MZ. Totally transumbilical endoscopic cholecystectomy without visible abdominal scar using improved instruments. Surg Endosc. 2009;23:1781-1784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Bucher P, Pugin F, Morel P. Transumbilical single incision laparoscopic sigmoidectomy for benign disease. Colorectal Dis. 2010;12:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 8. | Desai MM, Gill IS. LESS is more ... but needs even more. Eur Urol. 2011;60:1006-1007; discussion 1008-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Ross SB, Hernandez JM, Sperry S, Morton CA, Vice M, Luberice K, Rosemurgy AS. Public perception of LESS surgery and NOTES. J Gastrointest Surg. 2012;16:344-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc. 2010;24:1842-1848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 276] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 11. | Hu H, Zhu JF, Huang AH, Xin Y, Xu AA, Chen B. Covert laparoscopic cholecystectomy: a new minimally invasive technique. Acta Med Okayama. 2011;65:325-328. [PubMed] |
| 12. | Hu H, Zhu J, Wang W, Huang A. Optimized transumbilical endoscopic cholecystectomy: a randomized comparison of two procedures. Surg Endosc. 2010;24:1080-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Hu H, Xu AA, Huang A. Towards scarless surgery: a novel laparoscopic cholecystectomy by using 2-mm needle-shape instruments without trocar. J Laparoendosc Adv Surg Tech A. 2013;23:698-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Nakayama Y, Waisberg J S- Editor: Tian YL L- Editor: A E- Editor: Wu HL