Published online Dec 16, 2014. doi: 10.4253/wjge.v6.i12.625
Revised: October 15, 2014
Accepted: October 28, 2014
Published online: December 16, 2014
Processing time: 204 Days and 17.3 Hours
Acute upper gastrointestinal bleeding is a rare, but serious complication of gastric bypass surgery. The inaccessibility of the excluded stomach restrains postoperative examination and treatment of the gastric remnant and duodenum, and represents a major challenge, especially in the emergency setting. A 59-year-old patient with previous history of peptic ulcer disease had an upper gastrointestinal bleeding from a duodenal ulcer two years after having a gastric bypass procedure for morbid obesity. After negative upper endoscopy finding, he was urgently evaluated for gastrointestinal bleeding. At emergency laparotomy, the bleeding duodenal ulcer was identified by intraoperative endoscopy through gastrotomy. The patient recovered well after surgical hemostasis, excision of the duodenal ulcer and completion of the remnant gastrectomy. Every general practitioner, gastroenterologist and general surgeon should be aware of growing incidence of bariatric operations and coherently possible complications after such procedures, which modify patient’s anatomy and physiology.
Core tip: Bleeding duodenal ulcer after Roux-en-Y gastric bypass for morbid obesity is a rare, but life threatening situation. Anatomic rearrangement after bariatric operation prevents upper endoscopy from displaying stomach remnant, duodenum, and proximal jejunum. The bleeding duodenal ulcer was identified at emergency laparotomy by intraoperative endoscopy through gastrotomy. After surgical hemostasis, duodenal ulcer excision and completion of the remnant gastrectomy the postoperative course was uneventful.
- Citation: Ivanecz A, Sremec M, Ćeranić D, Potrč S, Skok P. Life threatening bleeding from duodenal ulcer after Roux-en-Y gastric bypass: Case report and review of the literature. World J Gastrointest Endosc 2014; 6(12): 625-629
- URL: https://www.wjgnet.com/1948-5190/full/v6/i12/625.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i12.625
Obesity in general is described as a global epidemic problem with growing prevalence by World Health Organization[1]. Bariatric surgery has been identified as a safe and effective treatment possibility for morbid obesity and allied comorbidities[2]. Increasing number of bariatric procedures correspond with severity of postsurgical complications[3].
Roux-en-Y gastric bypass (RYGB) is a frequent surgical procedure for these patients[2]. A significant flaw of RYGB is interrupted access to the bypassed stomach remnant by conventional endoscopy or contrast radiography[4,5]. Interrupted access could be a problem for evaluation and treatment of pathology in the bypassed gastric remnant. Severe complications in area of gastric remnant have been already reported, although the incidence of these complications following RYGB is very low[5-7]. There are retrospective series with 3000 cases of open RYGB presented, 8 patients (0.3%) had bleeding from peptic ulcer disease in the bypassed remnant and intestine[8,9]. Hemorrhage after RYGB could be early or late and in the literature is mostly limited to case reports only[10-12]. Although upper gastrointestinal bleeding originating from ulceration is infrequently reported, it could be a fatal complication.
This report describes the case of a 59-year-old patient, presented in an emergency setting with a life threatening bleeding from duodenal ulcer two years after RYGB.
A 59-year-old man presented to the emergency department complaining of weakness, faint and melena. His symptoms started one week before, with passing of darker stool. On the day he was admitted, he visited the market-place, where he fainted. On admission, the patient was pale, normotensive (126/76 mmHg), normocardic (89 per minute) and normopneic (16 per minute) with 85% SpO2. Anal exam showed melena.
His medical history included peptic ulcer disease, psoriatic arthritis and laparoscopic cholecistectomy. The patient has been overweight (BMI 50 kg/m2) in the past and underwent successful bariatric procedure two years prior at another institution. At the time of admission, there have been no data on exact type of bariatric surgery performed. The patient was a nonsmoker and denied alcohol abuse. The patient was on nonsteroidal anti-inflammatory medication (NSAID). Every day medications included diclofenac (100 mg) two times a day and combination of tramadol with paracetamol (37.5/325 mg) two times a day and once a week 12 mg of metotrexat. At the time of emergency admission, the patient had no prescription for any antiulcer drugs.
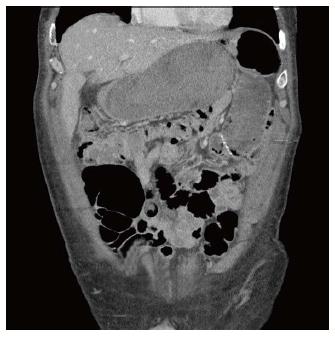
Laboratory results revealed decreased level of hemoglobin (83 g/L) and hematocrit (0.24) and coagulopathy. Despite multiple blood transfusions - 4 units of packed red blood cells administered - the patient’s anemia persisted. Two hours after admission an emergency upper endoscopy exposed a typical gastrojejunal anastomosis and was advanced 30 cm beyond, without evidence of active bleeding or clot. A longer pediatric endoscope was introduced. During endoscopy patient fainted again and felt stronger abdominal pain. The patient continued to maintain normal blood pressure and pulse. He was transferred to intensive care unit (ICU). A computed tomography (CT) scan demonstrated marked distention of a fluid-filled gastric remnant, a wider duodenal wall, and multiple fluid levels through proximal small intestine (Figure 1). No source of active bleeding was revealed.
As a result of ongoing hemorrhage, six hours after admission the patient was taken immediately to the operating room. An emergency midline laparotomy was undertaken.
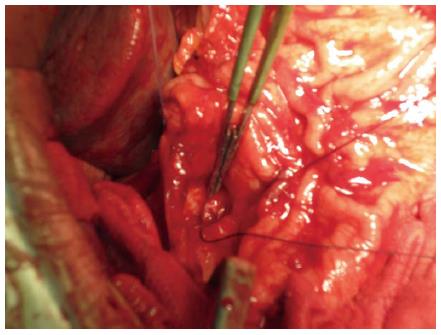
At surgical exploration a distended gastric remnant, filled with blood was revealed (Figure 2). The duodenum and the proximal jejunal loops were also filled with blood. Through gastrotomy the clothed blood was evacuated and the gastric remnant explored. No active bleeding was identified. Gastrotomy was extended distally to the pyloric region. There were no signs of bleeding; only bile was seen at this part. The duodenal region was covered by visceral adhesions after previous cholecistectomy; no external signs of ulceration could be identified. An intraoperative endoscopy performed trough gastrotomy showed a large ulcer in the posterior part of the second portion of the duodenum with a bleeding branch of gastro-duodenal artery at the bottom (Figure 3). Endoscopic hemostasis with adrenaline injection was ineffective. A gastrotomy was extended once again to duodenotomy and the bleeding ulcer was over-sewn with stitches. Additionally the gastroduodenal artery was ligated. The ulcer was excised together with first part of the duodenum and the stomach was mobilized to complete the remnant gastrectomy. The duodenal stump was closed primarily in two layered suture line with second layer fixing the stump to the head of the pancreas.
The first postoperative day was characterized by secretion of 1500 mL sero-hemorrhagic fluid trough drains. After initial improvement, decreasing hemoglobin levels were detected again. A relaparotomy was indicated, which revealed a 1 L of clothed blood in the upper abdominal cavity. No source of active bleeding was identified. The blood was evacuated, and the laparotomy closed.
The further postoperative course was uneventful and on 11th post-operative day the patient was discharged. After three months the patient was in very good shape with normal values of hemoglobin.
Histopathology revealed no Helicobacter pylori infection in duodenal or gastric tissue. Ulcer was 30 millimeters wide without any neoplastic or dysplastic cells.
Acute bleeding duodenal ulcer after Roux-en-Y gastric bypass for morbid obesity is a rare, but life threatening situation[10-12]. The presented patient developed first episode of such complication two years after bariatric operation at another institution. The type of previous surgical procedure (RYGB) was identified only after upper endoscopy and CT scan. The etiology of bleeding was unclear and continued despite aggressive volume replacement and multiple blood transfusions. Urgent laparotomy was the safest option in this life threatening situation. The patient had undergone intraoperative gastrotomy and intraoperative endoscopy through the gastrostomy. An active bleeding from duodenal ulcer was found and managed surgically. Additionally a remnant gastrectomy was performed.
There are many important issues, which should be emphasized in this case. Firstly, bariatric operations are frequently performed in Europe and United States[2]. With increasing number of such procedures, physicians should be familiar with its possible complications. In the emergency setting, the possible pitfall is not to known which type of bariatric surgery patient have had in the past. As in the reported case, the anatomical landmarks of RYGB were revealed only after endoscopic and CT investigations, while in the meantime dealing with threatening hemorrhagic shock.
Another point of interest is the rarity of this late complication. Bleeding from marginal ulcers localized near the pouch-enteric anastomosis is not uncommon after RYGB and could be easily diagnosed and managed by conventional endoscopy[2,13-16]. Bleeding duodenal ulcer after RYGB is rarely reported and it is mostly limited to case reports only[3,13,17-19].
Another issue of this report is difficulty of the diagnostic workup. Evaluation of the bypassed gastric remanant in patients with the possibility of bleeding peptic ulcer disease could be a major challenge. Endoscopic access becomes very difficult after RYGB because of excluded part of the stomach, duodenum, proximal jejunum, and biliary tree[9,20]. Conventional endoscopy of the gastric remnant and duodenum is not possible any more[2]. The long 90-150 cm Roux limb disables endoscopic approach, even with specialized instruments[3,9]. Many different methods have been suggested for displaying the bypassed gastrointestinal tract. These include endoscopy via percutaneous gastrostomy access, retrograde endoscopy and virtual gastroscopy using CT scan[21]. In our experience, it has been impossible to visualize the duodenum - even with longer pediatric endoscopes. A minimally invasive technique to access the bypassed stomach after RYGB for endoscopic diagnosis and treatment is described in the literature[9]. Ceppa et al[9] proposed a laparoscopic transgastric endoscopy. Such an approach was unattractive in this patient, where highly emergent ongoing bleeding from duodenal ulcer was present.
A special point of interest of this case concerns the proton-pump inhibitors regimens after RYGB. There are non-clear directives for managing patients after RYGB in this regard; however some surgeons advise lifelong proton-pump inhibitors for all patients undergoing RYGB surgery[22]. This patient underwent a complete diagnostic workup before bariatric surgery including upper endoscopy, and duodenal ulcer was diagnosed appropriately. Moreover, the patient was on every day therapy with NSAID for psoriatic arthritis. After the successful RYGB surgery, proton-pump inhibitors were prescribed for several months. Later, proton-pump inhibitors were abandoned. The reason for this is unclear.
Finally, the variety of the surgical management represents another point of interest. When the general and/or the hemodynamic status of the patient are critical, the surgical management should be limited only to a hemorrhage control[16]. After prompt control of the hemorrhage the surgical management was extended to resection of the gastric remnant. The rationale for this decision was to prevent the development of further possible complications, which include re-bleeding, perforation and gastric malignancy.
In conclusion, due to growing incidence of bariatric operations and possible complications, all healthcare professionals involved in the diagnostic workup of these patients, should be familiar with such procedures which modify patient’s anatomy and physiology. They should also be aware of the limitations of imaging methods, including urgent endoscopy.
Written informed consent for this case report was derived from the patient for the purpose of publication. A copy of the document could be presented for review by the Editor-in-Chief of this journal.
An 59-year-old male after gastric bypass procedure for morbid obesity with gastrointestinal bleeding.
The patient presented to the emergency department complaining of weakness, fainting, and melena.
Unexplained hemorrhagic shock with severe abdominal pain.
WBC 11.40 k/uL; HGB 8.30 gm/dL; coagulopathy with decreased levels of prothrombine; other liver function test were within normal limits.
CT scan showed marked distention of a fluid-filled gastric remnant and multiple fluid levels through proximal small intestine. Intraoperative endoscopy confirmed bleeding duodenal ulcer.
The excised duodenal ulcer was 30 millimeters wide and without any neoplastic or dysplastic cells.
At emergency laparotomy, the bleeding duodenal ulcer was identified by intraoperative endoscopy through gastrotomy. Surgical hemostasis, excision of the duodenal ulcer and completion of the remnant gastrectomy was performed.
Bariatric surgery modify patient’s anatomy and physiology. The treating physicians should be aware of the limitations of imaging methods, including urgent endoscopy.
Roux-en-Y gastric bypass is a common surgical procedure for morbid obese patients.
The increasing number of bariatric procedures correspond with the severity of postsurgical complications.
Nice case presentation: succint, linguistically correct, the references are well chosen and conform requirements of the Journal.
P- Reviewer: Buzas GM, Kate V S- Editor: Ji FF L- Editor: A E- Editor: Zhang DN
| 1. | Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1-253. |
| 2. | Peterli R, Borbély Y, Kern B, Gass M, Peters T, Thurnheer M, Schultes B, Laederach K, Bueter M, Schiesser M. Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg. 2013;258:690-64; discussion 695. |
| 3. | Zerey M, Sigmon LB, Kuwada TS, Heniford BT, Sing RF. Bleeding duodenal ulcer after roux-en-Y gastric bypass surgery. J Am Osteopath Assoc. 2008;108:25-27. |
| 4. | Sundbom M, Nyman R, Hedenström H, Gustavsson S. Investigation of the excluded stomach after Roux-en-Y gastric bypass. Obes Surg. 2001;11:25-27. |
| 5. | Voellinger DC, Inabnet WB. Laparoscopic Roux-en-Y gastric bypass with remnant gastrectomy for focal intestinal metaplasia of the gastric antrum. Obes Surg. 2002;12:695-698. |
| 6. | Macgregor AM, Pickens NE, Thoburn EK. Perforated peptic ulcer following gastric bypass for obesity. Am Surg. 1999;65:222-225. |
| 7. | Henneman D, Lagarde S, Geubbels N, Tuynman J, Jensch S, Van Wagensveld B. Complications after Laparoscopic Roux-en-Y gastric bypass: a diagnostic challenge. Report of three cases and review of the literature. G Chir. 2013;33:209-217. |
| 8. | Nguyen NT, Rivers R, Wolfe BM. Early gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg. 2003;13:62-65. |
| 9. | Ceppa FA, Gagné DJ, Papasavas PK, Caushaj PF. Laparoscopic transgastric endoscopy after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2002;3:21-24. |
| 10. | Braley SC, Nguyen NT, Wolfe BM. Late gastrointestinal hemorrhage after gastric bypass. Obes Surg. 2002;12:404-407. |
| 11. | Printen KJ, LeFavre J, Alden J. Bleeding from the bypassed stomach following gastric bypass. Surg Gynecol Obstet. 1983;156:65-66. |
| 12. | Spires WV, Morris DM. Bleeding duodenal ulcer after gastric bypass procedure for obesity. South Med J. 1987;80:1325-1326. |
| 13. | Issa H, Al-Saif O, Al-Momen S, Bseiso B, Al-Salem A. Bleeding duodenal ulcer after Roux-en-Y gastric bypass surgery: the value of laparoscopic gastroduodenoscopy. Ann Saudi Med. 2010;30:67-69. |
| 14. | Jamil LH, Krause KR, Chengelis DL, Jury RP, Jackson CM, Cannon ME, Duffy MC. Endoscopic management of early upper gastrointestinal hemorrhage following laparoscopic Roux-en-Y gastric bypass. Am J Gastroenterol. 2008;103:86-91. |
| 15. | Bhayani NH, Oyetunji TA, Chang DC, Cornwell EE, Ortega G, Fullum TM. Predictors of marginal ulcers after laparoscopic Roux-en-Y gastric bypass. J Surg Res. 2012;177:224-227. |
| 16. | Garancini M, Luperto M, Delitala A, Maternini M, Uggeri F. Bleeding from duodenal ulcer in a patient with bilio-pancreatic diversion. Updates Surg. 2011;63:297-300. |
| 17. | Mittermair R, Renz O. An unusual complication of gastric bypass: perforated duodenal ulcer. Obes Surg. 2007;17:701-703. |
| 19. | Gypen BJ, Hubens GJ, Hartman V, Balliu L, Chapelle TC, Vaneerdeweg W. Perforated duodenal ulcer after laparoscopic gastric bypass. Obes Surg. 2008;18:1644-1646. |
| 20. | Puri V, Alagappan A, Rubin M, Merola S. Management of bleeding from gastric remnant after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2012;8:e3-e5. |
| 21. | Husain S, Ahmed AR, Johnson J, Boss T, O’Malley W. CT scan diagnosis of bleeding peptic ulcer after gastric bypass. Obes Surg. 2007;17:1520-1522. |
| 22. | Gumbs AA, Duffy AJ, Bell RL. Incidence and management of marginal ulceration after laparoscopic Roux-Y gastric bypass. Surg Obes Relat Dis. 2006;2:460-463. |