Published online Jun 16, 2013. doi: 10.4253/wjge.v5.i6.275
Revised: April 10, 2013
Accepted: April 18, 2013
Published online: June 16, 2013
Processing time: 179 Days and 10 Hours
AIM: To evaluate the efficacy of circumferential endoscopic mucosal resection (EMR) with a tissue-anchoring device in comparison to forceps precut EMR and conventional endoscopic submucosal dissection (ESD).
METHODS: The study was designed as a prospective, randomized, ex vivo study. Fresh ex vivo specimens were harvested from adult white Yorkshire pigs weighing 30-50 kg. Seventy-five standardized, artificial lesions measuring 3 cm × 3 cm were created by methylene blue tattoo at the greater curvature in fresh ex vivo stomachs using the EASIE-R simulator platform (Endosim LLC, Berlin, MA, United States). The three advanced endoscopists performed the three resection techniques such as circumferential EMR using the tissue-anchoring device (TA-EMR), forceps precut EMR (FP-EMR), and endoscopic submucosal dissection. The endoscopists and the type of cutting methods were determined randomly by grouped randomized selection. The resection bed was grossly inspected to determine whether the lesion was resected “en-bloc” (defined as no remaining mucosal tattoo remaining on specimen). The resection bed was also probed for evidence of perforation. The procedural time of circumferential resection, submucosal dissection, and injection frequency were recorded by an independent observer.
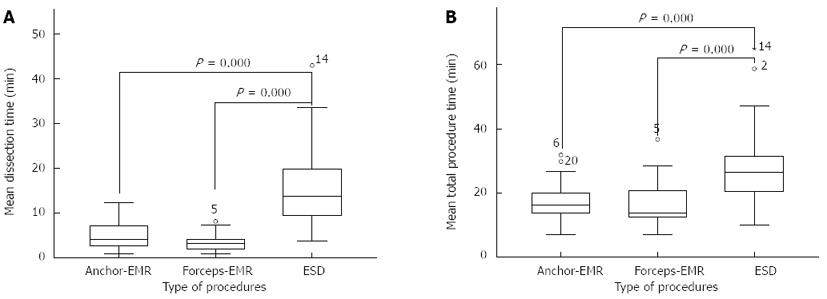
RESULTS: All 75 created lesions were successfully resected by three advanced endoscopists using the three techniques. The mean ± SD size of resected specimens (long axis) were 39.5 ± 5.6 mm, 36.5 ± 7.3 mm, and 44.6 ± 5.6 mm for TA-EMR, FP-EMR, and ESD respectively. The overall mean dissection time of both the TA-EMR and FP-EMR was significant shorter than ESD (TA-EMR: 5.1 ± 3.3 min, FP-EMR: 3.5 ± 2.0 min vs ESD: 15.8 ± 9.5 min, P < 0.001, P < 0.001). The overall mean total procedure time of both the tissue-anchoring and forceps circumferential EMR was significantly shorter than ESD (TA-EMR: 17.5 ± 6.0 min, FP-EMR: 16.6 ± 6.6 min vs ESD: 28.6 ± 13.9 min, P < 0.001, P < 0.001). The en-bloc resection rate of ESD was 100% (25/25) and the en-bloc resection rate of the TA-EMR (84.0%, 21/25) was higher than for the FP-EMR (60.0%, 15/25), yet not statistically significant (P = 0.18). The perforation rate of each technique was 8.0% (2/25).
CONCLUSION: TA-EMR appears to be quicker than ESD, and there was a trend towards improved en bloc resection rate with the TA-EMR when compared to the FP-EMR.
Core tip: The recently introduced tissue anchor device has the capability of deploying three spikes into the tissue that allow a reliable fixation of the tissue and facilitate retraction into snare. We demonstrated the efficacy of circumferential endoscopic mucosal resection (EMR) with a novel tissue-anchoring device in comparison with circumferential EMR using conventional forceps, and endoscopic submucosal dissection.
- Citation: Jung Y, Kato M, Lee J, Gromski MA, Chuttani R, Matthes K. Effectiveness of circumferential endoscopic mucosal resection with a novel tissue-anchoring device. World J Gastrointest Endosc 2013; 5(6): 275-280
- URL: https://www.wjgnet.com/1948-5190/full/v5/i6/275.htm
- DOI: https://dx.doi.org/10.4253/wjge.v5.i6.275
Endoscopic mucosal resection (EMR) is widely employed for the local treatment of early superficial cancer and dysplasia. Due to its simplicity and safety, it is one of the most common endoscopic techniques for resecting superficial lesions of the esophagus, stomach or colon. Various techniques of EMR such as ligation-EMR (EMRL), cap-EMR (EMRC), and strip-biopsy EMR (SB-EMR) have been developed. With these conventional techniques, however, the specimen size obtained from a one-piece resection is limited in size, with mean maximum resction sizes in the 10-15 mm range[1-5]. The precut-EMR (EMR-P) method, in which lesions are resected using a snare after circumferential precutting, allows en-bloc resection of lesion with a maximum diameter of 20 mm[6,7]. This snare technique is not reliable for lesions greater than 20 mm in diameter because of the difficulty of capturing and effectively ligating the significant amount of submucosal tissue in these lesions, even after successful circumferential precutting[3,8,9]. Endoscopic submucosal dissection (ESD) has a potential for a high rate of en-bloc resection, regardless of tumor size, leading to a more precise histological evaluation of the specimen and a lower recurrence rate at long-term follow up[10,11]. ESD, however, is a technically difficult procedure, and it can frequently cause serious complications such as significant bleeding or perforation. Thus, development of new endoscopic tools and the simplification of endoscopic resection techniques are necessary to enhance safety. Von Renteln and colleagues recently published a pilot study demonstrating the feasibility of grasp-and-snare circumferential EMR using a novel tissue-anchoring device (“Tissue Anchor”, Ovesco Endoscopy AG, Tübingen, Germany) for large-sized lesions[12]. To date, there is no study that compares circumferential EMR with this novel tissue-anchoring device and other resection techniques, including circumferential EMR with a conventional strip-biopsy technique and ESD. Therefore, the aim of this study is to evaluate of the efficacy of these three methods.
The study was designed as a prospective, randomized, ex vivo study. Fresh ex vivo specimens containing esophagus, stomach and duodenum were harvested from adult white Yorkshire pigs weighing 30-50 kg (from a commercial livestock vendor) and used with the EASIE-R simulator platform (Endosim, LLC, Berlin, MA, United States) (Figure 1). Institutional review board (IRB) review for human subject and/or live animal research was not required as there were no human research subjects or live animals involved in the study. A total of 75 procedures were performed by three advanced endoscopists. Prior to the study, the participants each practiced five cases of circumferential EMR using the novel tissue-anchoring device. Each endoscopist then performed eight to nine recorded cases of each: circumferential EMR using the tissue-anchoring device (TA-EMR), forceps precut EMR (FP-EMR), and endoscopic submucosal dissection (ESD).
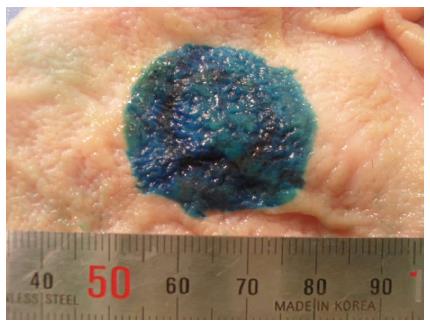
Seventy-five standardized, artificial lesions measuring 3 cm × 3 cm were created by methylene blue tattoo in the mucosa of fresh ex vivo stomachs at the anterior and posterior wall in the proximity of the greater curvature (Figure 2). The endoscopists and the type of cutting methods were determined randomly by grouped randomized selection (i.e., each endoscopist performed the same number of each procedure, but the order was randomized).
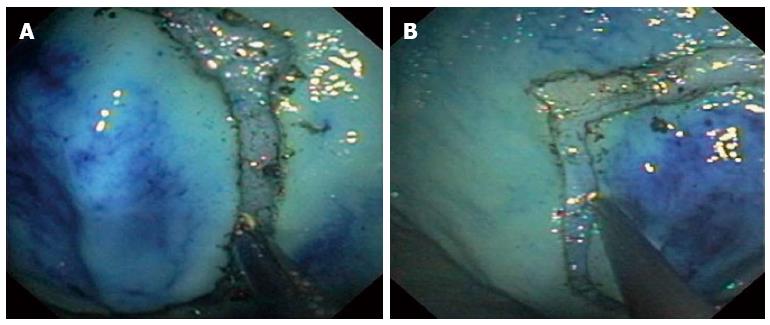
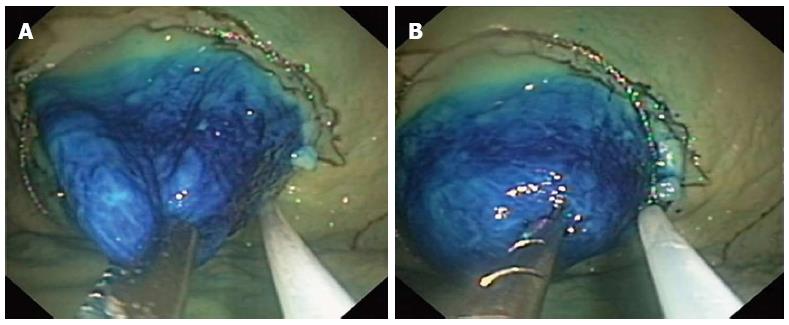
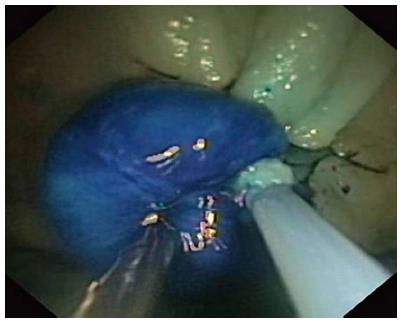
A double-channel endoscope (GIF-2T 160; Olympus America Inc, Center Valley, PA, United States) was used for all resections. A normal saline and methylene blue solution was injected to provide tissue separation between the mucosal and submucosal layers. For the circumferential TA-EMR, the tissue anchor was used to grasp the mucosal flap after circumferential cutting. For FP-EMR, a foreign body retrieval forceps (Olympus, Tokyo, Japan) was used to grasp the mucosal flap after circumferential cutting. For ESD, conventional ESD technique was used. All cases of direct circumferential resection were carried out with the hook knife, needle knife and IT knife, after repeated injection of the saline/methylene blue cushion solution (Figure 3A). The separation of the circumferential cutting area was carefully inspected (Figure 3B). The anchor and forceps accessories were used in the left channel of the double-channel endoscope for their respective resection techniques, and a 25 mm standard oval-shaped disposable electrosurgical snare (SD-210U-25, Olympus, Tokyo, Japan) was used in the right channel. Following injection with normal saline solution, the tissue anchor and forceps were then retracted into the endoscope to lift the mucosa, and the snare was placed into the circular pre-cut incision (Figure 4). The snare was subsequently closed and the specimen resected with electrocautery (UES-30 generator, 40 W output; Olympus America Inc, Center Valley, PA, United States) (Figure 5). For conventional ESD, a circular precut was made with the IT knife after an initial incision with the conventional needle knife. The lesion was then resected with a conventional needle knife and hook knife following injection to separate the mucosa and submucosa.
Immediately after retrieving the excised specimens, the lesions were spread and pinned on flat cork plates. The length and area of each excision specimen were measured. The resection bed was grossly inspected to determine whether the lesion was resected “en-bloc” (defined as no remaining mucosal tattoo remaining on specimen). The resection bed was also probed for evidence of perforation. The procedural time of circumferential resection, submucosal dissection, and injection frequency were recorded by an independent observer.
The sample size was calculated by 10 cases of initial data of each group (TA-EMR: 21.1 ± 6.4 min, FP-EMR: 20.1 ± 7.8 min, and ESD: 35.1 ± 18.5 min). We used the one-Way ANOVA method to estimate sample size, with an alpha of 0.05, a power of 80% and calculated an estimated sample size of 25 cases for each group. Data were analyzed by using SPSS software, version 18.0 (SPSS Inc Headquarters, Chicago, Ill). Statistical comparisons were made between the groups using the One-Way ANOVA test and statistical significance was defined as P < 0.05.
All 75 created lesions were successfully resected by three advanced endoscopists using the three techniques. All parameters (procedure time, specimen size, en-bloc resection status, and perforation) were successfully recorded by an independent observer for each procedure. The mean ± SD size of resected specimens (long axis) were 39.5 ± 5.6 mm, 36.5 ± 7.3 mm, and 44.6 ± 5.6 mm for the tissue-anchoring circumferential EMR (TA-EMR), forceps precut EMR (FP-EMR), and ESD respectively.
The overall mean total procedure time of TA-EMR was 17.5 ± 6.0 min (circumferential cutting: 7.4 ± 3.3 min, dissection: 5.1 ± 3.3 min) and the en-bloc resection rate was 84.0% (21/25) (Table 1).
| Endoscopist | Margin (min) | Dissection (min) | Total time (min) | Perforation (rate) | En-bloc(rate) |
| 1st | 7.3 ± 2.4 | 5.2 ± 3.8 | 17.8 ± 4.7 | 1/9 (11.1%) | 9/9 (100%) |
| 2nd | 9.0 ± 4.5 | 6.0 ± 3.7 | 21.5 ± 6.7 | 0/8 (0%) | 6/8 (75%) |
| 3rd | 5.8 ± 2.2 | 4.1 ± 2.1 | 13.2 ± 3.5 | 1/8 (12.5%) | 6/8 (75%) |
| Total | 7.4 ±3.3 | 5.1 ± 3.3 | 17.5 ± 6.0 | 2/25 (8.0%) | 21/25 (84.0%) |
The overall mean total procedure time of the forceps circumferential EMR was 16.6 ± 6.6 min (circumferential cutting: 7.9 ± 4.0 min, dissection: 3.5 ± 2.0 min) and the en-bloc rate was 60.0% (15/25). Two of the piecemeal resections (non en-bloc) resulted in 3 and 4 individual resection pieces, respectively (Table 2).
| Endoscopist | Margin (min) | Dissection (min) | Total time (min) | Perforation (rate) | En-bloc(rate) |
| 1st | 9.6 ± 4.1 | 3.8 ± 2.4 | 19.1 ± 9.2 | 0/8 (0%) | 5/8 (62.5%) |
| 2nd | 8.4 ± 2.9 | 3.6 ± 1.7 | 18.0 ± 3.8 | 0/9 (0%) | 4/9 (44.4%) |
| 3rd | 5.6 ± 2.3 | 3.0 ± 2.1 | 12.6 ± 4.3 | 2/8 (25%) | 6/8 (75%) |
| Total | 7.9 ± 4.0 | 3.5 ± 2.0 | 16.6 ± 6.6 | 2/25 (8.0%) | 15/25 (60.0%) |
The overall mean total procedure time of the ESD was 28.6 ± 13.9 min (circumferential cutting: 6.9 ± 4.9 min, dissection: 15.8 ± 9.5 min) and the en-bloc rate was 100% (25/25). The perforation rate of each technique was 8.0% (2/25) (Table 3). The overall mean dissection time of both the TA-EMR and FP-EMR was significant shorter than ESD (TA-EMR: 5.1 ± 3.3 min, FP-EMR: 3.5 ± 2.0 min vs ESD: 15.8 ± 9.5 min, P < 0.001, P < 0.001) (Figure 6A). The overall mean total procedure time of both the tissue-anchoring and forceps circumferential EMR was significantly shorter than ESD (TA-EMR: 17.5 ± 6.0 min, FP-EMR: 16.6 ± 6.6 min vs ESD: 28.6 ± 13.9 min, P < 0.001, P < 0.001) (Figure 6B).
| Endoscopist | Margin (min) | Dissection (min) | Total time (min) | Perforation (rate) | En-bloc(rate) |
| 1st | 7.2 ± 2.3 | 16.1 ± 7.0 | 30.5 ± 9.2 | 1/8 (12.5%) | 8/8 (100%) |
| 2nd | 8.3 ± 6.1 | 18.7 ± 12.1 | 33.1 ± 16.6 | 1/8 (12.5%) | 8/8 (100%) |
| 3rd | 5.5 ± 1.9 | 12.9 ± 7.0 | 22.9 ± 10.0 | 0/9 (0%) | 9/9 (100%) |
| Total | 6.9 ± 4.9 | 15.8 ± 9.5 | 28.6 ± 13.9 | 2/25 (8.0%) | 25/25 (100%) |
The ability to perform an en-bloc endoscopic resection of superficial cancerous and pre-malignant lesions may lead to an improvement of patient outcomes, since it provides an accurate and reliable histopathological evaluation. An inaccurate histopathological assessment from piece-meal resection may result in an inaccurate decision for further treatment and ultimately, local tumor recurrence[6,13]. EMR is used world-wide as the first-choice therapy for patients with early gastric cancer (EGC) who meet indications for this technique. The appropriate indication for EMR for EGC is considered to be an intramucosal differentiated type adenocarcinoma without ulceration or scarring, that is no more than 15 mm in size, regardless of macroscopic type[14]. The most common technique for upper gastrointestinal EMR include A) the strip biopsy method, also referred to as grasp-and-pull technique, using a double-channel endoscope, and B) the aspiration mucosectomy technique which uses a clear cap fitted onto the end of the endoscope. Using these techniques, only lesions of up to 10 mm in diameter can be reliably removed en-bloc with a sufficiently clear margin[15-18]. A definite histological diagnosis of the depth of invasion and the tumor margin from these resected specimens is frequently challenging, since the lesions measure only 10 mm or less in size. Circumferential incision with a tool such as the IT-knife, followed by snare resection (EMR-P), has been used to overcome such obstacles. Studies have demonstrated that the en-bloc resection rates of the EMR-P technique are 82% for lesions of 10 mm or less, 54%-75% for those between 11 and 20 mm, 14%-38% for those of over 20 mm. They showed that snaring a lesion of over 20 mm using this technique was difficult, even after successful circumferential incision by IT-knife[3,8,9].
The concept of tissue grasping in combination with snare resection, after circumferential cutting, may enable the performace of EMR to be expanded further. Ovesco’s recently introduced tissue anchor device has the capability of deploying three spikes into the tissue (Figure 7) that allow a reliable fixation of the tissue and facilitate retraction into snare. von Renteln et al[12] demonstrated that grasp-and-snare EMR using this tissue anchor, in combination with a 25 mm monofilament snare, is feasible and results in reliable en-bloc resections of up to 40 mm × 42 mm specimens. The group achieved 90% (9/10) complete en-bloc resections. They demonstrated an improved time-efficiency of this method (average of 32 min) when compared to ESD (average of 78 min). However, the study lacked a control group and allowed no direct comparison between various EMR/ESD methods.
In this study, we compared the efficacy (as defined by en bloc resection rate) and efficiency (as defined by time of total procedure) of grasp-and-snare circumferential EMR using a novel tissue-anchoring device in comparison to circumferential EMR with strip biopsy and direct ESD, using ex vivo porcine endoscopy simulator. Our results demonstrated that the overall mean total procedure time of TA-EMR was significantly shorter than ESD. Mean total procedure times of the anchor and forceps circumferential EMR were shorter than ESD. The overall mean total procedure time of TA-EMR was not significantly different from FP-EMR. The perforation rate of both TA-EMR and FP-EMR were comparable. However, the en-bloc rate of the TA-EMR (84.0%) was higher than for FP-EMR (60.0%), although this difference did not hold statistical significance (P = 0.18).
Based on our experience, the tissue-anchoring device was able to retract the mucosal flap into the snare easier and more efficiently than regular forceps since pulling the tissue with forceps resulted in a triangle shape of the mucosal flap as it only uses one point of traction. However, the tissue anchor is capable of retracting tissue from three anchor points (Figure 7). Therefore, it pulls the mucosal flap more efficiently into the snare thus avoiding a deformity of the lesion from unipolar traction. There is a theoretical potential for the three spikes of the tissue anchor to result in more injury of the resection specimen than the regular forceps since the spikes penetrate into the tissue. We did not, however, observe any injury of the specimens from the tissue anchor in any of the specimens retrieved. We believe that clear circumferential cutting is the most important factor for successful en-bloc resection. The operator should examine the adequate separation of the circumferential cutting area carefully before using the tissue-anchoring device for resection. A generous submucosal cushion should be injected and confirmed prior to retraction-assisted resection.
Limitations of this study include the fact that bleeding is not able to be accounted for as a complication in this simulation model. Of course, bleeding is a significant complication that must be managed in ESD and also occasionally in EMR. Furthermore, our study did not compare different sizes of lesions or compare multiple different anatomical resection locations.
In conclusion, the grasp-and-snare EMR using a novel tissue-anchoring device after circumferential cutting appears to be equivalent in performance to EMR using forceps, with a trend towards increased en bloc resection rate. When comparing the EMR techniques, we confirmed a known trade-off between techniques: ESD has more predictably successful en bloc resection of specimens, while the EMR techniques were significantly quicker to perform.
To date, there is no reliable endoscopic mucosal resection (EMR) method for en-bloc resection for lesions greater than 20 mm in diameter. Recently, a novel tissue-anchoring device was introduced to improve grasping and retraction of tissue for endoscopic resection.
This concept of tissue grasping in combination with snare resection after circumferential cutting is not new. However, the recently introduced tissue-anchoring device has the capability of deploying three spikes into the tissue that allow a reliable fixation of the tissue and facilitate retraction into snare. A pilot study demonstrated the feasibility of the grasp-and-snare EMR technique using a tissue-anchoring device for the resection of large-sized lesions.
The pilot study demonstrated that grasp-and-snare EMR using the tissue-anchoring device in combination with a 25 mm monofilament snare is feasible and results in reliable en-bloc resections of up to 40 mm x 42 mm specimens. The group achieved 90% complete en-bloc resections and time-efficiency of this method (average of 32 min) compared to the endoscopic submucosal dissection (ESD) (average of 78 min).
This study may represent another strategy for therapeutic intervention in the treatment of patients with large sized early gastric cancer or adenoma.
En-bloc was defined as no remaining mucosal tattoo on resected specimen.
Grasp-and-snare endoscopic mucosal resection using a novel tissue-anchoring device (TA-EMR) appears to be quicker than ESD, and there was a trend towards improved en bloc resection rate with the TA-EMR when compared to the conventional EMR technique.
P- Reviewers Yasud K, Yoshida S, Fujishiro M, Deutsch JC S- Editor Huang XZ L- Editor A E- Editor Zhang DN
| 1. | Yamaguchi Y, Katusmi N, Aoki K, Toki M, Nakamura K, Abe N, Morozumi K, Sugiyama M, Ishida H, Takahashi S. Resection area of 15 mm as dividing line for choosing strip biopsy or endoscopic submucosal dissection for mucosal gastric neoplasm. J Clin Gastroenterol. 2007;41:472-476. |
| 2. | Inoue H, Takeshita K, Hori H, Muraoka Y, Yoneshima H, Endo M. Endoscopic mucosal resection with a cap-fitted panendoscope for esophagus, stomach, and colon mucosal lesions. Gastrointest Endosc. 1993;39:58-62. |
| 3. | Ohkuwa M, Hosokawa K, Boku N, Ohtu A, Tajiri H, Yoshida S. New endoscopic treatment for intramucosal gastric tumors using an insulated-tip diathermic knife. Endoscopy. 2001;33:221-226. |
| 4. | Matsushita M, Hajiro K, Okazaki K, Takakuwa H. Endoscopic mucosal resection of gastric tumors located in the lesser curvature of the upper third of the stomach. Gastrointest Endosc. 1997;45:512-515. |
| 5. | Suzuki Y, Hiraishi H, Kanke K, Watanabe H, Ueno N, Ishida M, Masuyama H, Terano A. Treatment of gastric tumors by endoscopic mucosal resection with a ligating device. Gastrointest Endosc. 1999;49:192-199. |
| 6. | Ono H, Kondo H, Gotoda T, Shirao K, Yamaguchi H, Saito D, Hosokawa K, Shimoda T, Yoshida S. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225-229. |
| 7. | Choi IJ, Kim CG, Chang HJ, Kim SG, Kook MC, Bae JM. The learning curve for EMR with circumferential mucosal incision in treating intramucosal gastric neoplasm. Gastrointest Endosc. 2005;62:860-865. |
| 8. | Miyamoto S, Muto M, Hamamoto Y, Boku N, Ohtsu A, Baba S, Yoshida M, Ohkuwa M, Hosokawa K, Tajiri H. A new technique for endoscopic mucosal resection with an insulated-tip electrosurgical knife improves the completeness of resection of intramucosal gastric neoplasms. Gastrointest Endosc. 2002;55:576-581. |
| 9. | Muto M, Miyamoto S, Hosokawa A, Doi T, Ohtsu A, Yoshida S, Endo Y, Hosokawa K, Saito D, Shim CS. Endoscopic mucosal resection in the stomach using the insulated-tip needle-knife. Endoscopy. 2005;37:178-182. |
| 10. | Oka S, Tanaka S, Kaneko I, Mouri R, Hirata M, Kawamura T, Yoshihara M, Chayama K. Advantage of endoscopic submucosal dissection compared with EMR for early gastric cancer. Gastrointest Endosc. 2006;64:877-883. |
| 11. | Nakamoto S, Sakai Y, Kasanuki J, Kondo F, Ooka Y, Kato K, Arai M, Suzuki T, Matsumura T, Bekku D. Indications for the use of endoscopic mucosal resection for early gastric cancer in Japan: a comparative study with endoscopic submucosal dissection. Endoscopy. 2009;41:746-750. |
| 12. | von Renteln D, Schmidt A, Vassiliou MC, Rudolph HU, Caca K. Endoscopic mucosal resection using a grasp-and-snare technique. Endoscopy. 2010;42:475-480. |
| 13. | Gotoda T. Endoscopic resection of early gastric cancer: the Japanese perspective. Curr Opin Gastroenterol. 2006;22:561-569. |
| 14. | Miyata M, Yokoyama Y, Okoyama N, Joh T, Seno K, Sasaki M, Ohara H, Nomura T, Kasugai K, Itoh M. What are the appropriate indications for endoscopic mucosal resection for early gastric cancer? Analysis of 256 endoscopically resected lesions. Endoscopy. 2000;32:773-778. |
| 15. | Tanabe S, Koizumi W, Kokutou M, Imaizumi H, Ishii K, Kida M, Yokoyama Y, Ohida M, Saigenji K, Shimao H. Usefulness of endoscopic aspiration mucosectomy as compared with strip biopsy for the treatment of gastric mucosal cancer. Gastrointest Endosc. 1999;50:819-822. |
| 16. | Sadahiro S, Ishida H, Tokunaga N, Mukai M, Tajima T, Makuuchi H, Miyagawa M. Experimental assessment of endoscopic mucosectomy with a cap-fitted panendoscope. Endoscopy. 1998;30:713-717. |
| 17. | Inoue H, Tani M, Nagai K, Kawano T, Takeshita K, Endo M, Iwai T. Treatment of esophageal and gastric tumors. Endoscopy. 1999;31:47-55. |
| 18. | Makuuchi H, Kise Y, Shimada H, Chino O, Tanaka H. Endoscopic mucosal resection for early gastric cancer. Semin Surg Oncol. 1999;17:108-116. |