Published online Aug 16, 2012. doi: 10.4253/wjge.v4.i8.373
Revised: June 28, 2012
Accepted: August 8, 2012
Published online: August 16, 2012
Basaloid squamous carcinoma (BSC) of the esophagus is a rare esophageal tumor. A 79-year-old man with a history of proximal gastrectomy for gastric adenocarcinoma in 2000 was followed-up by esophagogastroduodenoscopy (EGD) annually. In June 2010, EGD revealed a new protruding lesion in the cervical esophagus. The small lesion was approximately 5 mm in size. A biopsy specimen showed poorly differentiated squamous cell carcinoma. We performed endoscopic mucosal resection using a cap-fitted endoscope (EMRC). The histological diagnosis of the endoscopically resected specimen was BSC and the invasion depth was limited to the muscularis mucosae. Horizontal and vertical margins were negative. We report the case of superficial BSC in the cervical esophagus successfully resected by EMRC.
- Citation: Nakamura M, Nishikawa J, Suenaga S, Okamoto T, Okamoto F, Miura O, Sakaida I. A case of EMRC for basaloid squamous carcinoma of the cervical esophagus. World J Gastrointest Endosc 2012; 4(8): 373-375
- URL: https://www.wjgnet.com/1948-5190/full/v4/i8/373.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i8.373
Basaloid squamous carcinoma (BSC) of the esophagus is a rare esophageal tumor[1]. It has been reported to have a poor prognosis because the incidences of lymph node and distant metastases are high in comparison with esophageal squamous cell carcinomas (SCCs)[2-4]. Therefore, surgical resection is generally performed for BSC. We report a case of small BSC in the cervical esophagus treated by endoscopic mucosal resection (EMR) using a cap-fitted endoscope (EMRC).
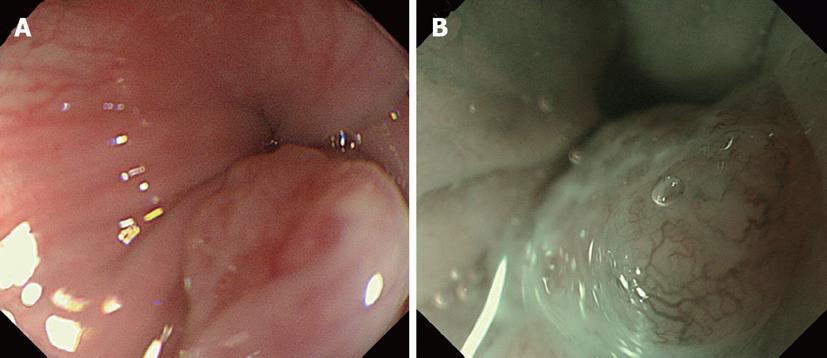
The patient was a 79-year-old man with a history of proximal gastrectomy due to gastric adenocarcinoma in 2000. He was annually followed-up by esophagogastroduodenoscopy (EGD). In June 2010, EGD revealed a new protruding lesion in the cervical esophagus. Pathological examination of an endoscopic biopsy specimen revealed poorly differentiated SCC, and he was referred to our hospital for further examination and treatment. The lesion was so small that he had no symptoms such as dysphagia. Physical examination and laboratory data revealed no abnormalities with the exception of an abdominal scar from laparotomy and mild anemia (Hb 111 g/L). Chest and abdominal computed tomography scanning and abdominal ultrasonography revealed no evidence of either lymph node or distant metastasis. EGD showed a protruding lesion located in the cervical esophagus (Figure 1A). The lesion was approximately 5 mm in size, and the surface was reddish and slightly rough. Magnifying endoscopy with narrow-band imaging (ME-NBI) showed the smooth surface of the lesion, and an avascular area surrounded by irregularly branched vessels (Figure 1B). The microvascular pattern was diagnosed as type 4M of Arima’s classification[5]. We diagnosed that the depth of tumor invasion was limited to the muscularis mucosae (MM) and performed EMRC with a GIF-H260Z (Olympus Corporation, Tokyo, Japan). Saline with indigocarmine was injected into the submucosa, and the lesion was lifted. The lesion was suctioned into the cap, and resected en bloc with the prelooped snare. There were no complications such as bleeding or perforation.
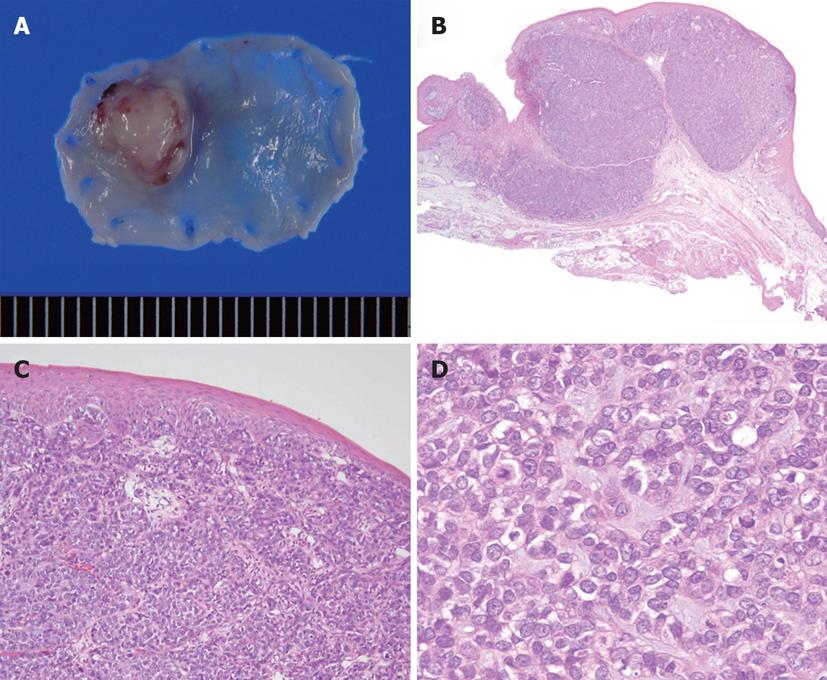
We show an image of the resected specimen in Figure 2A. The lesion was defined as 0-I (protruding type) according to endoscopic classification based on the Guidelines for Clinical and Pathologic Studies of the Japanese Society for Esophageal Disease[6]. The size of the lesion was 7 mm × 6 mm. The histological diagnosis was BSC and the invasion depth was limited to the MM (Figure 2B). The lesion was mainly located in the lamina propria mucosae (LPM) and covered with normal squamous epithelium (Figure 2C). The lesion consisted of oval cells like basal cells (Figure 2D). Horizontal and vertical margins were negative for cancer cells, and neither lymphatic nor venous invasion was observed. We followed the patient up without recurrence in the 6 mo after EMRC.
BSC of the esophagus is a rare tumor. It is reported in 0.068% of esophagectomy cases and 0.4% of autopsied cases[7]. BSC is derived from basal cells in the deepest epithelial layer and rapidly invades the LPM or deeper. Most BSC lesions reported previously in the literature invaded the muscularis propria or deeper[2-4]. In these cases, BSC was reported to have a worse prognosis than SCC of the esophagus because of the higher rates of lymph node and distant metastases[8].
Recently, it has been reported that superficial BSCs limited to within mucosal or submucosal layers have increased. Mori et al[9] reviewed 68 esophageal BSCs and found that the rates of lymph node metastasis were 0% (0/4) in mucosal BSCs and 21.8% (14/64) in the submucosal lesions. These results indicated that the rate of lymph node metastases of superficial BSCs did not differ from ordinary SCC of the esophagus. Thus, it might be possible for mucosal BSCs to be indicated for endoscopic therapy.
The rate of BSC located in the cervical esophagus is low and about 60% of lesions are in the middle esophagus[10]. Although EMRC for lesions in the cervical esophagus is generally difficult, we successfully resected the lesion en bloc while achieving a sufficient margin. Complete histological evaluation of the en bloc specimen is necessary to decide further clinical management. EMRC might be a better method than standard EMR for resection of BSCs because Farrell et al[11] reported that EMRC resulted in deeper histological resection than standard EMR.
Some investigators reported that superficial BSCs form small submucosal tumors. This finding might be a feature of the early stage of BSCs because they develop in the basal mucosal layer and invade the LPM and grew expansively. Our lesion was covered with normal squamous cells on the surface and the invasion depth was limited to the MM. BSC would grow upward, whereas BSCs invade deeper layers such as the submucosal or muscular layers.
It is reported that the microvascular pattern detected by ME-NBI is useful to diagnose the depth of tumor invasion of esophageal SCC[5,12]. As the cancer invades deeper into the mucosa, the intrapapillary capillary loops (IPCLs) become more dilated and elongated. When tumors invade the MM, the regular arrangement of IPCLs collapses and an avascular area surrounded by tumor vessels emerges. Arima et al[13] reported that these findings by ME-NBI could be employed for BSC as well. In this case, we diagnosed that the depth of tumor invasion was limited to within the MM and the histopathological findings for the resected specimen were identical. BSC limited to the MM in the cervical esophagus can be successfully resected en bloc by EMRC. Careful follow-up is necessary, though the rate of lymph node metastasis seems to be very low.
| 1. | Wain SL, Kier R, Vollmer RT, Bossen EH. Basaloid-squamous carcinoma of the tongue, hypopharynx, and larynx: report of 10 cases. Hum Pathol. 1986;17:1158-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 315] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 2. | Soriano E, Faure C, Lantuejoul S, Reyt E, Bolla M, Brambilla E, Righini CA. Course and prognosis of basaloid squamous cell carcinoma of the head and neck: a case-control study of 62 patients. Eur J Cancer. 2008;44:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Akagi I, Miyashita M, Makino H, Nomura T, Ohkawa K, Tajiri T. Basaloid squamous cell carcinoma of the esophagus: report of two cases. J Nihon Med Sch. 2008;75:354-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Tsukayama S, Hirano M, Murakami N, Uno Y, Nozawa H, Yoshino H, Orta N, Kikkawa H, Masuda S. A case report of basaloid-squamous carcinoma of the esophagus (in Japanese with English abstract). Nippon Shokaki Geka Gakkai Zasshi. 2000;33:462-466. |
| 5. | Arima M, Tada M, Arima H. Evaluation of microvascular patterns of superficial esophageal cancers by magnifying endoscopy. Esophagus. 2005;2:191-197 [doi: 10.1007/s10388-005-0060-6]. |
| 6. | Japanese Society for Esophageal Diseases. Guidelines for Clinical and Pathologic Studies on Carcinoma of the Esophagus. 9th ed. Tokyo: Kanahara 2001; . |
| 7. | Suzuki H, Nagayo T. Primary tumors of the esophagus other than squamous cell carcinoma--histologic classification and statistics in the surgical and autopsied materials in Japan. Int Adv Surg Oncol. 1980;3:73-109. [PubMed] |
| 8. | Lam KY, Law S, Luk JM, Wong J. Oesophageal basaloid squamous cell carcinoma: a unique clinicopathological entity with telomerase activity as a prognostic indicator. J Pathol. 2001;195:435-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Mori K, Ishii K. A case of superficial basaloid carcinoma of the esophagus (in Japanese). Nihon Gekakei Rengo Gakkaishi. 2008;33:742-745. |
| 10. | Ishii A, Chino O, Nishi T. Clinicopathological evaluation of basaloid carcinoma of the esophagus on endoscopic diagnosis (in Japanese with English abstract). Nippon Shokaki Naishikyou Gakkai Zasshi. 2007;49:2953-2961. |
| 11. | Farrell JJ, Lauwers GY, Brugge WR. Endoscopic mucosal resection using a cap-fitted endoscope improves tissue resection and pathology interpretation: an animal study. Gastric Cancer. 2006;9:3-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Kumagai Y, Toi M, Inoue H. Dynamism of tumour vasculature in the early phase of cancer progression: outcomes from oesophageal cancer research. Lancet Oncol. 2002;3:604-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Arima H, Arima M, Tada T. Microvascular patterns of esophageal micro squamous cell carcinoma on magnifying endoscopy. Dig Endosc. 2008;20:6-11. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Peer reviewer: Giuseppe Galloro, Professor, Department of General, Geriatric and Oncological Surgery and Advanced Technologies, Special Section of Digestive Surgical Endoscopy University of Naples “Federico II” - School of Medicine, Via S. Pansini, 5 80131 Napoli, Italy
S- Editor Song XX L- Editor A E- Editor Zheng XM