Published online Aug 16, 2012. doi: 10.4253/wjge.v4.i8.368
Revised: July 16, 2012
Accepted: August 8, 2012
Published online: August 16, 2012
AIM: To determine the learning curves for antegrade double-balloon enteroscopy (aDBE) and retrograde DBE (rDBE) by analyzing the technical success rates.
METHODS: A retrospective analysis in a tertiary referral center. This study reviewed all cases from June 2006 to April 2011 with a target lesion in the small-bowel identified by either capsule endoscopy or computed tomography scan posted for DBE examinations. Main outcome measurements were: (1) Technical success of aDBE defined by finding or excluding a target lesion after achieving sufficient length of small bowel intubation; and (2) Technical success for rDBE was defined by either finding the target lesion or achieving stable overtube placement in the ileum.
RESULTS: Two hundred and eighty two procedures fulfilled the inclusion criteria and were analyzed. These procedures were analyzed by blocks of 30 cases. There was no distinct learning curve for aDBE. Technical success rates for rDBE continued to rise over time, although on logistic regression analysis testing for trend, there was no significance (P = 0.09). The odds of success increased by a factor of 1.73 (95% CI: 0.93-3.22) for rDBE. For these data, it was estimated that at least 30-35 cases of rDBE under supervision were needed to achieve a good technical success of more than 75%.
CONCLUSION: There was no learning curve for aDBE. Technical success continued to increase over time for rDBE, although a learning curve could not be proven statistically. Approximately 30-35 cases of rDBE will be required for stable overtube intubation in ileum.
- Citation: Tee HP, How SH, Kaffes AJ. Learning curve for double-balloon enteroscopy: Findings from an analysis of 282 procedures. World J Gastrointest Endosc 2012; 4(8): 368-372
- URL: https://www.wjgnet.com/1948-5190/full/v4/i8/368.htm
- DOI: https://dx.doi.org/10.4253/wjge.v4.i8.368
The American Society for Gastrointestinal Endoscopy has guidelines specifically addressing standards for training, assessing competence, and granting privileges to endoscopy[1]. Together with American College of Gastroenterology, quality indicators for major endoscopic procedures like esophagogastroduodenoscopy (EGD)[2], colonoscopy[3], endoscopic retrograde cholangiopancreatography (ERCP)[4] and endoscopic ultrasonography (EUS)[5] were formulated. Efforts from numerous groups of researchers in the past in developing performance parameters contributed significantly in formulating endpoints that define high quality endoscopic services.
Since the introduction of double-balloon enteroscopy (DBE) by Yamamoto et al[6] in 2001, the technique has developed into a widely used intervention for small bowel diagnosis and therapy. However, performance parameters in DBE are lacking. Several recent papers[7,8] had addressed some questions regarding technical success. Gross et al[9] evaluated the improvement in clinical impact and noted that with experience, helpful clinical impact rose. We retrospectively studied all DBE cases performed in our institution and investigate the learning curves for both ante grade and retrograde approaches with a focus on technical end-points.
This is a single-center retrospective study in a tertiary referral teaching hospital in Sydney, Australia. In our institution, one endoscopist (who is the senior author of this article) with experience in DBE and in therapeutic endoscopy performed all procedures, with trainees assisting with the overtube. The endoscopist has an experience of performing approximately 10 000 EGD, 7000 colonoscopies, 4000 ERCPs and 2500 EUS. DBE was performed using the Fujinon enteroscope (Fujinon EN-450T5, Fujinon Corporation, Saitama, Japan). DBE was performed via the antegrade (aDBE) or retrograde (rDBE) route, and the intention was to perform a targeted approach with the DBE. The approach was determined by the endoscopist, based on the position the lesion was suspected most often determined by the time a lesion was seen in relation to the total small-bowel transit time on a capsule endoscopy (CE) study. If the lesion was within the proximal two thirds of the small-bowel, then an aDBE was used.
The DBE was performed with the patient under conscious or deep sedation with a combination of intravenous midazolam (Pfizer, Bentley, Australia), fentanyl (Mayne Pharma Ltd., Mulgrave, Australia), and propofol (Fresofol 1%, Pharmatel Fresenius Kabi Pty Ltd., Hornby, Australia) administered by the assistant or attending anesthetist. The preparation for the procedures included a fasting period of 8 h before the oral procedure and a routine bowel preparation with a sodium picosulfate–based (Picoprep, Pharmatel Fresenius Kabi Pty Ltd, Hornsby, Australia), or sodium phosphate-based preparations (Fleet, Ferring Pharmaceuticals, Gordon, Australia) with a clear fluid diet the day before the procedure for the anal approach. The technique of DBE was previously described by the innovator Yamamoto et al[6].
Institutional Review Board approval was obtained before data collection. Information on DBE was extracted from the endoscopy unit database. Clinical records of these patients were traced from the Medical Record Department. Information on patient demographics, indications, previous investigations (endoscopic and radiologic), findings and intervention with DBE, limitations of insertion, complication rates, and immediate follow-up after therapy were all retrieved.
Inclusion criteria for this study were patients who had lesions suspected on CE or other imaging techniques such as computed tomography (CT), small-bowel barium meal follow-through performed prior to DBE. These lesions were used as target lesions for DBE.
For aDBE: Success was defined by finding the target lesion seen on previous imaging or insertion of enteroscope beyond the suspected site of lesion as estimated on prior imaging, in such a way that it sufficiently excluded the presence of a lesion.
For rDBE: Success was defined by finding the target lesion or stable intubation into the ileum with overtube balloon securely placed beyond the ileocecal valve. This criterion was chosen since stable overtube placement in the ileum is fundamental to “anchor” the overtube above ileocecal valve and prevent frequent falling back into the cecum. This was perceived by the endoscopist by the disappearance of the resistance for advancement.
All cases included were discussed with the endoscopist, who is the senior author of this paper, to decide on their success rate based on the above pre-defined criteria.
All statistical analyses were performed using the Statistical Package for Social Sciences version 14.0 (Chicago, IL, United States). The mean ± SD, and range were calculated for continuous data. Categorical data analysis was performed by using the Fisher exact test. The analysis was performed separately for aDBE and rDBE. In each group, data was analyzed by dividing them into blocks of approximately 30 cases each. These were plotted against time. Logistic regression analysis was used to test for a trend in the proportion of successes in each block over time. Statistical analysis was also performed to evaluate the differences between the blocks of procedures. A P < 0.05 was considered to be statistically significant.
From June 2006 to April 2011, a total of 333 procedures (204 antegrade, 129 retrograde) were performed on 268 patients. Fifty-one procedures were excluded because of no target lesions seen on previous investigations (n = 32), procedures performed for colonic indications (n = 10), poor bowel preparation (n = 4), sedation failure (n = 3) and technical/equipment failure (n = 2). Thus 282 cases were analyzed (184 antegrade, 98 retrograde). The mean ± SD age was 62 (18) years and 152 patients were female (53.9%).
The target lesion was identified by either CE (95.4%) or CT scan (4.6%). The target lesions and their modalities of investigations were summarized in Table 1. Angioectasia was the most common target lesion and was the target lesion in 121 (42.9%) procedures, followed by small-bowel polyps in 44 (15.6%) procedures.
| Modalities of investigation | Target lesions | n |
| Capsule endoscopy (total = 269) | Vascular lesions | |
| Angioectasia | 100 | |
| Red spots | 9 | |
| Neoplastic lesions | ||
| Mass lesions | 36 | |
| Polyps | 35 | |
| Evidence of bleeding | ||
| Blood | 25 | |
| Other lesions | ||
| Ulcers | 23 | |
| Erosions | 6 | |
| Mucosal abnormality | 5 | |
| Enteritis | 4 | |
| Strictures | 4 | |
| Double pathology | ||
| Angioectasia and polyps | 9 | |
| Angioectasia and ulcers | 5 | |
| Angioectasia and erosions | 3 | |
| Angioectasia and mass lesions | 2 | |
| Angioectasia and stricture | 2 | |
| Blood and mass lesion | 1 | |
| CT scan (total = 13) | Thickened small bowel | 8 |
| Mass lesions | 5 |
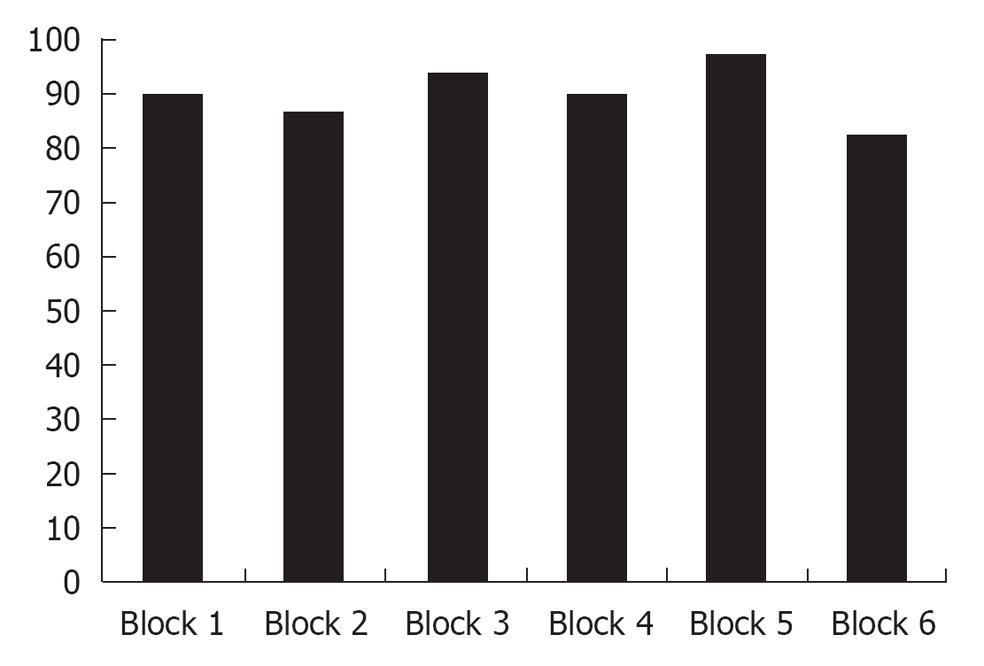
For aDBE: The overall technical success for the aDBE cohort was 89.7% (165/184). The technical success rates of aDBE were analyzed by 6 blocks of 30/30/30/30/30/34. The results are shown in Table 2 and Figure 1. The first 30 cases demonstrated a success of 90.0% and remained consistent throughout. There is no statistically significant improvement with increasing experience as logistic regression analysis testing for trend over time was not significant (P = 0.73).
| Block No. | Details on outcome | Cases classified as clinical success (a+b) | Success rate (%) | P1 | ||
| Target lesions found (a) | Target lesions excluded (b) | Failed (c) | ||||
| 1 (n = 30) | 18 | 9 | 3 | 27/30 | 90.0 | 0.73 |
| 2 (n = 30) | 20 | 6 | 4 | 26/30 | 86.7 | |
| 3 (n = 30) | 18 | 10 | 2 | 28/30 | 93.3 | |
| 4 (n = 30) | 17 | 10 | 3 | 27/30 | 90.0 | |
| 5 (n = 30) | 17 | 12 | 1 | 29/30 | 96.7 | |
| 6 (n = 34) | 16 | 12 | 6 | 28/34 | 82.4 | |
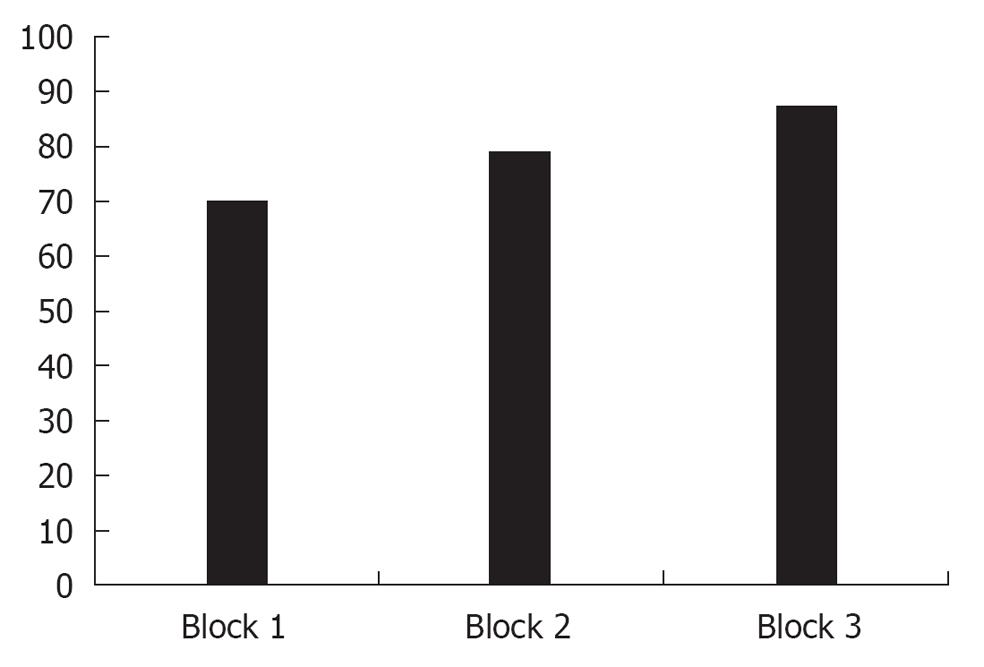
For rDBE: The overall technical success for the rDBE cohort was 78.6% (77/98). The technical success rates of aDBE were analyzed by 3 blocks of 33/33/32. Success according to increasing experience is shown in Table 3 and Figure 2. The initial success on first block was 70% but increased to 78.8% and 87.5% in subsequent blocks. There was no statistical significance when the second and third blocks were compared to the first block (P = 0.40 and 0.09). Logistic regression analysis testing for trend over time also did not show significance (P = 0.09).
| Block No. | Cases classified as technical success (finding the target lesion and/or stable overtube intubation in ileum) | Success rate (%) | P1 |
| 1 (n = 33) | 23/33 | 70.0 | 0.09 |
| 2 (n = 33) | 26/33 | 78.8 | |
| 3 (n = 32) | 28/32 | 87.5 |
One patient with ongoing small bowel bleeding from an angioectasia in the distal small bowel underwent a retrograde procedure with diathermy of the lesion presented 2 d later with a bowel perforation. He subsequently had a laparotomy and found a bowel perforation at the diathermy site. Resection and re-anastomosis were done and patient recovered well.
Endoscopic procedures have evolved over the years with new emerging techniques designed to improve the quality of imaging and interventions. Learning curves for various endoscopic procedures were defined in the past, leading to official recommendations of threshold procedure numbers that should be carried out by trainees in order to obtain competence in endoscopy. The determination of these numbers is important in order to guide the teachers and learners, allowing endoscopists to be credentialed accordingly. Available data suggest that at least 25-30 flexible sigmoidoscopies[1,10], 130 upper endoscopies[1], 140 colonoscopies[1,11], and 180-300 ERCPs[1,12,13] are required for the usual trainee to achieve competence. However, there were concerns that an arbitrary number of procedures do not guarantee competency[14-16] and different levels of competency are required for different clinical endpoints desired. For example, pancreatobiliary EUS demands more experience than esophageal EUS[17], while 40-50 cases may provide adequate preparation for the accurate evaluation of submucosal lesions.
In considering such recommendations, we must first define expert or experienced levels of success to help define what should be the benchmark for others particularly in the accreditation of training competency. Two aspects in defining the success of any procedure are the identification of a performance standard and defining an acceptable level of success. For instance, in ERCP, cannulation and opacification of desired duct can be considered the performance standard and 80% success rate is the minimum measure of competency[18].
To date, there is little evidence defining performance parameters and describing the benchmark success level for DBE. Mehdizadeh et al[7,8] analyzed initial experience in 6 United States centers with regards to the learning curve of the procedure based on technical parameters like examination duration, depth of insertion, findings and technical success. The same group concluded that there was a significant decline in overall procedural and fluoroscopy times after the initial 10 DBE cases[7]. Also, 20 cases were taken as the minimum number for retrograde procedures to attain certain level of competency[8]. The only other article addressing the learning curve of DBE studied the clinical impact of DBE. In this case, Gross et al[9] demonstrated a rise of clinically helpful procedures from 58% to 86% comparing the first and last 50 procedures in a 200 DBE series.
The technical success of a procedure is usually based upon attainment of certain anatomical landmarks such as the cecum in colonoscopy. Due to little or no differentiation in the proximal small-bowel, definition of the technical success was not very useful for antegrade procedures. For retrograde procedures, finding the target lesion and/or stable overtube intubation of the ileum were chosen to be the definition of technical success in this study. Stable overtube intubation beyond ileocecal valve prevents retrograde movement of the system into the cecum, a key point in allowing the advancement of the enteroscope more proximally. This landmark was taken as the division between a successful and a failed procedure technically, a view previously acknowledged by Mehdizabeh et al[8]. In our series the overall technical success was 78.6% in the retrograde procedures, which is similar to Mehdizabeh’s observation of a failure to intubate small-bowel in 21%-31%[7,8].
Our series indicates that an endoscopist experienced in standard endoscopy may be able to perform aDBE with limited training, a view shared by Gross et al[9]. With regards to retrograde procedures, there was a gradual improvement for better technical success over time, although this was not statistically significant on trend analysis. A minimum of 30-35 cases in our series were needed in order to achieve more than 75% technical success. With this we will have a suitable platform to measure acceptable levels of success in DBE and provide meaningful recommendations for future trainees. The current literature including our work touches on some of these key issues and some patterns are developing but no clear recommendations can be made for training at this point. The study showed a trend towards technical success over time for rDBE as compared to aDBE. This could be due to the technical complexity of the retrograde approach, as compared to rather featureless anatomical structure of upper small bowel. These differences translate to some sort of learning curve as reflected by a trend towards technical success over time for rDBE.
We recognized several limitations with this study. Being a retrospective series, we are subject to reporting and interpretation bias. In addition, the endpoints measured are subject to interpretation and as confidence built during our experience this could have led to the perceived increase in success. We acknowledged that the definition for technical success in antegrade procedures in this study may be subjective due to lack of distinct anatomical landmark in the upper small-bowel. In addition, a single operator/center experience limits our ability to widely apply these results.
In conclusion, there seems to be no learning curve for aDBE. However, a gradual increase of successful retrograde procedures was noted with ongoing experience. Our study indicated a minimum of 30-35 cases of retrograde procedures were required to achieve stable ileal intubation and meaningful endoscopic success. Further larger studies will be required to define technical and clinical endpoints and to measure acceptable levels of success in DBE.
This study investigated the learning curve of double-balloon-enteroscopy (DBE) based on certain predefined criteria as successful endpoints.
This is a not well-studied topic as current know-how on DBE is still lacking. Literatures on learning curve of the procedure are sparse as difficulties often encountered on definition of success in this procedure.
The paper used certain endpoints as technical success of the procedure. This is the first time these criteria were used to define the success of performing DBE.
This is an important area as it allows future policy-makers to determine number of cases required prior to attainment of competency in performing DBE. DBE is expected to find more applications clinically and knowledge on learning curve will allow an appropriate credentialing for the procedurists.
Antegrade DBE is used to imply DBE that uses an antegrade approach as compared to retrograde DBE which means the retrograde approach.
The reviewers appreciated that this is an interesting area whereby data are lacking and a good study is difficult. Despite the fact that this study is a single-operator experience, it has its value in providing reference in quality control of procedures.
| 1. | Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ, Waring JP. Methods of granting hospital privileges to perform gastrointestinal endoscopy. Gastrointest Endosc. 2002;55:780-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Cohen J, Safdi MA, Deal SE, Baron TH, Chak A, Hoffman B, Jacobson BC, Mergener K, Petersen BT, Petrini JL. Quality indicators for esophagogastroduodenoscopy. Am J Gastroenterol. 2006;101:886-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, Hoffman B, Jacobson BC, Mergener K, Petersen BT. Quality indicators for colonoscopy. Am J Gastroenterol. 2006;101:873-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, Hoffinan B, Jacobson BC, Petrini JL, Safdi MA. Quality indicators for endoscopic retrograde cholangiopancreatography. Am J Gastroenterol. 2006;101:892-897. [PubMed] [DOI] [Full Text] |
| 5. | Jacobson BC, Chak A, Hoffman B, Baron TH, Cohen J, Deal SE, Mergener K, Petersen BT, Petrini JL, Safdi MA. Quality indicators for endoscopic ultrasonography. Am J Gastroenterol. 2006;101:898-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 867] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 7. | Mehdizadeh S, Ross A, Gerson L, Leighton J, Chen A, Schembre D, Chen G, Semrad C, Kamal A, Harrison EM. What is the learning curve associated with double-balloon enteroscopy Technical details and early experience in 6 U.S. tertiary care centers. Gastrointest Endosc. 2006;64:740-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 199] [Article Influence: 10.0] [Reference Citation Analysis (1)] |
| 8. | Mehdizadeh S, Han NJ, Cheng DW, Chen GC, Lo SK. Success rate of retrograde double-balloon enteroscopy. Gastrointest Endosc. 2007;65:633-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Gross SA, Stark ME. Initial experience with double-balloon enteroscopy at a U.S. center. Gastrointest Endosc. 2008;67:890-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Hawes R, Lehman GA, Hast J, O'Connor KW, Crabb DW, Lui A, Christiansen PA. Training resident physicians in fiberoptic sigmoidoscopy. How many supervised examinations are required to achieve competence. Am J Med. 1986;80:465-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 44] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Cass OW, Freeman ML, Cohen J, Zuckerman G, Watkins J, Nord J, Locke GR, Jensen D, Diehl D, Cerulli M. Acquisition of competency in endoscopic skills (ACES) during training: A multicenter study. Gastrointest Endosc. 1996;43:308A. [RCA] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Jowell PS, Baillie J, Branch MS, Affronti J, Browning CL, Bute BP. Quantitative assessment of procedural competence. A prospective study of training in endoscopic retrograde cholangiopancreatography. Ann Intern Med. 1996;125:983-989. [PubMed] |
| 13. | Verma D, Gostout CJ, Petersen BT, Levy MJ, Baron TH, Adler DG. Establishing a true assessment of endoscopic competence in ERCP during training and beyond: a single-operator learning curve for deep biliary cannulation in patients with native papillary anatomy. Gastrointest Endosc. 2007;65:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 93] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Cass OW, Freeman ML, Peine CJ, Zera RT, Onstad GR. Objective evaluation of endoscopy skills during training. Ann Intern Med. 1993;118:40-44. [PubMed] |
| 15. | Friedman LS. How long does it take to learn endoscopy. Gastrointest Endosc. 1995;42:371-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Marshall JB. Technical proficiency of trainees performing colonoscopy: a learning curve. Gastrointest Endosc. 1995;42:287-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 100] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 17. | Hoffman BJ, Hawes RH. Endoscopic ultrasound and clinical competence. Gastrointest Endosc Clin N Am. 1995;5:879-884. [PubMed] |
| 18. | Training the gastroenterologist of the future: the gastroenterology core curriculum. The Gastroenterology Leadership Council. Gastroenterology. 1996;110:1266-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
Peer reviewer: Taro Osada, MD, PhD, Associate Professor, Department of Gastroenterology, Juntendo University, 2-1-1 Hongo Bunkyo-ku Tokyo 113-8421, Japan
S- Editor Song XX L- Editor A E- Editor Zheng XM