Published online Feb 16, 2026. doi: 10.4253/wjge.v18.i2.115745
Revised: November 25, 2025
Accepted: December 23, 2025
Published online: February 16, 2026
Processing time: 103 Days and 18 Hours
Esophageal or gastric submucosal hematoma is a rare condition. Esophageal and gastric submucosal hematomas rarely coexist, with only a few cases reported worldwide to date. Some of these gastric and esophageal submucosal hematomas were caused by pancreatitis, peptic ulcers, spontaneous hematomas, and endo
We present the case of a 57-year-old male who had repeated episodes of nausea and vomiting for 2 days. Physical examination was unremarkable. Complete blood count revealed moderate anemia and elevated inflammatory markers. A gastroscopy revealed esophageal stricture 40 centimeter from the incisors. Com
A ruptured vascular malformation represents an unusual cause of esophageal and gastric submucosal hematomas, conservative treatment following interventional therapy is an effective treatment option.
Core Tip: Submucosal hematoma of the stomach or esophagus is rare and can result due to endoscopic therapy, coa
- Citation: Wu JJ, Chen D, Liu D, Zhong DF. Huge esophagogastric submucosal hematoma associated with arterial malformations: A case report. World J Gastrointest Endosc 2026; 18(2): 115745
- URL: https://www.wjgnet.com/1948-5190/full/v18/i2/115745.htm
- DOI: https://dx.doi.org/10.4253/wjge.v18.i2.115745
Esophageal or gastric submucosal hematoma is a rare condition usually resulting from coagulopathy, trauma, peptic ulcer disease, pancreatitis, endoscopic therapy, or spontaneous hematomas[1]. However, submucosal hematoma related to arterial malformation, there is only one case of esophageal submucosal hematoma reported so far[2]. The presence of both esophageal and gastric submucosal hematomas associated with arterial malformation is extremely rare, with few cases reported worldwide to date. Here, we describe a patient with huge esophageal and gastric submucosal hematomas accompanied by nausea and vomiting, which were due to arterial malformations.
The 57-year-old male was admitted due to recurrent nausea and vomiting.
The patient experienced repeated nausea and vomiting for 2 days without any obvious inducement, which were particularly noticeable after eating.
His past medical history included hypertension and type 2 diabetes.
Personal and family history was negative for gastrointestinal diseases.
On physical examination no abnormalities were found. The patient had a normal body mass index. No abdominal tenderness and no masses were noted.
Initial investigations showed a hemoglobin level of 8.9 g/dL, C-reactive protein of 200 mg/L, and white blood cells of 9.3 × 109/L.
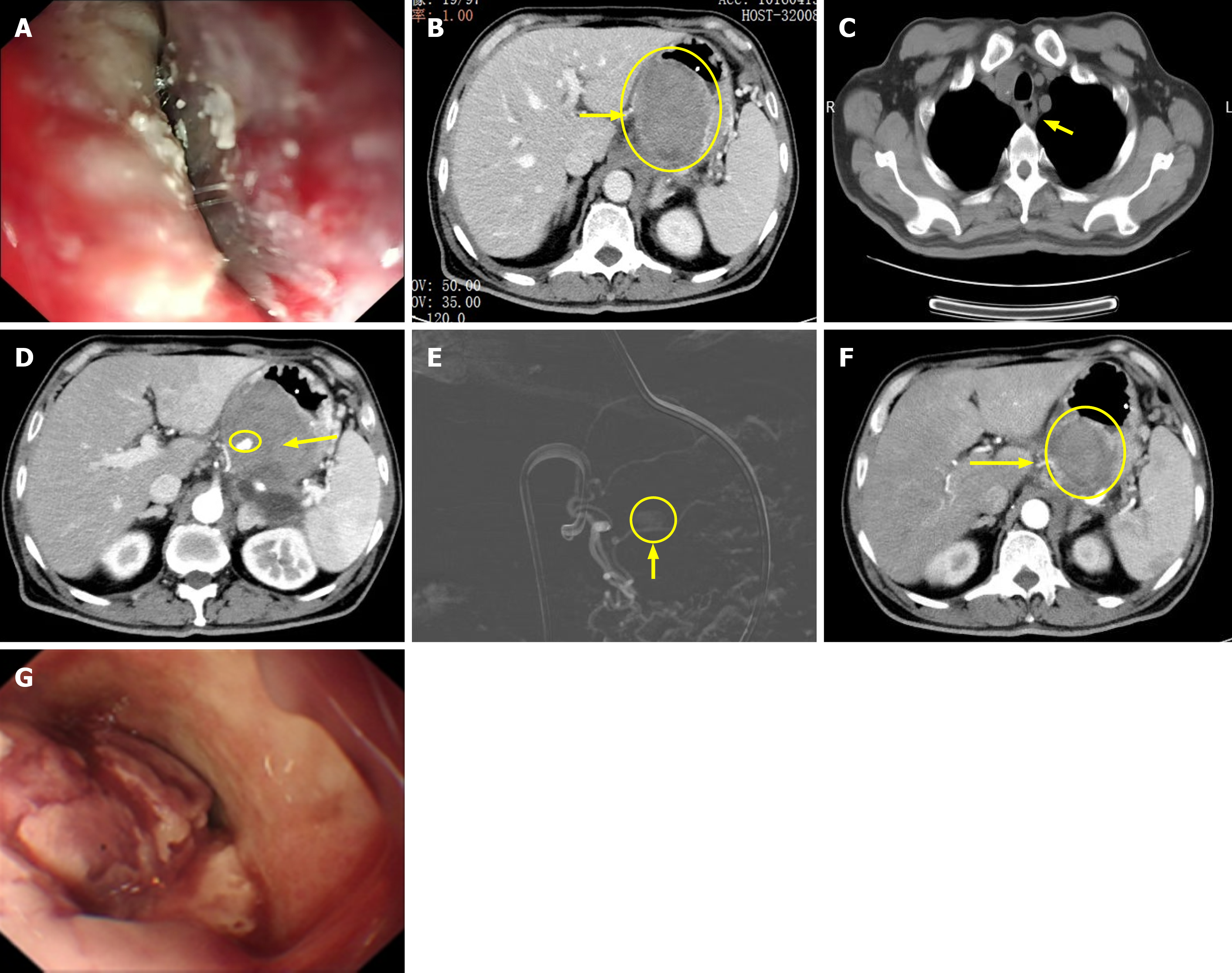
The results of an esophagogastroduodenoscopy revealed an esophageal stricture 40 centimeter from the incisors and the mirror body could not be passed (Figure 1A). Mucosal erosion was noted but without obvious rupture. An enhanced computed tomography (CT) of the chest and abdomen subsequently showed a mixed high-density mass opacity extending from the esophagus to the lesser curvature of the stomach suggestive of esophageal and gastric submucosal hematomas (Figure 1B and C). On contrast-enhanced scanning, a nodular hyperdense shadow of approximately 13 mm × 9 mm in size was seen in the left gastric artery, and vascular malformations were considered. Active hemorrhage in the hematoma area was also observed (Figure 1D).
Ming-Gao Chen, Chief Physician, Department of Vascular Interventional: The patient had no medical or trauma history. CT of the chest and abdomen suggested left gastric artery malformation. After careful consideration, we identified malformed artery rupture and bleeding as the most probable cause of the observed symptoms. Li Shi, Professor, Chief of Gastroenterology: Gastroscopy suggested esophageal stenosis and the endoscope could not be advanced. The current condition in the stomach could not be observed via gastroscopy. According to the CT results, vascular malformation was considered to cause the esophageal and gastric hematomas.
The final diagnosis of the presented case was huge esophageal and gastric submucosal hematomas associated with arterial malformations.
Considering that active bleeding was observed in the hematoma area, vascular embolization of the malformed arteries was performed first, followed by conservative treatment of the hematomas (Figure 1E). The conservative treatment regimen: The patient received high-dose proton pump inhibitor therapy and was provided with basic nutritional support while oral intake was completely prohibited. He also underwent gastrojejunal feeding tube insertion and was treated with ceftriaxone anti-infective therapy.
The patient was allowed oral intake liquid food 3 days after surgery, and normal diet was allowed 5 days later. There was no evidence of gastric leak upon commencing diet. The patient’s inflammatory markers returned to normal after 5 days, and hemoglobin remained stable. The patient’s symptoms were improved after 10 days of treatment. Follow-up CT showed that the hematomas had significantly reduced in size (Figure 1F). Re-examination gastroscopy showed that the surface of the hematoma was broken (Figure 1G), and the patient was discharged in remission after 8 days of continuous treatment.
Submucosal hematoma of the esophagus or stomach is rarely encountered[3]. There are several types which are limited to the mechanism involved in hematoma formation: Trauma, drugs, coagulation abnormality, and idiopathic. These causative factors can sometimes overlap. The most common contributing factor to esophageal or gastric submucosal hematoma is coagulopathy[4]. Traumatic submucosal hematoma can be a complication of endoscopic procedures. With the development of endoscopic technology, there have been more and more reports of traumatic hematomas[5-7]. Idiopathic mucosal hematoma is considered to be the result of a sudden increase in pressure caused by nausea and vomiting[8]. Symptoms include chest pain, epigastralgia, dysphagia, heartburn, and hematemesis. When the hematoma extends the entire esophagus, causing esophageal obstruction, the patient will experience nausea and vomiting. In the present case, we discuss the possibility of the appearance of hematoma in the following two situations: (1) The patient had huge esophageal and gastric submucosal hematomas caused by rupture and bleeding of the left gastric artery, and the hematomas gradually increased with continuous bleeding, resulting in increased gastric mucosal pressure and esophageal stenosis, and the patient presented with nausea and vomiting; and (2) The patient had a left gastric artery malformation as an underlying condition. Repeated nausea and vomiting resulted in increased intragastric and intraesophageal pressure, leading to rupture and bleeding of the malformed vessels, and finally led to submucosal hematoma in the esophagus and stomach.
Esophageal and gastric submucosal hematomas rarely coexist. Only four cases have been reported in PubMed[9-12]. These patients had coagulation disorders as an underlying condition or had been taking anticoagulant drugs for a long time, and were mostly cured through conservative treatment alone. Only one patient required interventional therapy. The past medical history of our patient was entirely negative, and laboratory examinations showed normal coagulation profiles and platelet count. In addition, our patient had not been taking any anticoagulant medications. He also had no history of vascular malformations in previous physical examinations, and the appearance of vascular malformations in the patient may be due to long-term hypertension causing endothelial damage in the blood vessels. Under the long-term impact of high pressure, some weak points in the structure of the blood vessel wall were destroyed, the elastic fibers were broken, and the of the vessel wall was reduced. With the continued action of pressure, these weak points bulge outward, forming vascular malformations. The patient had a malformation of the left gastric artery as an underlying disease, repeated nausea, and vomiting caused further increase in intraluminal pressure, resulting in the rupture and bleeding of the malformed artery, and the blood diffused and accumulated in the submucosal layer, separating the mucosal layer from muscularis layer and forming a sac, which was a submucosal hematoma. There is no established standard therapy for esophageal and gastric submucosal hematomas. In previous reports, most patients were treated with conservative treatment, and symptoms resolved within a few weeks[13]. However, our patient was found to have malformed vessels and bleeding due to rupture, and interventional therapy was necessary.
Esophageal or gastric submucosal hematoma is rare, the coexistence of both is extremely rare of which vascular mal
| 1. | Lee CC, Ravindranathan S, Choksi V, Pudussery Kattalan J, Shankar U, Kaplan S. Intraoperative Gastric Intramural Hematoma: A Rare Complication of Percutaneous Endoscopic Gastrostomy. Am J Case Rep. 2016;17:963-966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Kise Y, Suzuki R, Shimada H, Tanaka H, Oshiba G, Chino O, Makuuchi H. Idiopathic submucosal hematoma of esophagus complicated by dissecting aneurysm, followed-up endoscopically during conservative treatment. Endoscopy. 2001;33:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Wu B, Xie X, Li X, Zhu Q, Zhou C. Large intramural hematoma of the esophagus after endoscopic injection sclerotherapy: A case report. Medicine (Baltimore). 2023;102:e32752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Félix RH, Galvão BV, Góis AF. Warfarin-induced gastric intramural hematoma. Rev Assoc Med Bras (1992). 2014;60:16-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Zheng Z, Cheng X, Ding J, Ye X. Rescue endoscopic submucosal dissection for giant intramural hematoma after endoscopic mucosal resection of a small gastric polyp. Asian J Surg. 2023;46:5252-5253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Fujimoto Y, Shirozu K, Shirozu N, Akiyoshi K, Nishimura A, Kawasaki S, Motoyama Y, Kandabashi T, Iihara K, Hoka S. Esophageal Submucosal Hematoma Possibly Caused by Gastric Tube Insertion Under General Anesthesia. A A Case Rep. 2016;7:169-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Nayak HK, Krishna VP, Mohindra S, Saraswat VA, Mohindra N, Pande G. Gastric Submucosal Hematoma: An Unusual Complication of Extracorporeal Shockwave Lithotripsy. Am J Gastroenterol. 2016;111:1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Hosono I, Ogiso T, Matsuba T, Takayanagi M. [Gastric pyloric stenosis caused by submucosal hematoma in a patient with vascular type Ehlers-Danlos syndrome:a case report]. Nihon Shokakibyo Gakkai Zasshi. 2023;120:662-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Koike J, Matsushima M, Teraoka H, Igarashi M, Deguchi R, Suzuki T, Shirai T, Mine T. A case of submucosal hematoma of the esophagus and stomach, possibly caused by fish bone ingestion. Tokai J Exp Clin Med. 2010;35:46-56. [PubMed] |
| 10. | Oe S, Watanabe T, Kume K, Shibata M, Hiura M, Yoshikawa I, Harada M. A case of idiopathic gastroesophageal submucosal hematoma and its disappearance observed by endoscopy. J UOEH. 2014;36:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Iwado T, Honda H, Gotoda T. A case of idiopathic gastroesophageal submucosal hematoma in a patient with no predisposition to bleeding. DEN Open. 2024;4:e284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Kaise Y, Uno K, Ogata Y, Saito M, Jin X, Hatta W, Koike T, Ota H, Takase K, Masamune A. A case of esophagogastric submucosal hematoma with hemorrhagic shock. Clin J Gastroenterol. 2025;18:48-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Ladna M, George J. Large Esophageal Intramural Hematoma After Solid Food Ingestion in a Patient Without Identifiable Inherited or Acquired Coagulopathy. ACG Case Rep J. 2023;10:e01067. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/