Published online Jun 16, 2025. doi: 10.4253/wjge.v17.i6.106799
Revised: April 9, 2025
Accepted: May 18, 2025
Published online: June 16, 2025
Processing time: 94 Days and 21.1 Hours
Esophageal diverticulum can be broadly classified into three main types: Phar
Core Tip: Since submucosal tunneling endoscopic septum division was introduced for the endoscopic treatment of Zenker’s diverticulum, it has been proven to offer superior safety and clinical success rates. The treatment of esophageal diverticulum based on Zenker’s peroral endoscopic myotomy and its various technical modifications is collectively referred to as diverticular peroral endoscopic myotomy; however, the nomenclature and abbreviations for these techniques have not yet been fully standardized. This review will summarize the characteristics of esophageal diverticulum and key aspects of the diverticular peroral endoscopic myotomy procedure.
- Citation: Sun GY, Sun Y, Wang XZ, Jia W, Liu J, Yang Z, Gu JN. Current status of endoscopic treatment for esophageal diverticulum based on diverticular peroral endoscopic myotomy. World J Gastrointest Endosc 2025; 17(6): 106799
- URL: https://www.wjgnet.com/1948-5190/full/v17/i6/106799.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i6.106799
Twenty years ago, the introduction of flexible endoscopic septum division (FESD) revolutionized the treatment of Zenker’s diverticulum (ZD)[1,2]. Since then, a variety of cutting tools have been employed in FESD, including needles, hooks, stag-beetle knives, hybrid or dual knives, insulated-tip knives, coagulation forceps, hot biopsy forceps, and argon plasma coagulation[3]. To aid in dissection, devices like diverticuloscopes are commonly used, enabling precise delineation of the diverticulum’s extent and minimizing the risk of damaging surrounding tissues[4]. FESD has become a widely adopted approach for patients with ZD and Killian-Jamieson diverticulum (KJD), though its use is less common for mid-esophageal diverticulum and epiphrenic diverticulum. However, FESD carries a relatively high risk of recurrence and complications due to the inability to fully sever the diaphragmatic portion[5,6], and in the case of KJD surgery, there is an increased risk of damaging the recurrent laryngeal nerve. The advent of diverticular peroral endoscopic myotomy (D-POEM) offers a more promising future than FESD by providing better exposure of the diaphragm muscle and enabling complete myotomy, thereby reducing the risk of treatment failure and symptom recurrence[7]. D-POEM is a general term for endoscopic treatments of diverticulum based on the tunneling. D-POEM requires complete separation of the diaphragm to prevent increased submucosal fibrosis during recurrence, which would complicate future surgeries. While FESD can be used to relieve symptoms in cases requiring repeat surgery. Depending on the anatomical characteristics and location of the diverticulum, different surgical approaches have evolved from this technique.
Esophageal diverticulum develop through two primary mechanisms: Pulsion and traction. Pulsion occurs when increased intraluminal pressure causes the herniation of the mucosal and submucosal layers, resulting in a false diverticulum. In contrast, traction, often due to chronic inflammation, pulls the entire esophageal wall, including all layers, leading to the formation of a true diverticulum. ZD, resulting from pulsion, contains only mucosa and submucosa, and is classified as a false diverticulum. Ludlow first described it in 1767[8] and later named after the German pathologist Friedrich Albert von Zenker in 1877[9]. ZD is the most common type of esophageal diverticulum, with an incidence of approximately 0.01% to 0.11% in the population[10-12]. ZD and KJD together account for 70% of all esophageal diverticulum (Laimer’s diverticulum is negligible due to its rarity). ZD occurs at a physiological weak point known as “Killian’s triangle”, located at the junction of the hypopharynx and esophagus. This area consists of the cricopharyngeus muscle, the inferior pharyngeal constrictor muscle, and some muscle fibers of the cervical esophagus. Under normal conditions, these muscle fibers coordinate with the upper esophageal sphincter (UES) to facilitate swallowing. The formation of ZD may result from increased oropharyngeal pressure and impaired relaxation of the cricopharyngeus muscle during swallowing. These factors lead to incomplete relaxation of the UES, causing the esophageal mucosa to herniate through the relatively weak posterior wall of the pharyngoesophageal junction[13-15]. Early studies on UES function have confirmed its role as a critical barrier against gastric acid reflux[16]. The two factors mentioned above may be the primary causes of dysphagia and gastroesophageal reflux becoming the main symptoms. Although malignant transformation of ZD is exceedingly rare, the risk ranges from 0.3% to 7%[17,18]. Advanced age, larger diverticulum size, and longer disease duration are risk factors for malignancy in ZD, likely due to chronic irritation and inflammation caused by the prolonged accumulation of food and liquids[19-21].
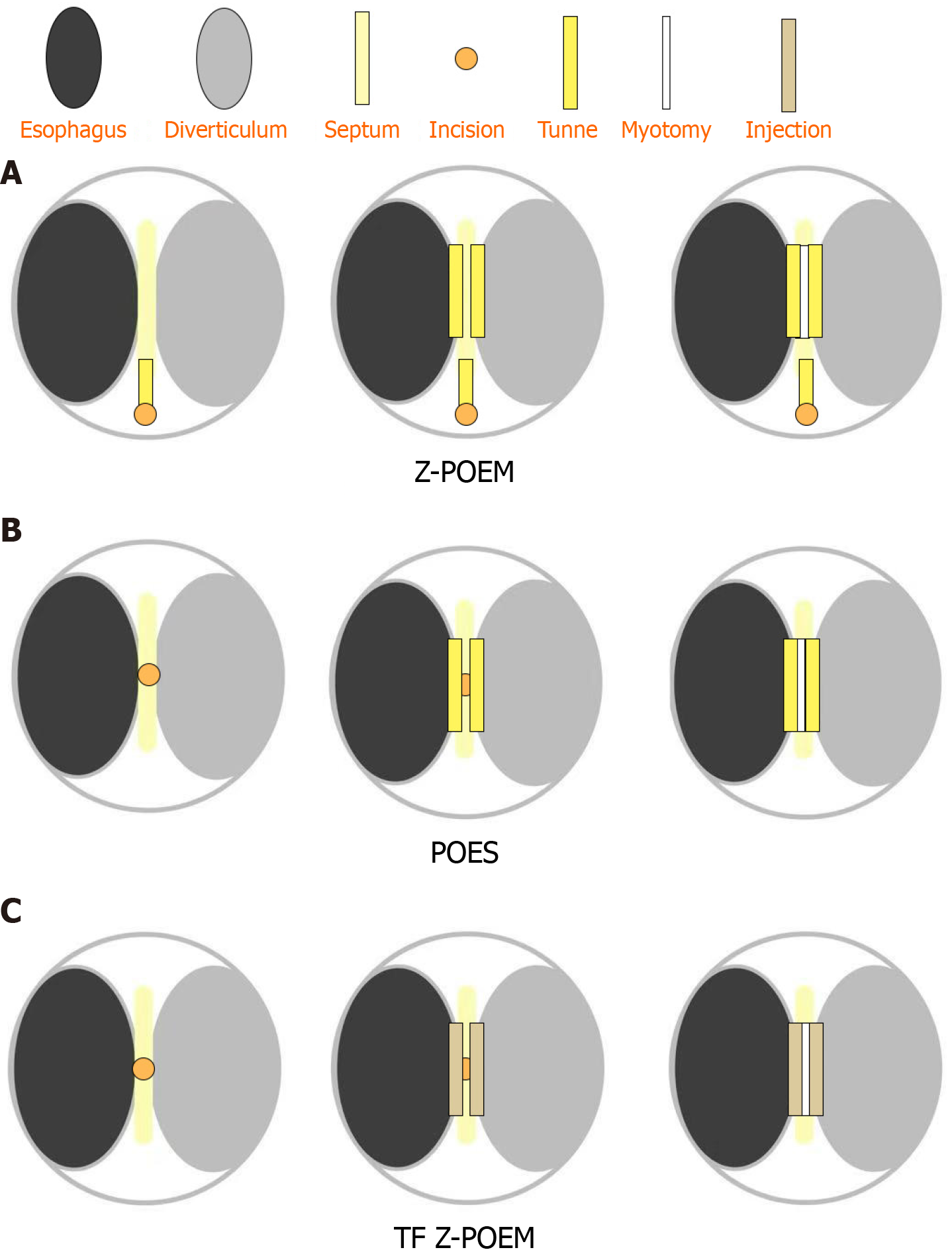
The general principle for ZD management is to intervene only in symptomatic cases[22]. Surgical procedures, refined through long-term practice, achieve treatment success rates of approximately 80% to 100% by removing the diverticulum or correcting anatomical abnormalities[23]. However, postoperative complications can occur in up to 11% of cases, and the recurrence rate remains close to 10%[24]. In 2016, Li et al[25] first used the submucosal tunneling endoscopic septum division technique to treat ZD, later known as Zenker’s peroral endoscopic myotomy (Z-POEM). The Z-POEM technique involves submucosal injection and mucosal incision 3 cm proximal to the diverticulum septum, followed by dissection of the submucosal fibers to create a tunnel between the esophagus and the diverticulum side of the septum. The septum is then divided, completing the myotomy, and the tunnel entry is finally closed. Z-POEM pioneered the tunneling approach for treating ZD. In contrast, the subsequent peroral endoscopic septotomy (POES) for ZD (ZD-POES, also referred to as Z-POES or simply POES) simplifies the procedure by initiating the tunneling directly at the septum, simplifying the procedure and broadening its range of indications[26-28]. Mavrogenis G and colleagues proposed replacing the creation of tunneling with a submucosal cushion formed by injecting a mixture of hydroxyethyl starch and indigo carmine[29,30]. This led to the development of the single tunnel technique (ST Z-POEM) and the tunnel-free technique (TF Z-POEM)[29,30]. Subsequently, they conducted a single-center retrospective study comparing Z-POEM (more accurately referred to as POES), ST Z-POEM, and TF Z-POEM techniques. The results demonstrated that, while maintaining safety, the modified techniques significantly reduced operative time[31]. Estevinho et al[32] described TF Z-POEM as “readily” peroral endoscopic septotomy (R-POES) and conducted a retrospective analysis of four cases. R-POES simplified the procedure, significantly reducing the operative time (mean duration: 9 ± 5 minutes) and avoiding potential mucosal injury associated with submucosal tunneling[32]. A 2025 meta-analysis showed that Z-POEM has a higher clinical success rate compared to FESD, while the technical success rate, operative time, adverse events, and symptom recurrence rates are similar[33]. Cartoon illustration of the D-POEM technique for ZD (Figure 1).
In 1983, Ekberg and Nylander[34] first described the KJD as an anterolateral pharyngoesophageal pouch and classified it as a false diverticulum. KJD is named in honor of Gustav Killian and James Jamieson for their significant contributions to the anatomy of the cervical esophagus. KJD arises from a prominent anatomical weak spot, located beneath the transverse fibers of the cricopharyngeus muscle and laterally to the longitudinal fibers of the cervical esophagus, forming an inverted triangle. KJD is more commonly found on the left side, possibly due to the thinner muscular layer on that side. Right-sided and bilateral cases of KJD have also been reported, but they are rare[35]. Additionally, concurrent occurrences of ZD and KJD in the same patient have been reported. However, current studies have not established a definitive correlation between the occurrence of the two[36].
Compared to ZD, a smaller proportion of patients with KJD are symptomatic, with dysphagia being the primary complaint and gastroesophageal reflux rarely reported. The average age at onset for KJD is 58 years, compared to 70 years for ZD[37,38]. Additionally, imaging studies have shown that the incidence of KJD is about a quarter of that of ZD. In general, KJD is smaller than ZD, with an average size of approximately 1.4 cm, compared to 2.5 cm for ZD[39]. To date, there have been no reports of malignant transformation associated with KJD.
KJD presents greater therapeutic challenges than ZD, due to its extension into the upper mediastinum and its close proximity to the recurrent laryngeal nerve. Thus, accurately differentiating between these two types of diverticulum is essential to prevent recurrent laryngeal nerve injury during surgery. A barium swallow is generally useful for delineating the relationship between the diverticulum’s opening and the cricopharyngeal muscle, while a computed tomography scan can provide additional diagnostic clarity. During cervical ultrasound, the anatomical location of KJD can easily lead to misdiagnosis as a thyroid nodule. Two case reports have suggested that dynamic ultrasound performed during soda ingestion can effectively differentiate KJD from thyroid nodules[40,41]. Nonetheless, ultrasound practitioners should exercise caution to avoid unnecessary thyroid biopsies[42]. Historically, open surgical resection has been the treatment of choice for KJD. Given the anatomical similarity between KJD and ZD, FESD is also applicable to KJD[43-45]. However, due to the need to avoid recurrent laryngeal nerve injury, a full-length myotomy comparable to that achieved in open surgery is not feasible, leading to a relatively higher recurrence rate[46]. Z-POEM and Z-POES have also been adapted for use in KJD, and are thus referred to as KJD-POEM or KJD-POES[47,48]. Assefa et al[49] collectively referred to these endoscopic approaches as KJD-POEM. Among the cases, all 8 FESD and 5 KJD-POES procedures achieved both clinical and technical success. Some patients were initially diagnosed with ZD based on barium esophagography, only to be found intraoperatively to have KJD[50,51]. Modayil et al[6] compared FESD with endoscopic tunneling diverticulotomy (including KJD-POEM and KJD-POES, favoring the latter), and noted one case in the FESD group with persistent dysphagia. Some studies suggest that under standard endoscopic orientation, ZD typically appears at the 6:00 position, while the more commonly left-sided KJD is seen at the 9:00 to 10:00 position[52]. Palisade vessels have also been noted to act as a landmark for the UES during endoscopy, helping to distinguish ZD from KJD[53]. Endoscopic findings, when combined with the gold-standard barium swallow, may enhance diagnostic accuracy in the future[54].
Laimer’s diverticulum is the rarest form of pharyngoesophageal diverticulum, with only five cases documented in the literature to date[55-59]. Laimer’s diverticulum is anatomically adjacent to both ZD and KJD, arising from the area between the cricopharyngeus muscle and the longitudinal muscle of the esophagus, known as the Laimer-Haeckerman triangle. Unlike ZD and KJD, Laimer’s diverticulum is a true diverticulum, involving all layers of the esophageal wall. Treatment typically involves open surgery through the neck, and currently, no endoscopic treatments have been reported for this condition. Due to its rarity and the diagnostic and therapeutic challenges it presents, further research and clinical experience are needed to improve our understanding and management of this type of diverticulum.
The mid-esophageal diverticulum, also referred to as Rokitansky’s diverticulum, typically occurs as a protrusion in the mid-esophagus. Its diameter is usually less than 2 centimeters. The traditional view suggests that its formation is due to chronic inflammation and fibrosis, leading to scar contracture or tumor infiltration, which results in a true diverticulum that includes all layers of the esophageal wall. Mid-esophageal traction diverticulum are most commonly located on the right side, owing to the close anatomical relationship between the esophagus and the subcarinal lymph nodes in this region[60]. However, recent studies suggest that the formation of the mid-esophageal diverticulum may also be associated with increased intraluminal pressure caused by esophageal motility disorders (EMD)[22,61]. A relatively small mid-esophageal diverticulum was successfully treated with FESD in 2004, resulting in favorable long-term outcomes[62]. Salvage peroral endoscopic myotomy (S-POEM) was first applied to a patient with significant submucosal fibrosis due to prior treatments, with a second submucosal tunnel created on the opposite side for treatment[63]. Subsequently, it was also applied to a patient with a mid-esophageal diverticulum. Although high-resolution manometry (HRM) did not show primary motor dysfunction, S-POEM was performed on the opposite side of the diverticulum, improving the patient’s symptoms[64]. In 2016, two cases of giant mid-esophageal diverticulum were reported, where patients successfully resolved their dysphagia through D-POEM treatment, demonstrating the efficacy of D-POEM in managing mid-esophageal diverticulum[65]. D-POEM avoids the postoperative complications associated with open surgery, such as tracheoesophageal fistula, pneumothorax, and empyema. In 2024, Wang et al[66] reported a case of a patient with an enlarging thoracic mid-esophageal diverticulum compressing the heart. The team employed endoscopic submucosal dissection (ESD) combined with metal clip closure to prevent further esophageal dilation and cardiac compression that could potentially be caused by D-POEM. Simple mucosal dissection is typically sufficient for pseudodiverticula, whereas for true diverticulum, part of the muscularis propria must also be dissected[67]. The ESD combined with metal clip closure approach represents a novel attempt tailored to a specific patient. However, further research and validation are needed to assess its applicability to the broader diverticulum patient population.
Epiphrenic diverticulum refers to a false diverticulum located within 10 cm of the distal esophagus, near the lower esophageal sphincter (LES), with the most common site being 4 cm to 8 cm above the gastroesophageal junction[68-70]. The majority of the epiphrenic diverticulum are located on the right side of the esophagus. This may be attributed to the adjacent left-sided mediastinal structures restricting diverticulum formation on that side[71,72]. Epiphrenic diverticulum is associated with an increased risk of malignancy, estimated at approximately 0.6%[17]. Therefore, regular follow-up for these patients is crucial. Esophagram, upper gastrointestinal endoscopy, and esophageal HRM are standard diagnostic procedures. Over 75% of patients with epiphrenic diverticulum have underlying EMD[73]. Achalasia is the most commonly associated EMD, followed by hypertensive LES, ‘nutcracker’ esophagus, and diffuse esophageal spasm. The onset of symptoms in patients with epiphrenic diverticulum is more likely related to the size of the diverticulum rather than underlying EMD.
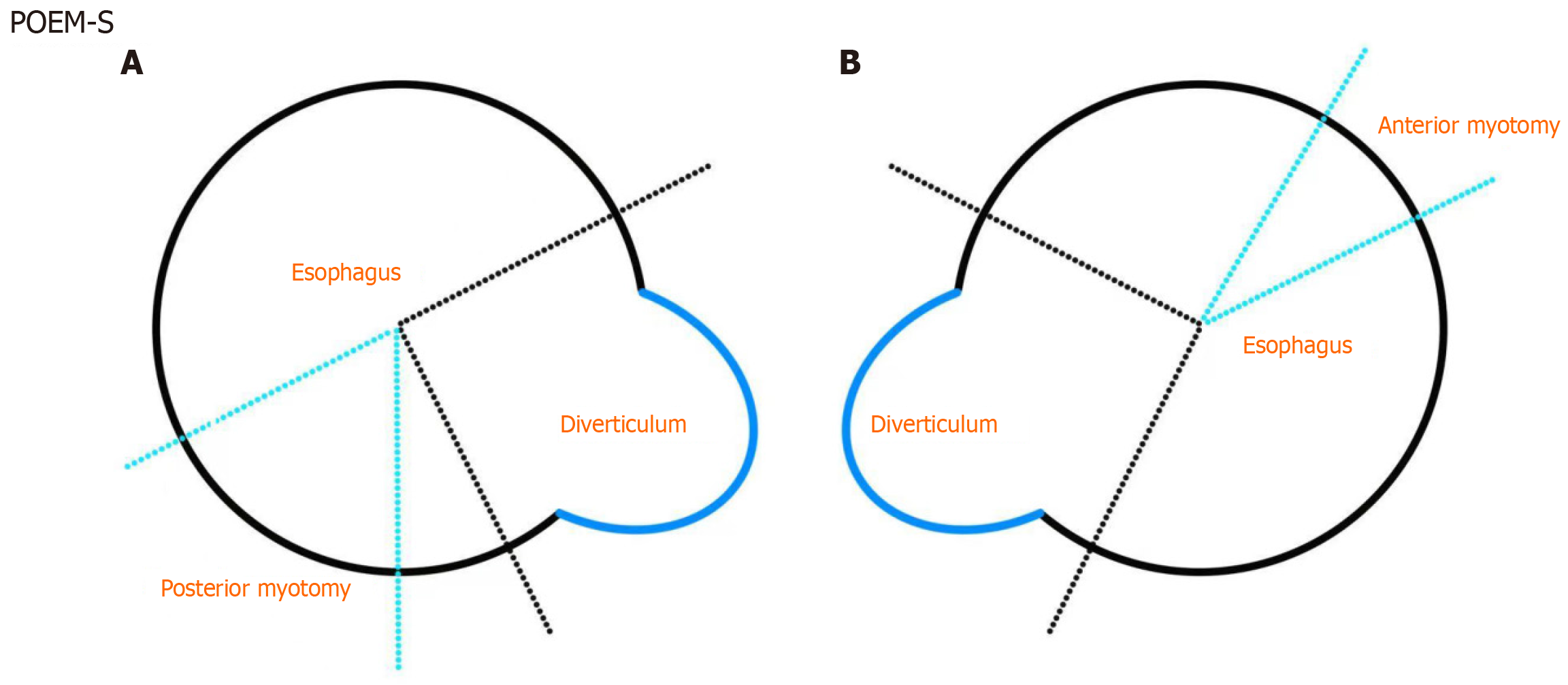
The treatment of epiphrenic diverticulum can be based on D-POEM technique[7,74,75]. In cases of EMD, the endoscopic treatment of epiphrenic diverticulum differs from that of other types of diverticulum. LES myotomy can effectively address the underlying motility disorder at its pathological origin. The current debate centers around whether to combine standard D-POEM. One approach is standard POEM (POEM-S or S-POEM)[76-80], which involves reducing LES pressure without septotomy and has been shown to be effective in relieving symptoms (Figure 2). An alternative is to combine D-POEM with LES myotomy (POEM + S or E-POEM): Septotomy is technically straightforward and can be performed within the same tunnel, while preserving the intact diverticulum and septum may increase the risk of recurrence[81-83]. In the POEM-S technique, the diverticulum is typically avoided, and standard POEM is performed only on the opposite side. In POEM + S, the submucosal tunnel is extended along the same side as the diverticulum, followed by LES myotomy (extending at least 2 cm beyond the gastroesophageal junction) and septotomy. A 2024 multicenter study comparing POEM + S and POEM-S for the treatment of epiphrenic diverticulum found no significant differences in clinical success rates (POEM + S: 89.6% vs POEM-S: 89.2%, P = 1) and adverse event rates (POEM + S: 4.2% vs POEM-S: 8.1%, P = 0.6)[84]. Due to the close relationship between esophageal diverticulum and EMD, and the fact that HRM cannot be applied in some cases, endoscopic treatment for epiphrenic diverticulum without accompanying EMD is still primarily based on POEM + S. Even when preoperative HRM does not clearly confirm the presence of motility disorders, Nabi et al[85] still perform LES myotomy as part of the procedure. A retrospective study by Noh et al[86], which applied the endoscopic functional luminal imaging probe (EndoFLIP) based on HRM, demonstrated the value of EndoFLIP and the indications for POEM + S in epiphrenic diverticulum without accompanying EMD. Current evidence suggests that approximately 17% to 40% of patients experience symptomatic reflux after POEM[87]. Due to the implementation of LES myotomy, both POEM + S and POEM-S increase the risk of postoperative reflux esophagitis. Although reflux esophagitis is common, most cases of gastroesophageal reflux are asymptomatic[79,84-86].
Compared with traditional surgical procedures, endoscopic treatment of esophageal diverticulum, as a minimally invasive approach, has gained increasing popularity due to its reduced trauma, faster recovery, and lower risk of complications. During the FESD era, treatment focused primarily on the mechanical separation of the septum using various instruments. However, in the current era of D-POEM technology, the focus is more on achieving complete division of the septum muscles within the tunnel, representing a more minimally invasive approach. Given the close connection between the epiphrenic diverticulum and motility disorders, the emergence of S-POEM and S + POEM represents a physiological, mechanism-based treatment approach. We performed a PubMed literature search for studies on the treatment of esophageal diverticulum using D-POEM, covering publications up to March 2025. The primary search term was “D-POEM”, and studies were included if they covered at least two of the three types of esophageal diver
| No. | Publication year | Researchers | Study type | Diverticulum type | Type of poem | Technical/clinical success rate and follow-up duration | Adverse events |
| 1 | 2019 | Yang et al[7] | Multicenter and retrospective | 7 ZD, 1 MED, 3 ED | D-POEM | 90.9%/100% (patients who successfully underwent POEM) (12 months) | None |
| 2 | 2019 | Maydeo et al[74] | Prospective | 20 ZD, 5 ED | D-POEM | 100%/86% (12 months) | None |
| 3 | 2020 | Basile et al[83] | Retrospective | 7 MED and ED | POEM + S (all diverticulum are associated with EMD) | 100%/85.71% (12 months) | None |
| 4 | 2021 | Zeng et al[88] | Retrospective | 2 ZD, 5 MED, 3 ED | D-POEM (POEM + S performed for ED with achalasia) | 100%/90% (11.0 months) (IQR: 10.25-17.25 months) | Emphysema (n = 1, 10%) |
| 5 | 2022 | Samanta et al[89] | Retrospective | 3ZD, 2ED | POEM (POEM + S for ED, larger diverticulum underwent POES) | 100%/100% (9.33 months) (range: 3.27-11 months) | Emphysema (n = 1, 20%); mucosal injury (n = 1, 20%) |
| 6 | 2024 | Ren et al[90] | Multicenter and prospective | 12 ZD, 12 MED, 10 ED | D-POEM (POEM + S performed for diverticulum with coexistent achalasia) | 100%/88.2% (25 months) (range: 3-68 months) | Emphysema (n = 5, 14.7%); mucosal injury (n = 1, 2.9%) |
| 1. | Ishioka S, Sakai P, Maluf Filho F, Melo JM. Endoscopic incision of Zenker's diverticula. Endoscopy. 1995;27:433-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 116] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Mulder CJ, den Hartog G, Robijn RJ, Thies JE. Flexible endoscopic treatment of Zenker's diverticulum: a new approach. Endoscopy. 1995;27:438-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 113] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Kenarli K, Ödemiş B. Flexible endoscopic treatment of Zenker's diverticulum: a retrospective study in a single center from Turkey. Clin Endosc. 2025;58:261-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Orbán-Szilágyi Á, Bakucz T, Gyökeres T. [Characteristics and outcomes of 47, conventional flexible endoscopic interventions for Zenker's diverticulum Review of therapeutic options]. Orv Hetil. 2022;163:677-687. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Ishaq S, Hassan C, Antonello A, Tanner K, Bellisario C, Battaglia G, Anderloni A, Correale L, Sharma P, Baron TH, Repici A. Flexible endoscopic treatment for Zenker's diverticulum: a systematic review and meta-analysis. Gastrointest Endosc. 2016;83:1076-1089.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 123] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 6. | Modayil RJ, Zhang X, Ali M, Das K, Gurram K, Stavropoulos SN. Endoscopic diverticulotomy for Killian-Jamieson diverticulum: mid-term outcome and description of an ultra-short tunnel technique. Endosc Int Open. 2022;10:E119-E126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Yang J, Zeng X, Yuan X, Chang K, Sanaei O, Fayad L, Kumbhari V, Singh V, Kalloo AN, Hu B, Khashab MA. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy. 2019;51:346-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 83] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 8. | Ludlow A. A case of obstructed deglutition from a preternatural dilatation of and bag formed in the pharynx. Med Observ Inq. 1769;3:85-101. Available from: https://cir.nii.ac.jp/crid/1572543024813430912?lang=en. |
| 9. | Zenker FA, Ziemssen H. Krankheiten des Oesophagus. [cited May 09, 2025]. Available from: https://www.abebooks.de/Krankheiten-Oesophagus-Zenker-Friedrich-Albert-Ziemssen/1602987735/bd. |
| 10. | Carrère N, Pradère B. [Esophageal diverticula]. J Chir (Paris). 2004;141:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Maran AG, Wilson JA, Al Muhanna AH. Pharyngeal diverticula. Clin Otolaryngol Allied Sci. 1986;11:219-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 49] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Wheeler D. Diverticula of the foregut. Radiology. 1947;49:476-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Gutschow C. [Update Esophageal Diverticula]. Ther Umsch. 2022;79:141-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Cook IJ, Gabb M, Panagopoulos V, Jamieson GG, Dodds WJ, Dent J, Shearman DJ. Pharyngeal (Zenker's) diverticulum is a disorder of upper esophageal sphincter opening. Gastroenterology. 1992;103:1229-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 181] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 15. | Bizzotto A, Iacopini F, Landi R, Costamagna G. Zenker's diverticulum: exploring treatment options. Acta Otorhinolaryngol Ital. 2013;33:219-229. [PubMed] |
| 16. | Gerhardt DC, Shuck TJ, Bordeaux RA, Winship DH. Human upper esophageal sphincter. Response to volume, osmotic, and acid stimuli. Gastroenterology. 1978;75:268-274. [PubMed] [DOI] [Full Text] |
| 17. | Herbella FA, Dubecz A, Patti MG. Esophageal diverticula and cancer. Dis Esophagus. 2012;25:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Fox SS, Nagasawa KK, Williams ZF. Incidental Squamous Cell Carcinoma In Situ in a Large Pharyngoesophageal (Zenker's) Diverticulum. Am Surg. 2017;83:e288-e290. [PubMed] |
| 19. | Brücher BL, Sarbia M, Oestreicher E, Molls M, Burian M, Biemer E, Stein HJ. Squamous cell carcinoma and Zenker diverticulum. Dis Esophagus. 2007;20:75-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Hajjar WM, Almutairi OT, Jameel MA, Al-Nassar SA, Raddaoui E, Hajjar AW. Squamous Cell Carcinoma Arising in Zenker's Diverticulum: A Case Report and Review of the Literature. Turk Thorac J. 2018;19:228-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Agarwal P, Jain N, Jindal S, Goel V, Jain P. Squamous Cell Carcinoma Arising in a Zenker's Diverticulum. Cureus. 2024;16:e53583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Herbella FA, Patti MG. Modern pathophysiology and treatment of esophageal diverticula. Langenbecks Arch Surg. 2012;397:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Feußner H, Hüser N, Wilhelm D, Fingerle A, Jell A, Friess H, Bajbouj M. [Surgical treatment of esophageal diverticula : Endoscopic or open approach?]. Chirurg. 2017;88:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Dell'Anna G, Fasulo E, Fanizza J, Barà R, Vespa E, Barchi A, Cecinato P, Fuccio L, Annese V, Malesci A, Azzolini F, Danese S, Mandarino FV. The Endoscopic Management of Zenker's Diverticulum: A Comprehensive Review. Diagnostics (Basel). 2024;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Li QL, Chen WF, Zhang XC, Cai MY, Zhang YQ, Hu JW, He MJ, Yao LQ, Zhou PH, Xu MD. Submucosal Tunneling Endoscopic Septum Division: A Novel Technique for Treating Zenker's Diverticulum. Gastroenterology. 2016;151:1071-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 26. | Brewer Gutierrez OI, Ichkhanian Y, Spadaccini M, Vosoughi K, Repici A, Khashab MA. Zenker's Diverticulum Per-Oral Endoscopic Myotomy Techniques: Changing Paradigms. Gastroenterology. 2019;156:2134-2135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 27. | Repici A, Spadaccini M, Belletrutti PJ, Galtieri PA, Fugazza A, Anderloni A, Carrara S, Di Leo M, Pellegatta G, Cappello A, Castoro C, Ichkhanian Y, Khashab MA, Maselli R. Peroral endoscopic septotomy for short-septum Zenker's diverticulum. Endoscopy. 2020;52:563-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Mavrogenis G, Tsevgas I, Zachariadis D, Bazerbachi F. Mucosotomy at the top of the septum facilitates tunneling and clipping during peroral endoscopic myotomy for Zenker's diverticulum (Z-POEM). Ann Gastroenterol. 2020;33:101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Mavrogenis G, Bazerbachi F. Peroral endoscopic myotomy for Zenker's diverticulum without tunneling. Endoscopy. 2023;55:1148-1150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 30. | Mavrogenis G, Maurommatis E, Koumentakis C, Tsevgas I, Zachariadis D, Bazerbachi F. Single-tunnel Zenker's diverticulum peroral endoscopic myotomy. Endoscopy. 2023;55:E604-E605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 31. | Mavrogenis G, Zachou M, Tsevgas I, Markoglou K, Zachariadis D, Spanomanoli A, Chatzis M, Bazerbachi F. Tunnel-free peroral endoscopic myotomy reduces procedural time and maintains efficacy in Zenker's diverticulum. Ann Gastroenterol. 2024;37:509-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 32. | Estevinho MM, Pinho R, Rodrigues J, Correia J, Freitas T. Tunneling-free peroral endoscopic septotomy for Zenker diverticulum. VideoGIE. 2023;8:295-297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 33. | Singh S, Chandan S, Bapaye J, Brar HS, Mohammed A, Kassab LL, Bhat I, Singh S, Bapaye A, Yang D. Peroral endoscopic myotomy (Z-POEM) versus flexible endoscopic septotomy (FES) for treatment of Zenker's diverticulum: does either make the cut? A systematic review and meta-analysis of outcomes. Ann Gastroenterol. 2025;38:20-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 34. | Ekberg O, Nylander G. Lateral diverticula from the pharyngo-esophageal junction area. Radiology. 1983;146:117-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 69] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Saisho K, Matono S, Tanaka T, Mori N, Hino H, Fujisaki M, Nakagawa M, Fujita F, Akagi Y. Surgery for Killian-Jamieson diverticulum: a report of two cases. Surg Case Rep. 2020;6:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 36. | Stewart KE, Smith DRK, Woolley SL. Simultaneously occurring Zenker's diverticulum and Killian-Jamieson diverticulum: case report and literature review. J Laryngol Otol. 2017;131:661-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 37. | Siddiq MA, Sood S, Strachan D. Pharyngeal pouch (Zenker's diverticulum). Postgrad Med J. 2001;77:506-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 120] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 38. | Haddad N, Agarwal P, Levi JR, Tracy JC, Tracy LF. Presentation and Management of Killian Jamieson Diverticulum: A Comprehensive Literature Review. Ann Otol Rhinol Laryngol. 2020;129:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 39. | Rubesin SE, Levine MS. Killian-Jamieson diverticula: radiographic findings in 16 patients. AJR Am J Roentgenol. 2001;177:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 72] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 40. | Kim TH, Kim S, Chang KS. Simple method of using soda for distinguishing Killian-Jamieson diverticulum from a thyroid nodule. Endocrine. 2015;48:351-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 41. | Liang TJ, Liu SI, Chiang CL. How Soda Ingestion Facilitates the Distinction between a Killian-Jamieson Diverticulum and a Malignant Thyroid Nodule. Diagnostics (Basel). 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 42. | Kim HK, Lee JI, Jang HW, Bae SY, Lee JH, Kim YS, Shin JH, Kim SW, Chung JH. Characteristics of Killian-Jamieson diverticula mimicking a thyroid nodule. Head Neck. 2012;34:599-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Lee CK, Chung IK, Park JY, Lee TH, Lee SH, Park SH, Kim HS, Kim SJ. Endoscopic diverticulotomy with an isolated-tip needle-knife papillotome (Iso-Tome) and a fitted overtube for the treatment of a Killian-Jamieson diverticulum. World J Gastroenterol. 2008;14:6589-6592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 44. | Tang SJ, Tang L, Chen E, Myers LL. Flexible endoscopic Killian-Jamieson diverticulotomy and literature review (with video). Gastrointest Endosc. 2008;68:790-793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Yang D, Draganov PV. Endoscopic Killian-Jamieson diverticulotomy using a scissor-type electrosurgical knife. Endoscopy. 2018;50:E175-E176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 46. | Johnson CM, Postma GN. Zenker Diverticulum--Which Surgical Approach Is Superior? JAMA Otolaryngol Head Neck Surg. 2016;142:401-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Zakaria A, Barawi M. Endoscopic treatment of Killian-Jamieson diverticulum using submucosal tunneling diverticulotomy technique. VideoGIE. 2020;5:525-526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 48. | Wander P, Trindade A, Benias PC. Peroral endoscopic myotomy approach to treating a Killian-Jamieson diverticulum. Endoscopy. 2020;52:E456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 49. | Assefa RL, Bejjani M, Mehta A, Shrigiriwar A, Fayyaz F, Shimamura Y, Inoue H, Mandarino FV, Azzolini F, Bowers SP, Li Z, Robles-Medranda C, Arevalo M, Dhir V, Andrisani G, Tantau A, Lajin M, Sampath K, Khashab MA. Peroral endoscopic myotomy as a treatment for Killian-Jamieson diverticulum (KJ-POEM). Endosc Int Open. 2024;12:E1214-E1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 50. | Sanders D, Murray T, Donnellan F. Endoscopic management of Killian-Jamieson diverticulum. VideoGIE. 2019;4:364-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 51. | Watanabe Y, Taniyama Y, Koseki K, Ishida H, Ozawa Y, Okamoto H, Sato C, Unno M, Kamei T. Distinguishing Killian-Jamieson diverticulum from Zenker's diverticulum. Surg Case Rep. 2023;9:21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 52. | Tanaka I, Shimamura Y, Inoue H, Azuma D, Ushikubo K, Yamamoto K, Okada H, Kimoto Y, Nishikawa Y, Owada K, Tanabe M, Onimaru M. Feasibility and safety of per-oral endoscopic septotomy for Killian-Jamieson diverticulum: Case series with video. Dig Endosc. 2024;36:895-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 53. | Kurahashi Y, Hojo Y, Nakamura T, Kumamoto T, Nakanishi Y, Ishida Y, Shinohara H. Endoscopic observation of the palisade vessels in Killian-Jamieson diverticulum was useful for diagnosis and surgical treatment: a case report. Surg Case Rep. 2020;6:192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 54. | Sun G, Jia W, Yang Z, Liu J, Sun Y. Endoscopic Treatment and Considerations for a Rare of Killian-Jamieson Diverticulum: A Case Report. JGH Open. 2025;9:e70127. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 55. | Boysen M, Aasen S, Løtveit T, Bakka A. Two simultaneously occurring hypopharyngo-oesophageal diverticula. J Laryngol Otol. 1993;107:49-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 56. | Kobayashi M IS, Sawada T, Deguchi M, Lin S, Okada D, Ohe H, Tsujino N. [A case of diverticulum originating from the Laimer's triangle (in Japanese)]. Geka Shinryou. 1993;35:889-892. |
| 57. | Kumoi K, Ohtsuki N, Teramoto Y. Pharyngo-esophageal diverticulum arising from Laimer's triangle. Eur Arch Otorhinolaryngol. 2001;258:184-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 58. | Ujiie N, Taniyama Y, Sato C, Kamei T. Surgical Intervention for Laimer's Diverticulum, a Rare Type of Pharyngoesophageal Diverticulum: A Case Report. OTO Open. 2019;3:2473974X19847670. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 59. | Guo TT, Dong YB, Liu YH, Lu C, Li WX. Diagnosis and Open Surgical Management of Laimer's Diverticulum: Case Series and Review of the Literature. Ear Nose Throat J. 2023;1455613231202245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 60. | Ballehaninna UK, Shaw JP, Brichkov I. Traction esophageal diverticulum: a rare cause of gastro-intestinal bleeding. Springerplus. 2012;1:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 61. | do Nascimento FA, Lemme EM, Costa MM. Esophageal diverticula: pathogenesis, clinical aspects, and natural history. Dysphagia. 2006;21:198-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 62. | Schubert D, Kuhn R, Nestler G, Lippert H, Pross M. Endoscopic treatment of a mid-esophageal diverticulum. Endoscopy. 2004;36:735-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 63. | Kedia P, Sharaiha R, Kumta NA, Lambroza A, Kahaleh M. Salvage posterior peroral endoscopic myotomy. Gastrointest Endosc. 2015;81:220-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 64. | Sato H, Sato Y, Takeuchi M, Takahashi K, Takeda SR, Inoue H, Kobayashi M. Salvage peroral endoscopic myotomy for esophageal diverticulum. Endoscopy. 2015;47 Suppl 1 UCTN:E14-E15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 65. | Mou Y, Zeng H, Wang Q, Yi H, Liu W, Wen D, Tang C, Hu B. Giant mid-esophageal diverticula successfully treated by per-oral endoscopic myotomy. Surg Endosc. 2016;30:335-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 66. | Wang Z, Bai B, Jiang J, Xu H, Zhao Q, Li B. Endoscopic submucosal dissection with metal clip closure for the treatment of a mid-esophageal diverticulum: a case report. Endoscopy. 2024;56:E768-E769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 67. | Shi L, Long F, Xu H, Chen N, Ge J, Jia R, Jiang J. Chronic esophagotracheal fistula secondary to esophageal diverticulum successfully treated by endoscopic submucosal dissection and dual action tissue clip. Endoscopy. 2023;55:E1128-E1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 68. | Nadaleto BF, Herbella FAM, Patti MG. Treatment of Achalasia and Epiphrenic Diverticulum. World J Surg. 2022;46:1547-1553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 69. | Nehra D, Lord RV, DeMeester TR, Theisen J, Peters JH, Crookes PF, Bremner CG. Physiologic basis for the treatment of epiphrenic diverticulum. Ann Surg. 2002;235:346-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 115] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 70. | Sato H, Takeuchi M, Hashimoto S, Mizuno KI, Furukawa K, Sato A, Yokoyama J, Terai S. Esophageal diverticulum: New perspectives in the era of minimally invasive endoscopic treatment. World J Gastroenterol. 2019;25:1457-1464. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 54] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (4)] |
| 71. | Fasano NC, Levine MS, Rubesin SE, Redfern RO, Laufer I. Epiphrenic diverticulum: clinical and radiographic findings in 27 patients. Dysphagia. 2003;18:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 72. | Bruggeman LL, Seaman WB. Epiphrenic diverticula. An analysis of 80 cases. Am J Roentgenol Radium Ther Nucl Med. 1973;119:266-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 31] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 73. | Zaninotto G, Portale G, Costantini M, Zanatta L, Salvador R, Ruol A. Therapeutic strategies for epiphrenic diverticula: systematic review. World J Surg. 2011;35:1447-1453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 74. | Maydeo A, Patil GK, Dalal A. Operative technical tricks and 12-month outcomes of diverticular peroral endoscopic myotomy (D-POEM) in patients with symptomatic esophageal diverticula. Endoscopy. 2019;51:1136-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 75. | Barquero Declara D, Juan Juan A, Caballero Suárez N, Blasco Pelicano A, Mata Bilbao A. Epiphrenic diverticulum: is diverticular peroral endoscopic myotomy (D-POEM) enough or do we need to go one step forward? Rev Esp Enferm Dig. 2025;117:234-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 76. | Sato H, Sato Y, Hashimoto S, Mizuno K, Nakajima N, Terai S. Gastrointestinal: Salvage peroral endoscopic myotomy for outflow obstruction with growing esophageal diverticulum. J Gastroenterol Hepatol. 2016;31:1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 77. | Otani K, Tanaka S, Kawara F, Fujikawa J, Sawada A, Uemura R, Tanigawa T, Watanabe T, Azuma T, Fujiwara Y. Distal esophageal spasm with multiple esophageal diverticula successfully treated by peroral endoscopic myotomy. Clin J Gastroenterol. 2017;10:442-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 78. | Demeter M, Bánovčin P Jr, Ďuriček M, Kunda R, Hyrdel R. Peroral endoscopic myotomy in achalasia and large epiphrenic diverticulum. Dig Endosc. 2018;30:260-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 79. | Demeter M, Ďuriček M, Vorčák M, Hyrdel R, Kunda R, Bánovčin P. S-POEM in treatment of achalasia and esophageal epiphrenic diverticula - single center experience. Scand J Gastroenterol. 2020;55:509-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 80. | Kinoshita M, Tanaka S, Kawara F, Sakaguchi H, Abe H, Ariyoshi R, Toyonaga T, Kodama Y. Peroral endoscopic myotomy alone is effective for esophageal motility disorders and esophageal epiphrenic diverticulum: a retrospective single-center study. Surg Endosc. 2020;34:5447-5454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 81. | Li X, Zhang W, Yang J, Wang X, Dang Y, Hu B, Cai Q, Zhou P, Zhang G. Safety and efficacy of submucosal tunneling endoscopic septum division for epiphrenic diverticula. Endoscopy. 2019;51:1141-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 82. | Nabi Z, Ramchandani M, Darisetty S, Kotla R, Reddy DN. Per-oral endoscopic myotomy with endoscopic septum division in a case of achalasia with large epiphrenic diverticulum. VideoGIE. 2019;4:14-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 83. | Basile P, Gonzalez JM, Le Mouel JP, Irarrazaval R, Caillo L, Barthet M. Per-oral endoscopic myotomy with septotomy for the treatment of distal esophageal diverticula (D-POEM). Surg Endosc. 2020;34:2321-2325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 84. | Shrigiriwar A, Mony S, Fayyaz F, Onimaru M, Monachese M, Zhang L, Corre F, Azmeera P, Wu H, Wu CCH, Choi K, Gandhi A, Chalikonda D, Keane MG, Ghandour B, Villamarin-Corrales J, Schlachterman A, Tinto RR, Arévalo FE, Arbizu EA, Bapaye A, Velanovich V, Nieto J, Pawa R, Pawa S, Samanta J, Sedarat A, Eleftheriadis N, Saxena P, Bechara R, Al-Haddad MA, Familiari P, Ujiki M, Ramchandani M, Barret M, Chang K, Moll F, Pioche M, Inoue H, Khashab M. Clinical outcomes of peroral endoscopic myotomy with and without septotomy for management of epiphrenic diverticula: an international multicenter experience (with video). Gastrointest Endosc. 2024;100:840-848.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 85. | Nabi Z, Chavan R, Asif S, Ramchandani M, Basha J, Darisetty S, Goud R, Kotla R, Reddy DN. Per-oral Endoscopic Myotomy with Division of Septum (D-POEM) in Epiphrenic Esophageal Diverticula: Outcomes at a Median Follow-Up of Two Years. Dysphagia. 2022;37:839-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 86. | Noh JH, Kim DH, Jung KW, Na HK, Ahn JY, Lee JH, Choi KD, Song HJ, Lee GH, Jung HY. Usefulness of EndoFLIP in Diverticular Peroral Endoscopic Myotomy for Symptomatic Epiphrenic Diverticulum. J Neurogastroenterol Motil. 2023;29:183-191. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 87. | Nabi Z, Ramchandani M, Reddy DN. Per-oral endoscopic myotomy and gastroesophageal reflux: Where do we stand after a decade of "POETRY"? Indian J Gastroenterol. 2019;38:287-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 88. | Zeng X, Bai S, Zhang Y, Ye L, Yuan X, Hu B. Peroral endoscopic myotomy for the treatment of esophageal diverticulum: an experience in China. Surg Endosc. 2021;35:1990-1996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 89. | Samanta J, Mandavdhare HS, Kumar N, Kumar-M P, Jafra A, Chauhan R, Gupta P, Kumar KH, Singh H, Dutta U, Kochhar R. Per Oral Endoscopic Myotomy for the Management of Large Esophageal Diverticula (D-POEM): Safe and Effective Modality for Complete Septotomy. Dysphagia. 2022;37:84-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 90. | Ren L, Ye H, Zhu Y, Xie W, Liang Y, Liu Y, Dong J, Chen W, Chen X, Wang B, Pan L, Shi R. Diverticular peroral endoscopic myotomy (D-POEM) for symptomatic oesophageal diverticulum: a multicentre cohort study with a minimum follow-up of 3 years. Surg Endosc. 2024;38:253-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/