Published online Jun 16, 2025. doi: 10.4253/wjge.v17.i6.106347
Revised: April 9, 2025
Accepted: May 8, 2025
Published online: June 16, 2025
Processing time: 108 Days and 3.6 Hours
Situs inversus viscerum (SIV) is a rare autosomal recessive genetic disorder characterized a complete mirror-image organ reversal in the thoracic and abdo
Herein, we report a case of an 80-year-old male with choledocholithiasis and acute obstructive empyematous cholangitis. Imaging revealed total visceral inversion in the patient. Endoscopic retrograde cholangiopancreatography (ERCP) was successfully performed to remove the stones, resulting to substantial relief of clinical symptoms and gradual improvement of the patient’s condition, leading to successful recovery and discharge.
Therapeutic ERCP is a safe and effective surgical option for patients with SIV. The main focus for successful ERCP in patients with SIV includes positioning adju
Core Tip: We describe a rare cholangitis case in a patient with complete visceral inversion treated with endoscopic retrograde cholangiopancreatography. Splanchnic inversion (SIV) is a rare congenital disorder characterized by mirror-image inversion of thoracic and abdominal organs, usually with minimal clinical impact. Although a direct link between SIV and specific organ abnormalities has not yet been established, SIV complicates diagnosis and treatment due to changes in its anatomy. Herein, therapeutic endoscopic retrograde cholangiopancreatography was a safe and effective approach in the patient with SIV. Positioning adjustments and specialized techniques, such as the dual-guidewire approach to biliary cannulation, could improve the procedure success rate.
- Citation: Gong KR, Zheng ZL, Li GF, Chen JM. Endoscopic retrograde cholangiopancreatography treatment of cholangitis stone in a patient with total situs inversus: A case report. World J Gastrointest Endosc 2025; 17(6): 106347
- URL: https://www.wjgnet.com/1948-5190/full/v17/i6/106347.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i6.106347
Situs inversus viscerum (SIV) is a rare condition characterized by a complete mirror-image organ reversal within the thoracic and abdominal cavities. This anomaly is typically inherited in an autosomal recessive manner, with an incidence of approximately 1/5000 to 1/10000 in neonates[1]. The incidence is marginally higher in males than in females, and most patients may not exhibit considerable clinical symptoms or discomfort, with minimal impact on daily life[2]. To date, no direct association has been established between visceral organ abnormalities and SIV; however, the unique anatomical structure does pose certain difficulties for clinical diagnosis and treatment.
Cholelithiasis is a common disease of the biliary tract. Although SIV is not considered a high-risk factor for cholelithiasis, its abnormal visceral organ positioning may complicate diagnosis. Abnormalities in the anatomical structure of the gallbladder and bile ducts may lead to misinterpretation of symptoms, prolonging the diagnostic process. Endoscopic retrograde cholangiopancreatography (ERCP) the preferred method for diagnosing and treating choledocholithiasis owing to its short procedure time, minimal trauma, and high diagnostic accuracy (96%-100%). Nevertheless, even experienced endoscopists may face challenges when performing ERCP on patients with situs inversus and choledocholithiasis. Herein, we report a rare case of a patient with total visceral inversion and associated choledocholithiasis, successfully treated with ERCP.
In September 2024, an 80-year-old male presented to our emergency department with a continuous left upper abdominal pain lasting 8 hours.
The patient reported persistent left upper quadrant abdominal pain for 8 hours, along with nausea without vomiting, fever, dizziness, headache, diarrhoea, or jaundice, and no aversion to oil. Upon admission to the emergency department, his blood pressure dropped to 70/40 mmHg, and he was admitted to the intensive care unit for further treatment and diagnosis.
The patient had no history of acute or chronic infectious diseases, cardiovascular disease, hypertension, diabetes, or surgery.
There was no relevant medical history in the patient’s family.
The patient was conscious and bilaterally blind with unexamined pupils. A palpable apex beat felt in the right chest suggested possible dextrocardia. Tenderness in the left upper abdomen, positive Murphy’s sign, and no palpable liver or spleen under the ribs were observed. Negative shifting dullness and weak bowel sounds were noted. A urinary catheter was in place, and the urine was cloudy and purulent.
Complete blood count: White blood cell count 12.31 × 109/L. Biochemistry: Total bilirubin 48.1 μmol/L, direct bilirubin 46.14 μmol/L, γ-glutamyl transferase 905.1 U/L, alanine aminotransferase 84.1 U/L, aspartate aminotransferase 238.1 U/L.
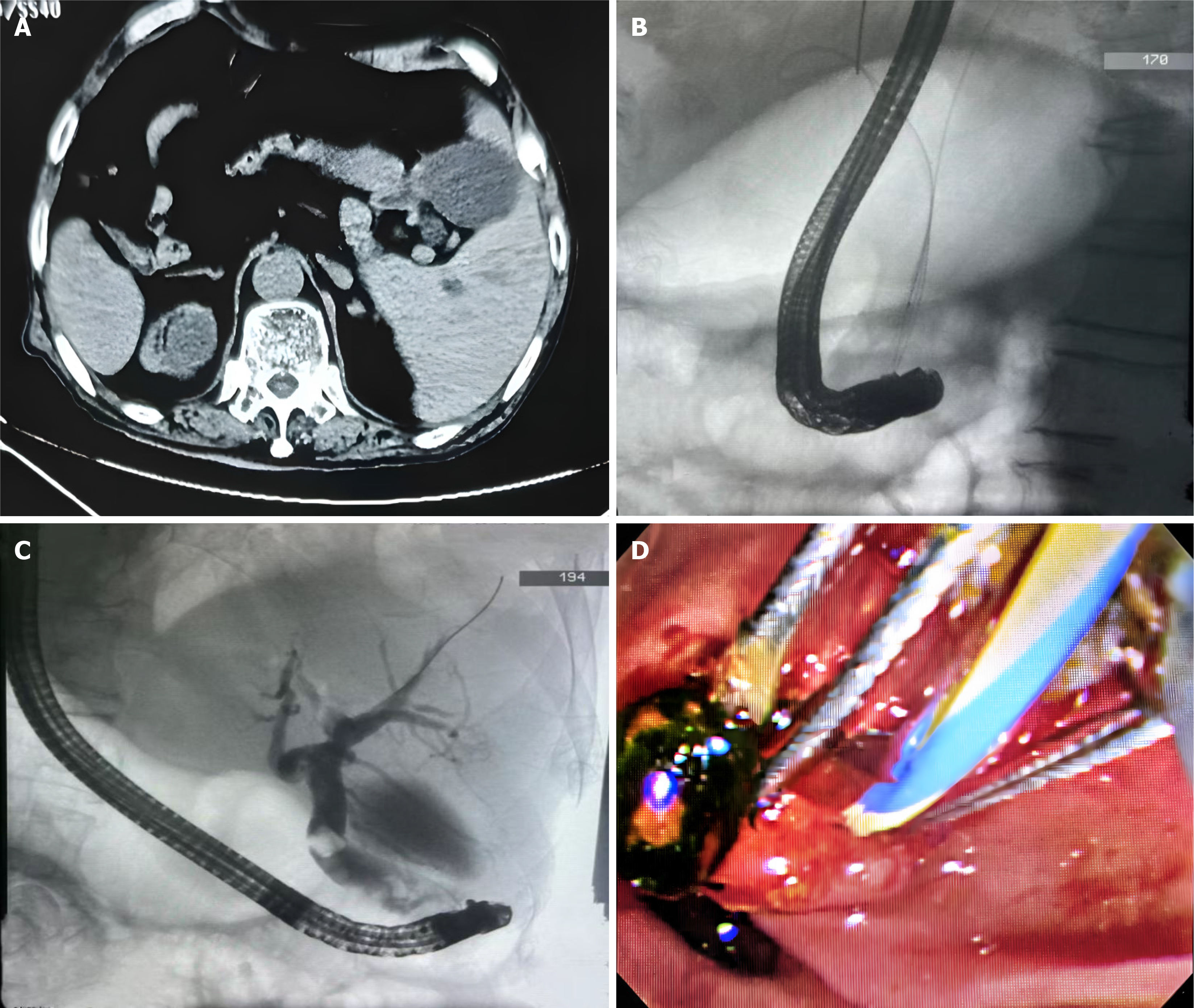
A chest X-ray, electrocardiogram, and echocardiogram confirmed the previous diagnosis of dextrocardia. Computed tomography scans revealed that the liver was primarily located on the left side of the abdomen, while the spleen was on the right. The gallbladder was found on the left side, marginally enlarged, with visibly dilated bile ducts. Mild dilation of the intrahepatic bile ducts and a dense shadow at the terminal end of the common bile duct was observed (Figure 1A).
Based on laboratory tests and imaging studies, the patient was diagnosed with total visceral inversion, choledocholithiasis, and acute suppurative cholangitis.
Given the patient’s severe infection and unstable hemodynamic status, treatment included piperacillin/tazobactam for antimicrobial therapy. Owing to severe inflammation, 10 mg aprepitant was administered once daily to suppress gastric acid secretion, 100 mg hepatoprotective factor once daily to protect the liver, 0.252 mg vitamin B1 once daily to prevent Wernicke’s encephalopathy, and bifid triple bacteria to regulate gastrointestinal flora. After stabilizing the patient’s condition, an emergency ERCP was performed. Prior to ERCP, the patient was successfully anesthetized and placed in a left lateral position and ERCP was performed on the right side by an endoscopist.
During the ERCP, the duodenoscope encountered a rotated gastrointestinal tract, reaching the ampulla of Vater. The ampulla was soft and large with a single-pore opening. Multiple attempts to adjust catheter direction for bile duct cannulation were unsuccessful. The patient was repositioned to a supine position wherein re-endoscopy was performed. The initial attempt at bile duct cannulation resulted in insertion into the pancreatic duct, with a guidewire left in place.
Thereafter, endoscopist used sphincterotomes to carry the guidewire and re-attempt bile duct cannulation. While inserting the catheter with sphincterotomes, which provided axial traction on the pancreatic duct wire. This facilitated separation of the bile and pancreatic ducts, allowing successful bile duct cannulation (Figure 1B). Iohexol contrast revealed an expanded common bile duct with a stone shadow (Figure 1C). A small incision was made in Oddi’s sphincter, and a ball and single-use balloon dilatation catheters were used to dilate the papilla and the lower bile duct segment. Purulent bile flowed out, and a stone basket and single-use stone retrieval balloon were used to remove a yellow-green hard stone into the intestinal lumen (Figure 1D). The bile duct was cleared with a single-use stone retrieval balloon. A subsequent contrast confirmed that the common bile duct was patent.
A nasobiliary drainage catheter was placed into the bile duct without considerable bleeding. The duodenoscope was removed and the nasobiliary drainage catheter was secured at the nasal skin and connected to a closed drainage bag, from which, yellow cloudy bile was drained. The procedure was 45 minutes, and the patient had no significant adverse reactions during the operation. Postoperatively, the patient’s vital signs remained stable.
Postoperative hepatoprotective treatment was performed. After treatment, the patient experienced improvement in liver and kidney functions, after which he was discharged successfully.
SIV is a rare congenital anomaly involving mirror-image organ reversal in the chest and abdomen, leading to anatomical deviations[3]. This organ malposition complicates both treatment and diagnostic procedures. In ERCP, the inversion of internal organs alters conventional anatomical orientation, which can significantly impact the execution of ERCP procedures. During ERCP, affecting endoscope insertion into the papilla and subsequent catheterization. Accurate catheterization is particularly difficult in patients with SIV[4]. Reasons for initial the failure to insert the catheter while the patient was in the left lateral position are as follows: (1) The altered anatomy and side-viewing scope design prevent the operator from using standard strategies in patients without SIV during surgery; (2) ERCP in patients with SIV requires rotating the duodenoscope counterclockwise by 90° in the stomach and again in the second part of the duodenum, complicating the procedure and preventing endoscope shortening. Once a ring-shaped structure is formed, the procedure cannot continue; and (3) Failure to shorten the endoscope results in an unstable field of view, making it difficult to adjust and stabilize the position of the ampulla of Vater, hindering catheterization and cholangiography. In summary, SIV’s unique anatomical challenges require specialized techniques and adaptations during ERCP to ensure successful catheterization and imaging.
In patients with SIV with biliary stones, catheterization is the most critical issue during ERCP. Accurate catheterization can be achieved by continuously changing the patient’s position. ERCP techniques and positioning choices for patients and endoscopists vary significantly SIV cases (Table 1 summarizes these reports of ERCP surgery in patients with biliary stone with SIV)[5-10]. Although reports on supine positioning are fewer, they all indicate that this position is safe and effective, with a high success rate for single procedures. In our case, the patient’s position to was changed to supine, with the operator located on the patient’s left side. Unlike traditional prone positioning for patients with normal anatomical structures, the supine position aligns more closely with organ distribution for patients with SIV. This positioning minimizes changes in the operator’s posture and holding mirror posture and enhances bile duct catheterization stability, significantly improving the success rate.
| Ref. | Patient’s position | Endoscopist’s position | Strategy | Successful within a single operation |
| Venu et al[12], 1985 | Right lateral → prone | Right side of the table | Cannulation by repositioning the patient | Yes |
| Fiocca et al[13], 2008 | Prone | Right side of the table | Rotate the endoscope 180° in the stomach and enter the duodenum | Yes |
| de la Serna-Higuera et al[4], 2010 | Prone | Right side of the table | Rotate the endoscope 180° in the stomach and use a rotating sphincterotomy | Yes |
| García-Fernández et al[5], 2010 | Right lateral | Right side of the table | All operations are performed in reverse to normal procedures | Yes |
| Patel et al[6], 2014 | Prone | Right side of the table | The endoscope is rotated 180° within the duodenum | Yes |
| Hu et al[7], 2015 | Supine → prone | Left side of the table | After the endoscope enters the duodenum, change the patient’s position to prone position | Yes |
| Lee et al[8], 2010 | Prone | Right side of the table | First time: The endoscope is rotated 180° counter clock-wise in the stomach. After entering the duodenum, the endoscope is rotated counterclockwise 180° again to shorten | No |
| The second time: The endoscope reaches the second part of the duodenum along the lesser curvature of the stomach, while slowly rotating the endoscope clockwise close to the ampulla and cannulation | ||||
| Rocha et al[9], 2020 | Supine | Left side of the table | The duodenal papilla is located in the 1 o’clock direction, and cannulation is performed in the one o’clock direction | Yes |
| Current study, 2024 | Left lateral position → supine | Left side of the table | Bile duct cannulation using a dual guidewire strategy | Yes |
However, some issues with using the supine position exist: (1) Gravity makes it difficult to firmly secure the position of the stomach, affecting endoscope stability. Intravenous anaesthesia in our reduced gastrointestinal motility and prevented nausea or vomiting reactions, improving endoscopic manipulation and view stability; and (2) Altered anatomical structures and catheterization angles increase the risk of accidental pancreatic duct insertion. Repeated pancreatic duct insertion can cause injury. Dumonceau et al[11] suggests placing a pancreatic guidewire for selective bile duct catheterization in patients with altered anatomy. If bile duct catheterization fails or the guidewire repeatedly enters the pancreatic duct without resolving the issue, the dual guidewire technique can be used by reserving a pancreatic duct guidewire. If catheterization remains challenging, percutaneous transhepatic ERCP can attempted to establish a biliary passage and guidewire insertion via ERCP guided. In summary, supine positioning is beneficial for patients with SIV undergoing ERCP, requiring meticulous technique and patient assessment to minimize potential complications and maximize the chances of successful catheterization.
Based on this case report, the following recommendations are proposed: (1) With informed consent of the patient, use deep venous anaesthesia should to minimize discomfort and reduce the need for frequent position changes in position, enhancing endoscopic stability; (2) If routing positioning causes catheterization difficulties, promptly adjust the patient’s position to try different catheterization methods; supine position catheterization is a viable and effective option; (3) In cases of difficult or repeated misinsertions into the pancreatic duct during catheterization, consider using the dual-guidewire strategy to improve the success rates; and (4) Complex cases required an experienced endoscopist. If the operator lacks ERCP proficiency or experience and the patient’s condition permits, laparoscopic cholecystectomy for stone removal can also be a feasible alternative. These recommendations aim to improve the safety and efficacy of ERCP in patients with SIV or other complex anatomical conditions. They highlight the importance of patient comfort, operator expertise, and the use of alternative techniques when standard approaches are challenging.
In summary, therapeutic ERCP is a safe and effective surgical option for patients with SIV. The main focus in ERCP for patients with SIV is position adjustment during surgery, and the dual-guidewire technique for biliary cannulation can increase the success rate of biliary cannulation.
| 1. | Feng Q, Liu J, Yao J. Retracted: Common bile duct stones with situs inversus totalis. ANZ J Surg. 2019;89:1527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Qiao T, Yang C. Endoscopic Retrograde Cholangiopancretography for bile duct stones with residual cystic duct stones in patients with situs inversus totalis. Asian J Surg. 2020;43:709-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Ding B, Wang J, Wei X, Du Y, Xia L, Sun C, Han K, Yang X, Guo X, Pan Y, Wang X. Efficacy and safety of ERCP in patients with situs inversus totalis: multicenter case series and literature review. BMC Gastroenterol. 2022;22:497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 4. | de la Serna-Higuera C, Perez-Miranda M, Flores-Cruz G, Gil-Simón P, Caro-Patón A. Endoscopic retrograde cholangiopancreatography in situs inversus partialis. Endoscopy. 2010;42 Suppl 2:E98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | García-Fernández FJ, Infantes JM, Torres Y, Mendoza FJ, Alcazar FJ. ERCP in complete situs inversus viscerum using a "mirror image" technique. Endoscopy. 2010;42 Suppl 2:E316-E317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Patel KS, Patel JN, Mathur S, Moshenyat Y. To twist or not to twist: a case of ERCP in situs inversus totalis. Endoscopy. 2014;46 Suppl 1 UCTN:E304-E305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Hu Y, Zeng H, Pan XL, Lv NH, Liu ZJ, Hu Y. Therapeutic endoscopic retrograde cholangiopancreatography in a patient with situs inversus viscerum. World J Gastroenterol. 2015;21:5744-5748. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Lee JH, Kang DH, Park JH, Kim MD, Yoon KT, Choi CW, Kim HW, Cho M. Endoscopic removal of a bile-duct stone using sphincterotomy and a large-balloon dilator in a patient with situs inversus totalis. Gut Liver. 2010;4:110-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Rocha M, Dias AM, Coimbra J. A Challenging Abdominal Pain. Gastroenterology. 2020;158:e11-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Aabakken L, Karlsen TH, Albert J, Arvanitakis M, Chazouilleres O, Dumonceau JM, Färkkilä M, Fickert P, Hirschfield GM, Laghi A, Marzioni M, Fernandez M, Pereira SP, Pohl J, Poley JW, Ponsioen CY, Schramm C, Swahn F, Tringali A, Hassan C. Role of endoscopy in primary sclerosing cholangitis: European Society of Gastrointestinal Endoscopy (ESGE) and European Association for the Study of the Liver (EASL) Clinical Guideline. Endoscopy. 2017;49:588-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 147] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 11. | Dumonceau JM, Devière J, Cremer M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy. 1998;30:S80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Venu RP, Geenen JE, Hogan WJ, Johnson GK, Taylor AJ, Stewart ET, Jackson A. ERCP and endoscopic sphincterotomy in patients with situs inversus. Gastrointest Endosc. 1985;31:338-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Fiocca F, Donatelli G, Ceci V, Cereatti F, Romagnoli F, Simonelli L, Modini C. ERCP in total situs viscerum inversus. Case Rep Gastroenterol. 2008;2:116-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/