Published online Nov 16, 2025. doi: 10.4253/wjge.v17.i11.109909
Revised: July 4, 2025
Accepted: October 10, 2025
Published online: November 16, 2025
Processing time: 160 Days and 3.8 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) is an essential diag
To evaluate ERCP indications, success rates, complications, and quality perfor
This retrospective study analyzed 13215 ERCP procedures performed between 2006 and 2023. Data included demographics, indications, cannulation rates, complications, and pediatric cases. Findings were assessed against American Society of Gastroenterology/European Society of Gastrointestinal Endoscopy quality indicators.
Biliary ERCP accounted for 93.1% of procedures; choledocholithiasis was the most common indication (40%). Cannulation success was 93.9% for biliary and 94.2% for pancreatic ERCP. Pediatric ERCP comprised 4% of cases, mostly for stones and chronic pancreatitis. Bleeding (1.7%) and post-ERCP pancreatitis (2.3%) were the most frequent complications. Performance met or exceeded most American Society of Benchmarks.
This study offers insight into nearly two decades of ERCP practice within a public sector hospital. Our experience echoes the quality and efficiency of ERCP not previously available in Pakistan. As healthcare systems in resource-limited sectors expand, our findings serve as a reference point. Continued training and quality improvement studies can further enhance ERCP effectiveness in the region and beyond.
Core Tip: We performed a retrospective analysis of 13215 endoscopic retrograde cholangiopancreatography (ERCP) procedures at a single tertiary care hospital in Karachi, Pakistan. We aimed to identify the quality, safety, and efficacy of ERCP in South Asia. The findings demonstrated the dependability of ERCP in a resource-constrained environment with excellent cannulation success rates (over 93%) and a low incidence of significant problems. The findings highlighted the critical need to increase ERCP access and specialized training throughout the region to improve outcomes for individuals with pancreatobiliary illnesses.
- Citation: Zakaria N, Tahseen MU, Niaz TS, Asim M, Yaseen A, Kadir S, Qureshi S, Ghazanfar S, Leghari A, Taj MA, Siddiqui AR, Altaf A, Ahmed N, Raza A, Salman J, Shoaib UB, Siyal M, Durvesh AK, Niaz SK. Endoscopic retrograde cholangiopancreatography in pediatric and adult populations: 17-year experience from Pakistan with trends, complications, and global comparison. World J Gastrointest Endosc 2025; 17(11): 109909
- URL: https://www.wjgnet.com/1948-5190/full/v17/i11/109909.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i11.109909
Endoscopic retrograde cholangiopancreatography (ERCP) is a minimally invasive therapeutic endoscopic procedure for the management of pancreatobiliary disorders. It is the first-line therapeutic modality for choledocholithiasis, periampullary tumors causing obstructive jaundice, management of periprocedural biliary adverse effects, and a spectrum of pancreatic disorders such as chronic pancreatitis[1]. A skilled endoscopist with the capacity to guide case selection based on high-quality evidence is essential to the success of ERCP. Therefore, a thorough benefit-risk assessment of ERCP must be undertaken for each patient. The most common risks of ERCP include pancreatitis (1.6%-15.7%), hemorrhage (1.3%), perforation (0.1%-0.6%), and cholangitis (1.0%)[2].
ERCP is an advanced procedure under intense scrutiny in training hospitals and credentialing bodies[3]. In Pakistan, although a large proportion of patients come from low socioeconomic backgrounds[4], the ERCP procedure is conducted free-of-charge in only a few facilities. Currently, there are limited nationwide, population-based ERCP audits that have been published. In the published studies the cohorts have been relatively small (3544 patients). Healthcare authorities remain focused on improving and standardizing the quality of endoscopy procedures. The American Society of Gastroenterology (ASGE) has provided specific training criteria for ERCP, and these guidelines detail the high-quality skills required to perform the procedure[5]. Herein we describe our retrospective analysis of ERCP procedures performed in the previous 17 years to evaluate the indications, procedure success, and safety of ERCP.
The registry defines successful ductal cannulation as the injection of contrast material into the duct, whereas failure occurs when the endoscopist fails to cannulate the papilla following visualization. We classified cases as unspecified jaundice if imaging revealed a dilated common bile duct (CBD) and laboratory results indicated elevated bilirubin levels.
Our endoscopy unit recently transitioned into an institute by the name of the Sindh Institute of Advanced Endoscopy and Gastroenterology. It is in the Dr Ruth K.M. Pfau Civil Hospital, which is one of the largest tertiary care public hospitals in Pakistan. Over 13000 ERCP procedures have been conducted free of cost from January 2006 to December 2023 at our hospital. The current unit is a 40-bed endoscopy facility staffed by a team of expert gastroenterologists and surgeons. The endoscopists were fully trained, having conducted more than 500 procedures annually. We are financially supported by the government and philanthropic endeavors. Our unit receives referrals from all over the country because our hospital is one of the busiest tertiary care facilities in Pakistan.
Inpatient and outpatient ERCP procedures are performed when the endoscopist deems the procedure necessary. A registry of all procedures is recorded on an in-house database. The database includes a record of patient identification, relevant lab investigations, and recent imaging findings along with procedure findings and outcomes. All records, including follow-up procedures, can be retrieved on demand, allowing easy analysis of procedure outcomes, including adverse effects. Key quality indicators set by the ASGE were mostly met by our unit, reflecting the good practice of ERCP (Table 1)[6]. Data was collected and analyzed retrospectively. To the best of our understanding, this was the largest retrospective ERCP registry to date in South Asia.
| Quality indicators | Grade of recommendation | Measure type | Performance target, % | Target achieved |
| Pre-procedure | ||||
| Frequency with which ERCP is performed for an indication that is included in a published standard list of appropriate indications, and the indication is documented (priority indicator) | 1C+ | Process | > 90.0 | Yes |
| Frequency with which informed consent is obtained, including specific discussions of risks associated with ERCP, and fully documented medical consent is obtained and fully documented | 1C | Process | > 98.0 | Yes |
| Frequency with which appropriate antibiotics for ERCP are administered for settings in which they are indicated | 2B | Process | > 98.0 | Yes |
| Frequency with which ERCP is performed by an endoscopist who is fully trained and credentialed to perform ERCP | 3 | Process | > 98.0 | Yes |
| Frequency with which the volume of ERCP procedures performed per year is recorded per endoscopist | 1C | Process | > 98.0 | Yes |
| Procedure | ||||
| Frequency with which deep cannulation of the ducts of interest is documented | 1C | Process | > 98.0 | Yes |
| Frequency with which deep cannulation of the ducts of interest in patients with native papillae without surgically altered anatomy is achieved and documented (priority indicator) | 1C | Process | > 90.0 | Yes |
| Frequency with which fluoroscopy time and radiation dose are measured and documented | 2C | Process | > 98.0 | No |
| Frequency with which CBD stones (1 cm) in patients with normal bile duct anatomy are extracted successfully and documented (priority indicator) | 1C | Outcome | > 90.0 | Yes |
| Frequency with which stent placement for biliary obstruction in patients with normal anatomy, whose obstruction is below the bifurcation, is successfully achieved and documented (priority indicator) | 1C | Outcome | > 90.0 | Yes |
| Post-procedure | ||||
| Frequency with which a complete ERCP report that details the specific techniques performed, particular accessories used, and all intended outcomes is prepared | 3 | Process | > 98.0 | Yes |
| Frequency with which acute adverse events and hospital transfers are documented | 3 | Process | > 98.0 | Yes |
| Rate of post-ERCP pancreatitis (priority indicator) | 1C | Outcome | N/A | Yes |
| Rate and type of perforation | 2C | Outcome | < 0.2 | Yes |
| Rate of clinically significant hemorrhage after sphincterotomy or sphincteroplasty in patients undergoing ERCP | 1C | Outcome | < 1.0 | Yes |
| Frequency with which patients are contacted at 14 days or greater to detect and record the occurrence of delayed adverse events after ERCP | 3 | Process | > 90.0 | Yes |
All patients who underwent ERCP in the stated timeline were included. Incomplete or records with missing data were excluded.
The primary outcome was to evaluate the success of biliary or pancreatic cannulation in a large retrospective cohort. Secondary outcomes included intra-procedural and immediate adverse events, clinically significant bleeding, perforation, and death.
The collected data were uploaded to Microsoft Excel and then imported to IBM SPSS statistics software, version 25 (IBM Corp., Armonk, NY, United States). In addition to descriptive statistical techniques such as means, percentages, and standard deviations, the study data were analyzed using the Student’s t-test for independent univariate analysis of measurement data and the χ2 test for independent univariate analysis of qualitative data. To identify independent predictors of successful cannulation, a multivariate regression analysis was also performed. This allowed us to adjust for potential confounding variables and gain a better understanding of the factors influencing procedural outcomes. The significance level was set at P < 0.05, and the results were assessed within the 95% confidence interval.
This study reviewed 17 years of retrospective data from 13215 ERCP records. The average age of the patients was 46.5 years with 4% aged under 18 years. Females comprised of 59.2% cases. For expert anesthesiologists, midazolam was the sedation of choice in 95.1% of cases followed by injection of propofol (6.3%) in both pediatric and adult patients. Demographics of patients along with pre-procedure investigations are presented in Table 2.
| Characteristics | n (%)/mean ± SD |
| Sex | |
| Male | 5392 (40.8) |
| Female | 7823 (59.2) |
| Age in years | |
| < 18 (pediatric) | 533 (4.0) |
| 0-3 (toddlers) | 6 |
| 4-11 (childhood) | 126 |
| 12-18 (adolescence) | 401 |
| > 18 (adult) | 12682 (96.0) |
| Mean age, years | 46.50 ± 16.03 |
| Clinical symptoms | |
| Jaundice | 6308 (47.7) |
| Abdominal pain | 5911 (44.7) |
| Other | 996 (7.6) |
| Laboratory parameters | |
| Increased total bilirubin | 8515 (64.4) |
| Mean total bilirubin in mg/dL | 9.50 ± 48.86 |
| Increased ALP | 10256 (77.6) |
| Mean ALP in IU/L | 605.6 ± 1218.4 |
| Post-ERCP pancreatitis | 356 (2.7) |
| Mild pancreatitis | 164 (1.2) |
| Moderate pancreatitis | 136 (1.0) |
| Severe pancreatitis | 56 (0.4) |
| Clinically significant bleeding after EST/EPLBD | 230 (1.7) |
| Hemostasis with balloon tamponade | 35 (0.2) |
| Hemostasis with adrenaline spray | 195 (1.5) |
| Cardio pulmonary adverse effects | 31 (0.2) |
| Perforation | 26 (0.2) |
| Death | 5 (0.0) |
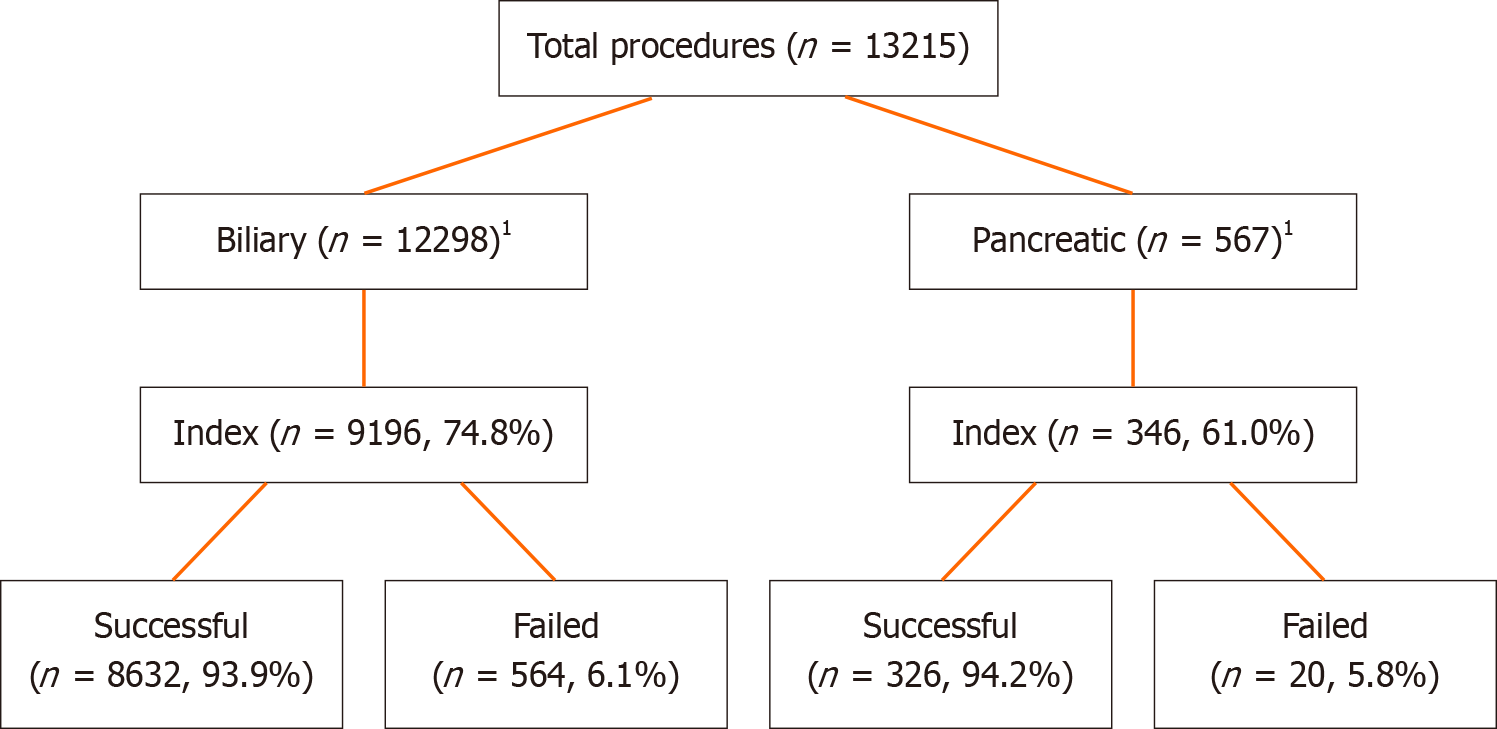
A total of 12298 procedures were biliary ERCP, and 567 procedures were pancreatic ERCP. The ampulla was inaccessible due to gastric or duodenal outlet obstruction in 350 patients. Successful cannulation during index ERCP for biliary cases was 93.9% and 94.2% for index ERCP for pancreatic cases (Figure 1 and Table 3).
Indications for ERCP referral are presented in Table 4.
| Types | n | % |
| Benign biliary cases | ||
| Choledocholithiasis | 3682 | 40.0 |
| Bile leak | 466 | 5.1 |
| Choledochal cyst | 22 | 0.2 |
| CBD worms | 21 | 0.2 |
| Unspecified jaundice1 | 3046 | 33.1 |
| Malignant cases | ||
| Pancreatic mass | 389 | 4.2 |
| Perihilar | 145 | 1.6 |
| Periampullary mass | 1307 | 14.2 |
| Gallbladder mass | 118 | 1.3 |
| Pancreatic cases | ||
| Chronic pancreatitis | 201 | 58.1 |
| Other | 145 | 41.9 |
Of the 3046 unspecified obstructive jaundice cases, 54.1% had CBD stones, 38.4% had biliary strictures, 7.3% had normal examination findings.
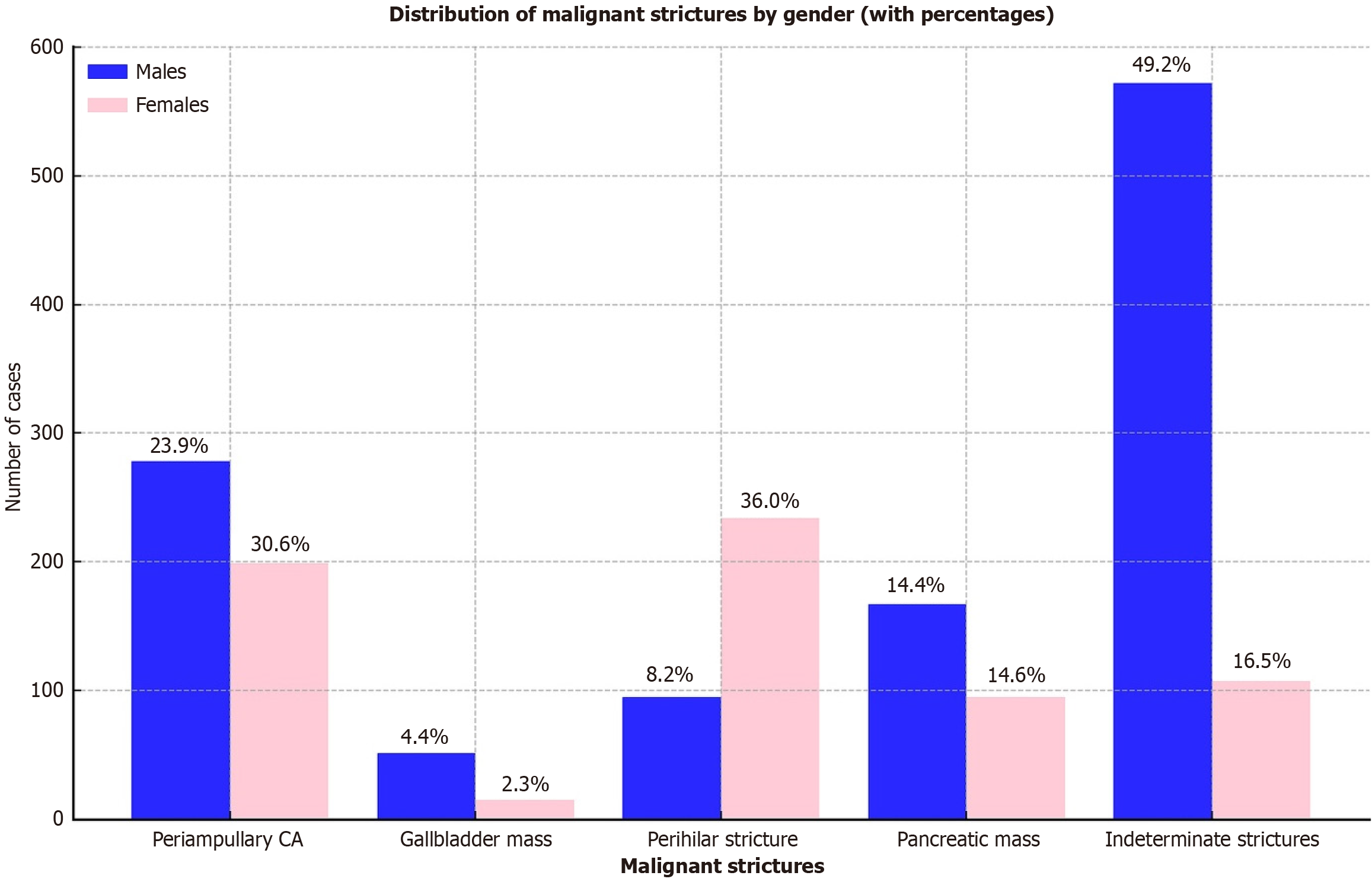
Index biliary ERCP was performed in 1959 cases for malignant indications with a cannulation success rate of 92.7% (Table 5)[7]. Males were most frequently found to have peri-ampullary mass (23.9%) followed by pancreatic malignancy (14.3%). In females’ perihilar cholangiocarcinoma (36.0%) was the most common malignant etiology for biliary obstruction followed by peri-ampullary mass (30.6%; Figure 2).
| ERCP findings | n | % |
| Benign cases | ||
| CBD stones | 4901 | 53.2 |
| Mirizzi syndrome | 53 | 0.6 |
| Normal CBD | 1545 | 16.8 |
| Bile leak | 740 | 8.0 |
| Post-laparoscopic cholecystectomy stricture | 55 | 0.6 |
| CBD worms | 28 | 0.3 |
| Choledochal cyst | 61 | 0.7 |
| Cannulation successful in benign biliary cases | 6955 | 94.2 |
| Cannulation unsuccessful in benign biliary cases | 428 | 5.8 |
| Malignant strictures | ||
| Periampullary cancer | 477 | 5.2 |
| Gallbladder mass | 66 | 0.7 |
| Perihilar stricture | 329 | 3.6 |
| Pancreatic mass | 262 | 2.9 |
| Indeterminate stricture | 679 | 7.4 |
| Total malignant strictures | 1813 | 19.7 |
| Gastric outlet obstruction, ampulla not accessed | 350 | |
| Cannulation successful in malignant strictures | 1681 | 92.7 |
| Cannulation unsuccessful in malignant stricture cases | 132 | 7.3 |
| Pancreatic cases | ||
| Normal PD | 27 | 7.8 |
| Dilated PD | 160 | 46.2 |
| DPDS | 22 | 6.4 |
| PD stones | 83 | 24.0 |
| PD stricture | 80 | 23.1 |
| Pancreatic divisum | 75 | 21.7 |
Table 6 highlights the characteristics of cases that underwent ERCP for CBD stones. Of the 6323 cases of biliary stones, majority were females. Ductal clearance was achieved in 77.5%. However, 1422 (22.5%) patients needed repeat procedure. Majority of stones were retrieved after sphincterotomy (67.8%) and sphincteroplasty (8.3%). Multivariate logistic regression analysis was performed to assess factors associated with successful CBD and pancreatic duct (PD) cannulation. For CBD cannulation, the variables included presence of Mirizzi’s syndrome (P = 0.998), biliary stricture (P = 0.993), CBD stone (P = 0.989), gender (P = 0.721), and age group (P = 1.000). None of these demonstrated a statistically significant association with CBD cannulation success. Similarly, for PD cannulation, the factors analyzed were age group (P = 0.518), gender (P = 0.523), PD stones (P = 0.987), PD strictures (P = 0.985), and disconnected PD syndrome (P = 0.994). None of these variables were significantly associated with PD cannulation either. These findings indicate that the assessed clinical and demographic factors did not independently influence the outcomes of either CBD or PD cannulation in this study.
| CBD stones | n (%) |
| Biliary stones | 6323 (52.3) |
| Duct clearance | |
| Index duct cleared | 4901 (77.5) |
| Follow-up duct clearance | 1422 (22.5) |
| Interventions | |
| Sphincterotomy | 4883 (39.7) |
| Sphincteroplasty | 965 (7.8) |
| Basket | 418 (3.4) |
| Spyglass EHL | 201 (1.6) |
| Maneuvers | |
| Biliary sphincterotomy | 8347 (67.8) |
| Balloon sphincteroplasty | 1024 (8.3) |
| Needle-knife papillotomy | 714 (5.8) |
| Cholangioscopy and EHL | 214 (1.7) |
| Trapezoid basket | 432 (3.5) |
| Soehendra dilator | 94 (0.8) |
| Biliary stenting | 5381 (43.8) |
| CBD cleared in one session | 1683 (13.7) |
Pancreatic ERCP procedures were performed in 567 cases, of which 61.0% were with native papilla. Chronic pancreatitis accounted for 58.1% cases. With ductal stones and strictures being predominant findings. In 75 cases, pancreatic divisum was diagnosed via pancreatogram performed during pancreatic ERCP.
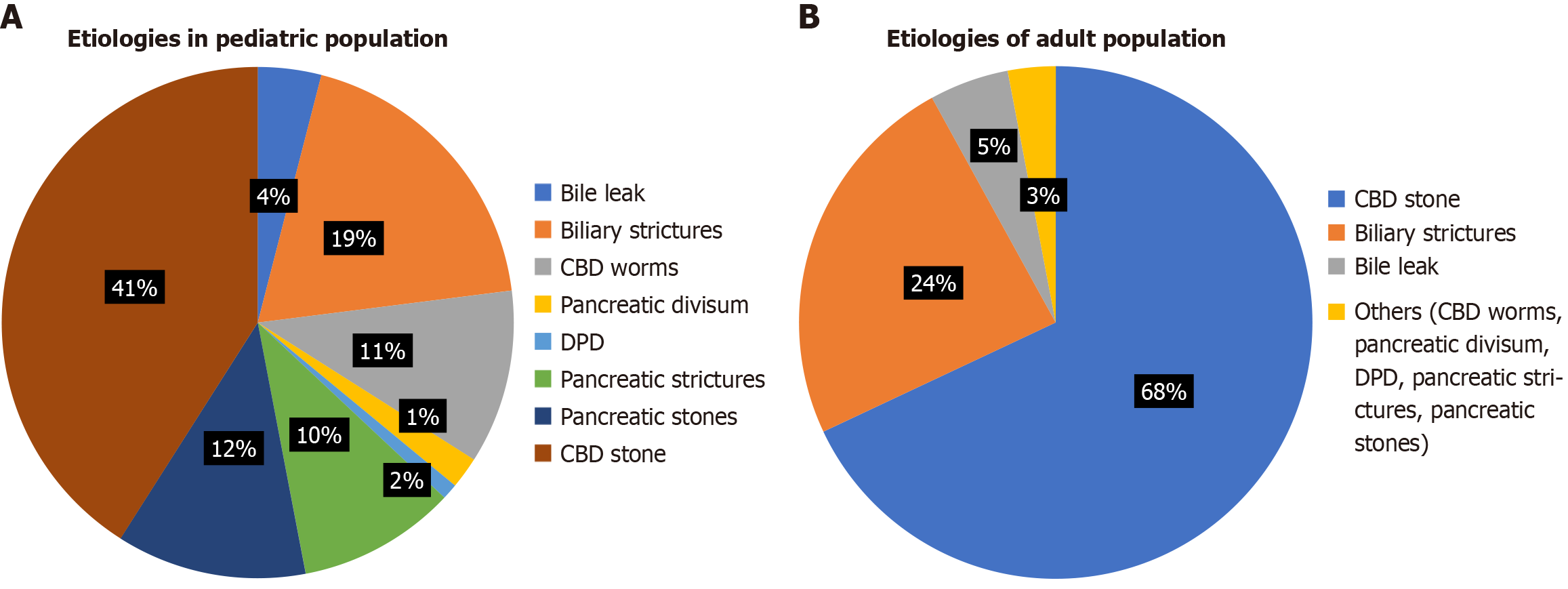
Pediatric ERCP procedures were performed in 533 patients with an average age of patients being 14 years. This included 401 adolescence, 126 patients between 4-11 years, and 6 patients under 4 years. Choledocholithiasis was the indication for 41% of the pediatric cases, followed by chronic pancreatitis in 35%. The imaging findings of native cases are presented in Table 4. No major complications were reported in pediatric patients. Sedation was tailored according to age and weight.
Peri-procedure bleeding was observed in 1.7% of all performed procedures. However, significant bleeding occurred in
ERCP is an ever-evolving advanced procedure that demands standard quality and safety. Meticulous training and adherence to protocol are of the utmost importance to achieve the best outcomes. The ASGE guidelines have guided ERCP practice in our unit, which is located in one of the busiest tertiary care centers in the 12th largest city in the world. Our unit comprises a team of expert endoscopists, surgeons, and anesthesiologists. The objective for this study was to assess the quality of ERCP procedures and report the success rate, complications, and findings for ERCP. This seventeen-year-old retrospective study is the largest recorded dataset for ERCP from South Asia to date. High cannulation success was observed (biliary ERCP 93.9%) and (pancreatic ERCP 94.2%) which aligned with ASGE benchmarks[9].
Park et al[10] conducted a nationwide survey in Korea about ERCP trends. They reported that ERCP was performed more frequently with increasing age of patients, likely linked to gallstones and pancreatobiliary malignancy. This is a stark contrast from our study findings where the average age of patients was mid-forties. Another study conducted by Moffatt et al[11] stated that ERCPs were more commonly done in women than in men (62%). The results tally with our study, where women more commonly had ERCP. A study by Parveen et al[12] reported a much higher incidence of perihilar carcinoma in both male and female populations. In our cohort, female predominance of perihilar cholangiocarcinoma. This suggests a possible biological difference that warrants for further investigation.
Our descriptive data revealed that 22% of patients achieved ductal clearance in the index ERCP. 59.64% of patients required only a single ERCP procedure (Table 7). Since 2013, Spyglass cholangioscopy has been occasionally used for selective cases (1.6%). Due to cost of equipment, the impact of new technology is yet to be further explored. Keil et al[13] retrospective study corroborated our findings with a cannulation success rate of 96% in peadiatric ERCP with choledochal cyst, choledocholithiasis, and pancreatic pathology as the most common findings. In contrast, the primary diagnosis in our unit was biliary stones, followed by pancreatic pathologies. A study conducted in India quoted similar findings to our unit[14]. Post-ERCP pancreatitis was the most frequent adverse effect. Significant gastrointestinal bleeding was infrequent. The rate of bleeding was below 1% and aligns with the standard quality indicators of ERCP recommended by both European and American societies of gastroenterology.
| Number of procedures | n | % |
| 18 | 1 | 0.007 |
| 17 | 1 | 0.007 |
| 16 | 1 | 0.007 |
| 15 | 1 | 0.007 |
| 14 | 1 | 0.007 |
| 13 | 1 | 0.007 |
| 12 | 2 | 0.015 |
| 11 | 3 | 0.022 |
| 10 | 5 | 0.037 |
| 9 | 9 | 0.068 |
| 8 | 20 | 0.151 |
| 7 | 61 | 0.461 |
| 6 | 109 | 0.824 |
| 5 | 255 | 1.929 |
| 4 | 631 | 4.774 |
| 3 | 2116 | 16.01 |
| 2 | 2116 | 16.01 |
| 1 | 7882 | 59.64 |
| Total | 13215 | 100 |
This study has several notable strengths. It was the largest single-center investigation conducted within a tertiary care facility that was offered entirely at no cost to participants. Importantly, it marked the first endeavor of this scale in South Asia and delivered meaningful data regarding the etiologies of both biliary and pancreatic ERCP procedures. Moreover, it comprises the most extensive dataset of pediatric pancreatic ERCP procedures (Figure 3) reported in Asia to date. Nevertheless, several limitations should be acknowledged. The retrospective design may introduce certain biases that are difficult to eliminate. Definitive histopathological confirmation was unavailable for several malignant strictures, and endoscopic ultrasound data were not incorporated as it was beyond the objective of this article. Additionally, post-procedural follow-up for delayed complications was suboptimal including cholangitis, potentially impacting the reliability of the study outcomes.
This study offers insight of nearly 2 decades of ERCP practice within a public sector hospital. Beyond the numbers, our experience echoes the quality and efficiency of ERCP that was otherwise not available for Pakistan. As healthcare systems in resource limited sectors move to expand, our findings can serve as a reference point. Moving forward, continued training measures, and further studies with quality improvements can help to further the effectiveness of ERCP within our region and beyond.
| 1. | Forbes N, Koury HF, Bass S, Cole M, Mohamed R, Turbide C, Gonzalez-Moreno E, Kayal A, Chau M, Lethebe BC, Hilsden RJ, Heitman SJ. Characteristics and Outcomes of ERCP at a Canadian Tertiary Centre: Initial Results from a Prospective High-Fidelity Biliary Endoscopy Registry. J Can Assoc Gastroenterol. 2021;4:78-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | ASGE Standards of Practice Committee; Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben-Menachem T, Cash BD, Decker GA, Early DS, Fanelli RD, Fisher DA, Fukami N, Hwang JH, Ikenberry SO, Jue TL, Khan KM, Krinsky ML, Malpas PM, Maple JT, Sharaf RN, Shergill AK, Dominitz JA. Complications of ERCP. Gastrointest Endosc. 2012;75:467-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 311] [Article Influence: 22.2] [Reference Citation Analysis (1)] |
| 3. | Rodrigues-Pinto E, Baron TH, Liberal R, Macedo G. Quality and competence in endoscopic retrograde cholangiopancreatography - Where are we 50 years later? Dig Liver Dis. 2018;50:750-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Khan SU, Hussain I. Inequalities in health and health-related indicators: a spatial geographic analysis of Pakistan. BMC Public Health. 2020;20:1800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Adler DG, Lieb JG 2nd, Cohen J, Pike IM, Park WG, Rizk MK, Sawhney MS, Scheiman JM, Shaheen NJ, Sherman S, Wani S. Quality indicators for ERCP. Am J Gastroenterol. 2015;110:91-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Domagk D, Oppong KW, Aabakken L, Czakó L, Gyökeres T, Manes G, Meier P, Poley JW, Ponchon T, Tringali A, Bellisario C, Minozzi S, Senore C, Bennett C, Bretthauer M, Hassan C, Kaminski MF, Dinis-Ribeiro M, Rees CJ, Spada C, Valori R, Bisschops R, Rutter MD. Performance measures for ERCP and endoscopic ultrasound: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2018;50:1116-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Enochsson L, Swahn F, Arnelo U, Nilsson M, Löhr M, Persson G. Nationwide, population-based data from 11,074 ERCP procedures from the Swedish Registry for Gallstone Surgery and ERCP. Gastrointest Endosc. 2010;72:1175-1184, 1184.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 151] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 486] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 9. | Baron TH. Experience is "what separates the good and the great": implications of ERCP volume on patient outcomes. Gastrointest Endosc. 2024;99:960-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Park JM, Kang CD, Lee JC, Hwang JH, Kim J. Recent 5-Year Trend of Endoscopic Retrograde Cholangiography in Korea Using National Health Insurance Review and Assessment Service Open Data. Gut Liver. 2020;14:833-841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Moffatt DC, Yu BN, Yie W, Bernstein CN. Trends in utilization of diagnostic and therapeutic ERCP and cholecystectomy over the past 25 years: a population-based study. Gastrointest Endosc. 2014;79:615-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Parveen S, Shah AH, Gulzar GM, Sodhi JS, Khan MA, Tiwari A, Mir TA, Sharma A, Ahmad SN, Dar NA. ERCP practice at a tertiary care hospital in Kashmir, North India: a large single-center cross-sectional study with focus on quality indicators, success rate, and indications. Ann Med Surg (Lond). 2023;85:1705-1711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Keil R, Drábek J, Lochmannová J, Šťovíček J, Koptová P, Wasserbauer M, Frýbová B, Šnajdauf J, Matouš J, Kotalová R, Rygl M, Hlava Š. ERCP in infants, children, and adolescents-Different roles of the methods in different age groups. PLoS One. 2019;14:e0210805. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Poddar U, Thapa BR, Bhasin DK, Prasad A, Nagi B, Singh K. Endoscopic retrograde cholangiopancreatography in the management of pancreaticobiliary disorders in children. J Gastroenterol Hepatol. 2001;16:927-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/