Published online Oct 16, 2025. doi: 10.4253/wjge.v17.i10.110172
Revised: June 22, 2025
Accepted: September 19, 2025
Published online: October 16, 2025
Processing time: 139 Days and 2.9 Hours
Bile duct leak (BDL) is a common complication of hepatobiliary surgery, including cholecystectomy, hepatic resection, and liver transplantation. Timely recognition and effective management are essential to prevent serious complications such as peritonitis, intra-abdominal abscesses, and sepsis. Endoscopic retrograde cholangiopancreatography (ERCP) has become the first-line diagnostic and therapeutic approach. Despite the high overall success rate, the optimal treatment strategies remain a subject of ongoing debate. This review summarizes the existing classification systems and current endoscopic management of BDLs, including drainage strategies, optimal timing of ERCP and stent removal, and approaches for com
Core Tip: Bile duct leak is a common but challenging complication after hepatobiliary surgery. This review summarizes current classification systems and endoscopic trea
- Citation: Chen DX, Chen SX, Zhang GJ, Liang YW, Han YM, Zhai YQ, Li MY. Endoscopic management of bile duct leaks: Current strategies and controversies. World J Gastrointest Endosc 2025; 17(10): 110172
- URL: https://www.wjgnet.com/1948-5190/full/v17/i10/110172.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i10.110172
Bile duct leaks (BDLs) most commonly occur as complications following hepatobiliary surgeries such as cholecystectomy, hepatic resection, or liver transplantation[1,2]. Early recognition and prompt management are critical, as delayed management may lead to life-threatening complications such as electrolyte disturbances, peritonitis, intra-abdominal abscesses, and, in severe cases, mortality rates approaching 40%-50%[3]. ERCP is the first-line diagnostic and therapeutic approach for BDLs, with diagnostic sensitivity exceeding 98% and therapeutic success rates ranging from 71.4% to 100%[4-7]. Treatment typically involves endoscopic sphincterotomy (EST), biliary drainage [plastic stents or nasobiliary drainage (NBD)], or a combination of both, aiming to reduce the bile duct-duodenum pressure gradient to promote bile flow and facilitate leak closure[8-10]. However, endoscopic management of BDLs remains challenging due to the lack of consensus on classification, drainage strategies, optimal timing of stents placement and removal, and strategies for complex cases[11,12].
This review aims to provide a comprehensive overview of current classification systems and endoscopic treatment strategies, including drainage strategies, optimal timing of ERCP and stent removal, and management of complex cases.
Classification of BDLs is critical for assessing injury severity, guiding individualized treatment, and improving clinical outcomes. The Bismuth classification, first proposed in 1982, was originally designed for surgical planning by describing strictures relative to the hepatic duct confluence, but is limited to bile duct injuries with strictures and has limited value for endoscopic management[13,14].
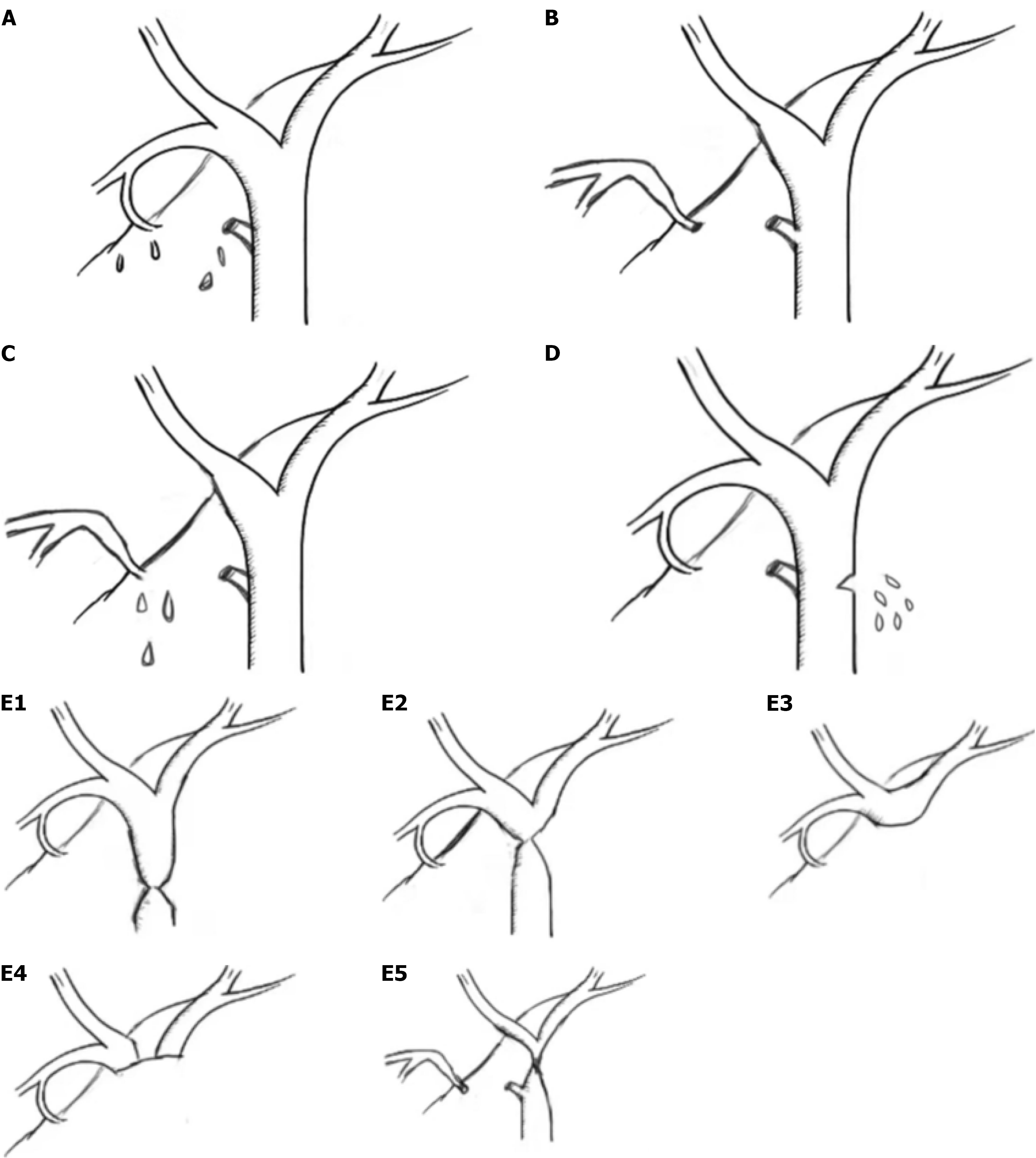
To address these limitations, the Strasberg classification was introduced in 1995, offering a more comprehensive classification that includes a wider range of injuries and is now widely used in clinical practice[15]. Types E1-E5 align with Bismuth types I-V, while type A injuries (cystic or Luschka duct) are the most common (up to 85%) and generally re
In 2004, Sandha et al[16] proposed an ERCP-based classification that stratifies BDLs into low-grade (leak visible only after complete intrahepatic opacification) and high-grade (extravasation evident before full opacification). High-grade leaks are associated with poorer outcomes and may require additional drainage or surgery. This system has been validated in several studies and aids in predicting the success of endoscopic treatment[7,17].
The International Study Group of Liver Surgery (ISGLS) classifies BDLs into grades A-C based on clinical severity: Grade A requires no intervention, Grade B necessitates endoscopic treatment, and Grade C requires surgical repair[18]. While the system standardizes the definition of each grade, its clinical utility remains limited, as it has been criticized for being overly simplistic[19,20].
Several other classifications, including the Amsterdam[21], Stewart-Way[22], Hannover[23], McMahon[24], Neuhaus[25], Siewert[26], Csencdes[27] classifications, have been proposed, but none have achieved widespread clinical use. The Strasberg, ISGLS and Sandha classifications remain the most practical for guiding endoscopic management. Table 1 summarizes these classifications and their clinical implications.
| Classification, year | Study objective | Type/grade | Practical implication |
| Bismuth[13], 1982 | To classify post-cholecystectomy biliary strictures for surgical planning and prognosis | Type I: Injury > 2 cm below confluence; Type II: < 2 cm; Type III: Hilar with no confluence; Type IV: Complete separation of right and left ducts; Type V: Aberrant right sectoral duct ± CHD injury | Designed for strictures, not leaks. Offers limited guidance for endoscopic management of BDLs such as cystic duct or Luschka leaks |
| Strasberg[15], 1995 | To classify bile duct injuries after cholecystectomy for treatment planning | Type A: Cystic duct/Luschka leak; B: Occluded right posterior duct; C: Leaking posterior duct; D: Lateral injury (< 50%); E1-E5: Strictures (Bismuth I-V). | Most widely adopted. Types A, C, D may be endoscopically managed; B and E often require surgery. Useful for guiding endoscopic decisions |
| Amsterdam[61], 1996 | To guide endoscopic management of bile duct injuries | Type A: Cystic duct/peripheral leak; B: Major duct leak; C: Stricture; D: Complete transection | Types A and B can be managed endoscopically; C and D generally need surgical repair. Aids decision-making for endoscopic vs surgical management |
| Stewart-Way[22], 2004 | To evaluate the mechanism and impact of RHAI in laparoscopic bile duct injury | Class I: CBD mistaken for cystic duct, recognized pre-transection; Class II: CHD injured by clip/cautery; Class III: CBD transected due to misidentification (most common); Class IV: RHD injured during dissection | Highlights the high RHAI incidence in severe injuries, especially Class III (35%) and IV (64%). Important for surgical planning; limited relevance for endoscopic strategies |
| Hannover[23], 2007 | To guide surgical strategies for bile duct and vascular injuries | Type A: Peripheral leaks (A1: Cystic duct; A2: Gallbladder bed); Type B: Strictures without injury (B1-B2); Type C: Tangential injuries (C1-C4); Type D: Complete transections (D1-D4); Type E: Strictures (E1-E4); Vascular injury suffixes: D, s, p, com, c, pv | Provides comprehensive anatomical and vascular classification, aiding surgical decision-making. Limited utility for endoscopic management |
| McMahon[24], 1995 | To classify bile duct injury severity and guide surgical repair | Minor: Laceration < 25% or cystic-CBD tear; Major: Laceration > 25%, CBD/CHD transection, postoperative stricture | Minor injuries often amenable to T-tube or suture repair; major injuries typically require hepaticojejunostomy. Endoscopy plays a limited role |
| Neuhaus[25], 2000 | To guide surgical/endoscopic management of post-cholecystectomy injuries | Type A (Peripheral leaks): A1, cystic duct leak; A2, gallbladder bed leak. Type B (Occlusion): B1, incomplete (e.g., clip); B2, complete. Type C (Lateral CBD injury): C1, lesion < 5 mm; C2, > 5 mm. Type D (Transection): D1, without tissue defect; D2, with tissue defect. Type E (Stricture): E1, < 5 mm; E2, > 5 mm; E3, confluence; E4, right hepatic/segmental duct | Type A: Sphincterotomy ± stent; percutaneous drainage if needed. Type B1: Endoscopic dilation + stent; B2: Surgery (clip removal) + long-term stenting. Type C1: Sphincterotomy or stent; C2: Surgery + stent ≥ 12 months. Type D: Surgical reconstruction (e.g., hepaticojejunostomy). Type E1: Stenting ≥ 12 months; E2-E4: Surgical resection + hepaticojejunostomy; extended hepatectomy if ischemic cholangiopathy |
| Siewert[26], 1994 | To stratify bile duct injuries for surgical planning | Type I: Immediate biliary fistula; Type II: Late stricture; Type IIIa/IIIb: Tangential lesion ± vascular injury; Type IVa/IVb: Duct disruption ± vascular injury | Type I may be endoscopically treated; Types II-IV typically require surgical reconstruction, especially with vascular involvement |
| Csencdes[27], 2001 | To guide surgical/endoscopic treatment of bile duct injuries | Type I: Small tear of hepatic duct or right hepatic branch. Type II: Injury at cysticocholedochal junction (e.g., from traction, catheter, electrocautery, or close transection). Type III: Partial or complete CBD section. Type IV: Resection of > 10 mm of CBD | Type I/II: May be managed with endoscopic stenting; Type III/IV: Typically require surgical repair (e.g., hepaticojejunostomy) |
ERCP is the first-line treatment for most BDLs. However, several aspects of endoscopic management remain controversial, including the choice between sphincterotomy, stent placement, or both; the optimal stent diameter and type; whether the stent should bridge the leak; and the predictors of ERCP outcomes. This section reviews current strategies and controversies in endoscopic management (summarized in Tables 2 and 3).
| Ref. | Study design (n) | Key findings | Conclusion | Quality1 |
| EST vs stents | ||||
| Dolay et al[62], 2010 | Single-center, prospective (27) | Stenting led to faster leak resolution than EST (4.5 ± 2.0 days vs 6.5 ± 3.4 days); 2 failures in EST group | Stenting > EST | High |
| Abbas et al[33], 2019 | Multicenter, retrospective (1028) | Stent alone (96%) and stent + EST (97%) had higher success than EST alone (89%) | Stenting ± EST > EST alone | Medium |
| Rainio et al[32], 2018 | Single-center, retrospective (71) | Comparable leak closure time and healing rates between EST and EST + stent | EST and EST + stent offer similar efficacy in type A leaks | Medium |
| Kaffes et al[63], 2005 | Single-center, retrospective (100) | Success: Stent and EST + stent (100%) vs EST alone (78%, P = 0.001) | Stenting ± EST > EST alone | Low |
| Haidar et al[29], 2020 | Single-center, retrospective (100) | Stenting (± EST) had higher success than EST (95.3% vs 72.7%, P < 0.05) | Stenting ± EST > EST alone | Low |
| Sachdev et al[12], 2012 | Single-center, retrospective (65) | EST + stent in 52 (80%), stent alone in 6 (9%), EST alone in 5 (8%), NBD in 2 (3%); all achieved clinical success | EST + stent may be optimal | Low |
| Sendino et al[64], 2018 | Dual-center, retrospective (65) | Stent ± EST (n = 47) led to higher resolution than EST alone (94% vs 58%, P < 0.01). Fewer required percutaneous (4% vs 12%) or surgical intervention (6% vs 42%, P < 0.001) | Stenting ± EST > EST alone | Medium |
| Chandra et al[31], 2019 | Single-center, retrospective (58) | Comparable initial success between EST and EST + stent (92% vs 90%, P = 0.85); stent group had slower resolution (P = 0.02) and more reinterventions (P < 0.01) | EST with or without stent is effective; stenting may delay resolution | Low |
| Flumignan et al[65], 2021 | Single-center, retrospective (31) | EST + stent (n = 22) and EST alone (n = 9) both reduced drainage volume and time to cessation; 2 failures (group unspecified) | No significant difference between EST and EST + stent | Low |
| NBD vs stent | ||||
| Raza et al[38], 2019 | Systematic review | Stent efficacy: 82.4%; NBD efficacy: 87.2% | Comparable efficacy between NBD and stent | - |
| Ref. | Study design (n) | Key findings | Conclusion | Quality1 |
| Leak-Bridging vs short stent | ||||
| Obata et al[37], 2025 | Single-center, retrospective (122) | Bridging stents (P < 0.001), percutaneous drainage (P = 0.0025), and leak severity (P = 0.015) were independent predictors of endoscopic success | Bridging stents across the leak are key to clinical success | Medium |
| Schaible et al[36], 2017 | Single-center, retrospective (35) | Bridging stents achieved 100% success (13/13) vs only 52.6% (10/19) for non-bridging stents | Bridging stents > non-bridging stents | Low |
| Quintini et al[42], 2024 | Dual-center, retrospective (65) | Success rate higher with bridging vs. non-bridging stents (91% vs 53%, P = 0.005) | Bridging stents more effective | Low |
| Stent diameter | ||||
| Katsinelos et al[40], 2008 | RCT (63) | Success: 93.5% (7 Fr) vs 96.9% (10 Fr) | Stent diameter did not impact outcome | High |
| Vlaemynck et al[28], 2019 | Meta (331) | Success: 95.4% (<10 Fr) vs 97.8% (≥10 Fr). | Stent size did not affect efficacy | High |
| Predictors | ||||
| Yabe et al[17], 2017 | Single-center, retrospective (58) | Success: 88% (low-grade) vs 59% (high-grade) | High-grade leak predicts failure | Medium |
| Quintini et al[42], 2024 | Dual-center, retrospective (65) | Success: 67% (main duct) vs 90%-100% (others); bridging stents superior (91% vs 53%) | Leak location and bridging predict success | Low |
| Schaible et al[36], 2017 | Single-center, retrospective (35) | Success: 64% (peripheral) vs 92% (central); not significant (P = 0.059); best with bridging at hepatic ducts | Peripheral leaks respond poorly | Low |
| Tewani et al[1], 2013 | Single-center, retrospective (223) | ERCP is more effective for cystic/Luschka leaks (P = 0.028) | Leak site and stenting predict success | Medium |
| Chen et al[7], 2024 | Multicenter, retrospective (106) | Positive: Bridging and cystic duct; Negative: SIRS, high-grade leaks | Location, severity, bridging stent, and systemic status are key predictors | Medium |
Endoscopic management of BDLs typically involves EST, stent placement, or a combination of both[28]. The principle is to reduce the pressure gradient between the bile duct and the duodenum, thereby promoting bile flow into the duodenum and facilitating closure of the leak site[29,30]. However, the optimal strategy remains controversial, particularly regarding whether EST alone is sufficient.
Chandra et al[31] reviewed 58 cases and reported slower resolution (P = 0.02) and higher reintervention rates (P < 0.01) in the stent group. The authors suggested that stents may impair epithelial healing by promoting bacterial colonization and reducing ductal contractility. Rainio et al[32] retrospectively analyzed 71 cases of Amsterdam type A leaks and found no significant difference in clinical success between EST alone and EST plus stent placement (90% vs 90.4%, P > 0.05).
In contrast, a large nationwide study by Abbas et al[33] involving 1028 patients showed better outcomes with stent placement—either alone or combined with EST—compared to EST alone. Similarly, a meta-analysis by Vlaemynck et al[28] demonstrated that combined EST with transpapillary stent placement achieved the highest success rate (98.3%)[34]. Therefore, EST alone may be sufficient for low-grade leaks, but is inadequate in more severe cases.
The necessity of bridging the leak during endoscopic biliary drainage remains a subject of debate. Haidar et al[29] emphasized that the primary goal is to reduce the pressure gradient between the bile duct and the duodenum. As the proximal bile duct typically exceeds the stent diameter, bridging the leak may not confer additional benefit. Furthermore, bile is thought to predominantly flow along the stent's outer surface rather than through its lumen[35]. However, a meta-analysis including 11 studies demonstrated that leak-bridging stent was associated with higher clinical success rates[28]. Technically, bridging the leak can be challenging, particularly in cases involving intrahepatic leaks or concurrent biliary strictures. The reported technical success rate of leak-bridging drainage in intrahepatic leaks is only 64%[36].
Therefore, leak-bridging drainage should be prioritized when technically feasible. If bridging is not achievable, non-bridging drainage remains a valid and effective alternative[37].
Both plastic stent drainage and NBD are commonly used during ERCP for the management of BDLs. A systematic review of 34 studies demonstrated comparable success rates in post-liver transplantation BDLs (plastic stents: 82.4% vs NBD: 87.2%)[38]. NBD provides real-time monitoring of bile output and enables cholangiography to confirm BDL healing without the need for repeat ERCP. However, its use is limited by poor patient tolerance, risk of dislodgement, electrolyte loss, and increased nursing demands. Additionally, the average duration of NBD is relatively short (2-11 days; mean 4.7 ± 0.9), compared to biliary stents (14-53 days; mean 29.1 ± 4.4)[39]. Therefore, NBD may be less appropriate for high-output leaks. Plastic stents are preferred for their longer drainage time and better patient tolerance.
In a randomized trial of 63 post-cholecystectomy patients, Katsinelos et al[40] found no significant difference in success rates between 7 Fr and 10 Fr stents (93.5% vs 96.9%, P > 0.05). Similarly, a meta-analysis reported comparable outcomes for stents ≥ 10 Fr and < 10 Fr (97.8% vs 95.4%)[28]. Plastic stent diameter may not significantly impact outcomes, unless it exceeds the bile duct lumen and directly seals the leak. However, to minimize the risk of stent occlusion, 10 Fr stents are generally preferred[41].
The location of BDLs is an important factor influencing endoscopic treatment success. Leaks from the cystic duct stump or ducts of Luschka after cholecystectomy are generally associated with high success rates[1,7]. In contrast, a retrospective study reported that leaks from the main bile duct (common hepatic or common bile duct) had a lower success rate compared to those from other sites (67% vs 90%-100%)[42]. This reduced efficacy is likely due to higher bile flow in the main ducts, which may hinder leak closure.
Intrahepatic leaks have also been associated with lower success rates, possibly due to their deeper anatomical location and the technical difficulty of bridging the leak with a stent[36].
Leak severity is another important predictor of endoscopic failure. High-grade leaks, defined as contrast extravasation before complete intrahepatic opacification, are associated with poorer outcomes[16]. In addition, systemic inflammatory response syndrome indicates more severe BDLs and systemic inflammation, and is associated with endoscopic failure[7].
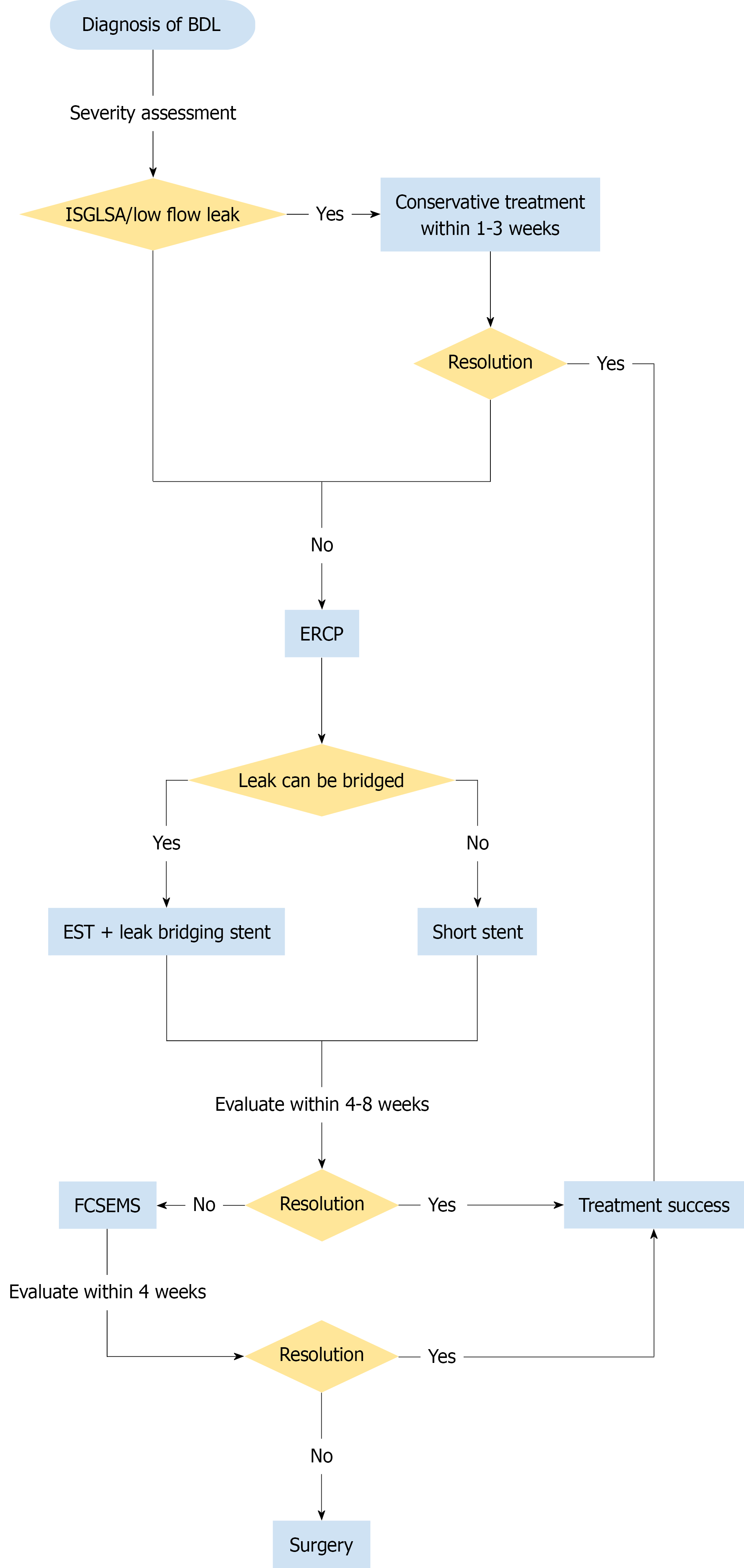
Optimal timing of ERCP and stent removal is essential for effective management of BDLs. Urgent ERCP is not necessary in all cases, and optimal stent retention time varies by stent type and leak severity (Supplementary Table 1).
Several studies have shown that the timing of ERCP, whether performed within 1 day, 2-3 days, or after 3 days, does not significantly affect clinical outcomes[33,43,44]. In a retrospective study of 593 hepatectomies, 34 cases of bile leaks were reported, with a 76.5% success rate for conservative management[45]. These findings suggest that urgent ERCP may not be necessary in all cases and could impose unnecessary procedural burden. When abdominal drainage is in place, ERCP can be performed electively[46,47].
According to the ISGLS definition, most Grade A BDLs resolve within one week with percutaneous drainage. Persistent output beyond one week or signs of infection are classified as Grade B and should be managed with endoscopic intervention[18]. Viganò et al[45] identified a drain output > 100 mL on postoperative day 10 as an inde
Therefore, in patients with abdominal drainage in place, conservative management may be appropriate during the first 1-3 weeks. If the bile output does not decrease or symptoms persist, ERCP should be performed within this period to prevent stricture formation.
The duration of stent retention should be individualized based on stent type and leak severity. For plastic stents, a retention period of 4-8 weeks is generally recommended to prevent stent occlusion[5,34,40]. A comparative study reported a mean healing time of 29.1 ± 4.4 days (range, 14-53 days) with plastic stents vs 4.7 ± 0.9 days (range, 2-11 days) with NBD[39]. For fully covered self-expandable metal stents (FCSEMS), optimal stent retention time remains unclear. In one study of 17 patients with refractory postcholecystectomy leaks after failed sphincterotomy and plastic stenting, the median stent duration was 16 days (range, 7-28 days)[6]. Another study reported a median leak closure time of 3.5 days[5]. Overall, FCSEMS should be retained within 3-4 weeks to minimize risks of strictures, pancreatitis, and stent migration[6,41,50,51].
Management of complex BDLs, including refractory leaks and bilomas, often requires additional endoscopic or surgical interventions. This section summarizes strategies for cases that fail to respond to standard treatment (Supplementary Table 2).
Endoscopic sphincterotomy with placement of a plastic stent is effective in most BDLs, but may be insufficient for high-grade or high-output leaks. Multiple plastic stents (MPS) provide a cost-effective salvage option, while FCSEMS, directly seal the leak, have demonstrated higher efficacy in refractory cases[5,6,41,50,52,53].
In a multicenter study of 178 patients who underwent sphincterotomy plus a single 10 Fr stent, 16 (9%) experienced initial treatment failure and were thus classified as refractory leaks. Among these, 62.5% responded to MPS, while the remainder required FCSEMS[5]. Predictors of MPS failure included the use of fewer than three stents, total diameter < 20 Fr, and high-grade leaks[5]. In a prospective study of 40 patients with refractory postcholecystectomy leaks, FCSEMS achieved superior efficacy compared to MPS (100% vs 65%, P = 0.004)[54].
Despite its effectiveness, FCSEMS is associated with a risk of biliary stricture, particularly in liver transplant cases, and is currently not recommended in this setting[55]. In one case series, 13 patients achieved leak resolution with FCSEMS, with 2 cases developing strictures[51]. In addition, FCSEMS placement across the sphincter of Oddi raises concerns about pancreatitis and stent migration. The use of a dumbbell-shaped FCSEMS may reduce these risks[54]. Persistent leaks unresponsive to endoscopic treatment may ultimately require surgical intervention, such as hepaticojejunostomy[56,57].
Bilomas are typically secondary to BDLs. While small or asymptomatic collections may resolve spontaneously with conservative management, symptomatic or large bilomas (> 5 cm) usually require drainage. Compared with percu
Both EUS-TD and transpapillary/transfistulary (TP/TF) drainage are effective minimally invasive options[58]. In a retrospective cohort of 30 patients with complex bilomas, clinical success rates were 75% for EUS-TD and 67% for TP/TF drainage[59]. Another study comparing ERCP and EUS-TD in 47 patients reported similar clinical success (87% vs 84%) and technical success (94% vs 100%), while EUS-TD demonstrated shorter procedure time (16.9 minutes vs 26.6 minutes, P = 0.009) and hospital stay (22 days vs 46 days, P = 0.038)[60].
ERCP is the first-line approach for the diagnosis and management of BDLs. This review summarizes current classifications, endoscopic strategies, optimal timing of ERCP and stent removal, and the management of complex cases. Figure 2 summarizes the proposed treatment algorithm for BDL based on current evidence. However, most current evidence is based on retrospective studies and case series. Well-designed prospective studies are needed to establish standardized, evidence-based management protocols for BDLs.
We would like to thank Guan-Jun Zhang, Ya-Wen Liang, Yu-Ming Han for their valuable contributions to literature search. Their assistance was essential to the successful completion of this study.
| 1. | Tewani SK, Turner BG, Chuttani R, Pleskow DK, Sawhney MS. Location of bile leak predicts the success of ERCP performed for postoperative bile leaks. Gastrointest Endosc. 2013;77:601-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Tsolakis AV, James PD, Kaplan GG, Myers RP, Hubbard J, Wilson T, Zimmer S, Mohamed R, Cole M, Bass S, Swain MG, Heitman SJ. Clinical prediction rule to determine the need for repeat ERCP after endoscopic treatment of postsurgical bile leaks. Gastrointest Endosc. 2017;85:1047-1056.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Reed DN Jr, Vitale GC, Wrightson WR, Edwards M, McMasters K. Decreasing mortality of bile leaks after elective hepatic surgery. Am J Surg. 2003;185:316-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Dumonceau JM, Tringali A, Papanikolaou IS, Blero D, Mangiavillano B, Schmidt A, Vanbiervliet G, Costamagna G, Devière J, García-Cano J, Gyökeres T, Hassan C, Prat F, Siersema PD, van Hooft JE. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated October 2017. Endoscopy. 2018;50:910-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 534] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 5. | Canena J, Horta D, Coimbra J, Meireles L, Russo P, Marques I, Ricardo L, Rodrigues C, Capela T, Carvalho D, Loureiro R, Dias AM, Ramos G, Coutinho AP, Romão C, Veiga PM. Outcomes of endoscopic management of primary and refractory postcholecystectomy biliary leaks in a multicentre review of 178 patients. BMC Gastroenterol. 2015;15:105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Canena J, Liberato M, Horta D, Romão C, Coutinho A. Short-term stenting using fully covered self-expandable metal stents for treatment of refractory biliary leaks, postsphincterotomy bleeding, and perforations. Surg Endosc. 2013;27:313-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Chen DX, Chen SX, Hou SL, Wen GH, Yang HK, Shi DP, Lu QX, Zhai YQ, Li MY. A nomogram for prediction of ERCP success in patients with bile duct leaks: a multicenter study. Surg Endosc. 2024;38:2465-2474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Fukuda K, Nakai Y, Mizuno S, Sato T, Noguchi K, Kanai S, Suzuki T, Hakuta R, Ishigaki K, Saito K, Saito T, Takahara N, Hamada T, Kogure H, Fujishiro M. Endoscopic Bridge-and-Seal of Bile Leaks Using a Fully Covered Self-Expandable Metallic Stent above the Papilla. J Clin Med. 2022;11:6019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 9. | Çelik M, Yilmaz H, Kılıç MC, Soykan M, Akbudak İH, Ozban M, Yilmaz M. Efficacy and safety of endoscopic retrograde cholangiopancreatography with endoscopic sphincterotomy and biliary stenting in post-operative bile leaks. Ulus Travma Acil Cerrahi Derg. 2023;29:904-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Siiki A, Ahola R, Vaalavuo Y, Antila A, Laukkarinen J. Initial management of suspected biliary injury after laparoscopic cholecystectomy. World J Gastrointest Surg. 2023;15:592-599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 11. | Coté GA, Ansstas M, Shah S, Keswani RN, Alkade S, Jonnalagadda SS, Edmundowicz SA, Azar RR. Findings at endoscopic retrograde cholangiopancreatography after endoscopic treatment of postcholecystectomy bile leaks. Surg Endosc. 2010;24:1752-1756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Sachdev A, Kashyap JR, D'Cruz S, Kohli DR, Singh R, Singh K. Safety and efficacy of therapeutic endoscopic interventions in the management of biliary leak. Indian J Gastroenterol. 2012;31:253-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Bismuth H, Majno PE. Biliary strictures: classification based on the principles of surgical treatment. World J Surg. 2001;25:1241-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 174] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 14. | Ma D, Liu P, Lan J, Chen B, Gu Y, Li Y, Yue P, Liu Z, Guo D. A Novel End-to-End Biliary-to-Biliary Anastomosis Technique for Iatrogenic Bile Duct Injury of Strasberg-Bismuth E1-4 Treatment: A Retrospective Study and in vivo Assessment. Front Surg. 2021;8:747304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 15. | Halle-Smith JM, Hodson J, Stevens LG, Dasari B, Marudanayagam R, Perera T, Sutcliffe RP, Muiesan P, Isaac J, Mirza DF, Roberts KJ. A comprehensive evaluation of the long-term clinical and economic impact of minor bile duct injury. Surgery. 2020;167:942-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Sandha GS, Bourke MJ, Haber GB, Kortan PP. Endoscopic therapy for bile leak based on a new classification: results in 207 patients. Gastrointest Endosc. 2004;60:567-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 144] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Yabe S, Kato H, Mizukawa S, Akimoto Y, Uchida D, Seki H, Tomoda T, Matsumoto K, Yamamoto N, Horiguchi S, Tsutsumi K, Okada H. Predictive factors for outcomes of patients undergoing endoscopic therapy for bile leak after hepatobiliary surgery. Dig Endosc. 2017;29:353-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 948] [Cited by in RCA: 1531] [Article Influence: 102.1] [Reference Citation Analysis (0)] |
| 19. | Sonbare D. Bile leakage after hepatobiliary and pancreatic surgery: is the ISGLS definition too simple? Surgery. 2012;151:634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Sarr MG, Warshaw AL. Consensus classifications of postoperative complications--are they really useful? Surgery. 2011;149:725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | de Reuver PR, Rauws EA, Vermeulen M, Dijkgraaf MG, Gouma DJ, Bruno MJ. Endoscopic treatment of post-surgical bile duct injuries: long term outcome and predictors of success. Gut. 2007;56:1599-1605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | Stewart L, Robinson TN, Lee CM, Liu K, Whang K, Way LW. Right hepatic artery injury associated with laparoscopic bile duct injury: incidence, mechanism, and consequences. J Gastrointest Surg. 2004;8:523-30; discussion 530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 121] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 23. | Bektas H, Schrem H, Winny M, Klempnauer J. Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Br J Surg. 2007;94:1119-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 93] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | McMahon AJ, Fullarton G, Baxter JN, O'Dwyer PJ. Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br J Surg. 1995;82:307-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 148] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 25. | Neuhaus P, Schmidt SC, Hintze RE, Adler A, Veltzke W, Raakow R, Langrehr JM, Bechstein WO. [Classification and treatment of bile duct injuries after laparoscopic cholecystectomy]. Chirurg. 2000;71:166-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 52] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Karanikas M, Bozali F, Vamvakerou V, Markou M, Memet Chasan ZT, Efraimidou E, Papavramidis TS. Biliary tract injuries after lap cholecystectomy-types, surgical intervention and timing. Ann Transl Med. 2016;4:163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Csendes A, Navarrete C, Burdiles P, Yarmuch J. Treatment of common bile duct injuries during laparoscopic cholecystectomy: endoscopic and surgical management. World J Surg. 2001;25:1346-1351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Vlaemynck K, Lahousse L, Vanlander A, Piessevaux H, Hindryckx P. Endoscopic management of biliary leaks: a systematic review with meta-analysis. Endoscopy. 2019;51:1074-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 29. | Haidar H, Manasa E, Yassin K, Suissa A, Kluger Y, Khamaysi I. Endoscopic treatment of post-cholecystectomy bile leaks: a tertiary center experience. Surg Endosc. 2021;35:1088-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Ishii T, Hatano E, Furuyama H, Manaka D, Terajima H, Uemoto S. Preventive Measures for Postoperative Bile Leakage After Central Hepatectomy: A Multicenter, Prospective, Observational Study of 101 Patients. World J Surg. 2016;40:1720-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Chandra S, Murali AR, Masadeh M, Silverman WB, Johlin FC. Comparison of Biliary Stent versus Biliary Sphincterotomy Alone in the Treatment of Bile Leak. Dig Dis. 2020;38:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Rainio M, Lindström O, Udd M, Haapamäki C, Nordin A, Kylänpää L. Endoscopic Therapy of Biliary Injury After Cholecystectomy. Dig Dis Sci. 2018;63:474-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 33. | Abbas A, Sethi S, Brady P, Taunk P. Endoscopic management of postcholecystectomy biliary leak: When and how? A nationwide study. Gastrointest Endosc. 2019;90:233-241.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | Mavrogiannis C, Liatsos C, Papanikolaou IS, Karagiannis S, Galanis P, Romanos A. Biliary stenting alone versus biliary stenting plus sphincterotomy for the treatment of post-laparoscopic cholecystectomy biliary leaks: a prospective randomized study. Eur J Gastroenterol Hepatol. 2006;18:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 35. | Ayres L, Cheriyan D, Scott R, Kim E, Lee T, Singer J, Donnellan F, Byrne M, Weiss A, Enns R, Amar J, Lam E, Telford J. A randomized trial comparing winged versus conventional plastic stents for malignant bile duct strictures. Endosc Int Open. 2017;5:E635-E641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Schaible A, Schemmer P, Hackert T, Rupp C, Schulze Schleithoff AE, Gotthardt DN, Büchler MW, Sauer P. Location of a biliary leak after liver resection determines success of endoscopic treatment. Surg Endosc. 2017;31:1814-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 37. | Obata T, Matsumoto K, Harada K, Hattori N, Sato R, Matsumi A, Miyamoto K, Terasawa H, Fujii Y, Uchida D, Horiguchi S, Tsutsumi K, Otsuka M. Endoscopic Bridging Stent Placement Improves Bile Leaks After Hepatic Surgery. J Clin Med. 2025;14:3381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 38. | Raza A, Omer A, Iqbal S, Gudsoorkar V, Koduru P, Krishnan K. Efficacy of Nasobiliary Tubes and Biliary Stents in Management of Patients with Bile Leak after Liver Transplantation: A Systematic Review. Clin Endosc. 2019;52:159-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 39. | Hii MW, Gyorki DE, Sakata K, Cade RJ, Banting SW. Endoscopic management of post-cholecystectomy biliary fistula. HPB (Oxford). 2011;13:699-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 40. | Katsinelos P, Kountouras J, Paroutoglou G, Chatzimavroudis G, Germanidis G, Zavos C, Pilpilidis I, Paikos D, Papaziogas B. A comparative study of 10-Fr vs. 7-Fr straight plastic stents in the treatment of postcholecystectomy bile leak. Surg Endosc. 2008;22:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 41. | Rio-Tinto R, Canena J. Endoscopic Treatment of Post-Cholecystectomy Biliary Leaks. GE Port J Gastroenterol. 2021;28:265-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 42. | Quintini D, Rizzo GEM, Tarantino I, Sarzo G, Fantin A, Miraglia R, Maruzzelli L, Ligresti D, Carrozza L, Rancatore G, Gruttadauria S, Cillo U, Ferrara F, Traina M. Endoscopic or combined management of post-surgical biliary leaks: a two-center recent experience. Surg Endosc. 2024;38:7233-7242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Desai A, Twohig P, Trujillo S, Dalal S, Kochhar GS, Sandhu DS. Clinical efficacy, timing, and outcomes of ERCP for management of bile duct leaks: a nationwide cohort study. Endosc Int Open. 2021;9:E247-E252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (4)] |
| 44. | Adler DG, Papachristou GI, Taylor LJ, McVay T, Birch M, Francis G, Zabolotsky A, Laique SN, Hayat U, Zhan T, Das R, Slivka A, Rabinovitz M, Munigala S, Siddiqui AA. Clinical outcomes in patients with bile leaks treated via ERCP with regard to the timing of ERCP: a large multicenter study. Gastrointest Endosc. 2017;85:766-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 45. | Viganò L, Ferrero A, Sgotto E, Tesoriere RL, Calgaro M, Capussotti L. Bile leak after hepatectomy: predictive factors of spontaneous healing. Am J Surg. 2008;196:195-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Schreuder AM, Busch OR, Besselink MG, Ignatavicius P, Gulbinas A, Barauskas G, Gouma DJ, van Gulik TM. Long-Term Impact of Iatrogenic Bile Duct Injury. Dig Surg. 2020;37:10-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 47. | Barbier L, Souche R, Slim K, Ah-Soune P. Long-term consequences of bile duct injury after cholecystectomy. J Visc Surg. 2014;151:269-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 48. | de'Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de'Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021;16:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 135] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 49. | Chen DX, Fang KX, Chen SX, Hou SL, Wen GH, Yang HK, Shi DP, Lu QX, Zhai YQ, Li MY. Optimal timing of endoscopic biliary drainage for bile duct leaks: A multicenter, retrospective, clinical study. World J Gastrointest Surg. 2025;17:99425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 50. | Baron TH, Poterucha JJ. Insertion and removal of covered expandable metal stents for closure of complex biliary leaks. Clin Gastroenterol Hepatol. 2006;4:381-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 51. | Wang AY, Ellen K, Berg CL, Schmitt TM, Kahaleh M. Fully covered self-expandable metallic stents in the management of complex biliary leaks: preliminary data - a case series. Endoscopy. 2009;41:781-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 52. | Wu G, Li WY, Gong YX, Lin F, Sun C. Impact of open hepatectomy on postoperative bile leakage in patients with biliary tract cancer. World J Gastrointest Surg. 2024;16:67-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 53. | Nakagawa K, Matsubara S, Suda K, Otsuka T, Oka M, Nagoshi S. Usefulness of Intraductal Placement of a Dumbbell-Shaped Fully Covered Self-Expandable Metal Stent for Post-Cholecystectomy Bile Leaks. J Clin Med. 2023;12:6530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 54. | Canena J, Liberato M, Meireles L, Marques I, Romão C, Coutinho AP, Neves BC, Veiga PM. A non-randomized study in consecutive patients with postcholecystectomy refractory biliary leaks who were managed endoscopically with the use of multiple plastic stents or fully covered self-expandable metal stents (with videos). Gastrointest Endosc. 2015;82:70-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 55. | Phillips MS, Bonatti H, Sauer BG, Smith L, Javaid M, Kahaleh M, Schmitt T. Elevated stricture rate following the use of fully covered self-expandable metal biliary stents for biliary leaks following liver transplantation. Endoscopy. 2011;43:512-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 56. | Alatise OI, Akinyemi PA, Owojuyigbe AO, Ojumu TA, Omisore AD, Aderounmu A, Ekinadese A, Asombang AW. Endoscopic management of postcholecystectomy complications at a Nigerian tertiary health facility. BMC Gastroenterol. 2024;24:375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 57. | Schertz PJ, Mao CA, Derrick KD, Galar F, Ortiz CB, Walker JA, Lopera JE. Biliary Leaks: Multidisciplinary Approach to Diagnosis and Treatment. Radiographics. 2024;44:e230155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 58. | Tonozuka R, Itoi T, Tsuchiya T, Sofuni A, Ishii K, Ikeuchi N, Umeda J, Tanaka R, Mukai S, Gotoda T, Moriyasu F. EUS-guided drainage of hepatic abscess and infected biloma using short and long metal stents (with videos). Gastrointest Endosc. 2015;81:1463-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 59. | Lorenzo D, Bromberg L, Arvanitakis M, Delhaye M, Fernandez Y Viesca M, Blero D, Pezzullo M, Racapé J, Lucidi V, Le Moine O, Devière J, Lemmers A. Endoscopic internal drainage of complex bilomas and biliary leaks by transmural or transpapillary/transfistulary access. Gastrointest Endosc. 2022;95:131-139.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 60. | Sakamoto J, Ogura T, Ueno S, Okuda A, Nishioka N, Hakoda A, Uba Y, Tomita M, Hattori N, Nakamura J, Bessho K, Nishikawa H. Evaluation of exclusive internal endoscopic drainage for complex biloma with transluminal and transpapillary stenting. Endosc Int Open. 2024;12:E262-E268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 61. | Bergman JJ, van den Brink GR, Rauws EA, de Wit L, Obertop H, Huibregtse K, Tytgat GN, Gouma DJ. Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut. 1996;38:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 186] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 62. | Dolay K, Soylu A, Aygun E. The role of ERCP in the management of bile leakage: endoscopic sphincterotomy versus biliary stenting. J Laparoendosc Adv Surg Tech A. 2010;20:455-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 63. | Kaffes AJ, Hourigan L, De Luca N, Byth K, Williams SJ, Bourke MJ. Impact of endoscopic intervention in 100 patients with suspected postcholecystectomy bile leak. Gastrointest Endosc. 2005;61:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 130] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 64. | Sendino O, Fernández-Simon A, Law R, Abu Dayyeh B, Leise M, Chavez-Rivera K, Cordova H, Colmenero J, Crespo G, Rodriguez de Miguel C, Fondevila C, Llach J, Navasa M, Baron T, Cárdenas A. Endoscopic management of bile leaks after liver transplantation: An analysis of two high-volume transplant centers. United European Gastroenterol J. 2018;6:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 65. | Flumignan VK, Sachdev AH, Nunes JPS, Silva PF, Pires LHB, Andreoti MM. Sphincterotomy alone versus sphincterotomy and biliary stent placement in the treatment of bile leaks: 10 year experience at a quaternary hospital. Arq Gastroenterol. 2021;58:71-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 66. | Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. 2014;14:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 770] [Cited by in RCA: 1838] [Article Influence: 153.2] [Reference Citation Analysis (0)] |
| 67. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 26257] [Article Influence: 1750.5] [Reference Citation Analysis (4)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/