Published online Mar 16, 2024. doi: 10.4253/wjge.v16.i3.148
Peer-review started: December 23, 2023
First decision: January 11, 2024
Revised: January 19, 2024
Accepted: February 23, 2024
Article in press: February 23, 2024
Published online: March 16, 2024
Processing time: 81 Days and 14.9 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) is an essential therapeutic tool for biliary and pancreatic diseases. Frail and elderly patients, especially those aged ≥ 90 years are generally considered a higher-risk population for ERCP-related complications.
To investigate outcomes of ERCP in the Non-agenarian population (≥ 90 years) concerning Frailty.
This is a cohort study using the 2018-2020 National Readmission Database. Patients aged ≥ 90 were identified who underwent ERCP, using the international classification of diseases-10 code with clinical modification. Johns Hopkins’s adjusted clinical groups frailty indicator was used to classify patients as frail and non-frail. The primary outcome was mortality, and the secondary outcomes were morbidity and the 30 d readmission rate related to ERCP. We used univariate and multivariate regression models for analysis.
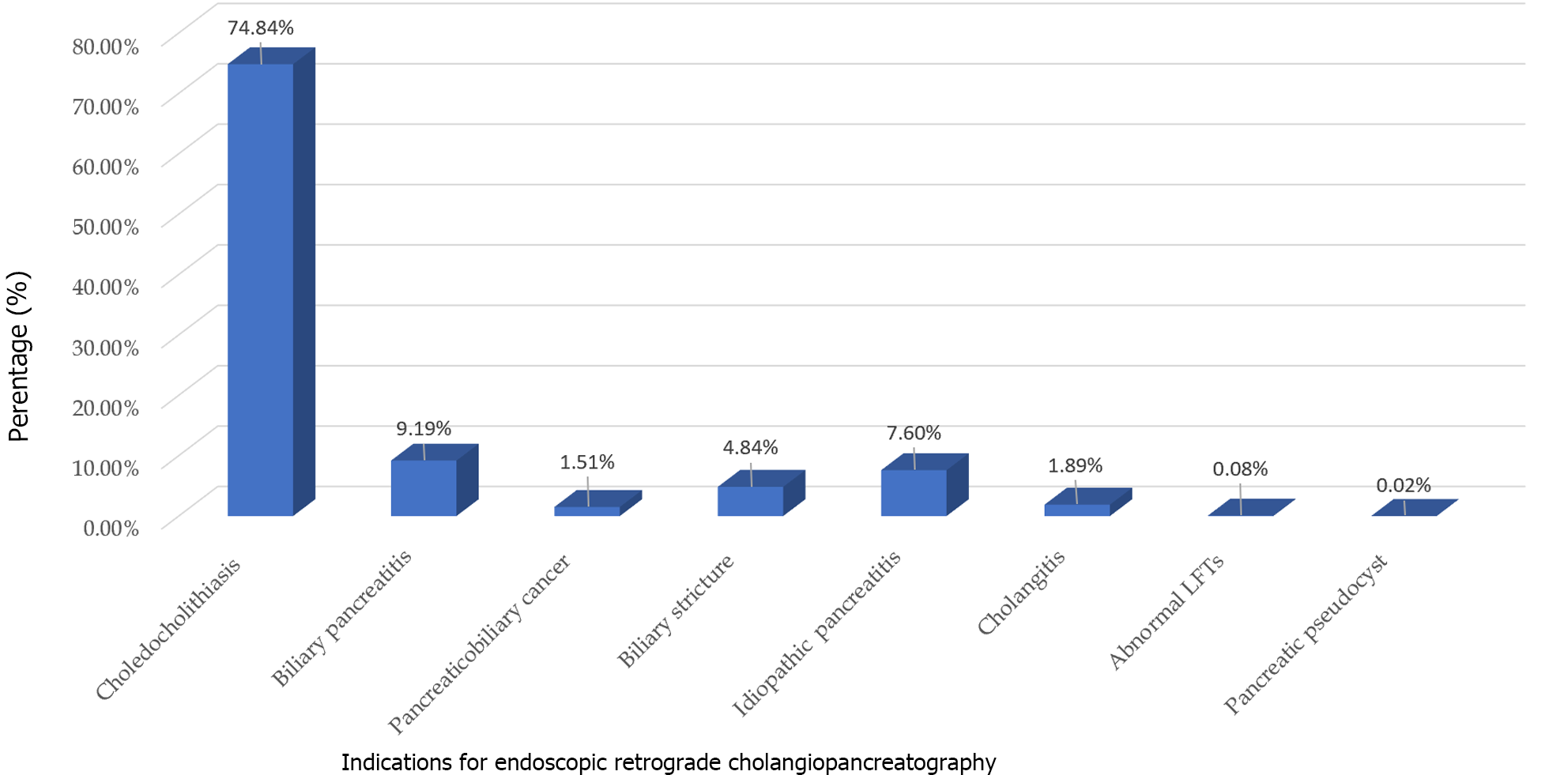
A total of 9448 patients were admitted for any indications of ERCP. Frail and non-frail patients were 3445 (36.46%) and 6003 (63.53%) respectively. Indications for ERCP were Choledocholithiasis (74.84%), Biliary pancreatitis (9.19%), Pancreatico-biliary cancer (7.6%), Biliary stricture (4.84%), and Cholangitis (1.51%). Mortality rates were higher in frail group [adjusted odds ratio (aOR) = 1.68, P = 0.02]. The Intra-procedural complications were insignificant between the two groups which included bleeding (aOR = 0.72, P = 0.67), accidental punctures/lacerations (aOR = 0.77, P = 0.5), and mechanical ventilation rates (aOR = 1.19, P = 0.6). Post-ERCP complication rate was similar for bleeding (aOR = 0.72, P = 0.41) and post-ERCP pancreatitis (aOR = 1.4, P = 0.44). Frail patients had a longer length of stay (6.7 d vs 5.5 d) and higher mean total charges of hospitalization ($78807 vs $71392) compared to controls (P < 0.001). The 30 d all-cause readmission rates between frail and non-frail patients were similar (P = 0.96).
There was a significantly higher mortality risk and healthcare burden amongst nonagenarian frail patients undergoing ERCP compared to non-frail. Larger studies are warranted to investigate and mitigate modifiable risk factors.
Core Tip: In this comprehensive national study, frail nonagenarians undergoing endoscopic retrograde cholangiopancreatography (ERCP) faced heightened mortality, prolonged hospital stays, and increased healthcare costs compared to non-frail counterparts. Surprisingly, intra-procedural and post-procedural complications showed no significant difference between the frail and non-frail groups, including bleeding and accidental punctures. Notably, post-ERCP pancreatitis rates were also comparable. Despite similar 30 d readmission rates, frailty emerged as an independent predictor of post-ERCP mortality in nonagenarians. With limited guidelines for such advanced procedures in this population, careful consideration of benefits vs risks is crucial, urging a personalized approach for those with approved indications for ERCP.
- Citation: Basida SD, Dahiya DS, Yousaf MN, Basida B, Pinnam BSM, Gangwani MK, Ali H, Singh S, Shah YR, Ahluwalia D, Shah MP, Chandan S, Sharma NR, Thakkar S. Impact of frailty on endoscopic retrograde cholangiopancreatography outcomes in nonagenarians: A United States national experience. World J Gastrointest Endosc 2024; 16(3): 148-156
- URL: https://www.wjgnet.com/1948-5190/full/v16/i3/148.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i3.148
Endoscopic retrograde cholangiopancreatography (ERCP) is indeed a high-risk endoscopic procedure to assess and treat conditions involving the pancreaticobiliary ductal system. ERCP was initially developed in the late 1960s as a diagnostic procedure. Over time, it has evolved from being primarily a diagnostic tool to a therapeutic procedure, enabling the treatment of various conditions like choledocholithiasis, acute cholangitis, bile duct strictures, etc.[1,2]. Both ERCP and procedures associated with therapeutic ERCP have the potential for complications, such as bleeding, pancreatitis, duodenum and pancreaticobiliary perforations, and cardiopulmonary distress[3,4]. Mortality rates up to 6%-7% related to ERCP procedures have also been documented[5-7].
While age has traditionally been employed as a predictor of clinical outcomes in ERCP, it alone proves insufficient for a comprehensive assessment of risk-benefit trade-offs. A more holistic approach is essential to gauge physiological resilience and functional capacity, which are crucial in determining overall risk. Several studies have employed the use of Johns Hopkins’s Adjusted Clinical Groups (ACG) frailty indicator to overcome this[8-10]. Frailty encompasses a physiological decline in function, manifesting as an inability to adapt and respond to stressors[11]. It should be perceived as a vulnerability stemming from a combination of internal physiological factors and external stressors.
Several studies have shown adverse surgical outcomes in frail patients including Orthopedic, Urological, and Otolaryngological procedures[10,12-14]. However, the data on ERCP, especially in the nonagenarian population, is scarce. Therefore, we aimed to investigate the impact of frailty on ERCP-related hospitalization in this high-risk population.
Data was extracted from the National Readmission Database (NRD) from 2018 to 2020. The NRD is part of the Healthcare Cost and Utilization Project, sponsored by the Agency for Healthcare Research and Quality. The NRD contains data from approximately 18 million discharges each year across 28 geographically dispersed states. This data set accounts for 60% of the total United States resident population, 59% of all United States hospitalizations, and includes all tax-payer data[15]. The present study was deemed exempt by the institutional review board because the database contained de-identified data sets with prior ethical committee approval. The NRD is publicly available and can be procured from the Healthcare Cost and Utilization Project website[15].
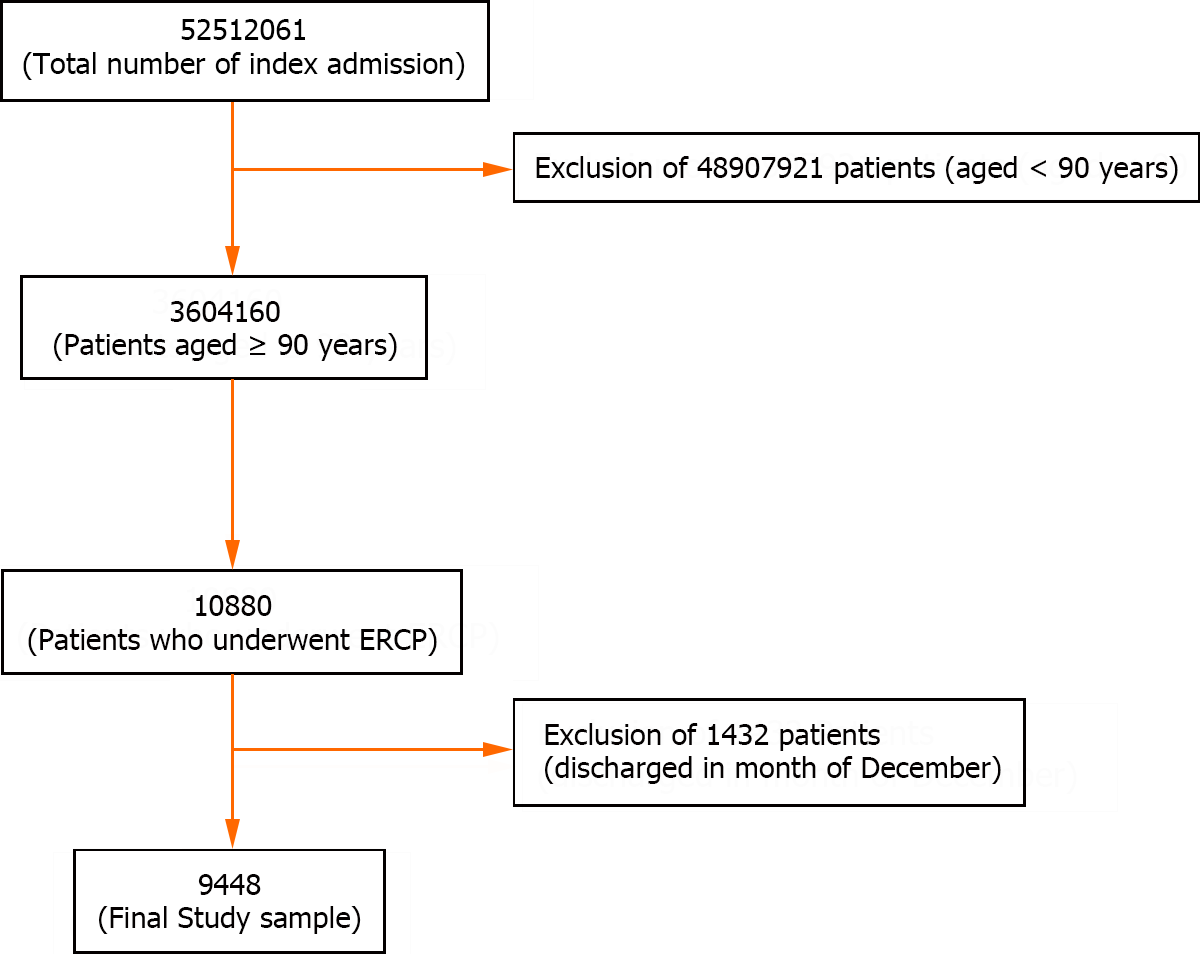
We identified 9448 patients who underwent elective or emergent ERCP, aged ≥ 90 years, using previously validated International Classification of Diseases, Tenth Revision, and Clinical Modification (ICD-10-CM) codes[16]. These patients were stratified into two cohorts based on Johns Hopkins’ ACG frailty indicator. These codes and strategies were validated and used in the previous studies[17]. Patients were excluded if they were aged < 90 years and were admitted in December.
We used the variables provided in the NRD by the Healthcare Cost and Utilization Project to identify patients’ baseline characteristics, including age, sex, primary expected payer, median household income category by patient zip code, and hospital information such as bed size, teaching status, and location. We used ICD-10-CM codes given by the Elixhauser comorbidity index calculator provided by the Healthcare Cost and Utilization Project to report hypertension, diabetes, hyperlipidemia, peripheral vascular disease, chronic heart failure, chronic pulmonary disease, anemia, obesity, smoking, and coagulopathy (Supplementary Table 1). Frailty was defined using Johns Hopkins’s ACG frailty indicator, which is based on a binary classification system, considering numerous clinical conditions as defined in Supplementary Table 1. Patients were classed as either frail or non-frail.
Statistical analyses were conducted using Stata, version 17.0 BE (StataCorp, College Station, TX, United States). The NRD is based on a complex sampling design that includes stratification, clustering, and weighting. Stata has a set of commands specifically designed to analyze the data while taking into consideration its complex design and produce nationally representative unbiased results, variance estimates, and P-values. A weighting of patient-level observations was implemented to obtain estimates for the entire population who underwent ERCP in the United States.
The Wilcoxon rank sum test was used for comparing continuous variables and χ2 tests for categorical variables. A multivariate regression analysis was used to calculate odds of all-cause 30 d readmission, inpatient mortality, length of stay, and total hospital charge (THC) after appropriately adjusting for age, gender, Elixhauser index, type of insurance, mean household income, and hospital characteristics, which included size, teaching status, and location.
The THC from 2018 through 2020 was adjusted for inflation in the healthcare sector using the Consumer Price Index inflation calculator maintained by the United States Bureau of Labor Statistics.
Multivariate regression models were used to adjust for confounders and were built using the following method: Univariate regression analyses on possible confounding factors were used to calculate the unadjusted odds ratio. Those with P-value ≤ 0.2 were chosen as potential confounding factors, along with clinical judgment. Indications for ERCP, which could also potentially be a part of Elixhauser's co-morbidity score were not included in the final analysis to prevent co-linearity. Potential confounding factors were then added to the final multivariate regression model. Missing values were not imputed. Two-sided P-values < 0.05 were taken to indicate statistical significance. We adhered to all methodological standards[18].
The primary outcome was in-hospital mortality following ERCP. Secondary outcomes were divided into in-hospital morbidity and 30 d readmission rates. In-hospital morbidity outcomes were Intra-procedural and post-procedural complications rates. Intra-procedural complications included bleeding, accidental punctures/lacerations of the biliary or gastrointestinal (GI) tract, and the need for mechanical ventilation. Post-procedural complications included bleeding (and post-ERCP pancreatitis. We described the ICD-10-CM coding of each outcome in Supplementary Table 1.
To evaluate the robustness of our findings, we conducted a falsification endpoint and E-value analysis to determine the validity of the study[19]. The E-value identifies the minimum strength of association that unmeasured confounders may need to have with both treatment and outcome, conditional on measured covariates, to fully explain the observed association. This estimates what the relative risk may have to be for any unmeasured confounder to overcome the observed association of study intervention with study outcomes.
Amongst patients aged 90 years or above, a total of 9448 underwent ERCP from 2018-2020 in the United States, excluding December (Figure 1). Of them, 3445 (36.46%) were frail while 6003 (63.53%) were non-frail. Females constituted 2305 (66.92%) and 3853 (64.19%) of Frail and the Non-frail population respectively. From a co-morbidity perspective, the number of patients progressively increased with the increasing score of the Elixhauser co-morbidity index. 81.29% of Frail patients had an Elixhauser score of 3 while in the non-frail group, it was 72.57% (P < 0.001). Frail patients had a higher proportion of Skilled nursing facility discharges (37.5%) while non-frail patients had a higher proportion of Routine/home discharges (49.18%) (P < 0.001). Frail patients had higher rates of sphincterotomies compared to non-frail patients (7.76% vs 5.62%; P = 0.002).
The intraprocedural complications including bleeding [0.11% vs 0.15%; adjusted odds ratio (aOR): 0.72] and accidental puncture/laceration of the biliary or GI tract (0.54% vs 0.65%; aOR: 0.77) between the frail and non-frail patients were insignificant (P > 0.05). Post-procedural complications including bleeding (0.49% vs 0.67%; aOR: 0.72) and post-ERCP pancreatitis (0.58% vs 0.4%; aOR: 1.4) were also insignificant between the two groups (P = 0.4).
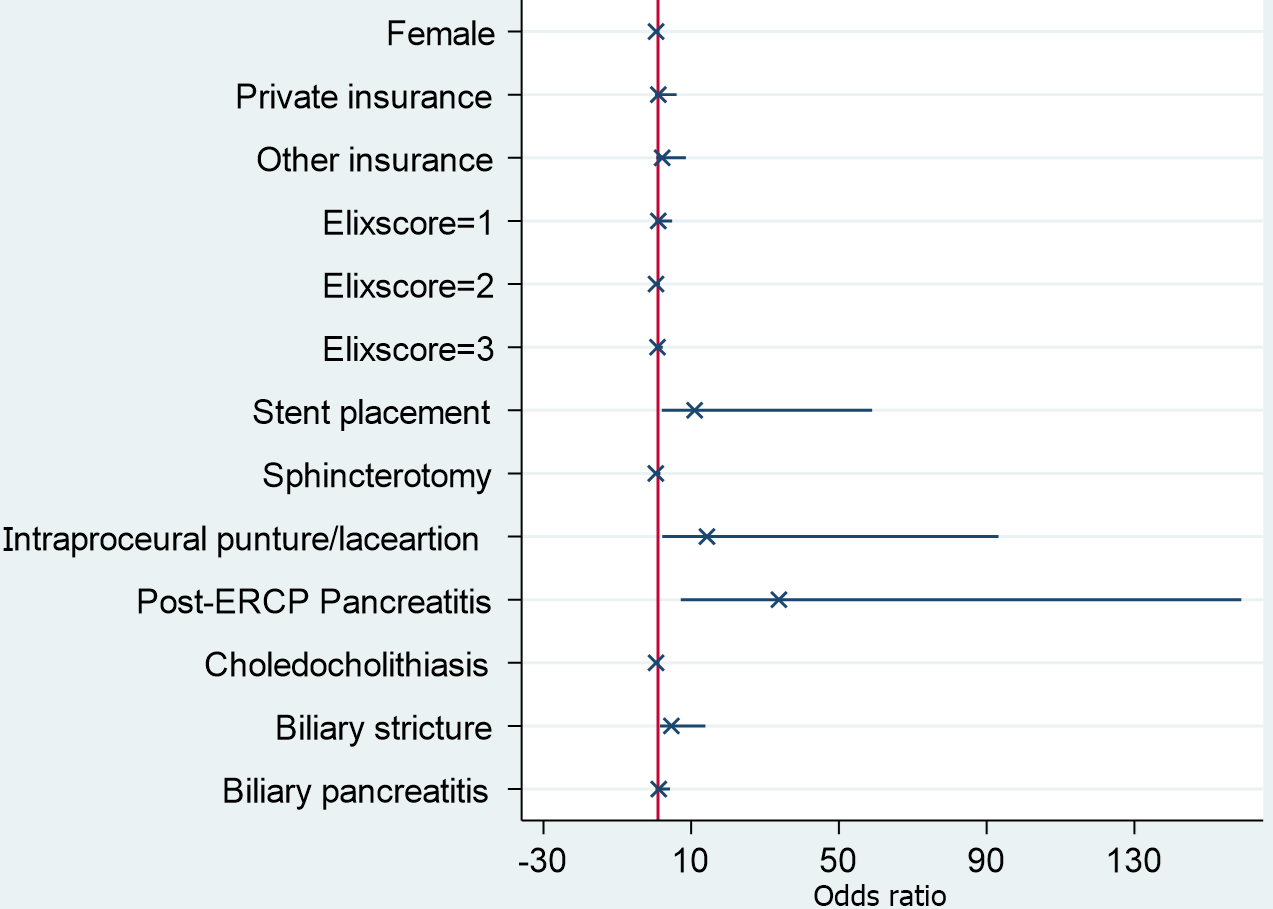
Indications for ERCP included choledocholithiasis (74.84%), biliary pancreatitis (9.19%), pancreaticobiliary cancer (7.6%), biliary stricture (4.84%), idiopathic pancreatitis (1.89%), cholangitis (1.51%), abnormal liver function tests (0.08%), and pancreatic pseudocyst (0.02%) shown in Figure 2. The mortality rate in frail patients was 2.03% vs 1.13% (aOR = 1.68%; P = 0.02) in non-frail patients. Female sex (aOR: 0.5, P = 0.02), stent placement (aOR: 9.8, P = 0.006), intraprocedural puncture/laceration of the biliary or GI tract (aOR: 11.3, P = 0.004) and post ERCP pancreatitis (aOR: 18.3, P < 0.001) were found to be an independent risk factor for mortality in the frail nonagenarian population (Figure 3). Frail patients also had a higher mean length of hospital stay (6.7 d vs 5.5 d; P < 0.001) and mean total hospital charges ($80490 vs $72878; P < 0.001) compared to non-frail patients.
The 30 d all-cause readmission rates between frail and non-frail patients were similar. (8.84% vs 8.57%, aOR: 0.99; P = 0.96). The most common causes of readmission included sepsis (44.8%), aspiration pneumonitis (13.03%), hypertensive heart disease with heart failure (19.7%), urinary tract infection (12.87%) and choledocholithiasis (12.29%).
To the best of our knowledge, this is the inaugural investigation employing the validated John Hopkins ACG frailty indicator to analyze clinical outcomes among nonagenarian patients who have undergone ERCP in the United States. In this study encompassing a national cross-section, we have noted several significant findings. First and foremost, frailty has exhibited an association with increased mortality rates following ERCP within this specific population, regardless of whether the admission was elective or emergent. Secondly, frailty has also shown a correlation with extended hospitalization durations and higher total hospital costs. Thirdly, the morbidity linked to the procedure and the readmission rates within 30 d did not exhibit substantial variations between frail and non-frail individuals.
Our study found that frail nonagenarian patients had a higher mortality risk compared to non-frail patients undergoing ERCP (aOR: 1.68, P = 0.02). Frailty has been identified as an independent risk factor of mortality across various surgical specialties[20]. Acosta et al[21] found a similar association between frailty and mortality in patients undergoing esophagogastroduodenoscopy for GI bleeding[21]. Traditionally, older age and/or multiple co-morbidities have been misunderstood as frailty. However, Frailty should be seen as a susceptibility to various internal physiological elements and external pressures. This phenomenon can manifest at different paces in various individuals, transcending age and impacting younger patients who have chronic illnesses or cognitive impairments[22]. Frail individuals tend to exhibit alterations in glucose metabolism, disruptions in the autonomic nervous system, modifications in the renin-angiotensin system and mitochondrial function, as well as irregularities in stress response systems[17]. These factors collectively contribute to unfavorable outcomes in these patients post-ERCP, as shown in our study. As for other predictors, female sex (aOR: 0.5, P = 0.02), stent placement (aOR: 9.8, P = 0.006), intraprocedural puncture/laceration of the biliary or GI tract (aOR: 11.3, P = 0.004) and Post ERCP pancreatitis (aOR: 18.3, P < 0.001) were found to be an independent risk factor for mortality in the frail nonagenarian population. Co-morbidities as defined by the Elixhauser co-morbidity index were significant in univariate analysis but lost their significance in the multivariate model to contribute towards mortality post-ERCP. This further re-reinforces the clinical significance of frailty in measuring outcomes.
We analyzed that the intra-procedural and post-procedural complication rates were insignificant between frail and non-frail patients, regardless of frailty and emergency of the procedure. Several studies have investigated whether elderly patients are at a higher risk for post-ERCP complications compared to their younger counterparts[23-26]. Sobani et al[27] showed that emergency ERCP and Charlson Comorbidity Index (CCI) ≥ 2 are associated with an increased adverse event rate in elderly patients[27]. Tabak et al[28] in their prospective study of 614 patients found that patients with a CCI ≥ 2 and difficult cannulation are associated with an increased overall adverse events rate, while age ≥ 80 years is not[28]. Takahashi et al[29] in their study found that age is a risk factor for increased rate of complications following ERCP[29]. There are several limitations in these studies including smaller sample size, overreliance on age and co-morbidities, and exclusion of the concept of frailty from the study.
In our study, frail patients exhibited a prolonged length of hospital stays compared to their non-frail counterparts (6.7 d vs 5.5 d; P < 0.001). Additionally, the mean total hospital cost for frail individuals was significantly higher, reaching $80490 compared to $72878 for non-frail individuals (P < 0.001). The observed numbers underscore the clinical significance of frailty, as they contribute to a notable increase in both healthcare costs and burden. Previous studies done by McDermott et al[30] and Khandelwal et al[31] have shown a similar association between frailty and increased mean length of hospital stay[30,31]. As previously discussed, altered physiological responses to stressors increase recovery time. The economic and healthcare implications of frailty emphasize the need for targeted interventions and strategies to address and mitigate the impact of frailty on both patient outcomes and healthcare resources.
The comparison of 30 d readmission rates between frail and non-frail patients yielded non-statistically significant results (P = 0.96). This discovery holds particular significance when it comes to the risk stratification of patients who might otherwise be overlooked or denied ERCP. While our study stands as the pioneering effort to employ frailty as a risk stratification tool for ERCP in the nonagenarian population, prior investigations have adopted a more limited approach by stratifying patients based on age. We consider this approach to be outdated for comprehending physi
Our study exhibits several strengths and, at the same time, some limitations. One notable strength is our utilization of a study population derived from the NRD, one of the largest and most ethnically diverse inpatient databases in the United States. Consequently, the findings from our study can be extrapolated to encompass all index hospitalizations and readmissions across the nation. Moreover, our study is among the few that scrutinize clinical outcomes of ERCP in frail nonagenarians at a national level, thereby providing a comprehensive perspective on the United States healthcare landscape. However, we must acknowledge the limitations associated with our study. Admissions were identified based solely on the primary diagnosis, aligning with the best practice methodologies outlined by the Healthcare Cost and Utilization Project. This established protocol ensures the accurate identification of cases requiring ERCP. However, it is important to note that there is a probability for patients to go undetected if their admission was a result of the disease, but the primary diagnosis did not reflect this.
Nonetheless, despite these limitations, we believe that the substantial sample size and our comprehensive analytical approach significantly contribute to a more profound understanding of the clinical outcomes of ERCP in the fragile nonagenarian population in the United States.
Identifying factors affecting inpatient mortality following ERCP is paramount as it furnishes therapeutic endoscopists with practical, real-world insights into individuals at an elevated risk of such outcomes. This information is instrumental in devising strategies that effectively reduce the mortality rates and the healthcare burden associated with these procedures. Furthermore, it is important to employ the concept of Frailty in daily clinical practice to help make better decisions in routine patient care.
Endoscopic retrograde cholangiopancreatography (ERCP) stands as a vital therapeutic instrument in the management of biliary and pancreatic disorders. Individuals classified as frail and elderly, particularly those aged ≥ 90 years, are commonly perceived as a high-risk demographic concerning complications associated with ERCP.
There is a paucity of literature and data in terms of large-scale multicenter retrospective studies that have investigated an association between Frailty and ERCP outcomes in the nonagenarian population.
To determine the association between Frailty and ERCP outcomes in the nonagenarian population. Outcomes included mortality, intra and post-procedural complication rates, length of hospital stay, healthcare cost, and 30 d readmission rates.
The 2018-2020 national readmission database was queried for patients aged ≥ 90 who underwent ERCP, using the international classification of diseases-10 code with clinical modification. Johns Hopkins’s adjusted clinical groups frailty indicator was used to classify patients as frail and non-frail. The primary outcome was mortality, and the secondary outcomes were morbidity and the 30 d readmission rate related to ERCP. We used univariate and multivariate regression models for analysis.
The population size included 9448 patients who were admitted for any indications of ERCP. Frail and non-frail patients were 3445 (36.46%) and 6003 (63.53%) respectively. Frail patients had higher mortality rates compared to non-frail individuals [adjusted odds ratio (aOR) = 1.68, P = 0.02]. There was no significant difference in intraprocedural complication rates, which included bleeding (aOR = 0.72, P = 0.67), accidental punctures/lacerations (aOR = 0.77, P = 0.5), and mechanical ventilation rates (aOR = 1.19, P = 0.6), between the two groups. Post-ERCP complication rate was similar for bleeding (aOR = 0.72, P = 0.41) and post-ERCP pancreatitis (aOR = 1.4, P = 0.44). Frail patients had a longer length of stay (6.7 d vs 5.5 d) and higher mean total charges of hospitalization ($78807 vs $71392) compared to controls (P < 0.001). The 30 d all-cause readmission rates between frail and non-frail patients were similar (aOR: 0.99; P = 0.96).
Frailty is associated with higher mortality post-ERCP in the nonagenarian population. Frailty is also associated with higher in-hospital length of stay and hospital costs.
There is a need for further prospective studies and randomized clinical trials to evaluate the impact of frailty in the nonagenarian population undergoing ERCP.
| 1. | Kröner PT, Bilal M, Samuel R, Umar S, Abougergi MS, Lukens FJ, Raimondo M, Carr-Locke DL. Use of ERCP in the United States over the past decade. Endosc Int Open. 2020;8:E761-E769. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 2. | Dahiya DS, Pinnam BSM, Chandan S, Gangwani MK, Ali H, Gopakumar H, Aziz M, Bapaye J, Al-Haddad M, Sharma NR. Clinical outcomes and predictors for 30-day readmissions of endoscopic retrograde cholangiopancreatography in the United States. J Gastroenterol Hepatol. 2024;39:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 3. | Facciorusso A, Ramai D, Gkolfakis P, Khan SR, Papanikolaou IS, Triantafyllou K, Tringali A, Chandan S, Mohan BP, Adler DG. Comparative efficacy of different methods for difficult biliary cannulation in ERCP: systematic review and network meta-analysis. Gastrointest Endosc. 2022;95:60-71.e12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 4. | Finkelmeier F, Tal A, Ajouaou M, Filmann N, Zeuzem S, Waidmann O, Albert J. ERCP in elderly patients: increased risk of sedation adverse events but low frequency of post-ERCP pancreatitis. Gastrointest Endosc. 2015;82:1051-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Glomsaker T, Hoff G, Kvaløy JT, Søreide K, Aabakken L, Søreide JA; Norwegian Gastronet ERCP Group. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg. 2013;100:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 102] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Coelho-Prabhu N, Shah ND, Van Houten H, Kamath PS, Baron TH. Endoscopic retrograde cholangiopancreatography: utilisation and outcomes in a 10-year population-based cohort. BMJ Open. 2013;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Coté GA, Imler TD, Xu H, Teal E, French DD, Imperiale TF, Rosenman MB, Wilson J, Hui SL, Sherman S. Lower provider volume is associated with higher failure rates for endoscopic retrograde cholangiopancreatography. Med Care. 2013;51:1040-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Hadaya J, Sanaiha Y, Juillard C, Benharash P. Impact of frailty on clinical outcomes and resource use following emergency general surgery in the United States. PLoS One. 2021;16:e0255122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Rubens M, Ramamoorthy V, Saxena A, Ruiz-Pelaez JG, Ahmed MA, Zhang Z, McGranaghan P, Chaparro S, Jimenez J. Association Between Frailty, 30-day Unplanned Readmission and Mortality After Hospitalization for Heart Failure: Results From the Nationwide Readmissions Database. J Aging Health. 2023;35:651-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Sia TY, Wen T, Cham S, Friedman AM, Wright JD. The effect of frailty on postoperative readmissions, morbidity, and mortality in endometrial cancer surgery. Gynecol Oncol. 2021;161:353-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Wleklik M, Uchmanowicz I, Jankowska EA, Vitale C, Lisiak M, Drozd M, Pobrotyn P, Tkaczyszyn M, Lee C. Multidimensional Approach to Frailty. Front Psychol. 2020;11:564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 83] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 12. | McIsaac DI, Bryson GL, van Walraven C. Association of Frailty and 1-Year Postoperative Mortality Following Major Elective Noncardiac Surgery: A Population-Based Cohort Study. JAMA Surg. 2016;151:538-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 247] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 13. | Goel AN, Lee JT, Gurrola JG 2nd, Wang MB, Suh JD. The impact of frailty on perioperative outcomes and resource utilization in sinonasal cancer surgery. Laryngoscope. 2020;130:290-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Michel J, Goel AN, Golla V, Lenis AT, Johnson DC, Chamie K, Litwin MS. Predicting Short-term Outcomes After Radical Cystectomy Based on Frailty. Urology. 2019;133:25-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Healthcare Cost and Utilization Project (HCUP) (2023). HCUP National Readmissions Database (NRD). In: Agency Healthc. Res. Qual. Rockville, MD. Available from: http://www.hcup-us.ahrq.gov/nrdoverview.jsp. |
| 16. | Radadiya D, Devani K, Ashhab A, Gaisinskaya P, Charilaou P, Reddy C, Gaddam S. US Nationwide Insight Into All-cause 30-day Readmissions following Inpatient Endoscopic Retrograde Cholangiopancreatography. J Clin Gastroenterol. 2023;57:515-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (1)] |
| 17. | Ramai D, Heaton J, Ofosu A, Gkolfakis P, Chandan S, Tringali A, Barakat MT, Hassan C, Repici A, Facciorusso A. Influence of Frailty in Patients Undergoing Endoscopic Retrograde Cholangiopancreatography for Biliary Stone Disease: A Nationwide Study. Dig Dis Sci. 2023;68:3605-3613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Khera R, Angraal S, Couch T, Welsh JW, Nallamothu BK, Girotra S, Chan PS, Krumholz HM. Adherence to Methodological Standards in Research Using the National Inpatient Sample. JAMA. 2017;318:2011-2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 602] [Article Influence: 66.9] [Reference Citation Analysis (0)] |
| 19. | Prasad V, Jena AB. Prespecified falsification end points: can they validate true observational associations? JAMA. 2013;309:241-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 222] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 20. | George EL, Hall DE, Youk A, Chen R, Kashikar A, Trickey AW, Varley PR, Shireman PK, Shinall MC Jr, Massarweh NN, Johanning J, Arya S. Association Between Patient Frailty and Postoperative Mortality Across Multiple Noncardiac Surgical Specialties. JAMA Surg. 2021;156:e205152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 21. | Acosta CJ, Goldberg D, Amin S. Evaluating the impact of frailty on periprocedural adverse events and mortality among patients with GI bleeding. Gastrointest Endosc. 2021;94:517-525.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Bagshaw SM, Stelfox HT, McDermid RC, Rolfson DB, Tsuyuki RT, Baig N, Artiuch B, Ibrahim Q, Stollery DE, Rokosh E, Majumdar SR. Association between frailty and short- and long-term outcomes among critically ill patients: a multicentre prospective cohort study. CMAJ. 2014;186:E95-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 402] [Article Influence: 30.9] [Reference Citation Analysis (0)] |
| 23. | Galeazzi M, Mazzola P, Valcarcel B, Bellelli G, Dinelli M, Pasinetti GM, Annoni G. Endoscopic retrograde cholangiopancreatography in the elderly: results of a retrospective study and a geriatricians' point of view. BMC Gastroenterol. 2018;18:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 24. | Saito H, Koga T, Sakaguchi M, Kadono Y, Kamikawa K, Urata A, Imamura H, Tada S, Kakuma T, Matsushita I. Safety and Efficacy of Endoscopic Removal of Common Bile Duct Stones in Elderly Patients ≥90 Years of Age. Intern Med. 2019;58:2125-2132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 25. | Iida T, Kaneto H, Wagatsuma K, Sasaki H, Naganawa Y, Nakagaki S, Satoh S, Shimizu H, Nakase H. Efficacy and safety of endoscopic procedures for common bile duct stones in patients aged 85 years or older: A retrospective study. PLoS One. 2018;13:e0190665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Yang JH, Li W, Si XK, Zhang JX, Cao YJ. Efficacy and Safety of Therapeutic ERCP in the Elderly: A Single Center Experience. Surg Laparosc Endosc Percutan Tech. 2018;28:e44-e48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Sobani ZA, Yunina D, Abbasi A, Tin K, Simkin D, Rojas M, Tsirlin Y, Mayer I, Rahmani R. Endoscopic Retrograde Cholangiopancreatography in Nonagenarian Patients: Is It Really Safe? Clin Endosc. 2018;51:375-380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Tabak F, Wang HS, Li QP, Ge XX, Wang F, Ji GZ, Miao L. Endoscopic retrograde cholangiopancreatography in elderly patients: Difficult cannulation and adverse events. World J Clin Cases. 2020;8:2988-2999. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 29. | Takahashi K, Tsuyuguchi T, Sugiyama H, Kumagai J, Nakamura M, Iino Y, Shingyoji A, Yamato M, Ohyama H, Kusakabe Y, Yasui S, Mikata R, Kato N. Risk factors of adverse events in endoscopic retrograde cholangiopancreatography for patients aged ≥85 years. Geriatr Gerontol Int. 2018;18:1038-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | McDermott A, Kerr G, Browne J. Association Between Clinical Frailty Scale Score and Length of Stay in a Complex Discharge Unit. Ir Med J. 2021;114:238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 31. | Khandelwal D, Goel A, Kumar U, Gulati V, Narang R, Dey AB. Frailty is associated with longer hospital stay and increased mortality in hospitalized older patients. J Nutr Health Aging. 2012;16:732-735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 143] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 32. | Parikh MP, Garg R, Chittajallu V, Gupta N, Sarvepalli S, Lopez R, Thota PN, Siddiki H, Bhatt A, Chahal P, Jang S, Stevens T, Vargo J, McCullough A, Sanaka MR. Trends and risk factors for 30-day readmissions in patients with acute cholangitis: analysis from the national readmission database. Surg Endosc. 2021;35:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 33. | Jeurnink SM. Clinical issues in endoscopic interventions for pancreatico-biliary disorders. s.n.; January 30, 2009. Available from: http://hdl.handle.net/1765/14646. |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Gastroenterology; American Society for Gastrointestinal Endoscopy; American Gastroenterological Association.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Giacomelli L, Italy S-Editor: Liu H L-Editor: A P-Editor: Cai YX