Published online Jan 16, 2024. doi: 10.4253/wjge.v16.i1.18
Peer-review started: August 26, 2023
First decision: November 20, 2023
Revised: December 2, 2023
Accepted: December 14, 2023
Article in press: December 14, 2023
Published online: January 16, 2024
Processing time: 141 Days and 17.3 Hours
The incidence and mortality rate of colorectal cancer progressively increase with age and become particularly prominent after the age of 50 years. Therefore, the population that is ≥ 50 years in age requires long-term and regular colonoscopies. Uncomfortable bowel preparation is the main reason preventing patients from undergoing regular colonoscopies. The standard bowel preparation regimen of 4-L polyethylene glycol (PEG) is effective but poorly tolerated.
To investigate an effective and comfortable bowel preparation regimen for hospitalized patients ≥ 50 years in age.
Patients were randomly assigned to group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) or group 2 (4-L PEG). Adequate bowel preparation was defined as a Boston bowel preparation scale (BBPS) score of ≥ 6, with a score of ≥ 2 for each segment. Non-inferiority was prespecified with a margin of 10%. Additionally, the degree of comfort was assessed based on the comfort questionnaire.
The proportion of patients with a BBPS score of ≥ 6 in group 1 was not significantly different from that in group 2, as demonstrated by intention-to-treat (91.2% vs 91.0%, P = 0.953) and per-protocol (91.8% vs 91.0%, P = 0.802) analyses. Furthermore, in patients ≥ 75 years in age, the proportion of BBPS scores of ≥ 6 in group 1 was not significantly different from that in group 2 (90.9% vs 97.0%, P = 0.716). Group 1 had higher comfort scores (8.85 ± 1.162 vs 7.59 ± 1.735, P < 0.001), longer sleep duration (6.86 ± 1.204 h vs 5.80 ± 1.730 h, P < 0.001), and fewer awakenings (1.42 ± 1.183 vs 2.04 ± 1.835, P = 0.026) than group 2.
For hospitalized patients ≥ 50 years in age, the bowel preparation regimen comprising 2-L PEG + 30-mL lactulose + a low-residue diet produced a cleanse that was as effective as the 4-L PEG regimen and even provided better comfort.
Core Tip: Individuals ≥ 50 years in age require long-term and regular colonoscopies. Uncomfortable bowel preparation is the main reason preventing patients from undergoing regular colonoscopies. The 4-L polyethylene glycol (PEG) regimen is effective but poorly tolerated. We observed that the 2-L PEG + 30-mL lactulose + low-residue diet regimen was not inferior to the 4-L PEG regimen. The 2-L PEG + 30-mL lactulose + low-residue diet regimen was more comfortable than the 4-L PEG regimen. In patients ≥ 75 years in age, 2-L PEG + 30-mL lactulose + low-residue diet regimen was still effective.
- Citation: He Y, Liu Q, Chen YW, Cui LJ, Cao K, Guo ZH. Bowel preparation protocol for hospitalized patients ages 50 years or older: A randomized controlled trial. World J Gastrointest Endosc 2024; 16(1): 18-28
- URL: https://www.wjgnet.com/1948-5190/full/v16/i1/18.htm
- DOI: https://dx.doi.org/10.4253/wjge.v16.i1.18
The incidence and mortality rate of colorectal cancer (CRC) progressively increase with age and become particularly prominent after the age of 50 years[1]. Furthermore, approximately 90% of CRC cases and deaths worldwide are estimated to occur in this age group[1]. Therefore, the notably higher risk for CRC in the population of ≥ 50 years in age necessitates long-term and regular colonoscopies. Using laxatives is one of the most uncomfortable aspects of the colonoscopy procedure and is a major deterrent to patients adhering to regular colonoscopies[2]. Thus, effective and comfortable bowel preparation regimens are required to promote regular colonoscopies among patients ≥ 50 years in age.
A high-dose (4 L) regimen of water-mixed polyethylene glycol (PEG) yields a good bowel cleansing effect[3], but patients poorly tolerate it due to the high volume of water consumed. Alternatively, a low-dose bowel preparation regimen using 2 L of water mixed with PEG and ascorbic acid has been proposed to improve tolerability in adults[4]. However, the risk of inadequate bowel preparation is higher in adults ≥ 50 years in age than in younger individuals. Advanced age, increasing prevalence of constipation, diabetes, and hypertension are all risk factors for inadequate bowel preparation[3,5]. Moreover, individuals of ages 50 years or older have a higher prevalence of comorbidities and are more likely to be on antiplatelet or anticoagulant medications, resulting in an increased risk during the pericolonoscopy period. Consequently, they have a higher proportion of hospitalizations for colonoscopy compared to younger individuals. Hospitalization itself is considered a risk factor for inadequate bowel preparation[3,5]. Limited clinical studies have been conducted to clarify the effectiveness and comfort of low-dose bowel preparation regimens in hospitalized patients ≥ 50 years in age.
Reducing water intake to 2 L can improve comfort[4], while following a low-residue diet[6] and using lactulose as an adjuvant[7] can enhance the effectiveness of bowel preparation. Therefore, we proposed a bowel preparation regimen involving a mixture of 2 L of water with PEG and lactulose along with a low-residue diet for hospitalized patients ≥ 50 years in age who were undergoing colonoscopy. We aimed to evaluate the effectiveness, comfort, and safety of this method. These study results may contribute to supporting and improving decision-making in clinical practice.
This was a prospective, single-blinded (endoscopist) randomized controlled trial conducted in a tertiary care hospital in Beijing, China, which included patients who underwent colonoscopy at the endoscopy center. All colonoscopies were scheduled in the afternoon. No endoscopists used additional adjuvants or adjuvant devices to improve bowel preparation.
Patients admitted to the Geriatrics Department for planned colonoscopy from January 2022 to June 2022 were included in the study. The criteria for patients to be admitted for colonoscopy were as follows: (1) Presence of ≥ 2 comorbidities (such as diabetes, hypertension, chronic heart failure, coronary heart disease, chronic kidney disease, chronic obstructive pulmonary disease, etc); (2) colon polyp diameter ≥ 1 cm, requiring polypectomy; (3) history of colon polyps with a diameter ≥ 1 cm; and/or (4) history of inadequate bowel preparation. Patient inclusion criteria included: (1) Age ≥ 50 years; (2) indication for colonoscopy; and (3) willingness to participate in the study. Exclusion criteria included: (1) Age < 50 years; (2) inability to complete bowel preparation; and (3) unwillingness to enroll in the study. The study design was reviewed and approved by the Ethics Committee of Beijing Tongren Hospital Affiliated to Capital Medical University (approval No. TRECKY2021-227). The trial registration number is NCT05397158.
A random sequence of 312 individuals was generated using statistical software. Participants were allocated to either group 1 or group 2 in accordance with their order of enrollment, following the sequentially assigned random sequence numbers. In group 1, the patients received 30 mL of lactulose in the morning before the colonoscopy day and consumed a low-residue liquid diet for breakfast, lunch, and dinner. The patients were then provided with 2 L of water mixed with PEG electrolyte powder on the morning of the colonoscopy and fasted for breakfast and lunch. In group 2, patients were allowed to have a regular diet for breakfast and lunch the day before the colonoscopy and a fasted, enteral nutritional emulsion or low-residue liquid diet for dinner (depending on the patient’s blood glucose and tolerance). They received 2 L of water mixed with PEG electrolyte powder in the afternoon before the colonoscopy. Then, the patients were administered 2 L of water mixed with PEG electrolyte powder on the morning of the colonoscopy and fasted for breakfast and lunch. The PEG electrolyte powder comprised PEG, sodium sulfate, sodium bicarbonate, sodium chloride, and potassium chloride.
Before bowel preparation, the physician explained the bowel preparation regimens to the patient and provided written bowel preparation instructions (Supplementary material) and a comfort questionnaire (Supplementary material). The questionnaire was completed by the patient and collected before the colonoscopy. Furthermore, the physician checked with the patient on the evening before the colonoscopy and on the morning of the colonoscopy to evaluate the bowel preparation. If the cleansing was poor and inadequate bowel preparation was predicted, 1 L of water mixed with PEG electrolyte powder was additionally provided on the morning of the colonoscopy, and the supplementation was recorded.
This study provided the foods that the patients should consume before their colonoscopy. A low-residue liquid diet was defined as a diet with a total fiber intake of < 10 g/d[3]. Breakfast included whole milk, white bread, and boiled eggs, lunch consisted of rice porridge, and dinner comprised rice porridge and steamed eggs. An enteral nutritional emulsion was used as a residue-free liquid diet.
The endoscopists were blinded in this study, wherein two endoscopists reviewed the colonoscopy images (30-50 images per patient) and assessed bowel preparation using the Boston bowel preparation scale (BBPS)[8] (Supplementary material). According to the BBPS, the colon is divided into three segments: right colon, transverse colon, and left colon (descending and rectosigmoid colon)[9]. Adequate bowel preparation was defined as a BBPS score of ≥ 6, with a score of ≥ 2 for each segment[10,11].
The following variables were recorded for the various aspects of the study: (1) Demographics of the study patients: Age, sex, lifestyle habits (including smoking and alcohol consumption), history of abdominopelvic surgery, comorbidities, and nutritional status (including body mass index, blood hemoglobin, and serum albumin); (2) Bowel preparation: Patient’s diet, type and dosage of laxatives administered, and interval between the last dose of laxatives and colonoscopy; (3) Colonoscopy: BBPS score of each bowel segment and the presence/absence of polyps, adenomas, or tumors (confirmed based on pathological examination); (4) Comfort: Comfort questionnaire results, including comfort score from 0 to 10, sleep duration on the night before colonoscopy, number of awakenings during sleep on the night before colonoscopy, and presence of bowel incontinence during bowel preparation; and (5) Safety: Laboratory test results of serum potassium, sodium, calcium, and creatinine and plasma B-type brain natriuretic peptide (BNP) before and after bowel preparation.
The primary outcome was to compare the percentage of adequate bowel preparation in each bowel segment and the whole colon in group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) with that in group 2 (4-L PEG) as well as to compare the mean BBPS scores in each bowel segment and the whole colon between the two groups. The secondary outcome was to compare the difference in the comfort and safety of bowel preparation between group 1 and group 2.
Continuous variables were expressed as mean ± SD, while categorical variables were represented as count (percentage). Continuous variables were compared using the student’s t-test or rank sum test, whereas the χ2 test was used to compare the categorical variables between the two groups. A P value of < 0.05 was considered significant. SPSS version 26 (IBM Corp, Armonk, NY, United States) was used for all statistical analyses.
Non-inferiority analysis was employed to determine whether the efficacy of the regimen of 2-L PEG + 30-mL lactulose + a low-residue diet was not inferior to that of the 4-L PEG regimen. According to the pre-experimental results and a previous study[12], the non-inferiority margin between the two bowel preparation regimens was set at 10%. A total of 22 patients per group was needed based on a type I error of 2.5%, power of 80%, and dropout rate of 10%. In this study, we intended to conduct a subgroup analysis on the population ≥ 75 years in age. In the preliminary experiment, this subgroup constituted approximately 15%-20% of the total population. To achieve a targeted subgroup sample size of 22 individuals per group, a final inclusion of 146 participants per group was determined. The analysis was performed using intention-to-treat and per-protocol approaches. We used the CONSORT reporting guidelines, with the CONSORT checklist published[13].
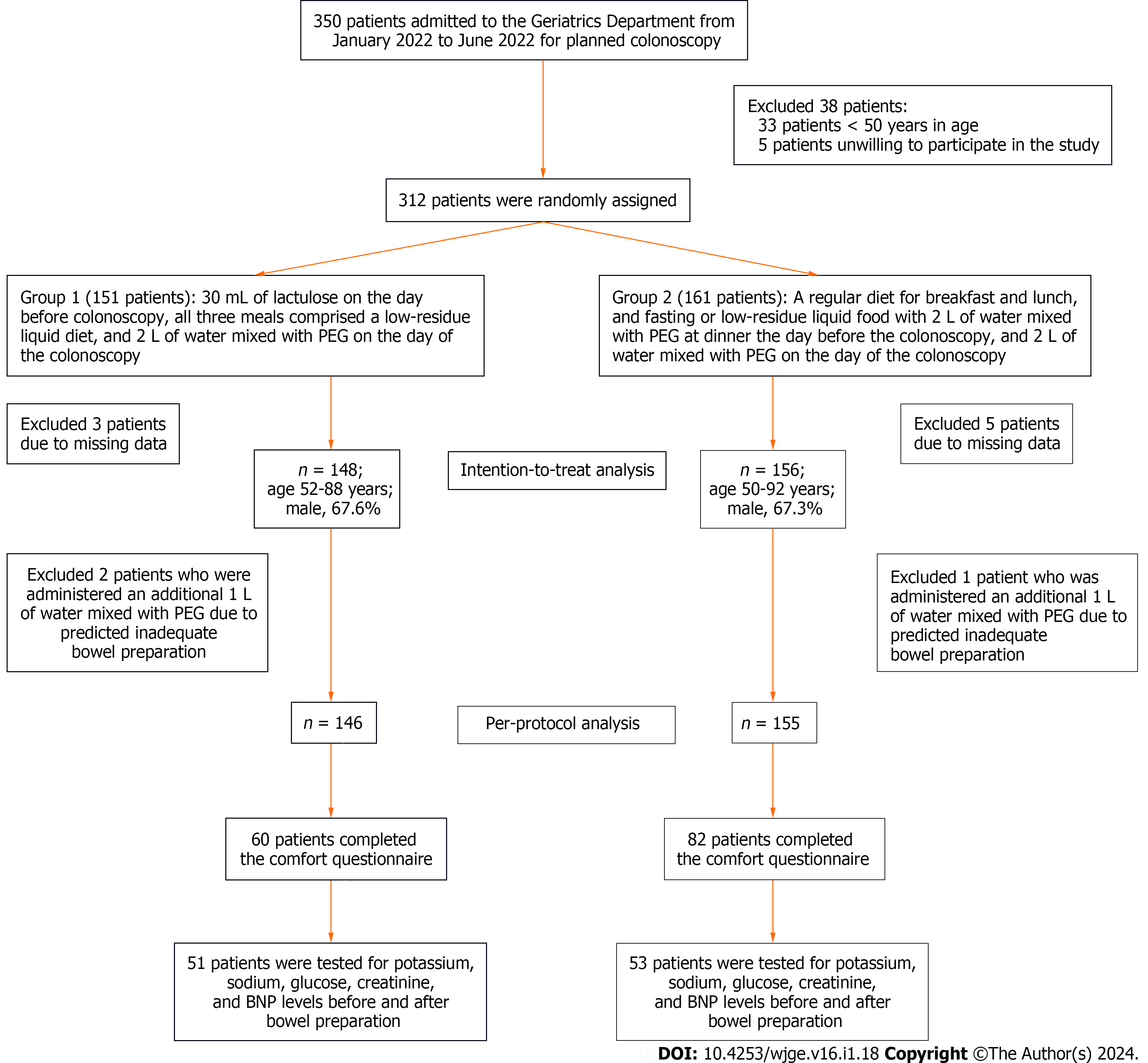
This study included 350 patients admitted to the Geriatrics Department for proposed colonoscopy between January 2022 and June 2022. Among these patients, 312 participated in the randomized grouping, from which 8 patients were excluded because of missing data. Ultimately, 148 patients were included in group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) and 156 in group 2 (4-L PEG). Further, 2 patients in group 1 and 1 patient in group 2 were excluded because they were administered an additional 1 L of PEG due to predicted inadequate bowel preparation. Figure 1 shows the flow chart of the study.
A total of 148 patients were included in group 1 (2-L PEG + 30-mL lactulose + a low-residue diet), with an age range of 52-88 years. Additionally, 156 patients were enrolled in group 2 (4-L PEG), with ages ranging from 50-92 years. No statistical differences in sex, age, lifestyle habits, history of abdominopelvic surgery, most comorbidities, or nutritional status were found between the two groups. Compared with the patients in group 2, those in group 1 had a significantly longer interval (4.71 ± 1.248 vs 4.26 ± 1.315, P = 0.003) between the last dose of laxatives and colonoscopy. Table 1 shows the complete demographic information.
| Characteristics | Group 11, n = 148 | Group 22, n = 156 | P value |
| Age in yr | 65.76 ± 7.843 | 66.99 ± 9.337 | 0.377 |
| Male sex | 100 (67.6) | 105 (67.3) | 0.961 |
| Lifestyle habits | |||
| Current smoking | 30 (20.3) | 33 (21.2) | 0.849 |
| Smoking history | 63 (42.6) | 66 (42.3) | 0.963 |
| Current drinking | 34 (23.0) | 35 (22.4) | 0.911 |
| Drinking history | 40 (27.0) | 41 (26.3) | 0.883 |
| History of abdominopelvic surgery | 41 (27.9) | 56 (36.1) | 0.125 |
| Comorbidity | |||
| Constipation | 19 (12.8) | 25 (16.0) | 0.430 |
| Drugs for constipation | 7 (4.7) | 10 (6.4) | 0.524 |
| Diabetes | 64 (43.2) | 74 (47.4) | 0.463 |
| Hypertension | 86 (58.1) | 89 (57.4) | 0.903 |
| Chronic heart failure | 2 (1.4) | 4 (2.6) | 0.728 |
| Coronary heart disease | 19 (12.8) | 34 (21.8) | 0.040 |
| Chronic kidney disease (≥ stage 2) | 99 (66.8) | 89 (57.0) | 0.280 |
| Chronic obstructive pulmonary disease | 6 (4.1) | 8 (5.1) | 0.655 |
| Nutritional status | |||
| BMI in kg/m2 | 24.325 ± 3.049 | 24.569 ± 2.936 | 0.718 |
| Hemoglobin in g/L | 135.91 ± 15.903 | 135.30 ± 15.906 | 0.675 |
| Albumin in g/L | 39.542 ± 3.0895 | 39.469 ± 3.7827 | 0.710 |
| Interval between last dose of laxatives and colonoscopy in h | 4.71 ± 1.248 | 4.26 ± 1.315 | 0.003 |
The results of the bowel preparation assessment in both groups were compared based on the intention-to-treat analysis (Table 2). The proportion of BBPS scores of ≥ 2 in the right colon (75.7% vs 74.4%, P = 0.791), transverse colon (98.0% vs 95.5%, P = 0.379), and left colon (100.0% vs 99.4%, P = 0.379) as well as the proportion of BBPS scores of ≥ 6 in the whole colon (91.2% vs 91.0%, P = 0.953) in group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) did not differ significantly from those in group 2 (4-L PEG). Similarly, the mean BBPS scores of the right colon, transverse colon, and left colon as well as that of the whole colon showed no differences between groups 1 and 2.
| Variables | Group 11 | Group 22 | P value |
| Intention-to-treat analysis | n = 148 | n = 156 | N/A |
| Right BBPS score ≥ 2 | 112 (75.7) | 116 (74.4) | 0.791 |
| Transverse BBPS score ≥ 2 | 145 (98.0) | 149 (95.5) | 0.379 |
| Left BBPS score ≥ 2 | 148 (100.0) | 155 (99.4) | 0.247 |
| Global BBPS score ≥ 6 | 135 (91.2) | 142 (91.0) | 0.953 |
| Mean BBPS in the right colon | 1.92 ± 0.634 | 1.92 ± 0.727 | 0.861 |
| Mean BBPS in the transverse colon | 2.73 ± 0.489 | 2.68 ± 0.556 | 0.539 |
| Mean BBPS in the left colon | 2.64 ± 0.483 | 2.58 ± 0.507 | 0.395 |
| Mean BBPS in the whole colon | 7.28 ± 1.167 | 7.18 ± 1.346 | 0.676 |
| Polyp detection rate | 108 (73.0) | 104 (66.7) | 0.232 |
| Adenoma detection rate | 84 (56.8) | 73 (46.8) | 0.082 |
| Tumor detection rate | 6 (4.1) | 5 (3.2) | 0.684 |
| Per-protocol analysis | n = 146 | n = 155 | N/A |
| Right BBPS score ≥ 2 | 112 (76.7) | 116 (74.8) | 0.705 |
| Transverse BBPS score ≥ 2 | 143 (97.9) | 148 (95.5) | 0.234 |
| Left BBPS score ≥ 2 | 146 (100.0) | 154 (99.4) | 0.331 |
| Global BBPS score ≥ 6 | 134 (91.8) | 141 (91.0) | 0.802 |
| Mean BBPS in the right colon | 1.93 ± 0.629 | 1.92 ± 0.726 | 0.924 |
| Mean BBPS in the transverse colon | 2.73 ± 0.488 | 2.68 ± 0.555 | 0.556 |
| Mean BBPS in the left colon | 2.64 ± 0.483 | 2.58 ± 0.508 | 0.354 |
| Mean BBPS in the whole colon | 7.30 ± 1.159 | 7.19 ± 1.347 | 0.639 |
| Polyp detection rate | 106 (72.6) | 103 (66.5) | 0.247 |
| Adenoma detection rate | 83 (56.8) | 72 (46.5) | 0.071 |
| Tumor detection rate | 6 (4.1) | 5 (3.2) | 0.674 |
The results of the bowel preparation assessment in the two groups were further compared using per-protocol analysis (Table 2). Group 1 and group 2 did not demonstrate significant differences in the proportion of BBPS scores of ≥ 2 in each segment as well as in the proportion of BBPS scores of ≥ 6 in the whole colon. Furthermore, no differences were observed between groups 1 and 2 in terms of mean BBPS scores of each segment as well as that of the whole colon.
Based on the intention-to-treat analysis, the detection rates of polyps (73.0% vs 66.7%, P = 0.232), adenomas (56.8% vs 46.8%, P = 0.082), and tumors (4.1% vs 3.2%, P = 0.684) were not significantly different between group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) and group 2 (4-L PEG) (Table 2).
The results of the per-protocol analysis also showed no significant differences in the detection rates of polyps, adenomas, and tumors between group 1 and group 2 (Table 2). Therefore, the bowel preparation regimen of 2-L PEG + 30-mL lactulose + a low-residue diet was not inferior to the 4-L PEG regimen for detecting polyps, adenomas, and tumors.
A total of 55 patients were of ages 75 years or older, among which 22 were in group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) and 33 in group 2 (4-L PEG). The two groups showed no differences in sex, age, history of abdominopelvic surgery, constipation, laxatives, diabetes mellitus, hypertension, nor nutritional status (body mass index, blood hemoglobin, and serum albumin) (Table 3).
| Characteristics | Group 11, n = 22 | Group 22, n = 33 | P value |
| Age in yr | 79.36 ± 4.22 | 81.03 ± 4.19 | 0.149 |
| Male sex | 15 (68.2) | 25 (75.8) | 0.537 |
| History of abdominopelvic surgery | 8 (36.4) | 15 (45.5) | 0.503 |
| Comorbidity | |||
| Constipation | 6 (27.3) | 8 (24.2) | 0.800 |
| Drugs for constipation | 2 (9.1) | 3 (9.1) | 1.000 |
| Diabetes | 12 (54.5) | 14 (42.4) | 0.378 |
| Hypertension | 17 (77.3) | 24 (72.7) | 0.848 |
| Nutritional status | |||
| BMI in kg/m2 | 24.16 ± 2.88 | 24.29 ± 2.53 | 0.542 |
| Hemoglobin in g/L | 128.50 ± 15.88 | 125.12 ± 16.39 | 0.203 |
| Albumin in g/L | 38.60 ± 4.05 | 37.88 ± 4.19 | 0.600 |
| Bowel preparation efficiency | |||
| Right BBPS score ≥ 2 | 16 (72.7) | 27 (81.8) | 0.641 |
| Transverse BBPS score ≥ 2 | 22 (100.0) | 32 (97.0) | 1.000 |
| Left BBPS score ≥ 2 | 22 (100.0) | 33 (100.0) | N/A |
| Global BBPS score ≥ 6 | 20 (90.9) | 32 (97.0) | 0.716 |
As revealed in Table 3, the proportions of BBPS scores of ≥ 2 in the right colon, transverse colon, and left colon as well as the proportion of BBPS scores of ≥ 6 in the whole colon in group 1 were not significantly different from those in group 2 (Table 3). Thus, in the case of patients ≥ 75 years in age, the bowel preparation efficiency in group 1 was not inferior to that in group 2.
Our results showed that group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) had higher comfort scores (8.85 ± 1.162 vs 7.59 ± 1.735, P < 0.001), longer sleep duration (6.86 ± 1.204 h vs 5.80 ± 1.730 h, P < 0.001), and fewer awakenings (1.42 ± 1.183 vs 2.04 ± 1.835, P = 0.026) on the night before the colonoscopy than group 2 (4-L PEG). Furthermore, compared with group 2, group 1 showed a reduced incidence of bowel incontinence during bowel preparation; however, this difference was not significant (Table 4). Therefore, patients in group 1 experienced better comfort than those in group 2.
The alterations in the levels of serum electrolytes (potassium, sodium, and calcium), serum creatinine, and plasma BNP before and after bowel preparation in group 1 were slight and not different from those in group 2 (Table 5). Thus, the two bowel preparation regimens had no significant effect on the electrolyte levels nor renal or cardiac function, with no significant difference between the two groups.
| Variables, before and after bowel preparation | Group 11, n = 51 | Group 22, n = 53 | P value |
| Serum potassium in mmol/L | 0.277 ± 0.288 | 0.275 ± 0.343 | 0.809 |
| Serum sodium in mmol/L | 1.804 ± 2.498 | 1.566 ± 2.508 | 0.878 |
| Serum calcium in mmol/L | 0.015 ± 0.117 | 0.018 ± 0.099 | 0.435 |
| Serum creatinine in µmol/L | 1.678 ± 6.110 | 3.832 ± 6.805 | 0.093 |
| Plasma BNP in pg/mL | 3.851 ± 30.264 | 8.0417 ± 64.987 | 0.216 |
Globally, the morbidity and mortality rates of CRC gradually increase with age and become particularly pronounced in individuals ≥ 50 years in age[1]. Hence, adults ≥ 50 years in age require regular colonoscopies. Our study results showed that the bowel preparation regimen comprising a low dose of 2-L PEG + 30-mL lactulose + a low-residue diet had a good bowel preparation effect along with comfort and safety profiles for patients ≥ 50 years in age. Furthermore, we observed that in the subgroup of patients ≥ 75 years in age who were at higher risk of inadequate bowel preparation, the 2-L PEG + 30-mL lactulose + a low-residue diet regime was not inferior to the 4-L PEG regimen.
In the subgroup analysis of individuals ≥ 75 years in age, group 1 exhibited a slightly lower percentage of adequate bowel preparation in the right colon compared to group 2, without statistical significance. This observation might be attributed to a longer time interval between the administration of the final bowel preparation agent and the colonoscopy procedure in group 1 compared to group 2. Furthermore, this study included a limited number of patients ≥ 75 years in age, and there was a disparity in the sample sizes between the two groups, which needs to be addressed in future studies. Therefore, further research is necessary to gain a more comprehensive understanding of the effectiveness of a low-dose bowel preparation regimen in achieving adequate preparation of the right colon in older individuals.
Comorbidities gradually increase with age in individuals ≥ 50 years in age. Multiple previous studies on bowel preparation have excluded patients with chronic kidney disease, chronic heart failure, long-term laxative use, long-term antiplatelet drug and anticoagulant drug use, or inflammatory bowel diseases[14,15]. In contrast, the present study included patients with such conditions, which reflected the real clinical practice situation. This makes the resulting findings more informative for clinical settings. In this study, notable differences were observed between the two groups of patients in terms of the proportion of individuals with concurrent coronary heart disease and the time interval between the administration of the final bowel preparation agent and the colonoscopy procedure. These differences might be attributed to the relatively small sample size in the study. In the future, it is necessary to further expand the sample size to reduce the influence of confounding factors on the study results.
Compared with fasting, a low-residue diet leads to better tolerance and patient compliance, leading to more patients being willing to review colonoscopy[6,16]. Previous studies also suggest that a longer low-residue diet (e.g., 3 d) before colonoscopy provides no additional benefit to bowel cleansing[17]. In the commonly used clinical method of 4 L of water mixed with PEG, there are no restrictions on breakfast and lunch on the day before the colonoscopy. Hence, in group 2 (4-L PEG), patients were allowed to consume a regular diet for breakfast and lunch on the day before the colonoscopy, while their dinner options were either a low-residue liquid diet or fasting, depending on the presence or absence of diabetes in each individual patient.
Laxative agents can be categorized into two main types: isotonic and hyperosmotic. Previous studies have shown that hyperosmotic laxatives can significantly increase the risk of deteriorating renal function[18]. Furthermore, in patients with inflammatory bowel disease, using hyperosmotic laxatives can increase the risk of worsening mucosal lesions associated with bowel preparation[19]. Therefore, the safer PEG-based isotonic laxative was chosen for this study of patients ≥ 50 years in age. Moreover, our results suggested that neither high doses (4 L) nor low doses (2 L) of PEG had a significant effect on electrolyte (potassium, sodium, and calcium) levels nor renal or cardiac function.
Lactulose, the adjuvant used in this study, is commonly used to treat constipation by promoting bowel movements. Previous studies in patients with constipation have demonstrated that the bowel preparation effect of PEG combined with lactulose is better than that of PEG alone[7]. Moreover, lactulose has a good taste and does not require large amounts of water in a short period. Thus, it can reduce the symptoms such as abdominal distension and nausea and improve patient tolerance.
In this study, BBPS was used to assess bowel preparation. The bowel preparation of the regimen was assessed after the endoscopist completed flushing and suction. The effectiveness and reliability of this scale have been confirmed by large sample-size studies[20].
Studies have demonstrated that an interval of 3-5 h between the last dose of laxatives and colonoscopy is optimal for good bowel preparation quality, with a minimum interval of at least 2 h[21]. However, the current study was limited by the number of endoscopists and scheduling of the colonoscopies. Thus, some patients had an interval of > 5 h between the last dose of laxatives and colonoscopy. The patients in group 1 (2-L PEG + 30-mL lactulose + a low-residue diet) had a significantly longer interval (closer to 5 h) between the last dose of laxatives and colonoscopy than those in group 2 (4-L PEG) (4.71 ± 1.248 vs. 4.26 ± 1.315, P = 0.003). Nevertheless, our results demonstrated that the 2-L PEG + 30-mL lactulose + a low-residue diet regimen was still not inferior to the 4-L PEG regimen for bowel preparation.
Regarding comfort during bowel preparation, previous studies have used the incidence of nausea and vomiting as an assessment indicator[15] but have not evaluated the sleep situation and fecal incontinence on the night before the colonoscopy. The present study highlighted that the 2-L PEG + 30-mL lactulose + a low-residue diet regimen resulted in longer sleep duration, fewer awakenings, and a reduced incidence of fecal incontinence than the 4-L PEG regimen on the night before the colonoscopy. Additionally, the overall comfort score was higher with the 2-L PEG + 30-mL lactulose + a low-residue diet approach than in the 4-L PEG regimen, suggesting better patient tolerance that may promote long-term regular colonoscopy participation.
The study results also indicated good bowel preparation in older adults (age ≥ 75 years) using a low dose of laxatives (2-L PEG + 30-mL lactulose + a low-residue diet). However, the comfort and safety parameters in this subgroup were not evaluated due to the limited number of patients available. Therefore, further studies should be conducted to assess bowel preparation in the older population of ≥ 75 years in age.
This study exclusively included hospitalized patients. However, in other countries, a portion of patients may choose outpatient colonoscopy examinations based on local circumstances. Due to the relatively short duration of hospital stay for the participants in this study, their clinical characteristics resembled those of outpatient cases. Therefore, the results of this study may be applicable to outpatient populations.
Patients ≥ 50 years in age require long-term and regular colonoscopies due to the notably higher CRC morbidity and mortality rates. The bowel preparation regimen of low-dose (2 L) PEG combined with lactulose and a low-residue diet was comparable with the high-dose (4 L) PEG regimen for bowel cleansing and even provided better comfort.
The incidence and mortality rates of colorectal cancer (CRC) progressively increase with age, and this rise is particularly prominent after the age of 50 years. Therefore, the population ≥ 50 years in age requires long-term and regular colonoscopies. Uncomfortable bowel preparation is the main reason that prevents patients from undergoing regular colonoscopies. The bowel preparation regimen of 4-L polyethylene glycol (PEG) is effective but poorly tolerated.
Reducing water intake to 2 L can improve comfort, while following a low-residue diet and using lactulose as an adjuvant can enhance the effectiveness of bowel preparation. Therefore, we proposed a bowel preparation regimen involving a mixture of 2 L water with PEG and lactulose along with a low-residue diet for hospitalized patients ≥ 50 years in age who were undergoing colonoscopy.
This study aimed to evaluate the effectiveness, comfort, and safety of a 2-L PEG + 30-mL lactulose + low-residue diet regimen.
Non-inferiority analysis was employed to determine whether the efficacy of the regimen of 2-L PEG + 30-mL lactulose + a low-residue diet was not inferior to that of the 4-L PEG regimen. The analysis was performed using intention-to-treat and per-protocol approaches. The primary outcome was to compare the percentage of adequate bowel preparation in each bowel segment and the whole colon in group 1 with that in group 2 as well as to compare the mean Boston bowel preparation scale scores in each bowel segment and the whole colon between the two groups. The secondary outcome was to compare the difference in the comfort and safety of bowel preparation between group 1 and group 2. The comfort assessment included comfort score, sleep duration on the night before colonoscopy, number of awakenings during sleep on the night before colonoscopy, and the presence of bowel incontinence during bowel preparation. Safety assessment included laboratory test results of serum potassium, sodium, calcium, and creatinine and plasma B-type brain natriuretic peptide before and after bowel preparation.
The bowel preparation regimen comprising a low dose of 2-L PEG + 30-mL lactulose + a low-residue diet had a good bowel preparation effect along with comfort and safety profiles for patients ≥ 50 years in age. Furthermore, in the subgroup of patients ≥ 75 years in age who were at higher risk of inadequate bowel preparation, the 2-L PEG + 30-mL lactulose + a low-residue diet regime was not inferior to the 4-L PEG regimen.
In patients ≥ 50 years in age, the bowel preparation regimen comprising 2-L PEG + 30-mL lactulose + a low-residue diet produced a cleanse that was as effective as that yielded by the 4-L PEG regimen and even provided better comfort.
Patients ≥ 50 years in age require long-term and regular colonoscopies due to their notably higher CRC morbidity and mortality. The bowel preparation regimen of 2-L PEG + 30-mL lactulose + a low-residue diet is comparable with the high-dose (4 L) PEG regimen for bowel cleansing and even provides better comfort. These study results may contribute to supporting and improving decision-making in clinical practice.
The authors are grateful to Han-Yang Wang for his help in completion of this manuscript.
| 1. | Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16:713-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 777] [Cited by in RCA: 1778] [Article Influence: 254.0] [Reference Citation Analysis (2)] |
| 2. | McLachlan SA, Clements A, Austoker J. Patients' experiences and reported barriers to colonoscopy in the screening context--a systematic review of the literature. Patient Educ Couns. 2012;86:137-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 207] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 3. | Hassan C, East J, Radaelli F, Spada C, Benamouzig R, Bisschops R, Bretthauer M, Dekker E, Dinis-Ribeiro M, Ferlitsch M, Fuccio L, Awadie H, Gralnek I, Jover R, Kaminski MF, Pellisé M, Triantafyllou K, Vanella G, Mangas-Sanjuan C, Frazzoni L, Van Hooft JE, Dumonceau JM. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2019. Endoscopy. 2019;51:775-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 407] [Cited by in RCA: 404] [Article Influence: 57.7] [Reference Citation Analysis (6)] |
| 4. | Xie Q, Chen L, Zhao F, Zhou X, Huang P, Zhang L, Zhou D, Wei J, Wang W, Zheng S. A meta-analysis of randomized controlled trials of low-volume polyethylene glycol plus ascorbic acid versus standard-volume polyethylene glycol solution as bowel preparations for colonoscopy. PLoS One. 2014;9:e99092. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Mahmood S, Farooqui SM, Madhoun MF. Predictors of inadequate bowel preparation for colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2018;30:819-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 154] [Article Influence: 19.3] [Reference Citation Analysis (1)] |
| 6. | Zhang X, Wu Q, Wei M, Ding Y, Gu C, Liu S, Wang Z. Low-residual diet versus clear-liquid diet for bowel preparation before colonoscopy: meta-analysis and trial sequential analysis of randomized controlled trials. Gastrointest Endosc. 2020;92:508-518.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Lu J, Cao Q, Wang X, Pu J, Peng X. Application of Oral Lactulose in Combination With Polyethylene Glycol Electrolyte Powder for Colonoscopy Bowel Preparation in Patients With Constipation. Am J Ther. 2016;23:e1020-e1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Jacobson BC, Calderwood AH. Measuring bowel preparation adequacy in colonoscopy-based research: review of key considerations. Gastrointest Endosc. 2020;91:248-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Parekh PJ, Oldfield EC 4th, Johnson DA. Bowel preparation for colonoscopy: what is best and necessary for quality? Curr Opin Gastroenterol. 2019;35:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Calderwood AH, Schroy PC 3rd, Lieberman DA, Logan JR, Zurfluh M, Jacobson BC. Boston Bowel Preparation Scale scores provide a standardized definition of adequate for describing bowel cleanliness. Gastrointest Endosc. 2014;80:269-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 156] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 11. | Clark BT, Protiva P, Nagar A, Imaeda A, Ciarleglio MM, Deng Y, Laine L. Quantification of Adequate Bowel Preparation for Screening or Surveillance Colonoscopy in Men. Gastroenterology. 2016;150:396-405; quiz e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 161] [Article Influence: 16.1] [Reference Citation Analysis (1)] |
| 12. | Gimeno-García AZ, Hernandez G, Aldea A, Nicolás-Pérez D, Jiménez A, Carrillo M, Felipe V, Alarcón-Fernández O, Hernandez-Guerra M, Romero R, Alonso I, Gonzalez Y, Adrian Z, Moreno M, Ramos L, Quintero E. Comparison of Two Intensive Bowel Cleansing Regimens in Patients With Previous Poor Bowel Preparation: A Randomized Controlled Study. Am J Gastroenterol. 2017;112:951-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 13. | Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 2010;1:100-107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 334] [Cited by in RCA: 1144] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 14. | Hernandez PV, Horsley-Silva JL, Snyder DL, Baffy N, Atia M, Koepke L, Buras MR, Lim ES, Ruff K, Umar SB, Islam S, Ramirez FC. Effect of bowel preparation volume in inpatient colonoscopy. Results of a prospective, randomized, comparative pilot study. BMC Gastroenterol. 2020;20:227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Zhang M, Zou W, Xu C, Jia R, Liu K, Xu Q, Xu H. Polyethylene glycol combined with linaclotide is an effective and well-tolerated bowel preparation regimen for colonoscopy: an endoscopist-blinded, randomized, controlled trial. Eur J Gastroenterol Hepatol. 2021;33:e625-e633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Wu R, Ji WY, Yang C, Zhan Q. A Systematic Review and Meta-Analysis of Low-Residue Diet Versus Clear Liquid Diet: Which Is Better for Bowel Preparation Before Colonoscopy? Gastroenterol Nurs. 2021;44:341-352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Gimeno-García AZ, de la Barreda Heuser R, Reygosa C, Hernandez A, Mascareño I, Nicolás-Pérez D, Jiménez A, Lara AJ, Alarcon-Fernández O, Hernandez-Guerra M, Romero R, Alonso I, González Y, Adrian Z, Hernandez G, Hernandez D, Delgado R, Quintero E. Impact of a 1-day versus 3-day low-residue diet on bowel cleansing quality before colonoscopy: a randomized controlled trial. Endoscopy. 2019;51:628-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Russmann S, Lamerato L, Motsko SP, Pezzullo JC, Faber MD, Jones JK. Risk of further decline in renal function after the use of oral sodium phosphate or polyethylene glycol in patients with a preexisting glomerular filtration rate below 60 ml/min. Am J Gastroenterol. 2008;103:2707-2716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 19. | Lawrance IC, Willert RP, Murray K. Bowel cleansing for colonoscopy: prospective randomized assessment of efficacy and of induced mucosal abnormality with three preparation agents. Endoscopy. 2011;43:412-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Di Leo M, Iannone A, Arena M, Losurdo G, Palamara MA, Iabichino G, Consolo P, Rendina M, Luigiano C, Di Leo A. Novel frontiers of agents for bowel cleansing for colonoscopy. World J Gastroenterol. 2021;27:7748-7770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 21. | Seo EH, Kim TO, Park MJ, Joo HR, Heo NY, Park J, Park SH, Yang SY, Moon YS. Optimal preparation-to-colonoscopy interval in split-dose PEG bowel preparation determines satisfactory bowel preparation quality: an observational prospective study. Gastrointest Endosc. 2012;75:583-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Chinese Society of Geriatric.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gunnarsson U, Sweden S-Editor: Qu XL L-Editor: A P-Editor: Cai YX