©The Author(s) 2025.
World J Gastrointest Endosc. Dec 16, 2025; 17(12): 114581
Published online Dec 16, 2025. doi: 10.4253/wjge.v17.i12.114581
Published online Dec 16, 2025. doi: 10.4253/wjge.v17.i12.114581
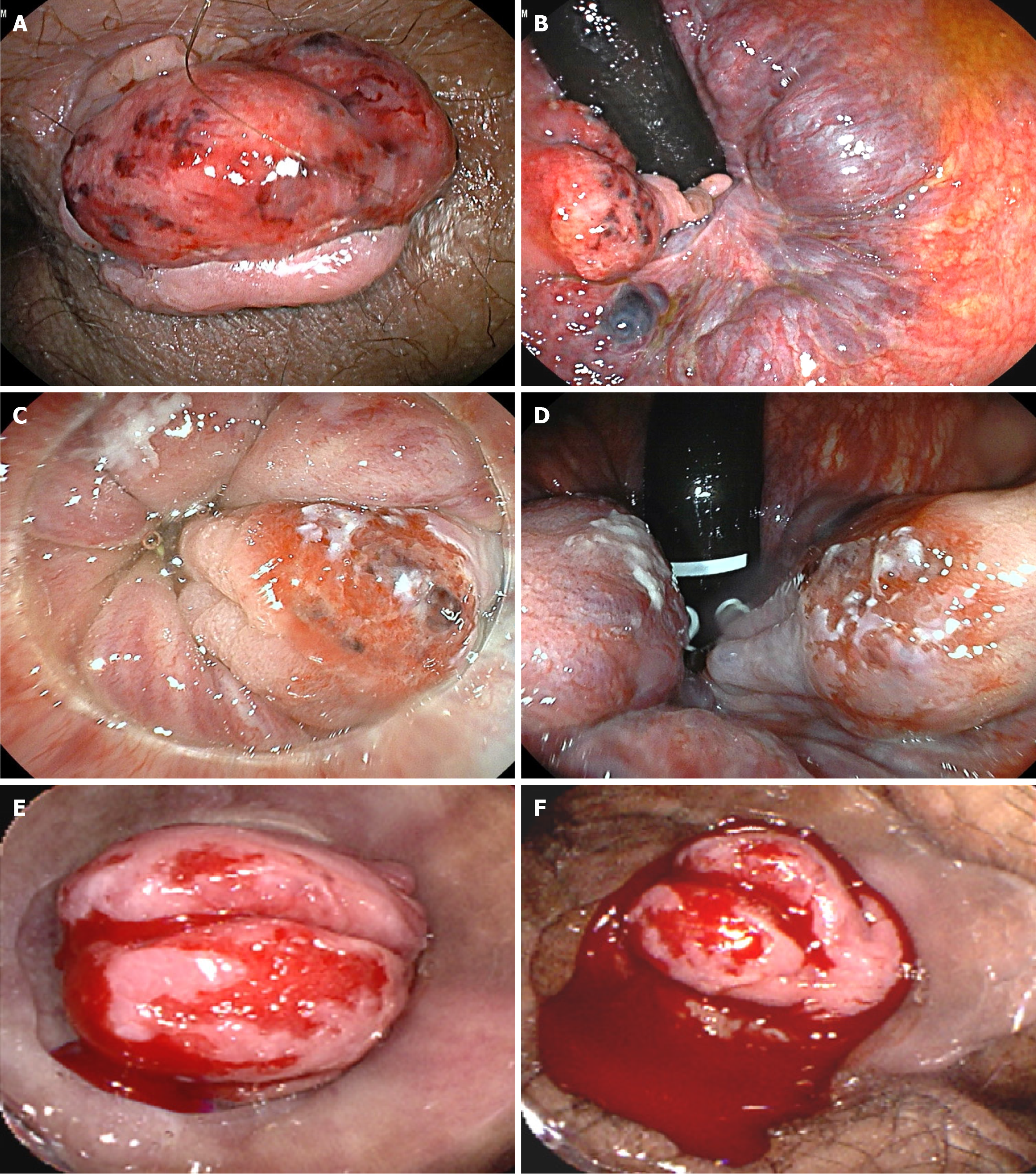
Figure 1 Internal hemorrhoid sites with evident bleeding.
A: Grade III hemorrhoidal prolapse and several small spots of active bleeding (case 1); B: Rectal retroflexion of the colonoscope (case 1); C: Grade II hemorrhoidal prolapse and stigmas of recent bleeding (case 2); D: Rectal retroflexion of the colonoscope (case 2); E and F: Massive hemorrhoidal bleeding (case 3).
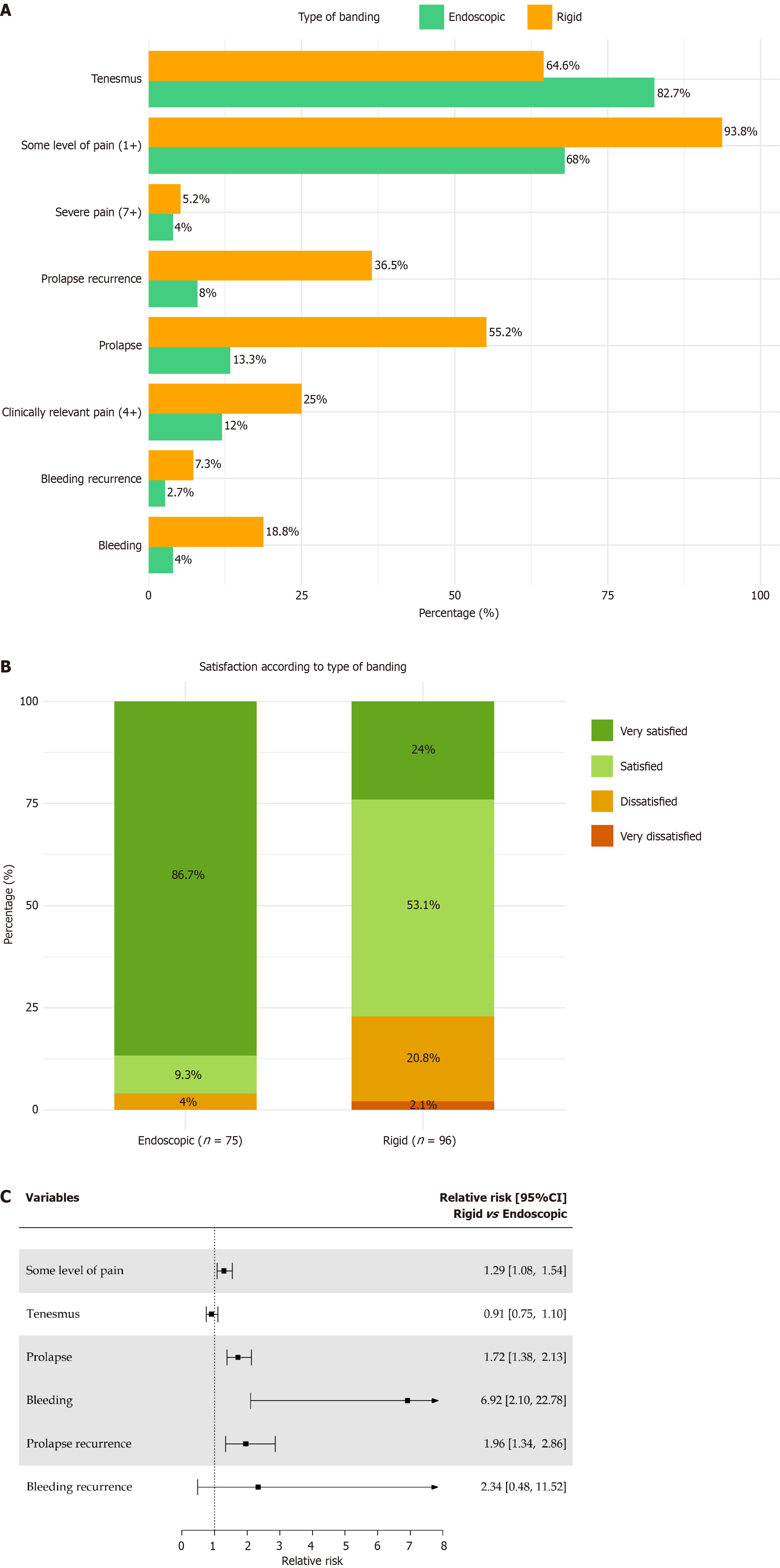
Figure 2 Comparative clinical outcomes of endoscopic vs rigid band ligation: From symptom distribution to patient satisfaction.
A: Distribution of symptoms according to the type of ligation; B: Forest plot of the relative risks of clinical outcomes according to the type of ligation; C: Patient satisfaction after endoscopic and rigid banding ligation, bleeding and prolapse resolution. CI: Confidence interval.
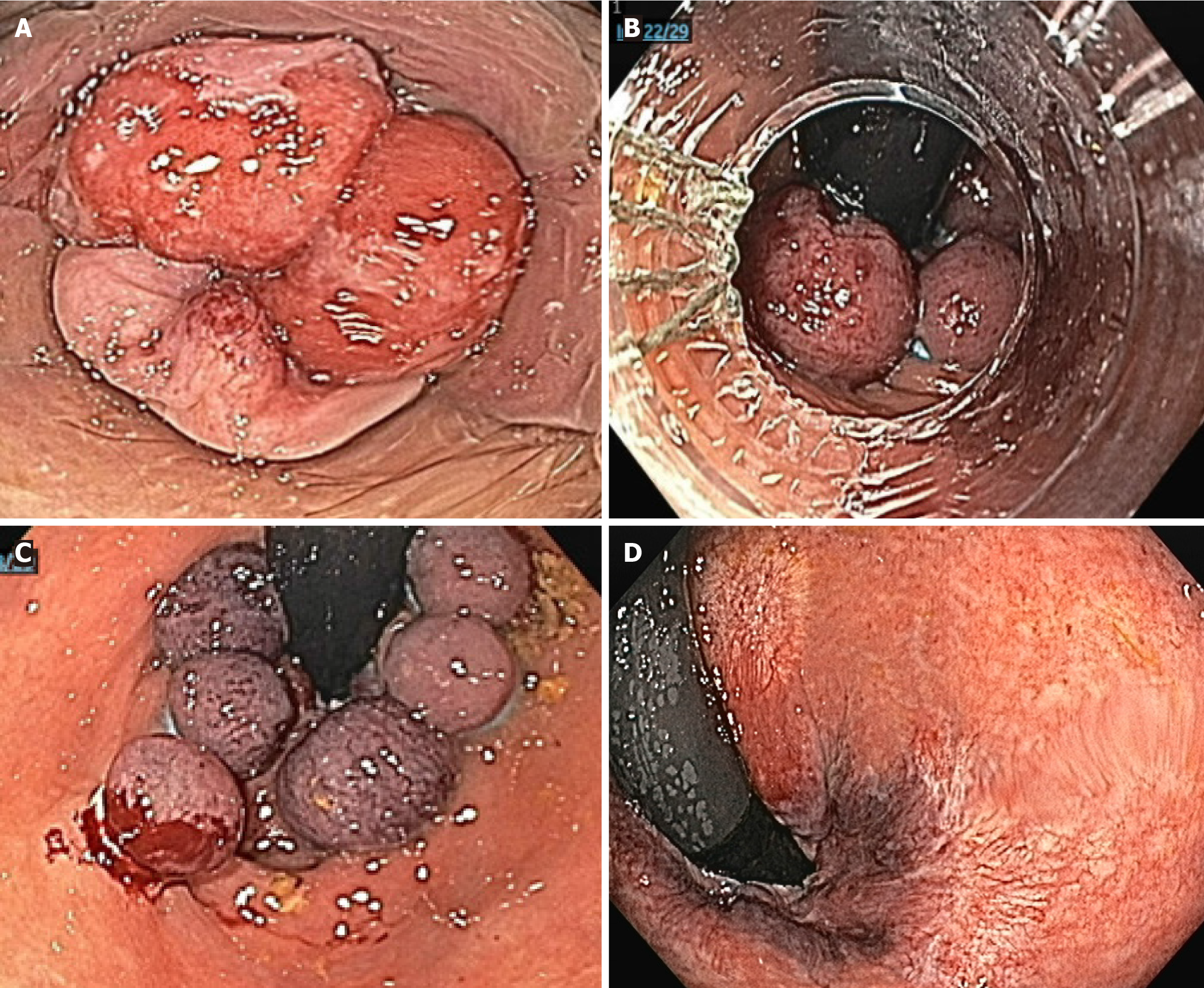
Figure 3 Endoscopic band ligation.
A: Grade III hemorrhoidal prolapse; B: Placement of 6 elastic bands above the dentate line; C: Rectal retroflexion after endoscopic band ligation; D: Complete resolution after 6 months.
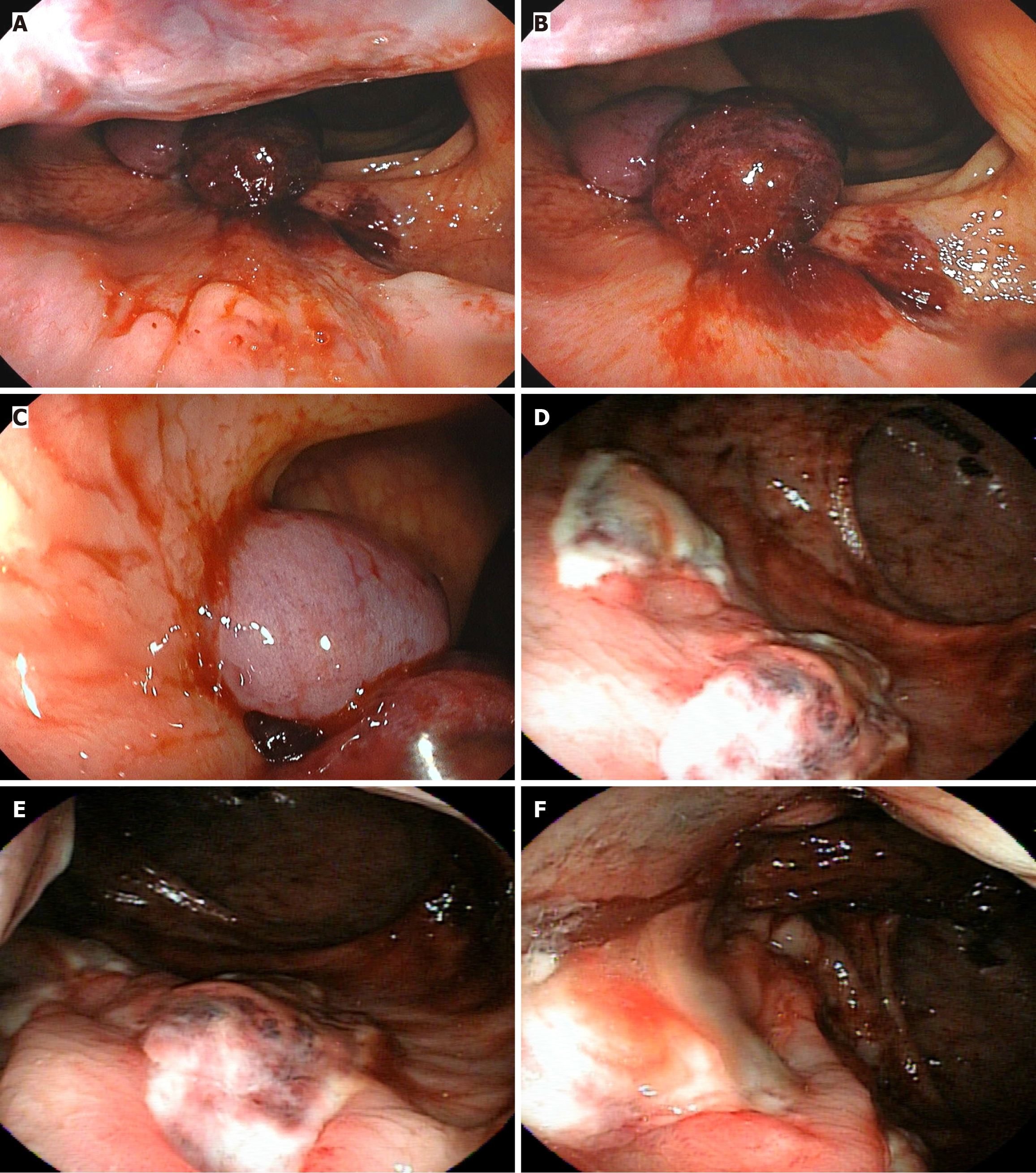
Figure 4 Ulcers in the anal canal after rigid proctoscope band ligation.
A-C: Placement of 4 elastic bands above the dentate line; D-F: Deep ulcers in the anal canal.
- Citation: Gomes A, Barrio E, Gomes G, Souza JHCG, Pinto PCC, Borghesi RA. Hemorrhoidal elastic band ligation during routine colonoscopy: A comparative study between flexible video endoscopy and rigid proctoscopy. World J Gastrointest Endosc 2025; 17(12): 114581
- URL: https://www.wjgnet.com/1948-5190/full/v17/i12/114581.htm
- DOI: https://dx.doi.org/10.4253/wjge.v17.i12.114581