Published online Feb 18, 2017. doi: 10.4254/wjh.v9.i5.263
Peer-review started: August 14, 2016
First decision: September 2, 2016
Revised: October 28, 2016
Accepted: December 7, 2016
Article in press: December 9, 2016
Published online: February 18, 2017
Processing time: 187 Days and 21.8 Hours
To verify how malnutrition is related to health-related quality of life (HRQL) impairment in patients with cirrhosis.
Data was retrospectively abstracted from medical records and obtained by direct interview. We included patients with cirrhosis from any etiology, evaluated at the Liver Clinic from Gastroenterology Department in a tertiary healthcare center, from June 2014 to June 2016. Child-Pugh score, data about complications, and demographic, clinical and anthropometric characteristics of patients were obtained. Nutritional status was evaluated by the Subjective Global Assessment (SGA). HRQL was evaluated through the Chronic Liver Disease Questionnaire. Patients were requested to assess their global HRQL with the following code: 0 = impairment of HRQL, when it was compared with other healthy subjects; 1 = good HRQL, if it was similar to the quality of life of other healthy subjects. To compare the primary outcome between malnourished and well-nourished groups, the χ2 test, Fisher’s exact test or Student’s t-test were used, based on the variable type. Associations between predictor variables and deterioration of HRQL were determined by calculating the hazard ratio and 95% confidence interval using Cox proportional hazards regression.
A total of 127 patients with cirrhosis were included, and the mean age was 54.1 ± 12.3 years-old. According to Child-Pugh scoring, 25 (19.7%) were classified as A (compensated), 76 (59.8%) as B, and 26 (20.5%) as C (B/C = decompensated). According to SGA, 58 (45.7%) patients were classified as well-nourished. Sixty-nine patients identified HRQL as good, and 76 patients (59.8%) perceived impairment of their HRQL. Multivariate analysis to determine associations between predictor variables and self-perception of an impairment of HRQL found strong association with malnutrition (P < 0.0001). The most important impaired characteristics in malnourished patients were: Presence of body pain, dyspnea on exertion with daily activities, decreased appetite, generalized weakness, trouble lifting or carrying heavy objects, and decreased level of energy (P < 0.0001).
Malnutrition is a key factor related to impairment of HRQL in patients with cirrhosis.
Core tip: Several factors, particularly the severity of disease, development of ascites, need for paracentesis and history of hospitalization for any cause, are factors that worsen the health-related quality of life (HRQL) of patients with cirrhosis. Noteworthy malnutrition is a very important factor which impacts negatively on HRQL of patients suffering cirrhosis; clinicians must recognize it promptly and search for strategies to avoid this preventable comorbidity.
- Citation: Rojas-Loureiro G, Servín-Caamaño A, Pérez-Reyes E, Servín-Abad L, Higuera-de la Tijera F. Malnutrition negatively impacts the quality of life of patients with cirrhosis: An observational study. World J Hepatol 2017; 9(5): 263-269
- URL: https://www.wjgnet.com/1948-5182/full/v9/i5/263.htm
- DOI: https://dx.doi.org/10.4254/wjh.v9.i5.263
Cirrhosis and its complications are important factors which contribute to mortality worldwide[1]. Compared with healthy people, the patients with compensated cirrhosis have five times more risk of non-survival, and those with decompensated cirrhosis have ten times more risk of non-survival during follow-up[2].
Malnutrition is highly prevalent in cirrhotic patients. It is related to development of complications, or even death[3-5].
Despite new treatment options for viral hepatitis, the high frequency of undiagnosed patients with chronic viral hepatitis and the increased incidence of metabolic syndrome with non-alcoholic steatohepatitis had led to the number of individuals progressing to cirrhosis being expected to increase until about 2030[6]. Moreover, despite increased knowledge of the pathogenesis of cirrhosis and major advances in the treatment, there remains a paucity of information related to health-related quality of life (HRQL) in these patients. Furthermore, the emotional impact of cirrhosis on individual’s lives is rarely considered in clinical practice[7].
HRQL is defined as the impact on three health domains regarding the patient’s perception of their wellbeing: Physical, psychological, and social health. Measurement of HRQL requires administration of self-reported questionnaires[8,9].
The Chronic Liver Disease Questionnaire (CLDQ) assesses HRQL in patients with chronic liver disease across diagnoses, at all stages of disease and treatment. The CLDQ is a 29-item self-reported questionnaire, with patient response options extending from 1 to 7 (all to none of the time). The CLDQ addresses the following domains that when combined give a composite score that indicates overall HRQL: Fatigue, activity, emotional function, abdominal pain, systemic symptoms, and anxiety. Mean domain scores and an overall quality of life score can be calculated, with higher scores representing better outcome[9,10]. Previous studies have confirmed how HRQL deteriorates from compensated to decompensated cirrhosis[11].
Our aim in this study was to verify how malnutrition is related to HRQL impairment in patients with cirrhosis.
We designed an observational analytic study. Data were retrospectively abstracted from medical records and obtained by direct interview. All study participants provided verbal informed consent prior to study enrollment.
We included patients with cirrhosis from any etiology, who were evaluated at the Liver Clinic from Gastroenterology Department in a tertiary healthcare center, from June 2014 to June 2016. The Child-Pugh score was used to define compensated cirrhosis (Child-Pugh A) and decompensated cirrhosis (Child-Pugh B/C). We also collected data about complications of cirrhosis, including: Ascites, need of paracentesis, variceal bleeding, hepatic encephalopathy, and bacterial infection needing hospitalization. Patients with other chronic comorbidities, such as diabetes, chronic renal failure, heart or lung disease, neoplasms and acquired immunodeficiency syndrome, were excluded. We collected demographic, clinical and anthropometric characteristics of patients.
Weight, height, mid-arm circumference and triceps skinfold thickness were measured[12]. Body mass index (BMI) and ideal mid-arm muscle circumference were also calculated[13,14].
Nutritional status was evaluated by the Subjective Global Assessment (SGA)[4,5,15]. Patients were catalogued as well nourished, or moderately or severely malnourished. We chose the SGA for this study because of its being a simple bedside method recommended by the experts when other more accurate methods, such as phase angle or body cell mass measured by bioelectric impedance analysis, are not available to assess nutritional status.
HRQL was evaluated through the CLDQ[10]. In addition, patients were requested to assess their global HRQL with the following coding system: 0 = impairment of HRQL, when it was compared with other healthy subjects; 1 = good HRQL, if it was similar to the quality of life of other healthy subjects.
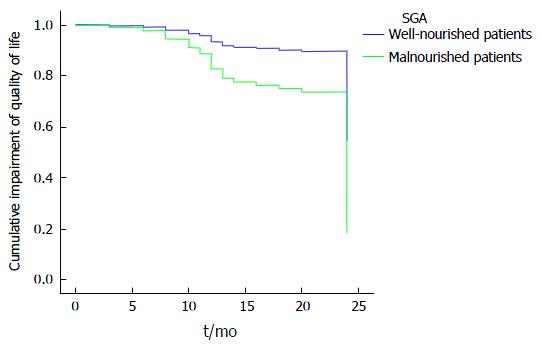
Numeric variables were stated as mean and standard deviation (SD); categorical variables were stated as proportions and percentages. To compare the primary outcome between malnourished and well-nourished groups, the χ2 test, Fisher’s exact test or Student’s t-test were used, as appropriate. Associations between predictor variables and deterioration of quality of life were determined by calculating the hazard ratio (HR) and 95% confidence interval (CI) using Cox proportional hazards regression. The significant variables (P < 0.05) in the univariate model were included in the multivariate model. Kaplan-Meier curves were constructed to compare quality of life between well-nourished and malnourished patients, and for this purpose, we identified the time when patients were diagnosed with cirrhosis and the estimated time when patients noticed impairment of their quality of life. Statistical significance was considered as a P-value < 0.05.
A total of 127 patients with cirrhosis were included, 70 of which were female (55.1%) and 57 were male (44.9%); the mean age was 54.1 ± 12.3 years-old. Regarding the etiology of the cirrhosis, 68 patients (53.3%) had alcoholic cirrhosis, 23 (18.1%) had chronic hepatitis C, 21 (16.5%) had cryptogenic etiology, 11 (8.7%) had autoimmune hepatitis, 3 (2.4%) had non-alcoholic steatohepatitis, and 1 (0.8%) had chronic hepatitis B. According to Child-Pugh scoring, 25 patients (19.7%) were classified as A (compensated), 76 (59.8%) as B, and 26 (20.5%) as C (B/C = decompensated). As determined by the SGA, 58 patients (45.7%) were well-nourished and 69 (54.3%) had some degree of malnutrition, including 66 (52%) with mild to moderate malnutrition and 3 (2.3%) with severe malnutrition. A total of 51 patients (40.2%) assessed their HRQL as good quality of life or similar to other healthy subjects; on the other hand, 76 patients (59.8%) perceived impairment of their HRQL in comparison with other healthy subjects. Characteristics of patients according to their self-perception of HRQL are shown and compared in Table 1. In the univariate analysis, decompensated cirrhosis, presence of ascites, need for paracentesis, hospitalization for any cause, and malnutrition were factors significantly associated with poor HRQL.
| Characteristic | Good quality of life (n = 51) | Impairment of quality of life (n = 76) | P |
| Male | 24 (47.1) | 33 (43.4) | 0.69 |
| Age (yr) | 54.8 ± 10.3 | 53.7 ± 13.5 | 0.61 |
| Decompensated or Child B/C | 30 (58.8) | 63 (82.9) | 0.003 |
| Etiology | |||
| Alcohol | 28 (55.0) | 40 (52.7) | 0.83 |
| Viral | 9 (17.6) | 15 (19.7) | |
| NASH | 2 (3.9) | 1 (1.3) | |
| Cryptogenic | 8 (15.7) | 13 (17.1) | |
| Autoimmune | 4 (7.8) | 7 (9.2) | |
| Weight in kg | 65.2 ± 14.9 | 63.7 ± 13.4 | 0.55 |
| Body mass index (kg/m2) | 26.6 ± 5.2 | 26.8 ± 4.0 | 0.32 |
| Triceps skinfold thickness (cm) | 1.4 ± 0.7 | 1.4 ± 0.8 | 0.79 |
| Mid-arm circumference (cm) | 26.4 ± 4.7 | 23.9 ± 3.7 | 0.001 |
| Ideal mid-arm muscle circumference (cm) | 22.1 ± 4.1 | 19.6 ± 2.8 | < 0.0001 |
| Malnourished according to SGA | 14 (27.5) | 55 (72.4) | < 0.0001 |
| Presence of ascites | 19 (37.3) | 48 (63.2) | 0.004 |
| Need for paracentesis | 7 (13.7) | 25 (32.9) | 0.02 |
| Development of variceal bleeding | 12 (23.5) | 18 (23.7) | 0.98 |
| Development of hepatic encephalopathy | 19 (37.3) | 30 (39.5) | 0.80 |
| Bacterial infection requiring hospitalization | 6 (11.8) | 14 (18.4) | 0.45 |
| Any complication requiring hospitalization | 32 (62.7) | 62 (81.6) | 0.02 |
Multivariate analysis to determine associations between predictor variables and self-perception of an impairment of HRQL is shown in Table 2. The most important factor related to poor HRQL was malnutrition (P < 0.0001). Also, patients with malnutrition had poorer HRQL through the time course of their chronic liver disease, when compared with the well-nourished patients (P < 0.0001) (Figure 1).
| Characteristic | HR (95%CI) | P |
| Malnourished according to SGA | 2.8 (1.6-5.0) | < 0.0001 |
| Need for paracentesis | 1.8 (1.0-3.2) | 0.05 |
| Presence of ascites | 1.4 (0.7-2.7) | 0.38 |
| Any complication requiring hospitalization | 1.1 (0.5-2.6) | 0.82 |
| Decompensated or Child B/C | 1.8 (0.0-4.0) | 0.14 |
Finally, the comparison of characteristics evaluated through CLDQ between malnourished and well-nourished patients is shown in Table 3. The most important impaired characteristics in malnourished patients were: Presence of body pain, dyspnea on exertion with daily activities, decreased appetite, generalized weakness, trouble lifting or carrying heavy objects, and decreased level of energy (P < 0.0001).
| CLDQ item | Well-nourished (n = 58) | Malnourished (n = 69) | P |
| 1 How much of the time during the last 2 wk have you been troubled by a feeling of abdominal bloating? | 5.72 ± 1.531 | 4.67 ± 2.056 | 0.001 |
| 2 How much of the time have you been tired or fatigued during the last 2 wk? | 3.69 ± 1.366 | 2.94 ± 1.259 | 0.002 |
| 3 How much of the time during the last 2 wk have you experienced body pain? | 4.14 ± 0.868 | 3.57 ± 0.848 | 0.0001 |
| 4 How often during the last 2 wk have you felt sleepy during the day? | 5.05 ± 1.343 | 4.55 ± 1.105 | 0.02 |
| 5 How much of the time during the last 2 wk have you experienced abdominal pain? | 5.45 ± 1.273 | 4.96 ± 1.529 | 0.05 |
| 6 How much of the time during the last 2 wk have you experienced dyspnea on exertion, being a problem for you in your daily activities? | 6.16 ± 0.951 | 5.33 ± 1.431 | 0.0001 |
| 7 How much of the time during the last 2 wk have you not been able to eat as much as you would like? | 6.12 ± 1.010 | 3.55 ± 1.549 | 0.0001 |
| 8 How much of the time in the last 2 wk have you been bothered by having decreased strength? | 4.91 ± 1.218 | 2.90 ± 1.447 | 0.0001 |
| 9 How often during the last 2 wk have you had trouble lifting or carrying heavy objects? | 5.62 ± 0.834 | 4.09 ± 1.391 | 0.0001 |
| 10 How often during the last 2 wk have you felt anxious? | 5.52 ± 1.112 | 5.33 ± 1.379 | 0.41 |
| 11 How often during the last 2 wk have you felt a decreased level of energy? | 5.19 +1.100 | 3.20 ± 1.491 | 0.0001 |
| 12 How much of the time during the last 2 wk have you felt unhappy? | 5.12 ± 1.077 | 4.41 ± 1.527 | 0.003 |
| 13 How often during the last 2 wk have you felt drowsy? | 4.97 ± 1.324 | 4.55 ± 1.051 | 0.05 |
| 14 How much of the time during the last 2 wk have you been bothered by a limitation of your diet? | 4.14 ± 1.206 | 3.91 ± 1.160 | 0.29 |
| 15 How often during the last 2 wk have you been irritable? | 5.52 ± 1.128 | 5.36 ± 1.175 | 0.45 |
| 16 How much of the time during the last 2 wk have you had difficulty sleeping at night? | 5.02 ± 1.493 | 4.87 ± 1.444 | 0.57 |
| 17 How much of the time during the last 2 wk have you been troubled by a feeling of abdominal discomfort? | 5.62 ± 1.437 | 4.77 ± 1.816 | 0.004 |
| 18 How much of the time during the last 2 wk have you been worried about the impact your liver disease has on your family? | 5.84 ± 1.056 | 5.94 ± 1.371 | 0.66 |
| 19 How much of the time during the last 2 wk have you had mood swings? | 5.50 ± 1.417 | 5.83 ± 1.283 | 0.18 |
| 20 How much of the time during the last 2 wk have you been unable to fall asleep at night? | 5.10 ± 1.360 | 4.67 ± 1.569 | 0.99 |
| 21 How often during the last 2 wk have you had muscle cramps? | 5.52 ± 1.047 | 5.39 ± 1.074 | 0.51 |
| 22 How much of the time during the last 2 wk have you been worried that your symptoms will develop into major problems? | 4.19 + 1.515 | 4.45 ± 1.586 | 0.35 |
| 23 How much of the time during the last 2 wk have you had a dry mouth? | 5.40 ± 1.184 | 5.30 ± 1.192 | 0.66 |
| 24 How much of the time during the last 2 wk have you felt depressed? | 5.33 ± 1.082 | 4.68 ± 1.745 | 0.01 |
| 25 How much of the time during the last 2 wk have you been worried about your condition getting worse? | 4.05 ± 1.191 | 4.28 ± 1.454 | 0.34 |
| 26 How much of the time during the last 2 wk have you had problems concentrating? | 5.34 ± 1.132 | 4.74 ± 1.569 | 0.01 |
| 27 How much of the time have you been troubled by itching during the last 2 wk? | 5.71 ± 1.451 | 6.20 ± 1.065 | 0.03 |
| 28 How much of the time during the last 2 wk have you been worried about never feeling any better? | 4.07 ± 1.153 | 4.36 ± 1.382 | 0.20 |
| 29 How much of the time during the last 2 wk have you been concerned about the availability of a liver if you need a liver transplant? | 4.22 ± 1.312 | 4.23 ± 1.467 | 0.97 |
Cirrhosis represents the final stage of all chronic liver diseases. In its decompensated form, cirrhosis can result in portal hypertension and hepatic dysfunction. Cirrhosis is a leading cause of morbidity and mortality worldwide, and not only is related to decreased survival but also to poor HRQL[16].
Quality of life is a concept that reflects the positive and negative aspects of an individual’s life. The term “HRQL” specifically addresses the impact of health on patients’ wellbeing[9]. There are many factors that influence outcome and HRQL in patients with cirrhosis, however liver function clearly plays a major role affecting the HRQL of patients with cirrhosis. Patients with decompensated cirrhosis have an important impairment on HRQL[17]. Also, many symptoms can negatively impact HRQL in patients with cirrhosis; these symptoms can include abdominal bloating, nausea, somnolence, weight loss, weakness, fatigue and itching. All of these may interfere with patient’s work, schooling, social activities, and sense of wellbeing[18].
In our study, we found that decompensated cirrhosis (Child B/C) is a factor related to impairment of HRQL; this finding is similar to other studies. Marchesini et al[19] also reported that the severity of liver disease or the development of complications were conditions clearly related to deterioration of perception of health. Similarly, we found that the presence of ascites and need for paracentesis were associated factors related to poor quality of life. Furthermore, hospitalization for any cause was a condition related to poor HRQL in patients with cirrhosis.
In our study, interestingly we found that patients with cirrhosis and malnutrition had a poorer HRQL when compared with well-nourished patients with cirrhosis. Furthermore, malnutrition was the main factor contributing to impairment of HRQL in these patients. Cirrhosis is also associated with malnutrition, which is a complication that negatively affects cirrhotic patients, particularly those decompensated[20-23]. In patients with cirrhosis, the prevalence of malnutrition has been reported between 20% to 60%[24-27]. In a previous study conducted by Pérez-Reyes et al[4] in a Hispanic population, the prevalence of malnutrition was as high as 56.3%. In the present study, we also found a high frequency of malnutrition in patients with cirrhosis (54.3%). Malnutrition in cirrhosis is related to development of ascites, encephalopathy, spontaneous bacterial peritonitis, other bacterial infections and hepatorenal syndrome[4,28-32]. But also, malnutrition deteriorates the HRQL in patients with cirrhosis[33-35] and several other gastrointestinal and non-gastrointestinal diseases[36,37]. Our study confirms that malnutrition is a key factor related to impairment of HRQL in patients with cirrhosis, even when we adjusted for advanced liver disease or decompensation status, and for other major complications such as ascites, need for paracentesis and need for hospitalization for any cause.
In conclusion, cirrhosis is the end-stage of all chronic liver diseases; it contributes importantly to morbidity and mortality worldwide but also has a negative impact on HRQL that must be considered. Several factors contribute to a poor HRQL in patients with cirrhosis, however malnutrition, which is a highly prevalent comorbidity in patients with cirrhosis, represents a key factor related to poor HRQL in these patients. There is a need for developing strategies to evaluate more accurately patients with cirrhosis and to identify promptly those patients at risk of malnutrition.
Cirrhosis is a significant contributor to global mortality. Prevalence of malnutrition is high in patients with cirrhosis and is related to increased complications or even death. Despite increased knowledge of the pathogenesis of cirrhosis, there remains a paucity of information related to health-related quality of life (HRQL) in these patients.
The emotional impact of cirrhosis on individual’s lives is rarely considered in clinical practice. The Chronic Liver Disease Questionnaire assesses HRQL in patients with chronic liver disease across diagnoses, at all stages of disease and treatment.
Cirrhosis is a leading cause of morbidity and mortality worldwide, and not only is related to decreased survival but also to poor quality of life. The term “HRQL”addresses the impact of health on a patient’s wellbeing. Many factors influence HRQL in patients with cirrhosis, however the impact of comorbidities, such as malnutrition, are not well understood. The authors found that patients with cirrhosis and malnutrition had worse quality of life when compared with well-nourished patients with cirrhosis. In this study, malnutrition was the main factor contributing to impairment of quality of life in these patients.
In this study, the authors found that several factors contribute to a poor health-related quality of life in patients with cirrhosis, however malnutrition, which is a highly prevalent comorbidity in these patients, represents a key factor related to poor quality of life in these patients. There is a need for developing strategies to evaluate more accurately patients with cirrhosis and to identify promptly those patients at risk of malnutrition.
Nutritional status was defined through the Subjective Global Assessment and patients were divided as follows: Well-nourished, or moderately or severely malnourished. The HRQL is defined as the impact on three health domains-physical, psychological, and social health-on patient perception of their wellbeing.
Very nice and well written paper.
| 1. | Tucker ME. Global burden of liver disease substantial. Available from: http://www.medscape.com/viewarticle/813788#1. |
| 2. | Fleming KM, Aithal GP, Card TR, West J. All-cause mortality in people with cirrhosis compared with the general population: a population-based cohort study. Liver Int. 2012;32:79-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Maharshi S, Sharma BC, Srivastava S. Malnutrition in cirrhosis increases morbidity and mortality. J Gastroenterol Hepatol. 2015;30:1507-1513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 116] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 4. | Pérez-Reyes E, Rivera-Sánchez J, Servín-Caamaño AI, Pérez-Torres E, Abdo-Francis JM, Higuera-de la Tijera F. Malnutrition is related to a higher frequency of serious complications in patients with cirrosis. Rev Med Hosp Gen Méx. 2016;79:11-16. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Landa-Galván HV, Milke-García MP, León-Oviedo C, Gutiérrez-Reyes G, Higuera-de la Tijera F, Pérez-Hernández JL, Serralde-Zúñiga AE. [Nutritional assessment of alcoholic liver cirrhotic patients treated in the liver Clinic of the Mexico’s General Hospital]. Nutr Hosp. 2012;27:2006-2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 6. | Davis GL, Albright JE, Cook SF, Rosenberg DM. Projecting future complications of chronic hepatitis C in the United States. Liver Transpl. 2003;9:331-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 442] [Cited by in RCA: 404] [Article Influence: 17.6] [Reference Citation Analysis (1)] |
| 7. | Anthony PP, Ishak KG, Nayak NC, Poulsen HE, Scheuer PJ, Sobin LH. The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health Organization. J Clin Pathol. 1978;31:395-414. [PubMed] |
| 8. | Les I, Doval E, Flavià M, Jacas C, Cárdenas G, Esteban R, Guardia J, Córdoba J. Quality of life in cirrhosis is related to potentially treatable factors. Eur J Gastroenterol Hepatol. 2010;22:221-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 9. | Loria A, Escheik C, Gerber NL, Younossi ZM. Quality of life in cirrhosis. Curr Gastroenterol Rep. 2013;15:301. [PubMed] |
| 10. | Younossi ZM, Guyatt G, Kiwi M, Boparai N, King D. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut. 1999;45:295-300. [PubMed] |
| 11. | Younossi ZM, Boparai N, McCormick M, Price LL, Guyatt G. Assessment of utilities and health-related quality of life in patients with chronic liver disease. Am J Gastroenterol. 2001;96:579-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 116] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL: Human Kinetic Books; 1988; . |
| 13. | Ratib S, Fleming KM, Crooks CJ, Walker AJ, West J. Causes of death in people with liver cirrhosis in England compared with the general population: a population-based cohort study. Am J Gastroenterol. 2015;110:1149-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 14. | Frisancho AR. New norms of upper limb fat and muscle areas for assessment of nutritional status. Am J Clin Nutr. 1981;34:2540-2545. [PubMed] |
| 15. | Morgan MY, Madden AM, Soulsby CT, Morris RW. Derivation and validation of a new global method for assessing nutritional status in patients with cirrhosis. Hepatology. 2006;44:823-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 122] [Article Influence: 6.1] [Reference Citation Analysis (1)] |
| 16. | Nusrat S, Khan MS, Fazili J, Madhoun MF. Cirrhosis and its complications: evidence based treatment. World J Gastroenterol. 2014;20:5442-5460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 128] [Cited by in RCA: 163] [Article Influence: 13.6] [Reference Citation Analysis (8)] |
| 17. | Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician. 2006;74:756-762. [PubMed] |
| 18. | Grattagliano I, Ubaldi E, Bonfrate L, Portincasa P. Management of liver cirrhosis between primary care and specialists. World J Gastroenterol. 2011;17:2273-2282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 36] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 19. | Marchesini G, Bianchi G, Amodio P, Salerno F, Merli M, Panella C, Loguercio C, Apolone G, Niero M, Abbiati R; The Italian Study Group for Quality of Life in Cirrhosis. Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology. 2001;120:170-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 363] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 20. | Tessari P. Protein metabolism in liver cirrhosis: from albumin to muscle myofibrils. Curr Opin Clin Nutr Metab Care. 2003;6:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 21. | Bianchi G, Marzocchi R, Agostini F, Marchesini G. Update on nutritional supplementation with branched-chain amino acids. Curr Opin Clin Nutr Metab Care. 2005;8:83-87. [PubMed] |
| 22. | Bilbao I, Armadans L, Lazaro JL, Hidalgo E, Castells L, Margarit C. Predictive factors for early mortality following liver transplantation. Clin Transplant. 2003;17:401-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Alvares-da-Silva MR, Reverbel da Silveira T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. 2005;21:113-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 324] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 24. | Peng S, Plank LD, McCall JL, Gillanders LK, McIlroy K, Gane EJ. Body composition, muscle function, and energy expenditure in patients with liver cirrhosis: a comprehensive study. Am J Clin Nutr. 2007;85:1257-1266. [PubMed] |
| 25. | Alberino F, Gatta A, Amodio P, Merkel C, Di Pascoli L, Boffo G, Caregaro L. Nutrition and survival in patients with liver cirrhosis. Nutrition. 2001;17:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 344] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 26. | Campillo B, Richardet JP, Bories PN. Enteral nutrition in severely malnourished and anorectic cirrhotic patients in clinical practice. Gastroenterol Clin Biol. 2005;29:645-651. [PubMed] |
| 27. | Plauth M, Schütz ET. Cachexia in liver cirrhosis. Int J Cardiol. 2002;85:83-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Kalaitzakis E, Simrén M, Olsson R, Henfridsson P, Hugosson I, Bengtsson M, Björnsson E. Gastrointestinal symptoms in patients with liver cirrhosis: associations with nutritional status and health-related quality of life. Scand J Gastroenterol. 2006;41:1464-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 29. | Kalaitzakis E, Olsson R, Henfridsson P, Hugosson I, Bengtsson M, Jalan R, Björnsson E. Malnutrition and diabetes mellitus are related to hepatic encephalopathy in patients with liver cirrhosis. Liver Int. 2007;27:1194-1201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 30. | Huisman EJ, Trip EJ, Siersema PD, van Hoek B, van Erpecum KJ. Protein energy malnutrition predicts complications in liver cirrhosis. Eur J Gastroenterol Hepatol. 2011;23:982-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 149] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 31. | Merli M, Lucidi C, Giannelli V, Giusto M, Riggio O, Falcone M, Ridola L, Attili AF, Venditti M. Cirrhotic patients are at risk for health care-associated bacterial infections. Clin Gastroenterol Hepatol. 2010;8:979-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 233] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 32. | Merli M, Giusto M, Gentili F, Novelli G, Ferretti G, Riggio O, Corradini SG, Siciliano M, Farcomeni A, Attili AF. Nutritional status: its influence on the outcome of patients undergoing liver transplantation. Liver Int. 2010;30:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 212] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 33. | Poupon RE, Chrétien Y, Chazouillères O, Poupon R, Chwalow J. Quality of life in patients with primary biliary cirrhosis. Hepatology. 2004;40:489-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 95] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 34. | Kalaitzakis E. Gastrointestinal dysfunction in liver cirrhosis. World J Gastroenterol. 2014;20:14686-14695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 72] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 35. | Shiraki M, Nishiguchi S, Saito M, Fukuzawa Y, Mizuta T, Kaibori M, Hanai T, Nishimura K, Shimizu M, Tsurumi H. Nutritional status and quality of life in current patients with liver cirrhosis as assessed in 2007–2011. Hepatol Res. 2013;46:106-112. [RCA] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 36. | Norman K, Kirchner H, Lochs H, Pirlich M. Malnutrition affects quality of life in gastroenterology patients. World J Gastroenterol. 2006;12:3380-3385. [PubMed] [DOI] [Full Text] |
| 37. | Noman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nut. 2008;27:5-15. [RCA] [DOI] [Full Text] [Cited by in Crossref: 827] [Cited by in RCA: 973] [Article Influence: 54.1] [Reference Citation Analysis (0)] |
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Mexico
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C, C
Grade D (Fair): D
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Ali A, Dina I, El-Karaksy HM, Facciorusso A, Gallo P, Sharma V S- Editor: Song XX L- Editor: Filipodia E- Editor: Li D