Published online Dec 8, 2016. doi: 10.4254/wjh.v8.i34.1535
Peer-review started: June 24, 2016
First decision: August 11, 2016
Revised: September 11, 2016
Accepted: October 25, 2016
Article in press: October 27, 2016
Published online: December 8, 2016
Processing time: 168 Days and 9 Hours
Right umbilical portion (RUP) is a rare congenital anomaly associated with anomalous ramifications of the hepatic vessels and biliary system. As such, major hepatectomy requires a careful approach. We describe the usefulness of the Glissonean approach in two patients with vessel anomalies, such as RUP. The first patient underwent a right anterior sectionectomy for intrahepatic cholangiocarcinoma. We encircled several Glissonean pedicles that entered the right anterior section along the right side of the RUP. We temporarily clamped each pedicle, confirmed the demarcation area, and finally cut them. The operation was performed safely and was successful. The second patient underwent a left trisectionectomy for perihilar cholangiocarcinoma. We secured the right posterior Glissonean pedicle. The vessels in the pedicle were preserved, and the other vessels and contents were resected. Identifying the vessels for preservation facilitated the safe lymphadenectomy and dissection of the vessels to be resected. We successfully performed the operation.
Core tip: Right umbilical portion (RUP) is a rare congenital anomaly, and its presence is associated with anomalous ramifications of the hepatic artery, portal vein, and biliary system. Major Hepatectomies for patients with this anomaly are complicated and require a careful approach. The Glissonean approach is acknowledged as a successful technique. The targeted Glissonean pedicle to be resected or preserved is easily identified by clamping; thus, the Glissonean approach can be used in various situations of hepatic resection. This report describes the usefulness of the Glissonean technique, especially in cases with an anomaly, such as RUP.
- Citation: Ome Y, Kawamoto K, Park TB, Ito T. Major hepatectomy using the glissonean approach in cases of right umbilical portion. World J Hepatol 2016; 8(34): 1535-1540
- URL: https://www.wjgnet.com/1948-5182/full/v8/i34/1535.htm
- DOI: https://dx.doi.org/10.4254/wjh.v8.i34.1535
Right umbilical portion (RUP) is a rare congenital anomaly, and its reported incidence ranges from 0.2% to 1.2%[1-6]. The presence of RUP is associated with anomalous ramifications of the hepatic artery, portal vein, and biliary system. During anatomical liver resection, only the vessels feeding the area intended for resection should be resected, whereas the other vessels should be preserved. Consequently, major hepatectomies for cases with RUP are complicated and require a careful approach and attention to the anomalous branching of those vessels. Only a few hepatectomy cases with RUP have been reported in the English literature. Here, we report two successful cases with RUP who safely underwent anatomical hepatectomy. We also describe the usefulness of the Glissonean approach.
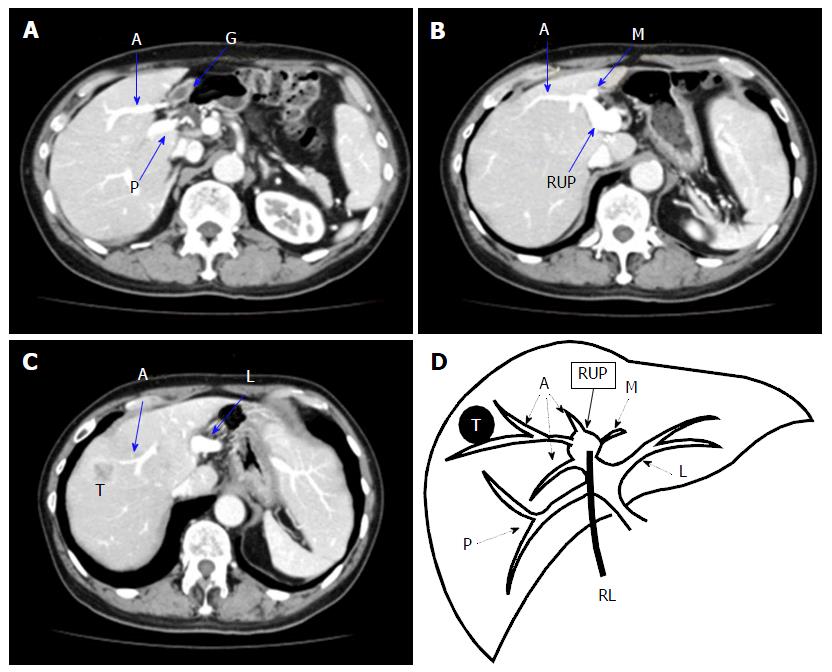
A 70-year-old man with hepatitis C presented with a liver tumour. He had a past medical history of distal gas–trectomy for gastric ulcer, Graves’ disease, and diabetes mellitus. Laboratory tests showed normal levels of carcino embryonic antigen (CEA), CA19-9 and alpha-fetoprotein (AFP) but elevated PIVKA-II at 808 mAU/mL. The indocyanine green retention rate at 15 min was 12.9% and the Child-Pugh score was 5 points, Grade A. He was diagnosed with intrahepatic cholangiocarcinoma or combined hepatocellular and cholangiocarcinoma located in segment 8. A computed tomography (CT) scan also revealed that his gallbladder was attached to the left side of the liver; RUP was noted (Figure 1).
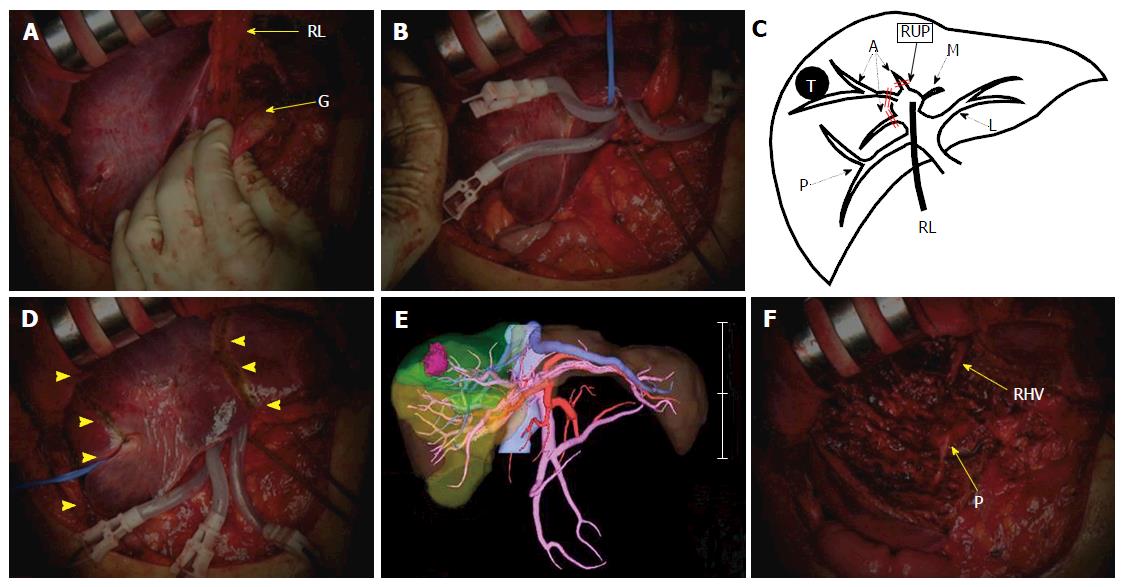
The patient underwent right anterior sectionectomy (Figure 2). Laparotomy showed that the gallbladder was attached to the round ligament. After the mobilization of the right lobe, the gallbladder was resected. Then, the right anterior Glissonean pedicles, which ramified along the right side of the RUP, were extrahepatically separated and encircled with tape. We temporarily clamped each pedicle and confirmed the demarcation area and blood flow via ultrasonography. The demarcation area was the same as the three-dimensional image visualization via preoperative simulation. The liver parenchyma was transected along the demarcation line using the Pringle manoeuvre. We finally ligated and cut the encircled right anterior Glissonean pedicles. The operation succeeded without injuring any of the vessels intended for preservation. The operation required 244 min, and the estimated blood loss was 776 mL.
Macroscopic findings showed an irregular mass, 25 mm in size. A histological examination revealed that the tumour was a poorly differentiated intrahepatic cholangiocarcinoma that invaded the intrahepatic portal vein. The patient was diagnosed as stage II (T2N0M0). All of the surgical margins were negative. He recovered uneventfully and was discharged on postoperative day 6.
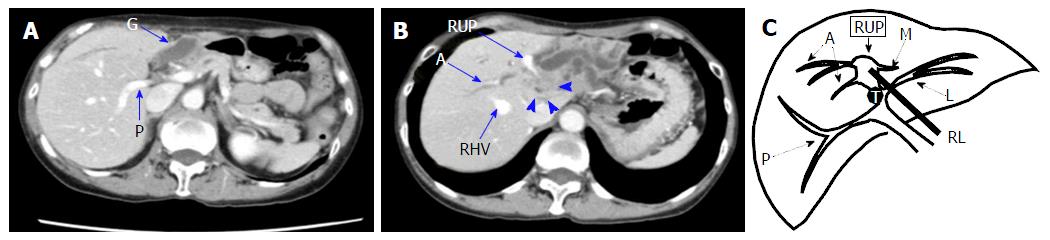
A 70-year-old woman presented with general fatigue and intrahepatic bile duct dilatation. Tumour markers, such as AFP, PIVKA-II and CEA, were normal, but CA19-9 was elevated at 843.6 U/mL. Other laboratory tests showed elevated ALP at 601 IU/L, elevated γ-GTP at 318 IU/L, and impaired serum albumin at 3.3 g/dL. Bilirubin was normal. The indocyanine green retention rate at 15 min was 4.6% and the Child-Pugh score was 6 points, Grade A. She was diagnosed with perihilar cholangiocarcinoma and RUP via ultrasound, CT and magnetic resonance cholangiopancreatography (Figure 3). The tumour involved the confluence of the left lateral, left medial, and right anterior hepatic ducts; the right posterior branch was intact.
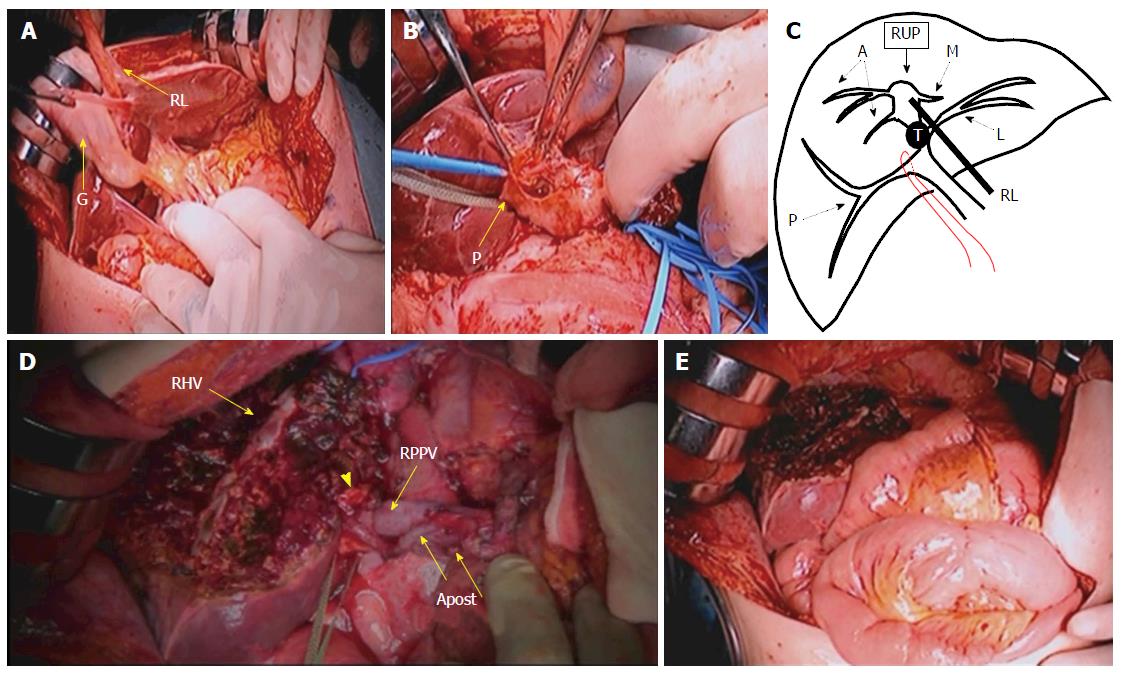
The patient underwent left trisectionectomy with extrahepatic bile duct resection (Figure 4). First, Kocher’s manoeuvre and lymphadenectomy around the pancreas head were performed. The distal common bile duct was transected at the level of the pancreas. Then, we performed lymphadenectomy in the hepatoduodenal ligament. The gallbladder was dissected and we secured and encircled the right lateral Glissonean pedicle with tape. The portal vein, the hepatic artery, and the hilar plate were separated from the other structures just proximal to the secured Glissonean pedicle. The vessels entering the pedicle were preserved and the other vessels and contents were resected. In the preoperative simulation, only one right posterior branch of the hepatic artery was identified. During the operation, however, two arteries were found entering the right posterior section. We preserved the vessels that nourished the right posterior section and resected the root of the left hepatic artery, the right anterior hepatic artery, and the common trunk of the left lateral portal vein and RUP; Next, the demarcation area was confirmed. The left side of the liver was fully mobilized, and the liver parenchyma was transected along the demarcation line; Finally, we cut the right posterior hepatic duct, and the specimen was removed. Hepaticojejunostomy to the right posterior bile duct and jejunojejunostomy were conducted, and the operation was successfully completed. The operative time was 697 min, and the estimated blood loss was 716 mL.
A histological examination showed moderately differentiated cholangiocarcinoma, 30 mm in size that was invading the hepatic duct and the portal vein. Two lymph node metastases were revealed. The patient was diagnosed as stage IIB (T3N1M0). All of the surgical margins were negative. The postoperative course was uneventful and this patient was discharged on postoperative day 13.
RUP, previously known as a left-sided gallbladder, is a rare congenital anomaly. However, we occasionally encounter it in our daily medical procedures (e.g., cholecystectomy). RUP is an anatomical anomaly in which the umbilical portion exists between the right anterior and left medial section. The right-sided round ligament adheres to the RUP. Other theories exist regarding liver segmentation with RUP. One is that segment 4 is absent[5]. Another is that the right side of the RUP is comparable with the dorsal segment of the right anterior section and the left side of the RUP with the ventral segment of the right anterior section[7]. In this report, we defined RUP as the umbilical portion that exists between the right anterior and left medial section. Nagai et al[1] reviewed the literature concerning this anomaly and classified the type of portal branching according to bifurcation type and trifurcation type. Nineteen cases with RUP have undergone hepatectomy in the English-language literature[1,3,6,8-15] (Table 1). RUP is associated with anomalous ramifications of the hepatic artery, portal vein, and biliary system; thus, surgery for cases with RUP requires careful procedures, especially with regard to hepatic resection. Previous reports described the importance of the thorough preoperative and intraoperative recognition of the various anomalies associated with RUP to prevent operative accidents.
| Ref. | Age (yr) | Sex | Disease | Surgical procedure | Type of intrahepatic portal venous branching |
| Uesaka et al[8] | 53 | Male | Liver metastasis of bile duct cancer | Right hepatectomy | Trifurcation type |
| Idu et al[9] | Unknown | Male | Perihilar cholangiocarcinoma | Left hepatectomy | Unknown |
| Nagai et al[1] | 67 | Male | Bile duct cancer | Right anterior sectionectomy, segmentectomy 1 and pancreatoduodenectomy | Trifurcation type |
| Nagai et al[1] | 67 | Male | Hepatocellular carcinoma | Segmentectomy 8, and partial resection of segment 1 | Trifurcation type |
| Asonuma et al[3] | 48 | Male | Living donor | Left lateral sectionectomy | Unknown |
| Asonuma et al[3] | 29 | Male | Living donor | Left lateral sectionectomy | Unknown |
| Asonuma et al[3] | 35 | Female | Living donor | Left lateral sectionectomy | Bifurcation type |
| Kaneoka et al[10] | 53 | Male | Perihilar cholangiocellular carcinoma | Left hepatectomy and segmentectomy 1 with extrahepatic bile duct resection | Trifurcation type |
| Kaneoka et al[10] | 61 | Male | Extrahepatic bile duct cholangiocarcinoma | Left hepatectomy, segmentectomy 1, and pylorous-preserving pancreaticduodenectomy | Trifurcation type |
| Tashiro et al[11] | 53 | Male | Hepatocellular carcinoma | Partial hepatectomy | Trifurcation type |
| Hwang et al[12] | 18 | Male | Living donor | Right hepatectomy | Bifurcation type |
| Hwang et al[12] | 24 | Unknown | Living donor | Right posterior sectionectomy | Trifurcation type |
| Hwang et al[12] | 39 | Unknown | Living donor | Left hepatectomy leaving S4a | Bifurcation type |
| Hsu et al[6] | Unknown | Unknown | Hepatocellular carcinoma | Right hepatectomy | Trifurcation type |
| Hsu et al[6] | Unknown | Unknown | Hepatocellular carcinoma | Partial resection of left lateral section | Trifurcation type |
| Hsu et al[6] | Unknown | Unknown | Hepatocellular carcinoma | Left lateral sectionectomy | Bifurcation type |
| Abe et al[13] | 70 | Female | Liver metastasis of uterine cervical cancer | Right hepatectomy with extrahepatic bile duct resection | Bifurcation type |
| Sakaguchi et al[14] | 76 | Male | Liver metastasis of rectal cancer | Right posterior sectionectomy and partial resection of segment 1 and right anterior section | Trifurcation type |
| Almodhaiberi et al[15] | 67 | Male | Perihilar cholangiocarcinoma | Extended left lateral sectionectomy and segmentectomy 1 with extrahepatic bile duct resection | Trifurcation type |
| Case 1 | 70 | Male | Intrahepatic cholangiocarcinoma | Right anterior sectionectomy | Trifurcation type |
| Case 2 | 70 | Female | Perihilar cholangiocarcinoma | Left trisectionectomy with extrahepatic bile duct resection | Trifurcation type |
CT and three-dimensional imaging have been developed, and preoperative simulation is of great help. We must preoperatively evaluate and recognize the anatomy precisely in cases with this anomaly. However, some vessels go unrecognized during the preoperative survey but can be encountered during the procedure, as was observed in case 2. Thus, paying special attention during the operation is important.
The Glissonean approach is acknowledged as a potentially successful technique for liver surgery, and it is widely performed for liver resection. The ramification pattern of the hepatic artery, portal vein and bile duct in the hepatoduodenal ligament often varies across patients. However, the Glissonean pedicle peripheral to the hilar plate, which is wrapped by connective tissue and contains the hepatic artery, portal vein, and bile duct, enters its proper area and never contains branches that nourish other areas. Consequently, the Glissonean pedicle transection peripheral to the extrahepatic hilar plate is a safe and sure method that enables the cutting of the intended vessels without damaging the vessels to be preserved. Secondary and tertiary branches of the Glissonian pedicle peripheral to the hilar plate can usually be approached and transected extrahepatically. When the targeted Glissonean pedicle is transiently and selectively clamped, we can recognize the area to be resected. Surgeons do not have to consider any variations in the hepatoduodenal ligament. The Glissonean approach is a successful method, especially in cases with anomalous ramifications of the hepatic artery, portal vein and biliary system. The Glissonean pedicle to be resected was separated in case 1, whereas that to be preserved was encircled in case 2. The Glissonean approach can be used in various situations of hepatic resection and it contributes to a safe and secure liver surgery.
In conclusion, we successfully performed two major hepatectomies using the Glissonean approach in cases with RUP. The Glissonean approach is a useful method and contributes to a safe procedure for cases with an anomalous anatomy such as RUP.
A 70-year-old man with hepatitis C presented with a liver tumour without any symptoms; a 70-year-old woman presented with general fatigue and intrahepatic bile duct dilatation.
Intrahepatic cholangiocarcinoma or combined hepatocellular and cholangiocarcinoma of the right umbilical portion (RUP); perihilar cholangiocarcinoma of the RUP.
Metastatic liver tumour; intrahepatic cholangiocarcinoma and inflammatory biliary stenosis.
The level of tumour marker PIVKA-II was elevated at 808 mAU/mL; other tumour markers were normal; the level of tumour marker CA19-9 was elevated at 843.6 U/mL; other tumour markers were normal.
A computed tomography (CT) scan showed RUP and a 25-mm sized tumour peripherally enhanced in the arterial phase in segment 8; a CT scan showed RUP and a 25-mm sized tumour in the left side of the perihilar region, which caused dilatation of intrahepatic distal bile duct and almost occluded the RUP.
A pathological examination showed a poorly differentiated intrahepatic cholangiocarcinoma invading the intrahepatic portal vein; the pathological findings revealed a moderately differentiated cholangiocarcinoma invading RUP.
The patient was treated with right anterior sectionectomy; the patient was treated with left trisectionectomy.
Only nineteen cases of hepatectomy among patients with RUP have been reported in the English-language literature.
RUP is a congenital anomaly in which the umbilical portion exists between the right anterior section and left medial section.
This report emphasizes that the Glissonean approach is useful, especially in cases with anomalous ramifications of the hepatic artery, portal vein and biliary system such as RUP. This procedure contributes to a safe and secure liver surgery.
This paper is the first report about major hepatectomy using the Glissonean approach in cases with RUP, and demonstrates the safety and usefulness of the Glissonean approach for hepatectomy in cases with anomalies such as RUP, and this report is very important guidance for surgeons who perform major hepatectomy for cases with RUP.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Bramhall S, Lau WYJ, Qin JM S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Nagai M, Kubota K, Kawasaki S, Takayama T, BandaiY M. Are left-sided gallbladders really located on the left side? Ann Surg. 1997;225:274-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 88] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 2. | Maetani Y, Itoh K, Kojima N, Tabuchi T, Shibata T, Asonuma K, Tanaka K, Konishi J. Portal vein anomaly associated with deviation of the ligamentum teres to the right and malposition of the gallbladder. Radiology. 1998;207:723-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Asonuma K, Shapiro AM, Inomata Y, Uryuhara K, Uemoto S, Tanaka K. Living related liver transplantation from donors with the left-sided gallbladder/portal vein anomaly. Transplantation. 1999;68:1610-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Baba Y, Hokotate H, Nishi H, Inoue H, Nakajo M. Intrahepatic portal venous variations: demonstration by helical CT during arterial portography. J Comput Assist Tomogr. 2000;24:802-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Savier E, Taboury J, Lucidarme O, Kitajima K, Cadi M, Vaillant JC, Hannoun L. Fusion of the planes of the liver: an anatomic entity merging the midplane and the left intersectional plane. J Am Coll Surg. 2005;200:711-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Hsu SL, Chen TY, Huang TL, Sun CK, Concejero AM, Tsang LL, Cheng YF. Left-sided gallbladder: its clinical significance and imaging presentations. World J Gastroenterol. 2007;13:6404-6409. [PubMed] |
| 7. | Gupta R, Miyazaki A, Cho A, Ryu M. Portal vein branching pattern in anomalous right-sided round ligament. Abdom Imaging. 2010;35:332-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Uesaka K, Yasui K, Morimoto T, Torii A, Kodera Y, Hirai T, Yamamura Y, Kato T, Kito T. Left-sided gallbladder with intrahepatic portal venous anomalies. J Hep Bil Pancr Surg. 1995;2:425-430. [RCA] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Idu M, Jakimowicz J, Iuppa A, Cuschieri A. Hepatobiliary anatomy in patients with transposition of the gallbladder: implications for safe laparoscopic cholecystectomy. Br J Surg. 1996;83:1442-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 1.4] [Reference Citation Analysis (2)] |
| 10. | Kaneoka Y, Yamaguchi A, Isogai M, Harada T. Hepatectomy for cholangiocarcinoma complicated with right umbilical portion: anomalous configuration of the intrahepatic biliary tree. J Hepatobiliary Pancreat Surg. 2000;7:321-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Tashiro H, Itamoto T, Nakahara H, Ohdan H, Kobayashi T, Asahara T. Resection of hepatocellular carcinoma in a patient with congenital anomaly of the portal system. Dig Surg. 2003;20:163-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Hwang S, Lee SG, Park KM, Lee YJ, Ahn CS, Kim KH, Moon DB, Ha TY, Cho SH, Oh KB. Hepatectomy of living donors with a left-sided gallbladder and multiple combined anomalies for adult-to-adult living donor liver transplantation. Liver Transpl. 2004;10:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 13. | Abe T, Kajiyama K, Harimoto N, Gion T, Shirabe K, Nagaie T. Resection of metastatic liver cancer in a patient with a left-sided gallbladder and intrahepatic portal vein and bile duct anomalies: A case report. Int J Surg Case Rep. 2012;3:147-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Sakaguchi T, Suzuki S, Morita Y, Oishi K, Suzuki A, Fukumoto K, Inaba K, Takehara Y, Baba S, Nakamura S. Hepatectomy for metastatic liver tumors complicated with right umbilical portion. Hepatogastroenterology. 2011;58:984-987. [PubMed] |
| 15. | Almodhaiberi H, Hwang S, Cho YJ, Kwon Y, Jung BH, Kim MH. Customized left-sided hepatectomy and bile duct resection for perihilar cholangiocarcinoma in a patient with left-sided gallbladder and multiple combined anomalies. Korean J Hepatobiliary Pancreat Surg. 2015;19:30-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |