Published online Sep 8, 2016. doi: 10.4254/wjh.v8.i25.1087
Peer-review started: April 13, 2016
First decision: May 17, 2016
Revised: July 4, 2016
Accepted: July 29, 2016
Article in press: August 1, 2016
Published online: September 8, 2016
Processing time: 156 Days and 6 Hours
To evaluate all the references about primary gallbladder hidatidosis looking for best treatment evidence.
Search: 1966-2015 in MEDLINE, Cochrane Library, SciELO, and Tripdatabase. Key words: “gallabladder hydatid disease” and “gallbladder hydatid cyst”. We found 124 papers in our searches but only 14 papers including 16 cases were about hydatid cyst of the gallbladder (GBHC).
Eight cases of GBHC were women and seven men. One not mentioned. Median age was 48.3 years. The most frequent clinical symptom was abdominal pain (94%) usually in the right upper quadrant. Ultrasound was performed in ten patients (62.5%) but in most cases a combination of several techniques was performed. The location of the cysts was intravesicular in five patients. Five patients presented GBHC and liver hydatid cysts. Two patients presented cholelithiasis and one choledocholithiasis. The most frequent surgical technique was cholecystectomy by laparotomy (81.25%). Simultaneous surgery of liver cysts was carried out in five cases. Eleven patients did not present postoperative complications, but one died. The mean hospital stay was seven days. No recurrence of GBHC was recorded.
In GBHC, the most frequent symptom is right hypocondrium pain (evidence level V). Best diagnostic methods are ultrasound and computed tomography (level V, grade D). Suggested treatment is open cholecystectomy and postoperative albendazole (level V, grade D) obtaining good clinical results and none relapses.
Core tip: Systematic review of gallbladder hydatidosis has not previously done. We have performed a systematic search trying to define best diagnostic procedures and best therapeutical strategies.
- Citation: Gómez R, Allaoua Y, Colmenares R, Gil S, Roquero P, Ramia JM. Hydatid cyst of the gallbaldder: A systematic review of the literature. World J Hepatol 2016; 8(25): 1087-1092
- URL: https://www.wjgnet.com/1948-5182/full/v8/i25/1087.htm
- DOI: https://dx.doi.org/10.4254/wjh.v8.i25.1087
Hydatid disease is a zoonotic infection found all over the world, which is caused by the larval stage of parasites of the Echinococcus species. Echinococcus granulosus is the most frequent (95% of cases); other species such as Echinococcus multilocularis are rare (5%). Hydatid disease is endemic in cattle-raising regions like the Mediterranean countries, Africa, South America, Middle East, Australia and New Zealand[1,2].
Echinococcus granulosus lives in the intestine of dogs and other wild canines, which are the definitive hosts. Humans are accidentally infected via the fecal-oral route. Larval embryos pass through the intestinal wall and reach the liver through the portal system. Subsequently, through the liver and lungs, parasites reach the arterial circulation and may spread through the rest of the organs[1-3]. The larvae can remain and develop into hydatid cyst anywhere in the body, but liver (70%) and lungs (20%) are the most commonly affected sites.
Primary hydatid cyst of the gallbladder (GBHC) is an exceptional location for hydatidosis, and its pathogenesis is not completely clear. While the literature on liver hydatid disease is abundant, references to the primary involvement of the gallbladder are limited to clinical cases and so it is difficult to reach meaningful conclusions[3-16]. In this paper we present a systematic review of the literature on GBHC published to date.
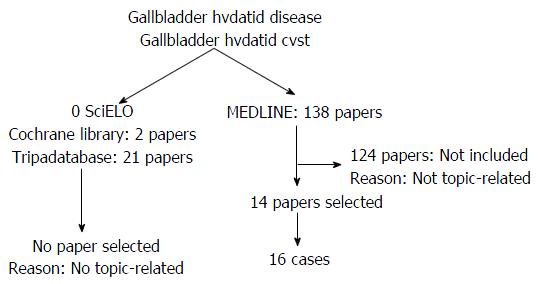
We introduced the following keywords in the MEDLINE (PubMed), Tripdatabase, SciELO and Cochrane Library databases: “gallbladder hydatid disease (GHD)” and “gallbladder hydatid cyst (GHC)” without restrictions on publication date or author until 31 December 2015[17]. The first selection of papers was made after reading title and abstract, and in case of doubt, after reading the full text. A flowchart is shown in Figure 1.
Our results were as follows: (1) zero results in SciELO; (2) 2 results for both searches (GHD and GHC) in the Cochrane Library: Neither met the inclusion criteria; (3) 21 results for GHD and 17 for GHC in Tripdatabase. After review, none were found to be related to the topic; and (4) 137 results for GHD and 138 for GHC in MEDLINE. Since the overlap between search results was 99%, we used the latter search with 138 results; of them, only 14 (10.14%) met the selection criteria for this study.
These 14 papers included 16 clinical cases covering a wide range of clinical, diagnostic and therapeutic aspects of GBHC. These characteristics are summarized in Tables 1-4.
| Ref. | Sex | Age | Abdominal pain | Nausea and vomiting | Fever | Jaundice | Abdominal exploration | Past medical history |
| Noomene et al[3], 2013 | Male | 48 | Diffuse | No (36.7 ºC) | Yes | Painful palpation in right hypocondrium | ||
| Ertem et al[4], 2012 | Male | 32 | Right hyponcondrium and epigastrium | Nausea | No | No | Painful palpation in right hypocondrium | |
| Krasniqi et al[5], 2010 | Female | 39 | Right hypocondrium (18 mo) | Nausea | No | Painful palpation in right hypocondrium | ||
| Murtaza et al[6], 2008 | Female | 32 | Right hyponcondrium and epigastrium (3 mo) | No | No | Hepatomegaly | Liver hydatid surgery 8 yr ago | |
| Sabat et al[7], 2008 | Female | 35 | Right hyponcondrium and epigastrium | Yes | Yes | |||
| Wani et al[8], 2005 | Female | 51 | Right hyponcondrium | |||||
| Pitiakoudis et al[9], 2006 | Male | 60 | Right hyponcondrium (10 d) | Vomiting | Yes (38 ºC-39.5 ºC) | Abdominal distension | ||
| Safioleas et al[10], 2004 | Female | 65 | Right hyponcondrium and epigastrium | Vomiting | ||||
| Safioleas et al[10], 2004 | Female | 51 | Right hyponcondrium (6 mo) | |||||
| Safioleas et al[10], 2004 | Male | 63 | Right hyponcondrium and epigastrium | Normal | ||||
| Kumar et al[11], 2004 | Female | 27 | Diffuse | Relapsed liver hydatid cyst | ||||
| Raza et al[12], 2003 | Male | 27 | Right hyponcondrium (4 mo) | No | No | Hepatomegaly | ||
| Kapoor et al[13], 2000 | Male | 53 | Right hyponcondrium (2 mo) | Yes (high fever, 10 d) | Yes | Abdominal distension, ascitis, gallbladder mass | ||
| Cangiotti et al[14], 1994 | Male | |||||||
| Rigas et al[15], 1979 | Female | 65 | Right hyponcondrium | Vomiting | No | Normal | ||
| Barón Urbano et al[16], 1978 | - | 76 | Right hyponcondrium | Sí | Hepatomegaly, rubi spots in thorax and abdomen | Hepatitis |
| Ref. | Alakaline phosphatase (UI/L) | Bilirrubin (mg/dL) | Ultrasound | CT | MRI | Cysts inside gallbladder | Cholelithiasis | Choledocolitihasis | Serology E. granulosus |
| Noomene et al[3], 2013 | 220 | 7.1 | Yes | Yes | Cholangio MRI | Yes | Positive | ||
| Ertem et al[4], 2012 | Yes | Yes | Yes | Yes | No | No | Negative | ||
| Krasniqi et al[5], 2010 | Yes | Yes | No | ||||||
| Murtaza et al[6], 2008 | 140 | 10.2 | Yes | ||||||
| Sabat et al[7], 2008 | Yes | Yes | |||||||
| Wani et al[8], 2005 | Yes | Yes | Yes | ||||||
| Pitiakoudis et al[9], 2006 | 0.9 | Yes | Yes | Yes | Yes | ||||
| Safioleas et al[10], 2004 | Dude | Dude | |||||||
| Safioleas et al[10], 2004 | Yes | ||||||||
| Safioleas et al[10], 2004 | Yes | Yes | Positive | ||||||
| Kumar et al[11], 2004 | Yes | Yes | |||||||
| Raza et al[12], 2003 | Yes | Yes | |||||||
| Kapoor et al[13], 2000 | 465 | 5.6 | Yes | Yes | Positive | ||||
| Cangiotti et al[14], 1994 | |||||||||
| Rigas et al[15], 1979 | Yes | No | |||||||
| Barón Urbano et al[16], 1978 | 266 | 8.8 |
| Ref. | Preoperative albendazole | Treatment | Liver hydatidosis | Intraoperative treatment cyst | Intraoperative findings |
| Noomene et al[3], 2013 | No | ERCP + Stent Laparoscopy cholecystectomy | No | No | Biliary sludge and stones in ampulla seen in ERCP |
| Ertem et al[4], 2012 | No | Cholecystectomy by laparotomy | No | No | Galbladder cyst with inflammatory changes |
| Krasniqi et al[5], 2010 | No | Cholecystectomy by laparotomy | Yes Cystopericystectomy | No | Calcified primary gallbladder cyst |
| Murtaza et al[6], 2008 | Yes (2 wk) | Subtotal Cholecystectomy by laparotomy | No | Yes | Biliary communication into the cyst closed with sutures |
| Sabat et al[7], 2008 | No | Cholecystectomy by laparotomy | No | Yes (aspiration + hypertonic solution cleaning) | - |
| Wani et al[8], 2005 | No | Cholecystectomy by laparotomy | No | No | - |
| Pitiakoudis et al[9], 2006 | No | Cholecystectomy by laparotomy | No | Yes | - |
| Safioleas et al[10], 2004 | No | Cholecystectomy by laparotomy | No | No | 5 cm × 4 cm cyst |
| Safioleas et al[10], 2004 | No | Cholecystectomy by laparotomy | No | No | 3 cm × 4 cm cyst |
| Safioleas et al[10], 2004 | No | Cholecystectomy by laparotomy | No | No | 5 cm × 4 cm cyst |
| Kumar et al[11], 2004 | No | Cholecystectomy by laparotomy | Yes Cysts segment IV and VIII. Cystopericystectomy segment IV + PAIR segment VII | Yes (aspiration + hypertonic solution cleaning) segment VII cyst | Cyst invading segment IV. Communication between cyst and galbladder |
| Raza et al[12], 2003 | No | Cholecystectomy by laparotomy | Yes Right Lobe Enucleation | No | In gallbladder: Stones and daughter vesicles |
| Kapoor et al[13], 2000 | No | NO. ERCP + Stent | No | No | - |
| Cangiotti et al[14], 1994 | No | Cholecystectomy by laparotomy | SI. Right lobe. Cystoperycystectomy | No | - |
| Rigas et al[15], 1979 | No | Cholecystectomy by laparotomy | No | No | - |
| Barón Urbano et al[16], 1978 | No | Cholecystectomy by laparotomy | Yes Segment IV. Done by thoracotomy | - | Enlarged liver. Cholangitis. Daughter vesicles in cystic conduct lumen |
| Ref. | Pathologic study | Stay | Postoperative treatment | Morbidity | Follow-up |
| Noomene et al[3], 2013 | Cysts in gallbladder. Chronic inflammation | 1 | Albendazole 400 mg/d | No | |
| Ertem et al[4], 2012 | Cyst in gallbladder | 4 | No | 6 mo | |
| Krasniqi et al[5], 2010 | Calcified cyst 7 cm × 5 cm located in gallbladder mucosa | 7 | Albendazole 400 mg/d, 42 d | No | 5 yr |
| Murtaza et al[6], 2008 | No | 2 mo | |||
| Sabat et al[7], 2008 | Albendazole 10 mg/kg, 9 mo | No | |||
| Wani et al[8], 2005 | |||||
| Pitiakoudis et al[9], 2006 | Echinococcus in gallbladder | 12 | Albendazole 800 mg/d, 4 mo | No | 2 yr |
| Safioleas et al[10], 2004 | Echinococcus in gallbladder | No | 10 yr | ||
| Safioleas et al[10], 2004 | Cyst with wall of 5 mm. Daughter vesicles | 7 | No | 6 yr | |
| Safioleas et al[10], 2004 | Calcified cyst with daughter vesicles | 10 | Albendazole 2 mo | Yes: Fever, atelectasis and pleural effusion | 4 yr |
| Kumar et al[11], 2004 | Albendazole | No | 1 yr | ||
| Raza et al[12], 2003 | Albendazole 10 mg/kg per day | No | 1 mo | ||
| Kapoor et al[13], 2000 | Postmortem: Cholangitis, chronic liver obstruction | Yes: Sepsis, Multiorganic failure. Death | |||
| Cangiotti et al[14], 1994 | |||||
| Rigas et al[15], 1979 | Cyst 5 cm × 4 cm with membranes. Echinococcus in gallbladder | 9 | No | ||
| Barón et al[16], 1978 |
In the next step, to assess the quality of the selected studies we used the rating scale described by Manterola et al[18], which assesses each publication individually depending on the type of study, the size of the sample and whether it is justified, and the methodology used. A mean score of all the selected studies is produced ranging from 6 to 36 points, with a quality cut-off score of 18 points. The mean score in our review was 10.3; however, due to the rarity of GBHC and the few studies of this issue published, we selected all the papers available.
We also carried out a qualitative analysis of the selected papers and their conclusions, based on the classical levels of evidence and grades of recommendation proposed in Cook et al[19] and Sackett[20].
Eight cases of GBHC were women and seven men. The sex of one patient was not specified. Median age was 48.3 years (range: 27-76). The most frequent clinical manifestation was abdominal pain (15/16) (94%) (Table 1), in the right upper quadrant in 13 patients) (81.25%), in the epigastrium in four (25%), (three of whom combined upper quadrant pain in right hypochondrium and epigastric pain), and finally diffuse abdominal pain in two (12.5%). In one case, no data on abdominal pain were included (6.25%). Three patients presented vomiting and two had nausea; no information on nausea or vomiting was reported in the rest of patients. Three patients had fever, four were fever-free, and no data on fever were available for the remaining nine patients. Four patients had jaundice, five did not, and no data were available in seven cases. As regards past medical history, two patients had been previously diagnosed with hydatid disease and one had had hepatitis.
On physical examination (Table 1), four patients presented abdominal tenderness, three hepatomegaly, two abdominal distension, and one a palpable mass. Serological information was available in only five cases (Table 2). Levels of alkaline phosphatase and bilirubin were high in four patients, normal in one, and no information was recorded for the other eleven. In the cases in which they were specified, alkaline phosphatase levels were between 140 and 465 IU/L and bilirubin between 5.6 and 10.2 mg/dL. Echinococcus serology was performed in four cases, being positive in three and negative in one.
Image diagnostic methods are described in Table 2. Abdominal ultrasound (US) was performed in ten patients (62.5%), abdominal computed tomography (CT) in nine (56.25%), and magnetic resonance imaging (MRI) in three (18.75%). In most cases a combination of several techniques was performed: US + CT + MRI in three cases, US + TC in three others; so four cases underwent US alone and three CT alone. The location of the cysts was intravesicular in five patients. Five patients presented GBHC and liver hydatid cysts. Two patients presented cholelithiasis and one choledocholithiasis.
The data on therapeutic management are displayed in Table 3. One patient received preoperative albendazole for two weeks, but no data on the other fifteen were available. The most frequent surgical technique was cholecystectomy by laparotomy (81.25%), performed in 13 patients; laparoscopic cholecystectomy was performed in two cases (12.5%), in one of them a previous endoscopic retrograde cholangiopancreatography (ERCP) was done and received a biliary stent; in the last patient, cholecystectomy was not performed, only ERCP and biliary stenting (6.25%). Cholecystectomies were total in 14 cases (93.3%) and subtotal in the patient treated preoperatively with albendazole (6.7%). Simultaneous surgery of liver hydatid cysts was carried out in five cases: Cystopericystectomy in three cases, enucleation in one, and in the other the surgical technique was not specified except for the fact that access was made by thoracotomy. Eleven patients did not present postoperative complications: One presented fever, atelectasis and pleural effusion, and another multiple organ failure and death. No data regarding postoperative outcome were recorded in three cases. The pathological examination (Table 4) was performed in nine patients. In three, the presence of Echinococcus granulosus was confirmed microscopically.
The mean hospital stay was seven days (range: 1-12 d). Seven patients were treated postoperatively with varying doses of albendazole. In nine cases follow-up after the postoperative period was recorded, for a mean period of 38 mo (range: 1-120 mo); no recurrence of GBHC was recorded.
Hydatidosis is a disease caused by the larva of the genus Echinococcus, within which Echinococcus granulosus is the most common species. Although cases have been diagnosed all over the world as a result of increased intercontinental migration, areas in which the incidence is significantly higher include the Mediterranean Sea, Africa, South America, Middle East, Australia and New Zealand. Hydatid disease is prevalent in pastoral areas where cattle and dogs are in close contact. Dogs are the definitive hosts; they excrete eggs in their feces, and humans become intermediate hosts through accidental fecal-oral infection[2,21].
The reviews of Dziri et al[21,22] and Gomez I Gavara et al[1] concluded that many questions about liver hydatidosis still lack evidence-based answers. In 2016, PAIR or surgery, systematic or selective preoperative ERCP, the best surgical approach (conservative or radical), type of technique (laparoscopic or laparotomy), and the use of albendazole all remain topics for debate[1,21,22].
GBHC is an extremely rare entity, even in places where hydatid disease is endemic. Primary involvement is even less common. It is essential to differentiate primary GBHC from secondary invasion of the gallbladder caused by daughter vesicles of primary liver hydatid disease. GBHC can be located within the vesicle or on its outer surface. GBHC pathogenesis is not very well documented; one of the most accepted hypotheses is infestation through the bile duct, although this explanation is unconvincing in cases of superficial cysts, and also often requires prior hepatic involvement. Larval spread through the lymphatic system after intestinal absorption is possible and may explain the intraluminal cysts. Other routes, such as contamination of gallbladder after surgery for hepatic hydatid cyst, should also be considered[3].
In this evidence-based systematic review we have attempted to answer questions about the symptoms, diagnosis and treatment of GBHC. The main limitation is the lack of published series; all the reviewed papers are clinical cases, and so we are unable to reach an acceptable level of evidence. The most common symptom in GBHC is pain in the right upper quadrant[4-10,12-16]. Suspicion of GBHC is established by ultrasound and/or CT[3-13,15]. The involvement of the gallbladder is usually an incidental finding in patients being examined for liver hydatid cysts[4-6,8,10-12,14-16]. The most common therapeutic approach is cholecystectomy by laparotomy and postoperative albendazole[4-12,14-16], Few cases present postoperative complications, and the recurrence of hydatid disease is practically zero[3-12,15].
In conclusion, three main conclusions can be drawn regarding the clinical diagnosis and treatment of GBHC: (1) the most common clinical finding is right upper quadrant pain with a very low level of evidence (level V, grade D recommendation); (2) the most useful diagnostic methods are diagnostic ultrasound and CT with a very low level of evidence (level V, grade D recommendation); and (3) the recommended treatment is cholecystectomy by laparotomy plus albendazole in the postoperative period. This strategy achieves good results: There is no postoperative recurrence in the subsequent months of follow-up, with a very low level of evidence (level V, grade D recommendation). To our knowledge, this is the first literature review that focuses on the clinical, diagnostic and therapeutic aspects of GBHC. The lack of published cases on the topic and the fact that all the papers included deal with clinical cases impeded us from achieving a higher level of evidence in the results. More studies are needed, especially randomized controlled trials, in order to reach meaningful conclusions.
Primary gallbladder hidatidosis is an unfrequent disease. No systematic reviews have been done before.
Obtaining best clinical evidence to treat primary gallbladder hydatidosis.
Future cases and publications will have a systematic review to treat these patients.
Hydatid disease of the gallbladder is very rare, from this point of view this systematic review has some interest.
| 1. | Gomez I Gavara C, López-Andújar R, Belda Ibáñez T, Ramia Ángel JM, Moya Herraiz Á, Orbis Castellanos F, Pareja Ibars E, San Juan Rodríguez F. Review of the treatment of liver hydatid cysts. World J Gastroenterol. 2015;21:124-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 91] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (1)] |
| 2. | Ramia-Angel JM, Gasz A, de la Plaza-Llamas R, Quinones-Sampedro J, Sancho E, Garcia Parreno J. Hidatidosis of the spleen. Pol Przegl Chir. 2011;83:271-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Noomene R, Ben Maamer A, Bouhafa A, Haoues N, Oueslati A, Cherif A. Primary hydatid cyst of the gallbladder: an unusual localization diagnosed by magnetic resonance imaging (MRI). Pan Afr Med J. 2013;14:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Ertem M, Aytaç E, Karaduman Z. Cystic hydatid disease of the gallbladder. Turk J Gastroenterol. 2012;23:825-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Krasniqi A, Limani D, Gashi-Luci L, Spahija G, Dreshaj IA. Primary hydatid cyst of the gallbladder: a case report. J Med Case Rep. 2010;4:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Murtaza B, Malik IB, Mahmood A, Sharif MA, Saeed S, Satti AA. Cholecysto-hydatid cyst fistula. J Coll Physicians Surg Pak. 2008;18:778-780. [PubMed] |
| 7. | Sabat SB, Barhate KP, Deshmukh MP. Cholecysto-hydatid cyst fistula. J Ultrasound Med. 2008;27:299-301. [PubMed] |
| 8. | Wani RA, Malik AA, Chowdri NA, Wani KA, Naqash SH. Primary extrahepatic abdominal hydatidosis. Int J Surg. 2005;3:125-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Pitiakoudis MS, Tsaroucha AK, Deftereos S, Laftsidis P, Prassopoulos P, Simopoulos CE. Primary hydatid disease in a retroplaced gallbladder. J Gastrointestin Liver Dis. 2006;15:383-385. [PubMed] |
| 10. | Safioleas M, Stamoulis I, Theocharis S, Moulakakis K, Makris S, Kostakis A. Primary hydatid disease of the gallbladder: a rare clinical entity. J Hepatobiliary Pancreat Surg. 2004;11:352-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Kumar A, Upadhyaya DN, Singh S, Kumar M, Ansari MA. Cholecysto-hydatid cyst fistula. Indian J Gastroenterol. 2004;23:76-77. [PubMed] |
| 12. | Raza MH, Harris SH, Khan R. Hydatid cyst of gall bladder. Indian J Gastroenterol. 2003;22:67-68. [PubMed] |
| 13. | Kapoor A, Sarma D, Gandhi D. Sonographic diagnosis of a ruptured primary hydatid cyst of the gallbladder. J Clin Ultrasound. 2000;28:51-52. [PubMed] [DOI] [Full Text] |
| 14. | Cangiotti L, Muiesan P, Begni A, de Cesare V, Pouchè A, Giulini SM, Tiberio G. Unusual localizations of hydatid disease: a 18 year experience. G Chir. 1994;15:83-86. [PubMed] |
| 15. | Rigas AM, Karatzas GM, Markidis NC, Bonikos DS, Sotiropoulou GG, Skalkeas G. Primary hydatid cyst of the gallbladder. Br J Surg. 1979;66:406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Barón Urbano C, Diego Estévez M, Pascual Montero J, Suberviola Gómez E. [Ectopia of the gallbladder associated with hepatic hydatidosis]. Rev Esp Enferm Apar Dig. 1978;53:691-698. [PubMed] |
| 17. | Manterola C, Astudillo P, Arias E, Claros N. [Systematic reviews of the literature: what should be known about them]. Cir Esp. 2013;91:149-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Manterola C, Vial M, Pineda V, Sanhueza A. Systematic Review of Literature with Different Types of Designs. Int J Morphol. 2009;27:1179-1186. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Cook DJ, Guyatt GH, Laupacis A, Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest. 1992;102:305S-311S. [PubMed] |
| 20. | Sackett DL. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Chest. 1989;95:2S-4S. [PubMed] |
| 21. | Dziri C, Haouet K, Fingerhut A. Treatment of hydatid cyst of the liver: where is the evidence? World J Surg. 2004;28:731-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 141] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Dziri C, Haouet K, Fingerhut A, Zaouche A. Management of cystic echinococcosis complications and dissemination: where is the evidence? World J Surg. 2009;33:1266-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 107] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Abbasoglu O, Nari GA, Roman A S- Editor: Gong ZM L- Editor: A E- Editor: Li D