Published online Jun 28, 2016. doi: 10.4254/wjh.v8.i18.749
Peer-review started: February 25, 2016
First decision: April 15, 2016
Revised: May 4, 2016
Accepted: June 1, 2016
Article in press: June 3, 2016
Published online: June 28, 2016
Processing time: 123 Days and 13.7 Hours
Quality of life (QoL) after deceased donor liver transplantation is increasingly recognized as a major outcome parameter. We reviewed recent publications in this rapidly evolving field in order to summarize recent achievements in the field and to define opportunities and perspectives for research and improvement of patient care. QoL does improve after liver transplantation according to a typical pattern. During the first year, there is a significant improvement in QoL. After one year, the improvement does stabilise and tends to decline slightly. In addition to the physical condition, different psychological parameters (such as depression, anxiety, sexual function) and sociodemographic elements (professional state, sex, marital state) seem to impact QoL. Opportunities for further research are the use of dedicated questionnaires and identification of influencing factors for QoL.
Core tip: Quality of life (QoL) after deceased donor liver transplantation (LT) is increasingly recognized as a major outcome parameter. This review summarizes a broad spectrum of factors that influence QoL in LT and elucidates the evolution in time of physical and mental QoL after LT. Furthermore attention is given to areas for further investigation and the use of self-report QoL questionnaires in LT. This way, we want to offer a recent and complete overview in this rapidly evolving field.
- Citation: Onghena L, Develtere W, Poppe C, Geerts A, Troisi R, Vanlander A, Berrevoet F, Rogiers X, Van Vlierberghe H, Verhelst X. Quality of life after liver transplantation: State of the art. World J Hepatol 2016; 8(18): 749-756
- URL: https://www.wjgnet.com/1948-5182/full/v8/i18/749.htm
- DOI: https://dx.doi.org/10.4254/wjh.v8.i18.749
In 1967, Thomas Starzl performed the first successful liver transplantation. Over the past few decades liver transplantation (LT) has become a widely accepted treatment for end-stage liver disease, acute liver failure and selected cases of hepatocellular carcinoma with excellent long-term results[1,2]. The first years after the introduction of liver transplantation were characterized by a marked increase of survival rates, due to better pre- and post-operative care, refinement of explanting techniques and organ preservation, better surgical techniques, the development of potent immunosuppressive drugs and improved patient selection. Therefore, mortality and morbidity have decreased[3,4]. Today liver transplantation has a three-month survival rate of about 91.2%, a five-year survival of about 73.3% and a ten-year survival of about 60%[3,5-7].
Survival is the main outcome parameter after liver transplantation and a conditio sine qua non. However, once survival is granted, the real outcome parameter to address the success of liver transplantation on the long term is quality of life (QoL). QoL can be defined as “an overall sense of well-being, including aspects of happiness and satisfaction with life as a whole, which is measurable through mental well being, physical functioning and overall health status”[8]. The World Health Organization defines health as a “state of complete physical, mental and social well-being and not merely the absence of disease and infirmity”. A shift of the focus from life expectancy to QoL can be observed in an increasing number of medical fields and is also taking place in organ transplantation research[9]. The goal of liver transplantation is to achieve a health status that is at least as good as it was before liver transplantation.
Since 2010 many authors have addressed the issue of QoL after LT. Our goal was to collect and compare these new insights and controversies in this research area.
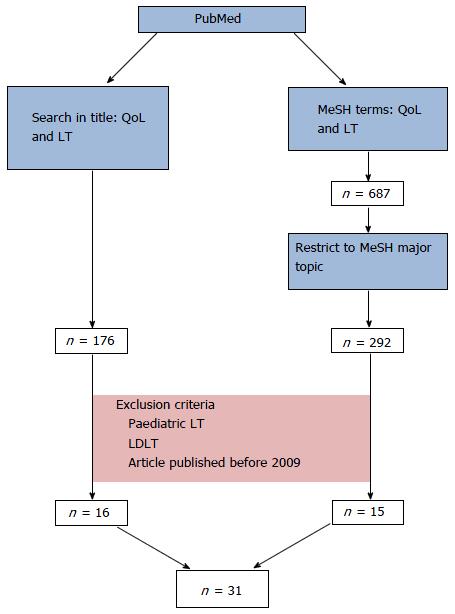
We searched for articles in major databases (PubMed, Google Scholar and Science Direct) from 2009 to 2015. English, French and Dutch manuscripts were eligible.
Search terms “Quality of life” and “Liver transplantation” were used as MeSH terms or searched in the title of the article. Exclusion criteria were paediatric LT, living donor liver transplantation (LDLT) and articles published before 2009. Paediatric patients were excluded due to different interpretation of QoL, reliance on parents and difficult data collection. LDLT patients were excluded due to a different psychosocial process pretransplantation. Only articles between 2009 and 2015 were eligible for inclusion.
Thirty-one publications met our criteria for the PubMed search, including 24 original articles and 7 reviews (Figure 1 and Table 1). The last search was performed September 1st , 2015.
| Ref. | Title | Study design | Population (n) | Instruments used to assess QoL | Main conclusions |
| Masala et al[1] | Quality of life and physical activity in liver transplantation patients: Results of a case-control study in Italy | Case-control | 45 transplant patients 108 controls | SF-36 IPAQ | Transplant recipients are more subject to psychological/emotional distress and low physical function than the general population |
| Lankarani et al[2] | Outcomes of liver transplantation for patients with acute liver failure | Retrospective cross-sectional study | 12 ALF patients 20 cirrhotic patients | N/A | Liver transplantation is safe, effective and should be considered in patients diagnosed with ALF |
| Drent et al[3] | Symptom experience, nonadherence and quality of life in adult liver transplant recipients | Review | N/A | N/A | Health-related quality of life is satisfactory, but below the level of the general population |
| O’Mahony et al[4] | The future of liver transplantation | Review | N/A | N/A | Improvements in surgical techniques, postoperative care, and donor and recipient selection have all contributed to the increased success of OLT and to higher survival rates in patients with advanced liver disease |
| Saidi[5] | Current status of liver transplantation | Review | N/A | N/A | New problems that include severe organ shortage, recurrence of primary disease, opportunistic infections, and development of de novo malignancies are the major problems affecting further implementation of LT |
| Butt et al[8] | Quality of life, risk assessment, and safety research in liver transplantation: New frontiers in health services and outcomes research | Review | N/A | N/A | Recipient quality of life is an area that has grown in importance in the published literature, but several important questions remain unanswered in these areas that merit programmatic, interdisciplinary research |
| Jay et al[9] | A review of quality of life instruments used in liver transplantation | Review | N/A | N/A | There are no available instruments that allow for the precise and reliable assessment of the full QoL impact of liver transplantation |
| Wang et al[10] | Health-related quality of life after liver transplantation: The experience from a single Chinese center | Case-control | 60 post-LT, 55 benign end-stage liver disease, 50 controls | SF-36 | LT patients generally have a good HRQoL although some respects of their HRQoL remains to be improved. Lower family income and poor education are important factors relating to the poor HRQoL of LT patients |
| Chen et al[11] | Health-related quality of life of 256 recipients after liver transplantation | RCT | 256 | SF-36, BAI, SDS | Age > 45 yr at time of transplant, DDLT, full-time working, no complications, anxiety and depression were possible factors influencing postoperative HRQoL in liver recipients |
| Braun et al[12] | Quality of life after liver transplantation | Case-control | 123 recipients, 40 patients on the waiting list and a cohort of healthy controls | EORTC QLQ C30 and a liver transplant specific module | Retransplantation was accompanied by a significant loss of QoL. Cyclosporine-treated recipients displayed a better QoL compared with those treated with tacrolimus. The influence of medical parameters, such of co-morbidity or immunosuppression, needs to be further established with reference to QoL |
| Cannesson et al[13] | Vie quotidienne, grossesse, qualité de vie après transplantation hépatique | Review | N/A | N/A | The global perception of quality of life increases after liver transplantation, but remains lower than in healthy subjects |
| Burra et al[14] | Vie quotidienne, grossesse, qualité de vie après transplantation hépatique | Review | N/A | N/A | Liver transplantation is associated with an improvement in overall QoL. However, this improvement is lower than expected. QoL improves significantly early after liver trans-plantation, but it seems to decrease after the first year after transplantation |
| Zaydfudim et al[15] | Reduction in corticosteroids is associated with better health-related quality of life after liver transplantation | Retrospective analysis of prospective, longitudinal data | 186 | SF-36, BAI, and Center for Epidemiologic Studies Depression Scale | High-dose steroid use for post-transplant immunosuppression in liver transplant recipients is associated with reduced physical and mental HRQoL and increased symptoms of anxiety |
| Sirivatanauksorn et al[16] | Quality of life among liver transplantation patients | Case-control | 57 pre-LT 95 post-LT | SF-36, CLDQ | OLT improved HRQoL of end-stage liver patients and their spouses or caregivers |
| Telles-Correia et al[17] | When does quality of life improve after liver transplantation? A longitudinal prospective study | Cohort study | 60 | SF-36 | Our findings suggested that quality of life improved early after liver transplantation (1 mo). Between the first and the sixth months, there only was a significant improvement in the physical quality of life |
| Bownik et al[18] | When does quality of life improve after liver transplantation? A longitudinal prospective study | Review | N/A | N/A | Greater attention must be paid to patients’ postoperative expectations and the effects of social influences (such as gender, education level, and socioeconomic and ethnic background) |
| Duffy et al[19] | When does quality of life improve after liver transplantation? A longitudinal prospective study | Prospective, cross-sectional study | 168 | SF-36, liver disease quality of life | More than 50% of LT recipients survive 20 yr, achieve important socioeconomic milestones, and report quality of life superior to patients with liver disease or other chronic conditions |
| Narumi et al[20] | Importance of awareness of perioperative social and physical situations of living donors for liver transplantation | Case-control study | 31 | SF-36, Hamilton’s depression and anxiety scores | We must pay attention to depression and anxiety among living donors |
| Thiel et al[21] | Contributors to individual quality of life after liver transplantation | Cross-sectional study | 71 | SF-36, SEIQoL-DW | The five most nominated areas related to QoL are not related to health. By focusing on health, the importance of health-related factors is overrated, and the impact of non-medical effects is under- represented |
| Volk et al[22] | Organ quality and quality of life after liver transplantation | Retrospective cross-sectional study | 171 | SF-36 | No association between organ quality and QOL after liver transplantation is found |
| Baranyi et al[24] | Overall mental distress and health-related quality of life after solid-organ transplantation: Results from a retrospective follow-up study | Retrospective follow-up | 123 | TERS, SCL-90-R SF-36 | Transplantation recipients may face major transplantation- and treatment-related overall mental distress and impairments to their HRQoL. Further, overall mental distress is a high-risk factor in intensifying impairments to patients’ overall quality of life |
| Jurado et al[25] | Coping strategies and quality of life among liver transplantation candidates | Observational | 93 | SF-36, MCMQ | Cirrhosis etiology is not a determinant factor of quality of life, whereas the acceptance-resignation coping strategy might lead to lower self-perception of quality of life |
| Lobo et al[26] | Care complexity, mood, and quality of life in liver pre-transplant patients | Cross-sectional | 60 | SF-36, HADS, INTERMED, EuroQol | High frequency of complexity in liver transplant candidates in European hospitals, but wide between-center differences suggest that local studies in specific hospitals and/or countries may be necessary to document care needs |
| Martín-Rodríguez et al[27] | Affective status in liver transplant recipients as a function of self-perception of general health | Cross-sectional | 168 | SF-36, HADS | Transplant recipients with worse self-perception of general health presented the same anxiety-depressive levels as patients with severe liver disease in the pretransplantation phase |
| Santos et al[28] | Affective status in liver transplant recipients as a function of self-perception of general health | Observational, descriptive and transversal | 73 | SF-36, BDI, structured interviews | Psychological aspects related to transplants require psychological intervention because they can affect the recuperation process, the quality of life, and the adherence to treatment for potential transplant patients |
| Stilley et al[29] | Pathways of psychosocial factors, stress, and health outcomes after liver transplantation | Longitudinal | 130 | N/A | A number of strong bidirectional relationships exist between coping style, self-regulatory ability, hostility, the caregiver relationship and family environment, personal and transplant-related stress over the second half of the first post-transplant year, and health (especially mental) outcomes at 12 mo post-transplant |
| Telles-Correia et al[30] | Predictors of mental health and quality of life after liver transplantation | Cross-sectional | 60 | SF-36 | Quality of life improved early after liver transplantation (1 mo). Between the first and the sixth months, there only was a significant improvement in the physical quality of life |
| Telles-Correia et al[31] | Mental health and quality of life in alcoholic liver disease patients after liver transplantation: A prospective controlled study | Cross-sectional | 45 | SF-36, HADS, brief coping inventory | There is a favorable adjustment of alcoholic liver disease patients after transplantation as shown in coping mechanisms evolution, which might explain the improved mental health and quality of life dimensions |
| Poppe et al[32] | Improving quality of life in patients with chronic kidney disease: Influence of acceptance and personality | Cross-sectional | 99 | SF-36, ICQ, NEO-FFI | Acceptance is an important positive variable in accounting for health-related quality of life |
| Åberg et al[33] | Cost of a quality-adjusted life year in liver transplantation: The influence of the indication and the model for end-stage liver disease score | Cross-sectional | 333 | 15D | The cost/QALY ratio for LT appears favorable, but it is dependent on the assessed time period and the severity of the liver disease |
| Fernández-Jiménez et al[34] | Comparison of quality of life between two clinical conditions with immunosuppressive therapy: Liver transplantation and multiple sclerosis | Cross-sectional | 62 | SF-36 | Transplant recipients belong to a population that still requires special health care. Bio-psychosocial functioning is not fully restored |
Overall QoL: In general, health related QoL (HRQoL) improves and remains stable throughout the years after transplantation, but does not reach the level of the general population. This can be explained by the presence of comorbidities, the severity of the disease and the transplant procedure[3,8,10-14].
HRQoL tends to increase rapidly during the first two years, and remains stable afterwards once almost normal values have been reached[8,15]. Some authors report a more fluctuating evolution with a rapid increase of QoL during the first six months, followed by a stabilization during the remainder of the first year and a rebound effect during the second year due to adaption to certain psychosocial conditions. Patients are confronted with their new health status and can experience problems with re-enrolment in society and more particular difficulties in their professional life. The rebound effect is due to the fact that patients slowly retrieve peer acceptance and can participate in professional and social activities. After two years, in these patients, an improvement can be found until the fifth year after LT[10].
Overall, many studies have proven significant improvements in general and mental health, vitality, social and physical functioning[1,16].
Physical QoL: Overall, physical health starts improving after the first month after transplantation. This effect lasts the first six months, up to 2 years after transplantation[17]. Fluctuations are not uncommon due to the rebound effect[10,13,16]. A lower physical activity can be seen 10 to 30 years post-transplantation in comparison to the general population. This can be explained by the effect of ageing[11,14]. Due to the rapid evolution in the field of LT, older studies do not reflect the common medical practice and should be read with caution.
In summary, an improvement is seen in physical functioning after LT after the first year, if major medical complications are absent, e.g., cytomegalovirus reactivation, rejection and revision[1,18-22].
Mental QoL: The World Health Organisation defines mental health as “a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community”[23]. This vague definition complicates the assessment of mental health QoL after liver and impedes the comparison of different studies. Some authors assessed the mental QoL by measuring anxiety and depression, because of the high correlation with these mental diseases. Burra and Germani[14] showed in their systematic review an increase of depression and anxiety scores during the first year, followed by a decrease afterwards. However, another study reported a significant improvement of depression and anxiety rates especially during the first year after LT in the absence of complications such as biliary events, endocrine disorders, physical and psychiatric problems[11,15]. The relief of the stressful time-lapse awaiting transplantation combined with a better physical health status could be a logical explanation. Furthermore, differences might be related to the presence of underlying psychiatric morbidities. Affective illness, maladjustment and severe anxiety have been diagnosed in 19%-54% of patients during psychiatric evaluation. Obsessive-compulsive, somatization, anxiety and depression symptoms were frequently found. The transplantation and stay at intensive care unit have been considered as traumatic stressors that diminish QoL and can cause overall mental distress. These patients are prone to some psychiatric disorders (e.g., anxiety and affective disorders, posttraumatic stress disorder) and a low QoL after LT[21,24-31].
The short form-36 questionnaire (SF-36) is extensively used to assess the health-related QoL, which is a reliable and standardized tool comparing as well the mental [the mental component summary score (MCS)] as the physical [physical component summary score (PCS)] aspects of QoL. During the first month after liver transplantation, studies show a rapid improvement of the MCS; the improvement of the PCS is slower though more durable and remains at higher levels six to twelve months after transplantation[13,15]. Side effects of immunosuppressive drugs and unmet expectations after liver transplantation can also hamper the improvement of MCS[17].
In summary an improvement is seen in the mental health status within the first months after transplantation and can be influenced by complications such as rejection, infections and biliary events. These are interesting targets for improvement[13-15,27].
Aetiology of liver disease: The original liver disease leading might influence QoL afterwards. Patients transplanted for non-cholestatic liver diseases report a significantly lower QoL after LT in comparison to those with a cholestatic liver disease[12]. Patients with viral hepatitis tend to suffer more from anxiety after LT than patients with alcoholic liver disease[13]. However, others challenge these data[10,14,21]. The influence of aetiology on QoL needs further investigation, since it influences all aspects of QoL[2,14].
Socio-demographic factors: The influence of gender on QoL remains a matter of debate, and data are conflicting[8,11,18].
Relational status however, does impact QoL. Married patients have a better QoL after liver transplantation than single or non-married patients[8,19,28]. This might be explained by a better social support.
Employment after LT is a crucial factor influencing QoL. Unfortunately, only 25% will return to work after two years. Restarting an active professional life after LT generates an income, but also restores the functional role of the patient in society. In employed patients, physical functioning is also improved and this results in an overall better QoL[10,12-14,21].
Early retirement, which is often observed in these patients, negatively impacts QoL. Patients with former alcoholic liver disease have a lower chance to return to work after transplantation, compared to other aetiologies, which can be related to the psychosocial burden present before liver transplantation. This can be explained by the psychosocial burden attached to addiction.
Professional activity before transplantation has a major impact on the general outcome after LT, which improves the activation grade after LT. As one might expect, the type of activities will determine the possibility to return to work, favouring higher educated patients compared to lower educated patients involved in physically demanding manual labour[1,3,13].
Patients regaining professional activities after only one year had a better QoL on the long term with less emotional problems[1,3,8,10,28]. A possible bias could be that only patients in good general condition will resume work. Unemployment leads to a circulus vitiosus: Unemployed patients are less active, therefore less motivated which leads to reduced physical functioning and to lower employment. Professional reactivation should be stimulated after liver transplantation and is an interesting target for improvement of QoL.
Depression and anxiety: Patients with anxiety disorders or depression before LT report a lower QoL. Generally, it is assumed that mental disorders such as anxiety disorders and depression are mostly correlated with the severity of the disease pre-transplant and the occurrence of complications. However, some studies show that the acceptance of the disease is more predictive for a good or bad QoL than the severity of the disease[13,32].
Importantly, high levels of depression may double the chances of mortality. More than half of the recipients experience at least one episode of anxiety disorder or depression within the first two years after transplantation. This negatively impacts MCS[8,11].
Sexual function: An aspect of QoL that often remains taboo, is sexual function after LT. We found some conflicting results. As expected, sexual dysfunction seems to be related to old age, a positive post-transplant status and the presence of depression[14]. In a study of Cannesson et al[13], 70% of the liver transplant recipients declare to have a satisfactory sexual life after LT, even though a decrease is seen in libido, sexual potency and starting of new sexual relationships, caused by bodily changes and immunosuppressive side effects. This high percentage may be caused by a reserve of patients to communicate openly about this topic. Sexual function after liver transplantation is a research area with unmet needs.
Immunosuppressive therapy: Intensified immunosuppressive therapy during the first six months after transplantation can cause uncomfortable side effects[5]. These side effects are common and remain a challenge on the long term[3]. Transplant recipients take a variation of immunomodulating drugs, such as mTOR and calcineurin inhibitors. Their side effects include diabetes mellitus, renal failure, hypertension, tremor, obesity and hypercholesterolemia[4,11,15]. Furthermore, corticosteroids, often used in the first 3 mo can cause insomnia, mood swings and anxiety[15]. Especially high doses of corticosteroids are associated with physical and mental health, however this correlation is not seen with low-dose corticosteroids. Corticosteroid restricting strategies can reduce long-term complications and support QoL[4,15]. Noteworthy, some observations report better QoL in patients using cyclosporines than patients using tacrolimus[8]. However, rejection and re-transplantation affect QoL, and should be avoided by proper immunosuppressive therapy[8,12,13]. We can conclude that the maximal reduction of side effects has a beneficial effect on QoL[12,33,34].
Waiting list: Waiting for a liver transplantation can be long and stressful. The QoL of patients on the waiting list is significantly lower than the QoL of the general population. Length of time spent on the waiting list has a negative impact on QoL. Thirty-eight percent of these patients are fearful (for rejection, death, recurrence of illness), 53% struggle with keeping up with their work-related functions and 23% experience social isolation. Anxiety and negative mood are known to get worse with increasing waiting time[13]. Nevertheless, some authors do not describe an increase in psychosocial stress[28]. More than half of the patients on the waiting list express a need for psychological counselling, which decreases during the waiting time[27].
Areas for further investigation: Although QoL has been extensively studied, we identified several areas of ambiguity. Identifying influencing factors of QoL is crucial to increase QoL after liver transplantation and needs further research[3,12]. In this line some interesting areas of research are: The influence of the underlying condition on QoL, gender, length of stay, immunosuppressive regimens, the influence of the recurrence of the initial liver disease, sexual function and professional reactivation. The development of more liver transplant specific outcome measures could be helpful[13,14].
Self-report QoL questionnaires: For the assessment of QoL more than 50 different instruments are used, measurement is not standardized and generic health assessment questionnaires are very commonly used. The largest part of these instruments has not been designed to evaluate the health status of liver transplant patients. Consequently it is difficult to interpret the results of these questionnaires in a meaningful way[9,14]. The SF-36 is the most commonly used generic questionnaire. It offers broad-spectrum questions applicable to a variety of patient groups and enables comparison between different populations[1,9]. These questionnaires can be distributed before and after LT.
Alternative questionnaires are the Transplant Effects Questionnaire, the Positive Effects of Transplant Scale, the schedule for the evaluation of individual expects of QoL - direct weighting (SEIQoL-DW)... The SEIQoL-DW allows patients to name areas important for him/herself and weigh each area to the relative importance and fulfilment level. On the downside, it is a qualitative interview-based assessment with his inherent disadvantages[21]. This complicates its use in clinical studies and does not enable repeated questioning of the same patient. Other questionnaires are the International Physical Activity Questionnaire and the Chronic Liver Disease Questionnaire. Only 16% of the reported authors used disease-specific instruments[1,9,16].
In conclusion, the best way to measure QoL after LT is the combination of generic questionnaires and disease-specific questionnaires, which offers a broad and thorough assessment of QoL. Jay et al[9] proposed the consistent use of validated, treatment-specific QoL instruments. This will result in a more accurate assessment of QoL in LT and lead to an increasing number of studies with comparable endpoints.
Quality of life should be a major concern for health workers involved in transplant medicine and should be the final “major outcome” to evaluate the success of liver transplantation on the long term. Fortunately, authors report a significant increase in QoL during the first year after liver transplantation, which remains stable afterwards. In general an improvement is seen both in physical and mental QoL. However, they express distinct dynamics after transplantation with a slower but more durable increase for the physical QoL compared to the mental QoL. An integrated biopsychosocial approach is the preferred model to evaluate QoL after liver transplantation.
QoL in liver transplantation is definitely influenced by numerous factors: Mental health, sociodemographic factors, underlying liver disease, immunosuppressive therapy, time on the waiting list, etc.
Our minireview has several limitations. Studies with different endpoints were used, since a lot of studies use different questionnaires to measure QoL. A general image of QoL in LT is given. Consequently not all aspects of QoL are reviewed in detail.
The latter could also be seen as strength of this article since we looked into almost all the aspects of QoL in liver recipients.
We can conclude that in order to further increase the QoL in LT recipients, multidisciplinary interventions of biosocial and psychological treatment are needed. An integrated approach of rehabilitation programs, psychological treatment and thorough repetitive medical follow-up seems to be helpful in these patients with physical and social problems, and stimulates the rehabilitation progress[8,10,28]. Longitudinal monitoring of QoL could increase insight into dynamics of QoL after LT and identify patients at risk for more thorough and individualized follow-up. This is a growing field of research with a lot of unanswered questions and opportunities for improvement strategies.
| 1. | Masala D, Mannocci A, Unim B, Del Cimmuto A, Turchetta F, Gatto G, Santoro R, Ettorre GM, Boccia A, La Torre G. Quality of life and physical activity in liver transplantation patients: results of a case-control study in Italy. Transplant Proc. 2012;44:1346-1350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 2. | Lankarani KB, Eshraghian K, Malek-Hosseini SA, Janghorban P, Geramizadeh B, Eshraghian A. Outcomes of liver transplantation for patients with acute liver failure. Arch Iran Med. 2013;16:64-67. [PubMed] |
| 3. | Drent G, De Geest S, Dobbels F, Kleibeuker JH, Haagsma EB. Symptom experience, nonadherence and quality of life in adult liver transplant recipients. Neth J Med. 2009;67:161-168. [PubMed] |
| 4. | O'Mahony CA, Goss JA. The future of liver transplantation. Tex Heart Inst J. 2012;39:874-875. [PubMed] |
| 5. | Saidi RF. Current status of liver transplantation. Arch Iran Med. 2012;15:772-776. [PubMed] |
| 6. | United Network for Organ Sharing. Richmond, VA (United States of America), 2014. [accessed 2014 Dec]. Available from: http://www.unos.org. |
| 7. | European Liver Transplant Registry. Villejuif (France), 2014. [accessed 2014 Dec]. Available from: http://www.eltr.org/spip.php?article4. |
| 8. | Butt Z, Parikh ND, Skaro AI, Ladner D, Cella D. Quality of life, risk assessment, and safety research in liver transplantation: new frontiers in health services and outcomes research. Curr Opin Organ Transplant. 2012;17:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Jay CL, Butt Z, Ladner DP, Skaro AI, Abecassis MM. A review of quality of life instruments used in liver transplantation. J Hepatol. 2009;51:949-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Wang GS, Yang Y, Li H, Jiang N, Fu BS, Jin H, Yang JX, Chen GH. Health-related quality of life after liver transplantation: the experience from a single Chinese center. Hepatobiliary Pancreat Dis Int. 2012;11:262-266. [PubMed] |
| 11. | Chen PX, Yan LN, Wang WT. Health-related quality of life of 256 recipients after liver transplantation. World J Gastroenterol. 2012;18:5114-5121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Braun F, Teren K, Wilms P, Günther R, Allmann J, Broering DC, Küchler T. Quality of life after liver transplantation. Transplant Proc. 2009;41:2564-2566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Cannesson A, Boleslawski E, Declerck N, Mathurin P, Pruvot FR, Dharancy S. [Daily life, pregnancy, and quality of life after liver transplantation]. Presse Med. 2009;38:1319-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Burra P, Germani G. Long-term quality of life for transplant recipients. Liver Transpl. 2013;19 Suppl 2:S40-S43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Zaydfudim V, Feurer ID, Landman MP, Moore DE, Wright JK, Pinson CW. Reduction in corticosteroids is associated with better health-related quality of life after liver transplantation. J Am Coll Surg. 2012;214:164-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Sirivatanauksorn Y, Dumronggittigule W, Limsrichamrern S, Iramaneerat C, Kolladarungkri T, Kositamongkol P, Mahawithitwong P, Asavakarn S, Tovikkai C. Quality of life among liver transplantation patients. Transplant Proc. 2012;44:532-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Telles-Correia D, Barbosa A, Mega I, Mateus E, Monteiro E. When does quality of life improve after liver transplantation? A longitudinal prospective study. Transplant Proc. 2009;41:904-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Bownik H, Saab S. Health-related quality of life after liver transplantation for adult recipients. Liver Transpl. 2009;15 Suppl 2:S42-S49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Duffy JP, Kao K, Ko CY, Farmer DG, McDiarmid SV, Hong JC, Venick RS, Feist S, Goldstein L, Saab S. Long-term patient outcome and quality of life after liver transplantation: analysis of 20-year survivors. Ann Surg. 2010;252:652-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 205] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 20. | Narumi S, Umehara M, Toyoki Y, Ishido K, Kudo D, Kimura N, Kobayashi T, Sugai M, Hakamada K. Importance of awareness of perioperative social and physical situations of living donors for liver transplantation. Transplant Proc. 2012;44:328-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Thiel C, Landgrebe K, Knubben E, Nadalin S, Ladurner R, Grasshoff C, Königsrainer A, Schenk M, Thiel K. Contributors to individual quality of life after liver transplantation. Eur J Clin Invest. 2013;43:11-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Volk ML, Hagan M. Organ quality and quality of life after liver transplantation. Liver Transpl. 2011;17:1443-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | World Health Organisation. Copenhagen (Denmark), 2014. [accessed 2014 Dec]. Available from: http://www.who.int/features/qa/62/en/. |
| 24. | Baranyi A, Krauseneck T, Rothenhäusler HB. Overall mental distress and health-related quality of life after solid-organ transplantation: results from a retrospective follow-up study. Health Qual Life Outcomes. 2013;11:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Jurado R, Morales I, Taboada D, Denia F, Mingote JC, Jiménez MÁ, Palomo T, Rubio G. Coping strategies and quality of life among liver transplantation candidates. Psicothema. 2011;23:74-79. [PubMed] |
| 26. | Lobo E, Stiefel F, Söllner W, Santabarbara J, Lobo A, Huyse F, Marcos G, Michaud L, Hohenberger W, Ludwig G. Care complexity, mood, and quality of life in liver pre-transplant patients. Clin Transplant. 2013;27:417-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Martín-Rodríguez A, Pérez-San-Gregorio MA, Domínguez-Cabello E, Fernández-Jiménez E, Pérez Bernal J. Affective status in liver transplant recipients as a function of self-perception of general health. Transplant Proc. 2012;44:2619-2621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Santos GG, Gonçalves LC, Buzzo N, Mendes TA, Dias TP, da Silva RC, da Silva RF, de Felicio HC, Santos Júnior R, Miyazaki MC. Quality of life, depression, and psychosocial characteristics of patients awaiting liver transplants. Transplant Proc. 2012;44:2413-2415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Stilley CS, Flynn WB, Sereika SM, Stimer ED, DiMartini AF, deVera ME. Pathways of psychosocial factors, stress, and health outcomes after liver transplantation. Clin Transplant. 2012;26:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Telles-Correia D, Barbosa A, Mega I, Monteiro E. Predictors of mental health and quality of life after liver transplantation. Psychother Psychosom. 2011;80:60-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Telles-Correia D, Barbosa A, Mega I, Monteiro E, Barroso E. Mental health and quality of life in alcoholic liver disease patients after liver transplantation: a prospective controlled study. Transplant Proc. 2011;43:184-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Poppe C, Crombez G, Hanoulle I, Vogelaers D, Petrovic M. Improving quality of life in patients with chronic kidney disease: influence of acceptance and personality. Nephrol Dial Transplant. 2013;28:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 33. | Åberg F, Mäklin S, Räsänen P, Roine RP, Sintonen H, Koivusalo AM, Höckerstedt K, Isoniemi H. Cost of a quality-adjusted life year in liver transplantation: the influence of the indication and the model for end-stage liver disease score. Liver Transpl. 2011;17:1333-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 34. | Fernández-Jiménez E, Pérez-San-Gregorio MA, Martín-Rodríguez A, Domínguez-Cabello E, Navarro-Mascarell G, Bernardos-Rodríguez A. Comparison of quality of life between two clinical conditions with immunosuppressive therapy: liver transplantation and multiple sclerosis. Transplant Proc. 2012;44:2609-2611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Feier FH, Gutierrez JA, Mittal PK, Srivastava M S- Editor: Gong XM L- Editor: A E- Editor: Li D