Published online Mar 27, 2013. doi: 10.4254/wjh.v5.i3.149
Revised: January 18, 2013
Accepted: January 29, 2013
Published online: March 27, 2013
Processing time: 132 Days and 10.7 Hours
Portal venous aneurysm (PVA) is a rare condition characterized by dilatation of the portal venous system. PVA manifestation of symptoms is varied and depends on the aneurysm size, location and related-complications, such as thrombosis. While the majority of reported cases of PVA are attributed to portal hypertension, very little is known about the condition’s pathophysiology and clinical management remains a challenge. Here, we describe a 67-year-old woman who presented with complaint of dyspepsia and without a significant medical history, for whom PVA was incidentally diagnosed. The initial upper abdominal ultrasound revealed marked dilatation of the main portal vein, and subsequent contrast-enhanced computed tomography with angiography revealed a large aneurysm arising from the extrahepatic troncus portion of the portal vein, as well as gastroesophageal varices. A conservative approach using beta-blocker therapy was chosen. The patient was followed-up for 60 mo, during which time the asymptomatic status was unaltered and the PVA remained stable.
- Citation: Debernardi-Venon W, Stradella D, Ferruzzi G, Marchisio F, Elia C, Rizzetto M. Extrahepatic aneurysm of the portal venous system and portal hypertension. World J Hepatol 2013; 5(3): 149-151
- URL: https://www.wjgnet.com/1948-5182/full/v5/i3/149.htm
- DOI: https://dx.doi.org/10.4254/wjh.v5.i3.149
Portal vein aneurysm (PVA) is a disorder of hepatic vascularization that is clinically diagnosed upon imaging findings of venous dilatation larger than 2 cm[1]. The majority of reported PVAs are localized to the main portal vein. Moreover, an appreciable amount of PVAs are associated with artero-venous fistula or vascular malformations, such as hereditary teleangectasia[2]. PVAs are classified as congenital or acquired, and etiologies of the acquired cases include chronic liver disease, pancreatitis, abdominal surgery, or trauma[3]. The manifestation of PVA symptomatology is various and can depend upon the size and related complications, such as thrombosis. However, many cases are asymptomatic and are detected as an incidental finding in routine radiological examinations performed for other indications[2,4-6].
PVA, including asymptomatic types left undiagnosed or untreated, are associated with several severe complications with high mortality rates, including rupture, local compression, or portal hypertension[7-10]. While recent advances in imaging technologies have increased the number of PVA routinely discovered, our knowledge of the underlying pathophysiology remains limited and clinical management remains a challenge.
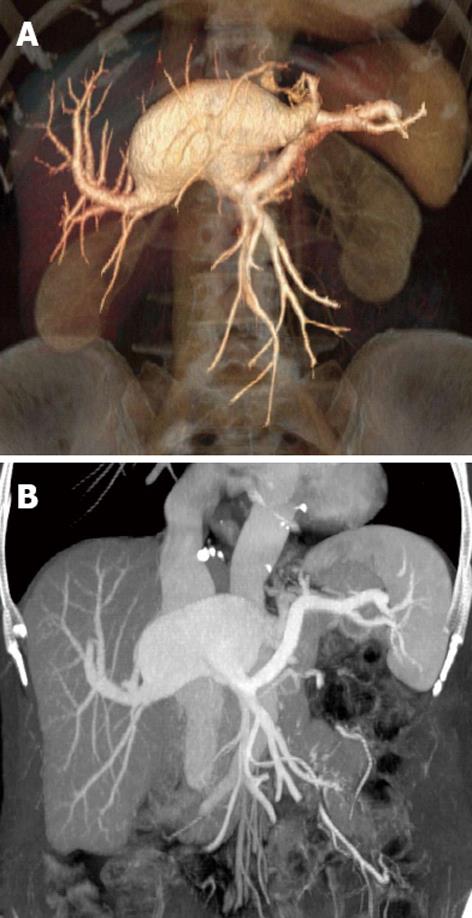
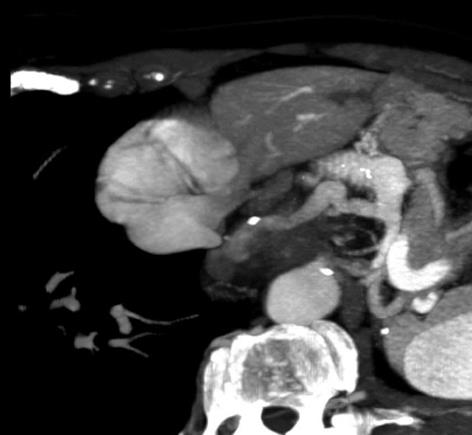
A 67-year-old Caucasian woman was referred to our gastroenterological unit for evaluation of dyspeptic complaint. The patient’s past medical history was unremarkable, and she denied experiencing recent weight change or melena, or abusing alcohol. Initial physical examination revealed no evidence of abdominal pain, jaundice, or hepatomegaly. Results of standard blood tests, including the hepatic function marker profile panel, were within reference ranges. An upper abdominal ultrasound revealed marked dilatation of the main portal vein (diameter: 4 cm; length: 8.5 cm). However, the superior mesenteric vein, splenic vein, and other extrahepatic segments of the portal vein appeared normal. No features of thrombosis were present. The liver itself showed homogeneous parenchyma and normal size. The spleen and pancreas also appeared grossly normal. Subsequent contrast-enhanced computed tomography with angiography (CTA) was performed. The aneurysm was found to arise at the troncus of the extrahepatic portion of the portal vein, proximal to its bifurcation (Figure 1A). The overall size was measured as 8 cm × 4.5 cm, and the neck was 0.2-0.3 cm. The posterior of the aneurysm was located at the portal confluence (Figure 1B). Turbulent blood flow was observed inside the aneurysm, and again no signs of thrombosis were observed (Figure 2). The CTA scanning also showed the spleen to be moderately enlarged (oblique diameter: 12 cm), the pancreas to be normal, and presence of gastric varices (Figure 3). No biliary stones were detected. Upper gastrointestinal endoscopy was performed and revealed small gastroesophageal varices.
The hepatic vein-portal pressure gradient (HVPG) was normal (6 mmHg), confirming a prehepatic origin of portal hypertension. The presence of esophageal varices and signs of portal hypertension prompted the initial consideration of an intrahepatic portocaval shunt to reduce the portal pressure and maintain blood flow. However, the risk of shunt dysfunction and the patient’s refusal for intervention led to the use of a medical therapy approach. The patient was administered carvedilol (50 mg once daily) and monitored by laboratory testing and sonographic imaging every 12 mo. The patient attended routine follow-up appointments, the last being 60 mo after discharge to home. All follow-up examinations indicated asymptomatic status and maintenance of the PVA as stable.
Diagnosis of PVA is often overlooked in asymptomatic patients. Symptomatic clinical presentation is often the result of PVA rupture or secondary thrombosis, portal hypertension, or biliary compression-induced cholestasis[3,7-10]. In the patient described herein, the PVA was diagnosed incidentally by ultrasonographic and CTA examinations, in accordance with its asymptomatic nature. The patient lacked a history of risk factors or indicating signs of PVA, which suggests that the aneurysm may be congenital. The patient’s portal hypertension was determined to be secondary to an increased portal blood flow. The prehepatic origin of inflow justified the HVPG, which is typically normal in prehepatic portal hypertension. The asymptomatic nature of the PVA somewhat complicated the choice of therapy and the patient’s willingness to accept various treatment options.
Portocaval shunting is a successful treatment approach frequently performed in patients with complicated portal aneurysms accompanied by portal hypertension, and intrahepatic portosystemic shunting is considered an effective option for cirrhotic patients as it may prevent the risk of portal thrombosis[11,12]. Accordingly, we considered that a portosystemic shunt may reduce the portal pressure and turbulent flow within the aneurysm to achieve blood stasis in our patient, thereby reducing the risk of thrombosis and rupture. However, the intrahepatic portosystemic shunt is not a recognized therapy of portal aneurysm, and the risk of dysfunction in a patient without history of variceal bleeding is uncertain. This fact, in conjunction with the patient’s preference, led us to apply a conservative management approach. A beta-blocker was selected for the therapy since the patient’s gastroesophageal varices could be a contraindication for anticoagulation therapy[13].
In conclusion, the findings from our case highlights the benefit of ultrasonography and CTA scanning to diagnose asymptomatic PVA and suggests its utility for monitoring PVA patients following conservative therapy.
| 1. | Lau H, Chew DK, Belkin M. Extrahepatic portal vein aneurysm: a case report and review of the literature. Cardiovasc Surg. 2002;10:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Sezgin O, Gürkaynak G, Temuçin G. Portal vein aneurysm in hereditary hemorrhagic telangiectasia. Am J Gastroenterol. 1999;94:3642-3643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Gallego C, Velasco M, Marcuello P, Tejedor D, De Campo L, Friera A. Congenital and acquired anomalies of the portal venous system. Radiographics. 2002;22:141-159. [PubMed] |
| 4. | Glazer S, Gaspar MR, Esposito V, Harrison L. Extrahepatic portal vein aneurysm: report of a case treated by thrombectomy and aneurysmorrhaphy. Ann Vasc Surg. 1992;6:338-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Oliver MI, Calpena R. Images in hepatology. Extrahepatic portal vein aneurysm. J Hepatol. 1998;28:168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Ma R, Balakrishnan A, See TC, Liau SS, Praseedom R, Jah A. Extra-hepatic portal vein aneurysm: A case report, overview of the literature and suggested management algorithm. Int J Surg Case Rep. 2012;3:555-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Okur N, Inal M, Akgül E, Demircan O. Spontaneous rupture and thrombosis of an intrahepatic portal vein aneurysm. Abdom Imaging. 2003;28:675-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Wolff M, Schaefer N, Schmidt J, Hirner A. Thrombosis of a large portal vein aneurysm: treatment by thrombectomy, aneurysmorrhaphy, and portocaval shunt. J Gastrointest Surg. 2006;10:128-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | De Gaetano AM, Andrisani MC, Gui B, Maresca G, Ionta R, Bonomo L. Thrombosed portal vein aneurysm. Abdom Imaging. 2006;31:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Cho SW, Marsh JW, Fontes PA, Daily MF, Nalesnik M, Tublin M, De Vera ME, Geller DA, Gamblin TC. Extrahepatic portal vein aneurysm--report of six patients and review of the literature. J Gastrointest Surg. 2008;12:145-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Turner KC, Bohannon WT, Atkins MD. Portal vein aneurysm: a rare occurrence. J Vasc Nurs. 2011;29:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Senzolo M, M Sartori T, Rossetto V, Burra P, Cillo U, Boccagni P, Gasparini D, Miotto D, Simioni P, Tsochatzis E. Prospective evaluation of anticoagulation and transjugular intrahepatic portosystemic shunt for the management of portal vein thrombosis in cirrhosis. Liver Int. 2012;32:919-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 263] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 13. | Lall P, Potineni L, Dosluoglu HH. Complete spontaneous regression of an extrahepatic portal vein aneurysm. J Vasc Surg. 2011;53:206-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
P- Reviewer Bordas JM S- Editor Wen LL L- Editor A E- Editor Li JY