Revised: February 22, 2011
Accepted: March 1, 2011
Published online: March 27, 2011
Bacillus Calmette-Guerin (BCG) intravesical instillation has been adopted in the treatment of patients with superficial bladder cancer. BCG-induced disseminated infection, though rare, has been associated with the histological finding of epithelioid granulomas in different organs, including the liver. We report the case of an adult patient with multi-organ failure, who developed sepsis, acute respiratory failure and acute hepatic failure with encephalopathy whose liver biopsy confirmed the presence of atypical, granulomatous-like lesions. Recovery was observed only after empirical therapy for Mycobacterium bovis with isoniazid, rifampicin, ethambutol and steroids was introduced. This case highlights the importance of a thorough patient assessment in order to exclude other more common causes of hepatic granulomas and to confirm diagnosis. Histological findings may be non-specific when the liver is involved in BCG-induced disseminated infection.
- Citation: Kaklamanos M, Hardavella G, Trigidou R, Dionellis G, Paissios N, Koulouris N, Goritsas C. Multi-organ failure with atypical liver granulomas following intravesical Bacillus Calmette-Guerin instillation. World J Hepatol 2011; 3(3): 79-82
- URL: https://www.wjgnet.com/1948-5182/full/v3/i3/79.htm
- DOI: https://dx.doi.org/10.4254/wjh.v3.i3.79
Bacillus Calmette-Guerin (BCG) is an attenuated live-strain of Mycobacterium bovis (M.bovis), initially developed as a vaccine against Mycobacterium tuberculosis, which is currently used in the treatment of superficial bladder carcinoma[1,2].
Minor side-effects, such as irritative bladder symptoms, hematuria, fever, arthralgia and myalgia, are the rule in up to 90% of patients treated[3,4]. Significant adverse reactions are uncommon (< 5%), but systemic complications such as severe sepsis, pancytopenia, acute respiratory failure, abscess formation, mycotic aneurysms and haemolytic-uremic syndrome have also been reported[3,4]. BCG-induced disseminated M.bovis infection has been associated with the histological appearance of epithelioid granulomas in various organs, such as the liver, prostate, lungs and bone marrow[5-8].
We report the case of an adult, immunocompetent patient with multi-organ failure comprising sepsis, acute respiratory failure and acute hepatic failure with encephalopathy that had atypical histological findings on liver biopsy and responded well on standard treatment for M.bovis.
A 52-year-old Caucasian male was admitted to our hospital complaining of high fever (39.0°C) with chills, productive cough, dysuria and gross hematuria that started eight days earlier after a traumatic session of intravesical BCG-instillation.
He was diagnosed with a stage II (T3aN0) papillary bladder carcinoma a year previously, had undergone two endoscopic operations and introduced on a BCG-instillation protocol.
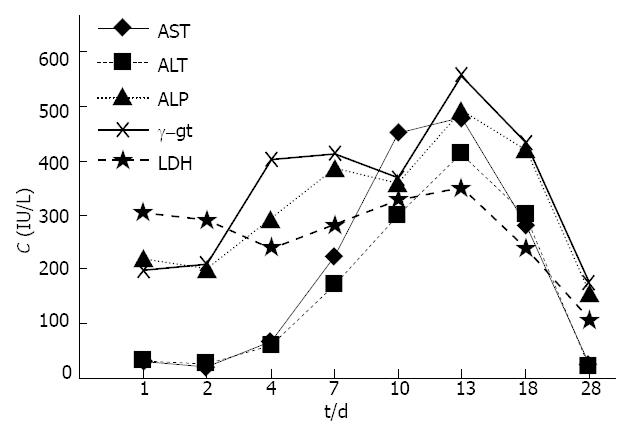
Upon admission, he was febrile (39.0°C) with BP: 125/80 mmHg, HR: 90 beats/min sinus rhythm, RR: 25 breaths/min and SatO2 = 93% (on ambient air). Clinical examination was unremarkable apart from a few scattered bibasal inspiratory crackles. ECG was consistent with sinus tachycardia and ABGs revealed mild hypoxemia/hypocapnia. His liver biochemistry was only mildly affected. The chest X-ray showed a right-sided pleural effusion. Figure 1 shows the time-related deterioration of liver biochemistry parameters.
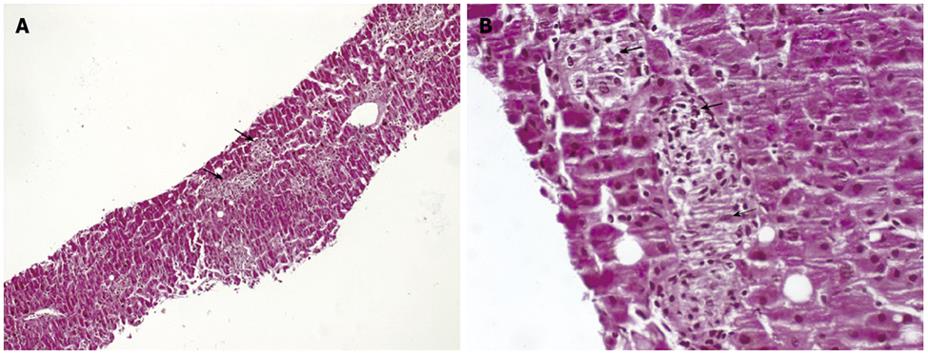
Although, intravenous Piperacillin/Tazobactam (4/0.5 g qds) was initiated on admission for a probable lower respiratory tract infection, he became septic with acute respiratory failure on day 4. A chest CT scan showed alveolar-type consolidating lesions at both lung bases. Therefore, we initiated empirical therapy with isoniazid (5 mg/kg od), rifampicin (10 mg/kg od), ethambutol (20 mg/kg) and prednisolone (15 mg od), after discontinuation of Pip/Tazo (Table 1). Although there was improvement in the patients’ haemodynamic and respiratory parameters by day 7, his laboratory tests continued to deteriorate and, on day 10, he became acutely jaundiced with early signs of hepatic encephalopathy (i.e. flapping and resting tremor). At that point, his liver biochemistry was more consistent with acute hepatitis. Oral lactulose and neomycin were added to the treatment in order to halt the progression of hepatic encephalopathy. A liver fine needle biopsy (FNB) was performed in order to investigate the cause of the persistently deteriorating hepatic function and to exclude drug-related hepatitis as a cause. The biopsy specimen revealed several small, non-specific, granulomatous-like lesions, including histiocytes, findings which were inconclusive for a type-specific hepatitis (Figure 2 A,B). Ziehl-Nielsen staining and a polymerase-chain-reaction (PCR) performed on the biopsied liver tissue were negative while his liver biochemistry kept deteriorating.
| Procedure | Cultures, acid-fast,PCR blood, urine,sputum | Chest CT scan | FNB and liverPCR | |||||
| Day | 1 | 2 | 4 | 7 | 10 | 13 | 18 | 28 |
| Bilirubin | 0.4 | 0.6 | 1.4 | 2.0 | 3.6 | 3.3 | 2.7 | 1.4 |
| CRP | 3.7 | 5.7 | 18.6 | 16.2 | 14.5 | 6.0 | 5.6 | 3.8 |
| Hb | 14.8 | 13.6 | 11.9 | 9.4 | 9.5 | 8.7 | 9.6 | 10.6 |
| WBC | 4.2 | 3.7 | 3.3 | 3.2 | 2.9 | 2.0 | 2.4 | 5.3 |
| PLT | 440.0 | 300.0 | 92.0 | 66.0 | 74.0 | 87.0 | 134.0 | 342.0 |
| Fever | Y | Y | Y | Y | Y | N | N | N |
| Pip/Tazo | STx | Tx | DTx | - | - | - | - | - |
| Isonia | - | - | STx | Tx | Tx | Tx | Tx | Tx |
| Rifamp | - | - | STx | Tx | Tx | Tx | Tx | Tx |
| Ethamb | - | - | STx | Tx | Tx | Tx | Tx | Tx |
| Prednis | - | - | STx | Tx | Tx | Tx | Tx | Tx |
Blood, urine, sputum and bone marrow cultures were all negative for mycobacteria and common bacteria. PCR failed to detect mycobacterial DNA in any of these samples. Serological testing for several gram-positive and gram-negative bacteria, as well as, fungi spp was negative. Viral testing was also negative. Ziehl-Nielsen staining performed on both sputum and urine samples and IFN-γ Release Assay (QuantiFERON-TB Gold) were also negative. Mantoux skin-test at 48 h was less than 5 mm. The results of tumour marker and autoantibody screening were negative. Serum angiotensin-converting enzyme, serum calcium, ferritin, B12 and folate levels were measured within the normal range. An abdominal CT scan was normal and no vegetations were detected on a transthoracic ultrasound heart examination. Bone marrow biopsy findings were inconclusive for a specific diagnosis. Bronchoscopy was not performed due to patient’s hemodynamic decompensation. Apart from liver biopsy, all diagnostic tests were performed prior to the introduction of anti-mycobacterial drugs and steroids (Table 1).
While the patient continued on triple anti-mycobacterial treatment and prednisolone, his liver function began to improve only after day 18 and he was discharged, on day 28, afebrile and with near-normal liver biochemistry. A triple anti-mycobacterial regimen (isoniazid, rifampicin, ethambutol) was continued for for six months and of oral prednisolone for three months post-discharge. A follow-up liver FNB was scheduled after completion of his therapy.
Disseminated infection (“BCG-itis”) following intravesical BCG instillation is a rare, though well-recognized, side-effect of this treatment modality that may present with an early or late onset[3-9]. In particular, biopsy-proven, BCG-induced granulomatous hepatitis and pneumonitis may occur in up to 0.7% and 0.2% of cases, respectively[3,4].
Two possible mechanisms have been implicated in the pathogenesis of systemic BCG infection; hematogenous spread of M.bovis and a delayed-hypersensitivity reaction[5,10]. Although, hematogenous spread seems to be the dominant pathogenetic mechanism, this may not always be supported by solid evidence. The demonstration of mycobacteria may become very cumbersome, as cultures of urine, blood, sputum or biopsied tissues (bone marrow, liver, lungs), as well as acid-fast smears and PCR, are often negative[5,6,10]. Liver biopsies have been reported with positive acid-fast staining in less than 10% of liver tuberculosis cases[6]. This should not inhibit physicians from instigating the recommended anti-mycobacterial regimen (a combination of isoniazid, rifampicin and ethambutol; M.bovis strains are usually resistant to pyrazinamide) for three to six months combined with steroids for three months, as this therapeutic scheme has been reported to be effective in most of the cases of suspected M.bovis disseminated infection[3,5,7,8]. Thus, although in this case we could not isolate M.bovis from any of the different biological specimens (blood, urine, sputum, bone marrow and liver), we strongly considered the possibility of a BCG-induced disseminated infection, in agreement with observations by other colleagues [5,10].
A dramatic improvement in respiratory and haemodynamic parameters was noticed following introduction of a triple anti-mycobacterial/steroids regimen and withdrawal of broad-spectrum iv antibiotics. This response is consistent with that reported by several authors when a possible BCG-related pneumonitis was suspected[7,10]. Usually, the liver is only mildly affected during BCG-related disseminated infection[4,5,8] and this is usually associated with the presence of granulomas containing Langhan’s giant cells[5,7,8]. Our patient, however, developed a severe form of acute hepatic failure, early signs of which were evident even before the introduction of anti-mycobacterial therapy (Figure 1 and Table 1). The applied therapeutic scheme definitely improved his liver biochemistry, and possibly led to the altered findings from FNB(performed on the 6th day of combined anti-mycobacterial/steroids treatment), where we observed small, granulomatous-like lesions rather than the typical giant-cell granulomas. Epithelioid granulomas have been reported in 2-15% of unselected liver biopsies[11]. The etiological classification of diseases causing epithelioid-hepatic granulomas is broad ranging (infectious, hepatobiliary, neoplastic, idiopathic and drug-related), but only a few diseases (primary biliary cirrhosis, sarcoidosis and Q-fever) can be linked directly to specific histological findings[12-14]. Therefore, it is possible that other rarer and less studied causes of granulomatous hepatitis, such as “BCG-itis”, could present with more atypical histological characteristics, as depicted in our case. Steroids could have contributed to the overall clinical and histological response although the extent of their effect cannot be predicted. The timing of liver FNB and the therapy being applied when the biopsy is performed are factors that may influence histological findings.
Finally, the recovery of all blood cell counts only after several days of combined therapy indicates the possible involvement of bone marrow in the BCG-disseminated infection (Table 1).
In conclusion, BCG-induced disseminated disease can cause multi-system failure. Standard, triple anti-M.bovis therapy with steroids led to recovery of our patient’s multi-organ failure. Atypical histological liver findings cannot exclude the diagnosis of BCG-induced liver failure when this is strongly supported by clinical data and therapeutic response.
| 1. | Brassel SA, Kamat AM. Contemporary intravesical treatment options for urothelial carcinoma of the bladder. J Natl Compr Canc Netw. 2006;4:1027. |
| 2. | Kamat AM, Lamm DL. Immunotherapy for bladder cancer. Curr Urol Rep. 2001;2:62-69. |
| 3. | Lamm DL, van der Meijden PM, Morales A, Brosman SA, Catalona WJ, Herr HW, Soloway MS, Steg A, Debruyne FM. Incidence and treatment of complications of bacillus Calmette-Guerin intravesical therapy in superficial bladder cancer. J Urol. 1992;147:596-600. |
| 4. | Lamm DL, Stogdill VD, Stogdill BJ, Crispen RG. Complications of bacillus Calmette-Guerin immunotherapy in 1 278 patients with bladder cancer. J Urol. 1986;135:272-274. |
| 5. | Van Outryve SM, Francque SM, Gentens PA, De Pauw FF, Van den Bogaert E, Van Marck EA, Pelckmans PA, Michielsen PP. Bacillus Calmette-Guerin-induced granulomatous hepatitis in a patient with a superficial bladder carcinoma. Eur J Gastroenterol Hepatol. 2004;16:1027-1032. |
| 6. | Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 29-1998. A 57-year-old man with fever and jaundice after intravesical instillation of bacille Calmette-Guérin for bladder cancer. N Engl J Med. 1998;339:831-837. |
| 7. | Nadasy KA, Patel RS, Emmett M, Murillo RA, Tribble MA, Black RD, Sutker WL. Four cases of disseminated Mycobacterium bovis infection following intravesical BCG instillation for treatment of bladder carcinoma. South Med J. 2008;101:91-95. |
| 8. | Fradet V, Gaudreau C, Perrotte P, Côté J, Paquin JM. Management of hepatic granulomatous tuberculosis complicating intravesical BCG for superficial bladder cancer. Can Urol Assoc J. 2007;1:269-272. |
| 9. | Gonzalez OY, Musher DM, Brar I, Furgeson S, Boktour MR, Septimus EJ, Hamill RJ, Graviss EA. Spectrum of bacille Calmette-Guérin (BCG) infection after intravesical BCG immunotherapy. Clin Infect Dis. 2003;36:140-148. |
| 10. | Molina JM, Rabian C, D’Agay MF, Modai J. Hypersensitivity systemic reaction following intravesical bacillus Calmette-Guerin: successful treatment with steroids. J Urol. 1992;147:695-697. |
| 11. | McCluggage WG, Sloan JM. Hepatic granulomas in Northern Ireland: a thirteen year review. Histopathology. 1994;25:219-228. |
| 12. | Gaya DR, Thorburn D, Oien KA, Morris AJ, Stanley AJ. Hepatic granulomas: a 10 year single centre experience. J Clin Pathol. 2003;56:850-853. |
| 13. | Mills PR, Russell RI. Diagnosis of hepatic granulomas: a review. J R Soc Med. 1983;76:393-397. |
Peer reviewers: Pietro Invernizzi, MD, PhD, Division of Internal Medicine and Hepatobiliary Immunopathology Unit, IRCCS Istituto Clinico Humanitas, via A. Manzoni 113, Rozzano 20089, Milan, Italy; Andrea Nicolini, Professor, Department of Internal Medicine, University of Pisa, via Roma 67, Pisa 56126, Italy
S- Editor Zhang HN L- Editor Hughes D E- Editor Zhang L