Published online Apr 27, 2010. doi: 10.4254/wjh.v2.i4.167
Revised: March 28, 2010
Accepted: April 4, 2010
Published online: April 27, 2010
Transjugular intrahepatic portosystemic shunt (TIPS) is a safe and effective procedure for the treatment of complications of liver cirrhosis, such as refractory ascites, hepatic hydrothorax and refractory variceal bleeding. The aim of this paper is to describe a rare case of liver failure after a TIPS procedure. A 38-year-old diabetic male with Child-Pugh C liver cirrhosis due to chronic hepatitis C infection who had developed refractory ascites was scheduled for a TIPS procedure. Within 24 h following TIPS placement, the patient developed distributive shock, jaundice, persistentgrade 3 hepatic encephalopathy, severe coagulopathy and acute renal failure. He was treated with lactulose enemas, broad-spectrum antibiotics and blood-derived products. Laboratory data revealed a 100-fold increase in aminotransferases and a non-enhanced computed tomography showed an irregular hypodense area in the right posterior segment of the liver. Despite being initially being in a stable condition, the patient developed progressive liver failure and died 2 mo later. Hepatic infarction is an uncommon phenomenon after a TIPS procedure; however, it can greatly complicate the course of a disease in a patient with an already compromised liver function.
- Citation: López-Méndez E, Zamora-Valdés D, Díaz-Zamudio M, Fernández-Díaz OF, Ávila L. Liver failure after an uncovered TIPS procedure associated with hepatic infarction. World J Hepatol 2010; 2(4): 167-170
- URL: https://www.wjgnet.com/1948-5182/full/v2/i4/167.htm
- DOI: https://dx.doi.org/10.4254/wjh.v2.i4.167
Transjugular intrahepatic portosystemic shunts (TIPS) have become a valuable tool in the management of cirrhotic patients[1]. TIPS are frequently employed in the treatment of refractory variceal bleeding, refractory ascites, the Budd-Chiari syndrome, and hepatic hydrothorax and hepatorenal syndromes[2]. TIPS reduce portal pressure by creating a connection between a suprahepatic vein and an intrahepatic branch of the portal vein through a minimally invasive approach. These shunts can be placed by a skilled gastroenterologist or interventional radiologist. The mortality rate is around 1%-2%[3].
The major complications of TIPS are stent dysfunction and hepatic encephalopathy[4]. Stent dysfunction has been significantly reduced with the use of polytetrafluoroethylene (PTFE)-covered stents, with low reintervention rates[5,6]. Hepatic encephalopathy and other less frequent complications of TIPS remain a concern and are subjects for future research, as the number of procedures performed worldwide increases. The aim of this report is to describe a rare case of liver failure after a TIPS procedure.
A 38-year-old male with a history of hypergonadotrophic hypogonadism due to bilateral testicular atrophy after cryptorchidism, and type 2 diabetes mellitus treated with insulin, developed thrombocytopenia. A diagnostic work-up for the hematological cytopenia revealed portal hypertension due to a chronic hepatitis C virus infection.
He had experienced variceal bleeding which was treated with band ligation and portal hypertensive colopathy, treated with argon plasma. One year prior to admission he developed refractory ascites which was treated with evacuatory paracentesis every two weeks. A TIPS procedure was proposed for the treatment of refractory ascites and a comprehensive work-up was performed. A transthoracic echocardiogram showed normal right and left cardiac function without evidence of pulmonary hypertension. A critical flicker test revealed minimal hepatic encephalopathy, which was managed with oral L-ornithine-L-aspartate.
Serum alpha fetoprotein was normal. The portal vein was patent and no focal hepatic lesions were identified on ultrasound evaluation.
Prior to the TIPS procedure, the Model for End-stage Liver Disease score was 6. Physical examination showed tension ascites with no signs of hepatic encephalopathy. Laboratory data at admission (d 0) and follow-up are shown in Table 1. After an evacuatory paracentesis, the patient underwent a TIPS procedure, shunting the right portal vein to the right suprahepatic vein using a 10 mm, 6 cm long uncovered stent (Figure 1). An uncovered stent was placed due to the patient’s poor income.
| Lab/Day | Day 0 | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 |
| Hemoglobin | 10 | 11.6 | 8.4 | 7 | 8.1 | 7.4 | 7.5 |
| WBC | 3.8 | 13.5 | 5.6 | 3.9 | 2.2 | 1.9 | 1.8 |
| Platelets | 40 | 83 | 41 | 25 | 18 | 22 | 26 |
| Creatinine | 0.7 | 1.1 | 1.0 | 1.1 | 0.8 | 0.8 | 0.7 |
| Bilirubin | 1.2 | 5.4 | 5.6 | 4.1 | 4 | 4.3 | 3.9 |
| ALT | 25 | 1209 | 816 | 567 | 389 | 212 | 153 |
| AST | 37 | 3128 | 1110 | 467 | 282 | 145 | 74 |
| INR | 1.2 | 2.2 | 3.2 | 2.1 | 1.5 | 2.1 | 2.0 |
| Albumin | 2.7 | 1.8 | 1.7 | 1.9 | 2.3 | 2.2 | 2.3 |
| HE | 0 | 3 | 2 | 2 | 2 | 2 | 1-2 |
| Troponin I | - | 0 | 0 | - | - | - | - |
| CK/CK-MB | - | 30/11 | 28/11 | - | - | - | - |
| TPT | - | - | 40 | 38.8 | - | - | - |
| Fibrinogen | - | - | 94 | 200.8 | - | - | - |
| D-dimer | - | - | 203 | 363.4 | - | - | - |
| MELD | 6 | 23 | 26 | 21 | 14 | 18 | 16 |
Within 24 h of the procedure, the patient developed fever (38.7°C), tachycardia, hypotension, grade 1-2 hepatic encephalopathy, jaundice, left-shifted leucocytosis and acute renal failure; alanine aminotransferase increased up to 1 209 UI/L and aspartate aminotransferase to 3 128 UI/L, with worsening hyperbilirubinemia and coagulopathy. Blood and ascites cultures were taken and supportive therapy was begun.This included dosing the patient with broad-spectrum antibiotics (imipenem, vancomycin and amikacin adjusted to renal function), rectal lactulose, and vasopressor treatment with norepinephrine lasting 36 h. Antibiotics were suspended on the fifth day due to the absence of clinical, radiological or microbiological evidence of infection. Liver failure was identified as the cause of distributive shock. After discontinuing the antibiotics, the patient did not exhibit any further worsening of his general condition, and no fever or leukocytosis were documented.
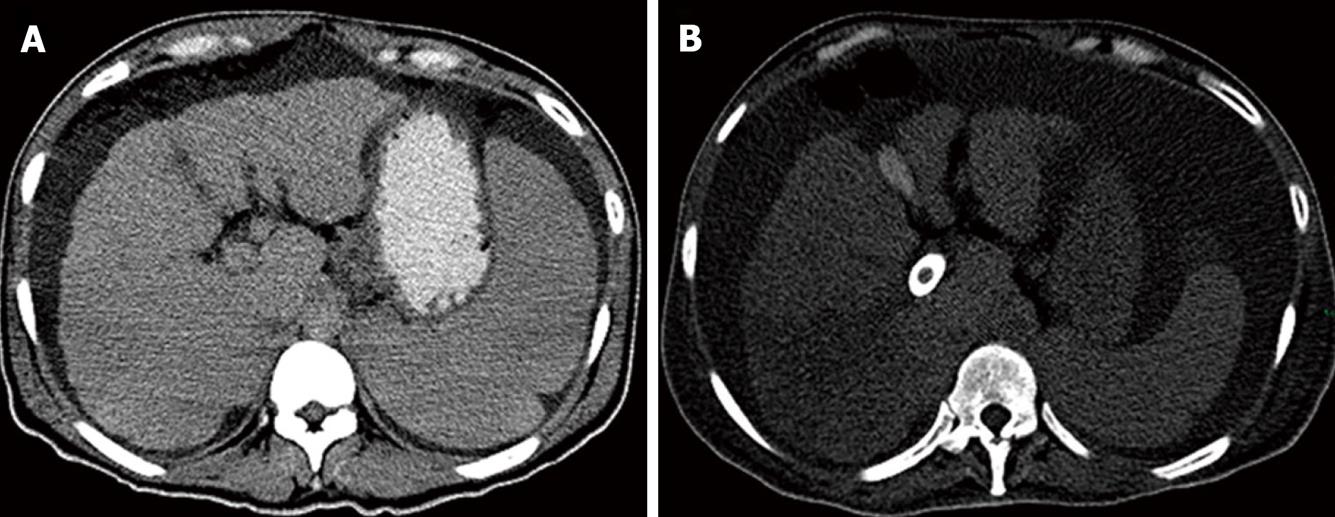
However, during the next 48 h, the patient’s condition worsened. He developed lower gastrointestinal bleeding which was attributed to portal colopathy, with a hemoglobin drop from 11.6 to 7 gr/dL and disseminated intravascular coagulation (DIC), which was treated with an infusion of fresh frozen plasma and cryoprecipitates. A Doppler ultrasound showed a patent TIPS and normal flow in main hepatic artery. An abdominal Computed Tomography scan showed abundant ascites and a hypodense triangular-shaped heterogeneous area in segment 5 of the liver, suggestive of hepatic infarction (Figure 2). No clinical signs of heart failure or electrocardiographic changes were identified. Cardiac enzymes were within normal limits and a new transthoracic echocardiogram showed left ventricle hyperkinesia with normal ejection fraction and no signs of pulmonary hypertension.
After 7 d of supportive therapy the patient’s condition improved; liver enzymes, bilirubin, international normalized ratio and blood cell count all improved, but none returned to baseline. He was discharged with a close follow-up. The patient developed progressive liver failure and died 2 mo later.
TIPS provide rapid decompression of portal pressure by creating a shunt, from a high-pressure portal vein branch to a low-pressure hepatic vein through the hepatic parenchyma. During the last two decades, TIPS have revolutionized the field of portal hypertension management. Inserting PTFE-covered stents has resulted in low thrombosis and stenosis rates, a technological breakthrough that, in turn, has reduced reintervention rates. Because of the low morbidity and mortality rates associated with it, a TIPS procedure now often constitutes a therapeutic bridge to liver transplantation for an increasing number of patients unfit for a surgical derivation procedure.
The hyperdynamic circulation state that characterizes liver cirrhosis induces an increase in hepatic blood flow in these patients, leading to a total hepatic perfusion 25% higher than healthypatients, but portosystemic intrahepatic shunts and sinusoidal capillarization reduce the amount of blood flow in contact with the sinusoidal membrane (functional hepatic flow), leading to a 60% lower sinusoidal perfusion in cirrhotic patients, compared with 95% in healthy patients[7-10].
Hepatic ischemia is a rare event after a TIPS procedure, with fewer than 10 cases described in the literature. The first case reported was an asymptomatic hepatic infarction identified incidentally by nuclear imaging and confirmed by angiography[11]. Other cases of hepatic ischemia have been related to hepatic arterial injury by occlusion or placement of TIPS in the artery and an arterio-venous fistula treated with embolization with subsequent infarction[12-14]. Two cases of liver failure associated with hepatic infarction after a TIPS procedure have been reported[15,16].
The pathogenesis of hepatic infarction after a TIPS procedure is not clear. The stolen portal flow to the hepatic veins via TIPS could compromise hepatic perfusion in the involved segments; however, in order to perpetuate infarction in such a localized manner, arterial flow could also be disturbed. Several hypotheses have been proposed, such as direct arterial injury, decreased hepatic arterial flow due to hypotension and shock, and occult hepatic artery thrombosis due to DIC[15]. An alternative hypothesis that could explain this complication following TIPS is the extrinsic compression of a branch of the hepatic artery after the deployment of the stent in the parenchyma. Histological studies have shown that this compression is usually minimal[17], however, those patients with a higher degree of compression might be those who ultimately develop infarction.
On the other hand, it has been argued that the pathophysiology of hepatic infarction after TIPS is a “partial” Budd-Chiari syndrome, in which the PTFE-covered part of the stents produces hepatic congestion by obstructing a part of the hepatic vein, suggesting that puncturing the hepatic vein near its ostium, would avoid occlusion of the hepatic flow[18]. Nevertheless, neither the occlusion of the hepatic vein has been constantly associated with hepatic infarction nor has this approach ever been proven useful to prevent it[16]. Furthermore, the current case developed it in spite of using uncovered TIPS.
In conclusion, hepatic infarction following a TIPS procedure is a rare but potentially devastating complication. Avoidance of any injury to the hepatic artery during the procedure, ensuring an adequate postoperative hepatic perfusion as well as aggressive therapeutic treatment of early complications are mandatory. Patients with Child-Pugh C cirrhosis should be monitored closely so that potentially fatal liver failure may be overcome.
Peer reviewer: Gareth John Morris-Stiff, MD, PhD, Department of Surgery, Cwm Taf NHS Trust, Ynysmaerdy, LLantrisant, Rhondda Cynon Taf, CF72, XR, Wales, United Kingdom
| 1. | Wong F. The use of TIPS in chronic liver disease. Ann Hepatol. 2006;5:5-15. |
| 2. | LaBerge JM. Transjugular intrahepatic portosystemic shunt--role in treating intractable variceal bleeding, ascites, and hepatic hydrothorax. Clin Liver Dis. 2006;10:583-598, ix. |
| 3. | Rosado B, Kamath PS. Transjugular intrahepatic portosystemic shunts: an update. Liver Transpl. 2003;9:207-217. |
| 4. | Riggio O, Angeloni S, Salvatori FM, De Santis A, Cerini F, Farcomeni A, Attili AF, Merli M. Incidence, natural history, and risk factors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt with polytetrafluoroethylene-covered stent grafts. Am J Gastroenterol. 2008;103:2738-2746. |
| 5. | Bureau C, Garcia-Pagan JC, Otal P, Pomier-Layrargues G, Chabbert V, Cortez C, Perreault P, Péron JM, Abraldes JG, Bouchard L, Bilbao JI, Bosch J, Rousseau H, Vinel JP. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology. 2004;126:469-475. |
| 6. | Bureau C, Pagan JC, Layrargues GP, Metivier S, Bellot P, Perreault P, Otal P, Abraldes JG, Peron JM, Rousseau H, Bosch J, Vinel JP. Patency of stents covered with polytetrafluoroethylene in patients treated by transjugular intrahepatic portosystemic shunts: long-term results of a randomized multicentre study. Liver Int. 2007;27:742-747. |
| 7. | Pan Z, Wu XJ, Li JS, Liu FN, Li WS, Han JM. Functional hepatic flow in patients with liver cirrhosis. World J Gastroenterol. 2004;10:915-918. |
| 8. | Weidekamm C, Cejna M, Kramer L, Peck-Radosavljevic M, Bader TR. Effects of TIPS on liver perfusion measured by dynamic CT. AJR. 2005;184:505-510. |
| 9. | Yamamoto T, Kobayashi T, Phillips MJ. Perinodular arteriolar plexus in liver cirrhosis. Scanning electron microscopy of microvascular casts. Liver. 1984;4:50-54. |
| 10. | Baron A, Gulberg V, Sauter G, Waggershauser T, Reiser M, Gerbes AL. Effects of transjugular intrahepatic portosystemic shunt (TIPS) on quantitative liver function tests. Hepatogastroenterology. 1998;45:2315-2321. |
| 11. | Villemaire JM, Dufresne MP, Lebouthillier G, Picard D, Morais J, Chartrand R, Picard M. Vascular complication of a transjugular intrahepatic portacaval stent. Clin Nucl Med. 1993;18:955-957. |
| 12. | Lim HL, Abbitt PL, Kniffen JC, Myers BM. Hepatic infarction complicating a transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. 1993;88:2095-2097. |
| 13. | Haskal ZJ, Pentecost MJ, Rubin RA. Hepatic arterial injury after transjugular intrahepatic portosystemic shunt placement: report of two cases. Radiology. 1993;188:85-88. |
| 14. | Sawhney R, Wall SD, Yee J, Hayward I. Hepatic infarction: unusual complication of a transjugular intrahepatic portosystemic shunt. J Vasc Interv Radiol. 1997;8:129-132. |
| 15. | Mayan H, Kantor R, Rimon U, Golubev N, Heyman Z, Goshen E, Shalmon B, Weiss P. Fatal liver infarction after transjugular intrahepatic portosystemic shunt procedure. Liver. 2001;21:361-364. |
| 16. | Vizzutti F, Arena U, Rega L, Zipoli M, Abraldes JG, Romanelli RG, Tarquini R, Laffi G, Pinzani M. Liver failure complicating segmental hepatic ischaemia induced by a PTFE-coated TIPS stent. Gut. 2009;58:582-584. |
| 17. | Freedman AM, Sanyal AJ, Tisnado J, Cole PE, Shiffman ML, Luketic VA, Purdum PP, Darcy MD, Posner MP. Complications of transjugular intrahepatic portosystemic shunt: a comprehensive review. Radiographics. 1993;13:1185-1210. |
| 18. | LaBerge JM, Kerlan RK. Liver infarction following TIPS with a PTFE-covered stent: is the covering the cause? Hepatology. 2003;38:778-779; author reply 779. |
| 19. | Kobayashi S, Matsui O, Yoshikawa J, Gabata T, Kawamori Y, Sanada J, Terayama N, Kadoya M. Prevention of hepatic infarction as acute-phase complication of TIPS by temporary balloon occlusion in a patient with primary myelofibrosis. Radiat Med. 2004;22:432-436. |