Published online Sep 27, 2025. doi: 10.4254/wjh.v17.i9.107631
Revised: May 22, 2025
Accepted: September 9, 2025
Published online: September 27, 2025
Processing time: 176 Days and 2.9 Hours
Primary liver cancer is the sixth most prevalent malignancy worldwide and the third leading cause of cancer-related death. According to the latest data from the National Cancer Center of China, its mortality rate has risen, making it the country’s second-deadliest tumor. Hepatocellular carcinoma (HCC), the predo
Core Tip: This article provides a comprehensive evaluation of postoperative adjuvant therapies for hepatocellular carcinoma in patients at high risk of recurrence, detailing the clinical advantages of diverse diagnostic and therapeutic modalities. It highlights the significance and challenges of adjuvant treatment, highlighting the necessity and benefits of multimodal strategies and interdisciplinary collaboration. These insights aim to improve prognosis, extend survival, and inform personalized adjuvant therapy following liver cancer resection.
- Citation: Liu F, Zhang J, Li K. Postoperative adjuvant management in hepatocellular carcinoma: A review of therapeutic efficacy and prognostic outcomes. World J Hepatol 2025; 17(9): 107631
- URL: https://www.wjgnet.com/1948-5182/full/v17/i9/107631.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i9.107631
According to World Health Organization estimates, approximately 900000 new cases of primary liver cancer were diagnosed worldwide in 2020, resulting in about 830000 deaths. China accounted for nearly half of these cases, with 410000 new diagnoses (45.3% of the global total) and 390000 deaths (47.1%), the highest numbers globally[1]. Data from China’s National Cancer Center indicate that hepatocellular carcinoma (HCC) constitutes 7.6% of all cancers, making it the fourth most common malignancy in the country; it is now the second leading cause of cancer related mortality[2]. HCC is the predominant pathological subtype of primary liver cancer, comprising roughly 90% of cases[3]. Surgical resection remains the standard treatment for eligible patients. Although advances in operative technique and perioperative care have improved 5-year survival compared with historical data, the global 5-year survival rate remains only 14.1% because of the tumor’s aggressive biology and late presentation[4]. Postoperative recurrence is also frequent, occurring in up to 70% of patients within five years, with most recurrences arising during the first 2 years after surgery[5]. Wu et al[6] reported similarly unfavorable outcomes, with 27.9% of patients relapsing between years 1 and 3 after rese
Postoperative adjuvant therapy seeks to prevent tumor recurrence after curative treatment, thereby improving patient survival[7]. Selecting an appropriate regimen is crucial for reducing recurrence rates and improving long-term outcomes. A Chinese expert consensus recommends individualized adjuvant therapy based on surgical and tumor-related factors to optimize tertiary prevention and improve prognosis[8]. Nevertheless, preventing postoperative HCC recurrence remains a substantial clinical challenge. The efficacy and potential interactions of available adjuvant options have not been fully elucidated, and standardized guidelines are still lacking[9-11].
Recurrence is the principal obstacle to successful HCC management, markedly limiting the benefits of surgery and worsening patient prognosis. Identifying high-risk factors and implementing suitable adjuvant strategies are therefore critical. Recurrence follows a bimodal pattern, peaking at 1-2 years (early recurrence) and again at 4-5 years (late recu
Three broad categories of recurrence risk factors have been identified: Tumor-related characteristics, surgical variables, and patient-specific features. Early recurrence is primarily linked to tumor biology and surgical parameters, whereas late recurrence is more closely associated with the status of the underlying liver disease. Key independent predictors of early recurrence include large tumor diameter (> 5 cm), portal vein thrombosis, microvascular invasion (MVI), and peritumoral infiltration[18-22]. Additional established contributors are multifocal tumors, poor differentiation (Edmondson III/IV), lymphnode metastasis, a narrow surgical margin (≤ 1 cm), and persistently elevated α-fetoprotein levels. Risk factors for late recurrence relate chiefly to hepatic condition and patient demographics: Advanced age (> 60 years); hepatitis B surface antigen positivity; active viral hepatitis; hypoalbuminemia; and advanced fibrosis (Ishak score > 6)[23-29].
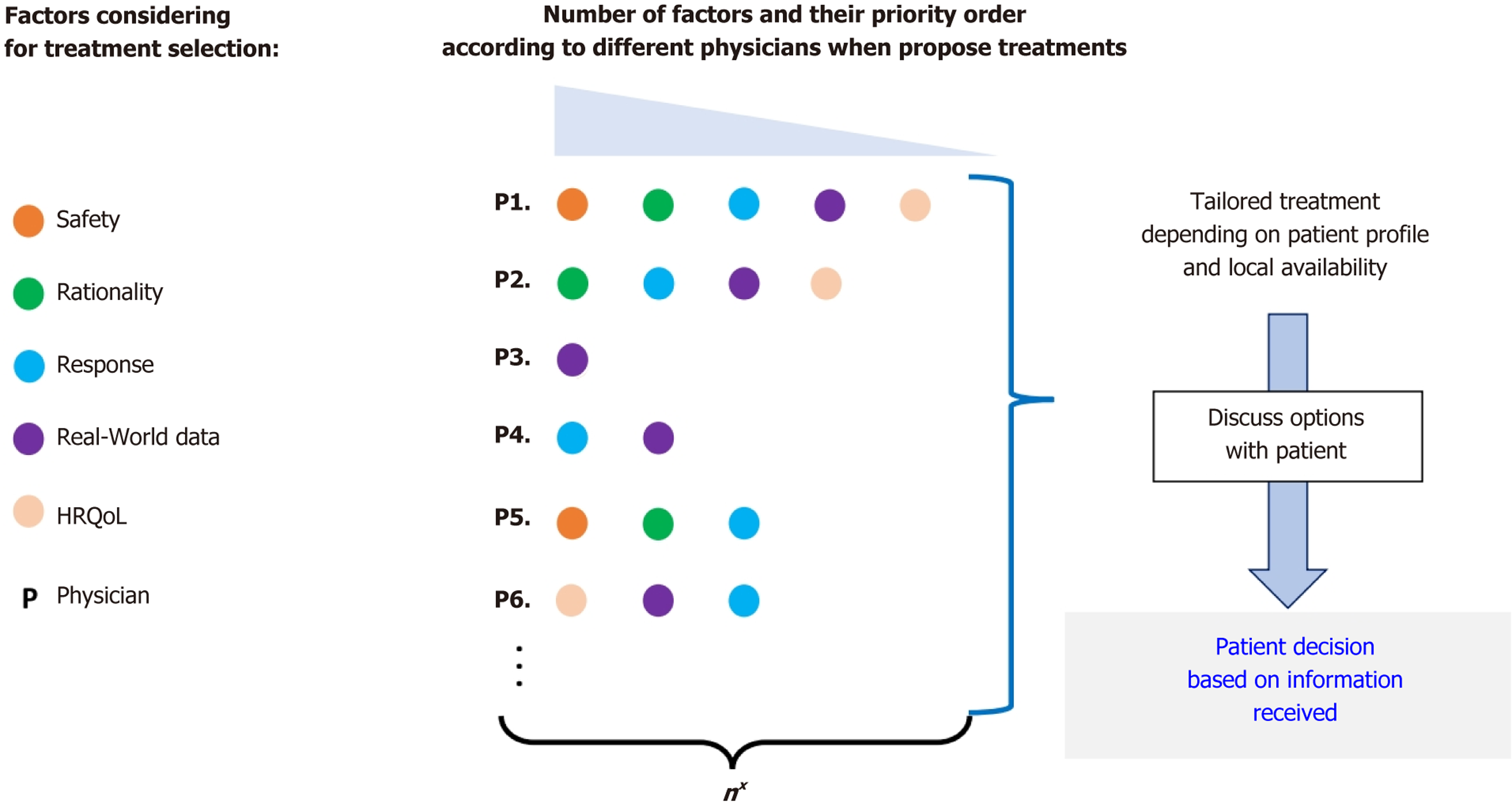
To date, convincing evidence that adjuvant therapy can prevent postoperative HCC recurrence or metastasis is lacking. Nonetheless, several modalities are in use, and multiple promising approaches are under active investigation. Current research focuses on systemic antitumor agents - such as targeted drugs and immune checkpoint inhibitors (ICIs) - and localized treatments, including transarterial chemoembolization (TACE) and radiotherapy, evaluated both individually and in combination. When selecting an adjuvant regimen, clinicians should weigh safety, efficacy, adverse event profiles, and real-world data. Muñoz-Martínez et al[30] emphasized that therapeutic choices can vary among physicians, de
TACE is a widely used locoregional therapy for intermediate to advanced stage HCC, yet its efficacy as an adjuvant treatment after curative resection remains uncertain. Large studies suggest that prophylactic TACE may improve disease-free survival (DFS) in high-risk patients, particularly those with MVI or a substantial tumor burden[31]. For example, Wang et al[32] reported that postoperative TACE reduced recurrence by 33% and mortality by 41% in patients with MVI, multiple tumors, or single tumors > 5 cm compared with surgery alone. Likewise, Wei et al[33] found that adjuvant TACE sig
Conversely, other evidence calls these benefits into question. In a 2020 prospective randomized controlled trial (RCT), Hirokawa et al[34] allocated 114 resected HCC patients to adjuvant TACE (n = 55) or observation (n = 59) and observed no significant difference in DFS at 1, 3, and 5 years (82%, 55%, and 40% vs 75%, 48%, and 35%; P > 0.05). In contrast, Luo et al[35] analyzed a large retrospective cohort (n = 1505) with propensity score matching (PSM) and showed that TACE significantly improved DFS and OS in patients with MVI (all P < 0.001). Using a similar PSM design, Bai et al[36] confirmed in 2023 that adjuvant TACE is an independent prognostic factor for favorable outcomes after resection.
Growing evidence shows that adjuvant TACE lowers recurrence rates and extends survival in HCC patients with high-risk features, and emerging data suggest that combining TACE with systemic agents may further enhance outcomes in this population.
The 2023 Chinese expert consensus[8] recommends hepatic arterial infusion chemotherapy (HAIC) with a folinic acid, fluorouracil, and oxaliplatin regimen as an effective adjuvant to TACE, reporting significant improvements in RFS among patients with MVI. Folinic acid, fluorouracil, and oxaliplatin - suppresses tumor cell proliferation through the synergistic activity of its three components. Supporting evidence from He et al[37] indicates that HAIC increases surgical resectability and reduces recurrence in early-to-intermediate stage HCC; when combined with resection, HAIC also significantly improves OS. Although these findings are encouraging, the evidence base remains limited because few clinical studies have assessed HAIC in the postoperative setting.
Radiofrequency ablation (RFA) is a minimally invasive thermal technique that destroys tumors through localized heating. Approved by the Food and Drug Administration in 1997 for hepatic indications, RFA has become the first-line ablative therapy worldwide for both primary and metastatic liver malignancies[38]. Clinical studies show 5-year survival rates of 60.2%-64% for early-stage HCC (≤ 3 cm), with 10-year survival reaching 27.3%[39,40]. Optimized protocols now extend their use to the management of locally advanced disease[41].
Current evidence for adjuvant postoperative radiotherapy in HCC is limited and inconclusive. Few RCTs have assessed this approach, and results have been inconsistent. A retrospective analysis by Zhu et al[42] indicated that radiotherapy might prolong RFS and OS, but these findings require validation. In a comprehensive meta-analysis, Wang et al[43] pooled data from three RCTs, one phase 2 trial, and six retrospective studies, demonstrating improved DFS and OS, particularly in patients with narrow surgical margins, MVI, or portal vein tumor thrombosis. Although these obse
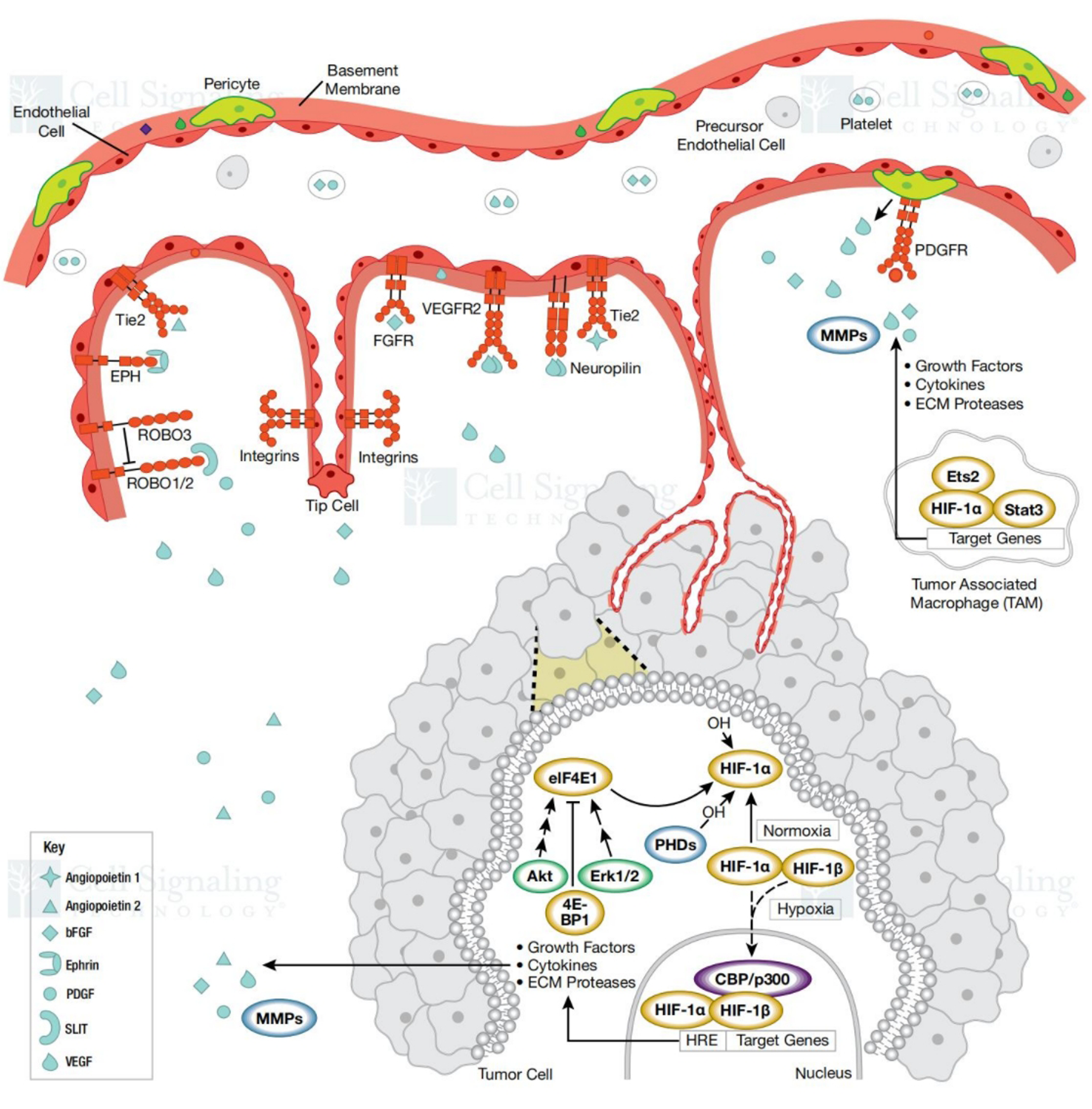
Paradoxically, some evidence indicates that RFA itself may increase the risk of HCC recurrence. In addition to residual micro metastases, hypoxia-driven pathways triggered after ablation can enhance tumor invasiveness[44,45]. Ra
The therapeutic landscape of HCC shifted in 2007 with the approval of sorafenib, inaugurating molecular targeted therapy. Subsequent agents - regorafenib, lenvatinib, and cabozantinib - have further expanded treatment options. Llovet et al[52] summarized the mechanisms of these agents and their efficacy in advanced HCC. Although sorafenib, lenvatinib, donafenib, and regorafenib confer survival benefits in unresectable disease[53-57], their value as adjuvant therapy after curative resection remains uncertain.
The phase 3 STORM trial[58] found no significant difference in RFS between sorafenib (33.3 months) and placebo (33.7 months; P = 0.26); however, 92% of participants had single tumors ≤ 3.5 cm, 68% lacked MVI, and median α-feto
| Ref. | Drug | Type of trial | Primary end point | Result |
| Molecular targeted therapy | ||||
| Bruix et al[58], 2015 | Sorafenib | A phase 3, randomised, double-blind, placebo-controlled trial | RF | mRFS: 33.3 m |
| Zhang et al[59], 2014 | Sorafenib | Single-center retrospective analysis | RFS and OS | RFS: 11.7 m |
| OS: 32.4 m | ||||
| Bai et al[60], 2022 | Lenvatinib | A retrospective analysis | Recurrence and survival rates | 1-year, 2-year recurrence rate: 15.9%, 43.2% |
| 1-year, 2-year survival rate: 85.8%, 71.2% | ||||
| Sun et al[6], 2020 | Apatinib | Single-center, open-label, phase II trial | RFS and OS | mRFS: 7.6 m |
| 1-year RFS and OS: 36.1%, 93.3% | ||||
| Zhou et al[62], 2022 | Lenvatinib | A multi-center, single-arm, prospective clinical trial | RFS | mRFS: 16.5 m |
| Immunotherapy | ||||
| Kudo et al[65], 2022 | Nivolumab | Multi-center, single-arm clinical trial | 1-year RFS | 1-year RFS: 78.6% |
| Zhang et al[66], 2023 | Anti-PD-1 antibodies include camrelizumab, toripalimab, sintilimab, and pembrolizumab | Retrospective study | OS and RFS | The 1-year, 2-year, 3-year, and 4-year OS rates: 93.1%, 86.8%, 78.2%, and 51.1% |
| The 1-year, 2-year, 3-year, and 4-year RFS rates: 81.7%, 77.0%, 52.3%, and 23.1% | ||||
| Wang et al[67], 2024 | Sintilimab | A multicenter, open-label, randomized, controlled, phase 2 trial. | RFS | mRFS: 27.7 m |
| Xu et al[68], 2023 | Pembrolizumab, tislelizumab, sintilimab, camrelizumab, and toripalimab | A retrospective, multicenter, PSM analysis | RFS and OS | mRFS: 29.6 m mOS: 35.1 m |
| Targeted combination immunotherapy | ||||
| Qin et al[74], 2023 | Atezolizumab, bevacizumab | A randomised, open - label, multicentre, phase 3 trial | RFS | 1-year RFS: 78% |
| Xia et al[75], 2022 | Camrelizumab, apatinib | A single-arm, open label, phase II clinical trial | RFS | 1-year RFS: 53.85% |
| Wang et al[76], 2023 | C + A | Retrospective cohort study | RFS and OS | mPFS: C + A: 14.0 m, C + L: 18.0 m, C + S: 12.0 m |
| C + L | mOS: C + A: 17.0 m, C + L: 19.0 m, C + S: 15.0 m | |||
| C + S | ||||
However, most available evidence comes from small retrospective series. Although high-quality trials that directly demonstrate a survival benefit are still lacking, the existing data suggest that these agents may offer meaningful clinical value as adjuvant therapy for carefully selected high-risk patients.
Immunotherapy, particularly programmed death 1 (PD-1)/programmed death-ligand 1 (PD-L1) inhibitors such as nivo
In a phase 2 study (UMIN000026648), adjuvant nivolumab achieved a 78.6% 1-year RFS rate and a median RFS of 26.3 months in high-risk patients[65]. In a PSM analysis of 46 patients, Zhang et al[66] showed superior outcomes with PD-1 blockade vs standard care: 1 to 4year OS rates were 93.1%/86.8%/78.2%/51.1% vs 85.3%/70.2%/47.7%/30.0% (P < 0.001), and RFS rates were 81.7%/77.0%/52.3%/23.1% vs 68.4%/47.7%/25.8% (P < 0.001).
Collectively, these findings highlight immunotherapy as a potentially transformative option for both advanced and postoperative HCC management, although further validation in large, randomized trials is warranted.
Wang et al[67] conducted a multicenter, randomized phase 2 trial showing that adjuvant sintilimab nearly doubled the median RFS compared with observation (27.7 vs 15.5 months; P = 0.002). In a prospective, PSM analysis, Xu et al[68] reported superior median RFS with immunotherapy (29.6 vs 19.3 months; P = 0.031); improved OS (35.1 vs 27.8 months; P = 0.036); and multivariate analysis confirmed immunotherapy as an independent prognostic factor for RFS (P = 0.015) and OS (P = 0.013).
The heterogeneous clinical efficacy of ICIs is largely attributed to therapeutic resistance. Primary resistance mec
Current evidence indicates that immunotherapy holds promise as an adjuvant strategy for HCC, but most data originate from small retrospective studies. These preliminary findings must be validated in large, multicenter prospective trials to confirm therapeutic efficacy and optimize treatment protocols.
Targeted combination immunotherapy: Current clinical evidence, exemplified by the ORIENT-32[72] and IMbrave150[73] studies, demonstrates that combining targeted therapy with immunotherapy significantly improves RFS and OS in patients with advanced, unresectable HCC. Nevertheless, data on the efficacy of this approach as postoperative adjuvant therapy for HCC patients at high risk of recurrence remain limited. The landmark IMbrave050 study[74] - the first international trial to evaluate postoperative adjuvant targeted immunotherapy in HCC - yielded encouraging findings. In this trial, high-risk patients received either 12 months of adjuvant atezolizumab plus bevacizumab or observation alone. The combination arm achieved a significantly higher 1-year RFS rate (78%) than the control arm (P = 0.012). Although median survival endpoints were not reached because of limited follow-up, IMbrave050 represents the first positive trial of adjuvant targeted immunotherapy in HCC.
Camrelizumab is an antitumor agent developed independently in China. It belongs to the immunoglobulin CD28/B7 superfamily and comprises 288 amino acids. As a type I transmembrane protein, its extracellular segment contains an extracellular domain, a hydrophobic hinge region, and a cytoplasmic tail, together functioning as an immunosuppressive receptor. Xia et al[75] conducted a phase 2 single-arm study evaluating adjuvant apatinib plus camrelizumab in post
Several multicenter RCTs are investigating combination immunotherapy for HCC patients at high risk of recurrence after radical resection: Ongoing studies include durvalumab plus bevacizumab (EMERALD-2, NCT03847428); sintilimab plus bevacizumab (DaDaLi, NCT04682210); camrelizumab plus apatinib (SHR1210-III-325, NCT04639180); and tislelizumab plus sitravatinib (NCT05564338).
TACE combined with immunotherapy: Recent evidence supports the use of combination adjuvant therapies. Huang et al[77] conducted a PSM retrospective analysis of patients with giant HCC treated with either TACE + PD-1 inhibitor or TACE alone. The combination group showed higher RFS at 1 year: 49.9% (combination) vs 24.7% (TACE alone); 2 years: 35.7% vs 15.5% (P < 0.05); OS: 1 year: 83.6% vs 50.6%; 2 years: 66.9% vs 36.8% (P < 0.05). Liang et al[78] retrospectively compared three adjuvant strategies for HCC with MVI: Lenvatinib monotherapy, TACE alone, and TACE plus Lenvatinib - and found that the combination regimen yielded superior 5 years RFS and OS relative to no adjuvant therapy and to either monotherapy. Although current data suggest clinical benefits from integrating local therapy (TACE) with systemic agents (targeted therapy or immunotherapy) after resection, prospective studies are needed to validate these findings and optimize treatment protocols.
Research on postoperative adjuvant chemotherapy for HCC remains limited. Zhu et al[42] evaluated several che
Huaier granule, a fungal extract preparation, has demonstrated clinical activity as either monotherapy or combination therapy in several malignancies, including breast, colon, gastric, and lung cancers; HCC; leukemia; and osteosarcoma[79]. Its active proteoglycan fraction consists of 41.5% polysaccharides, 12.93% amino acids, and 8.72% water. Mechanistically, Huaier granule modulates innate immunity by inducing cytokine release and reactive oxygen species/nitric oxide production and exerts antitumor effects by triggering G0/G1 cell cycle arrest and inhibiting angiogenesis[80-82].
Chen et al[83] conducted the first multicenter, randomized, open-label clinical trial in China to evaluate Sophora granules as adjuvant therapy after HCC resection. Participants mixed 20 g of Sophora granules with 100 mL of water and took the preparation orally three times daily for 2 years. The Sophora group achieved a significantly longer mean RFS (75.5 weeks vs 68.5 weeks, P = 0.0001). OS was also higher (95.19% vs 91.46%, P = 0.0207), and the extrahepatic recurrence rate was lower (8.60% vs 13.61%, P = 0.0018). This trial provides the first clinical evidence that Sophora granules can prolong RFS and reduce extrahepatic recurrence after HCC surgery. Supporting these findings, another study[84] reported that Huachansu (a traditional Chinese medicine) likewise improved RFS and OS following resection. Col
Adoptive immunotherapy (AIT) improves the prognosis of HCC by activating immune responses against tumor cells. Current AIT strategies primarily employ lymphokine-activated killer (LAK) cells and cytokine-induced killer (CIK) cells[85]. These approaches restore cellular immunity and exert antitumor activity. Although AIT is used as an adjuvant therapy after curative treatment for HCC, its clinical efficacy remains controversial.
Evidence on adjuvant LAK therapy is mixed. Kawata et al[86] reported comparable 1-/2-/3-year survival rates (91.7%, 82.9%, and 72.5%, respectively) between LAK-treated patients and controls, concluding that AIT conferred limited postoperative benefit. In contrast, two independent trials demonstrated significant reductions in recurrence and mortality with AIT and documented 100% five-year survival in the treatment groups[87,88]. These studies also found a lower micrometastatic burden in immunotherapy recipients than in controls. A meta-analysis of eight RCTs by Zhao et al[89] showed that AIT significantly decreased 1-/2-/3-year recurrence and mortality rates, although no advantage was seen at five years. Notably, the analysis attributed therapeutic effects mainly to CIK rather than LAK cells.
Two additional investigations confirmed the efficacy of CIK therapy in HCC. In a multicenter phase III trial, Lee et al[90] reported a significantly longer median relapse-free survival in CIK-treated patients than in controls (44.0 months vs 30.0 months; P < 0.05), supporting the role of adjuvant CIK therapy in preventing postoperative recurrence. Similarly, Yu et al[91] prospectively analyzed 132 patients with advanced HCC and observed higher 1-/2-/3-year OS rates in the CIK group than in controls (all P < 0.05), with manageable treatment-related adverse events.
Postoperative adjuvant therapy for HCC remains an active field of investigation, but substantial controversies and challenges persist. To date, no universally accepted regimen reliably prevents recurrence and metastasis, and the optimal strategy is still debated. A primary challenge is accurately identifying patients at high risk for relapse - a group most likely to benefit from adjuvant treatment. Emerging evidence suggests that triple-agent combinations may surpass dual-agent regimens; however, adding additional agents does not automatically translate into superior outcomes. Further studies are required to refine such combinations. Future work should prioritize: (1) Individualizing therapy according to each tumor’s molecular and clinical profile; and (2) Discovering biomarkers that predict treatment response. These ad
| 1. | World Health Organization. The global cancer observatory. [cited 2 April 2025]. Available from: https://gco.iarc.fr/en. |
| 2. | Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, Li L, Wei W, He J. Cancer incidence and mortality in China, 2022. J Natl Cancer Cent. 2024;4:47-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 1162] [Article Influence: 581.0] [Reference Citation Analysis (0)] |
| 3. | Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, Lencioni R, Koike K, Zucman-Rossi J, Finn RS. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7:6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4432] [Cited by in RCA: 4390] [Article Influence: 878.0] [Reference Citation Analysis (4)] |
| 4. | Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, Bonaventure A, Valkov M, Johnson CJ, Estève J, Ogunbiyi OJ, Azevedo E Silva G, Chen WQ, Eser S, Engholm G, Stiller CA, Monnereau A, Woods RR, Visser O, Lim GH, Aitken J, Weir HK, Coleman MP; CONCORD Working Group. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391:1023-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2711] [Cited by in RCA: 3663] [Article Influence: 457.9] [Reference Citation Analysis (1)] |
| 5. | Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2066] [Cited by in RCA: 3349] [Article Influence: 478.4] [Reference Citation Analysis (44)] |
| 6. | Wu F, Wang L, Wu J, Rong W, Tian F, Bi C. [Analysis of risk factors of recurrence in patients with BCLC 0-A hepatocellular carcinoma after surgical resection]. Zhonghua Yi Xue Za Zhi. 2015;95:1747-1750. [PubMed] |
| 7. | Schwartz JD, Schwartz M, Mandeli J, Sung M. Neoadjuvant and adjuvant therapy for resectable hepatocellular carcinoma: review of the randomised clinical trials. Lancet Oncol. 2002;3:593-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 184] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 8. | Alliance of Chinese Expert Consensus on Neoadjuvant Therapy for Hepatocellular Carcinoma; Committee of Digestive Surgery of Chinese Research Hospital Association; Committee of Liver Cancer, Chinese Anti-Cancer Association. [Chinese expert consensus on neoadjuvant therapy for hepatocellular carcinoma (2023 edition)]. Zhonghua Wai Ke Za Zhi. 2023;61:1035-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 9. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines on the management of hepatocellular carcinoma. J Hepatol. 2025;82:315-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 303] [Article Influence: 303.0] [Reference Citation Analysis (6)] |
| 10. | Hasegawa K, Takemura N, Yamashita T, Watadani T, Kaibori M, Kubo S, Shimada M, Nagano H, Hatano E, Aikata H, Iijima H, Ueshima K, Ohkawa K, Genda T, Tsuchiya K, Torimura T, Ikeda M, Furuse J, Akahane M, Kobayashi S, Sakurai H, Takeda A, Murakami T, Motosugi U, Matsuyama Y, Kudo M, Tateishi R; committee for Revision of the Clinical Practice Guidelines for Hepatocellular Carcinoma, Tokyo, Japan. Clinical Practice Guidelines for Hepatocellular Carcinoma: The Japan Society of Hepatology 2021 version (5th JSH-HCC Guidelines). Hepatol Res. 2023;53:383-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 175] [Article Influence: 58.3] [Reference Citation Analysis (0)] |
| 11. | Singal AG, Llovet JM, Yarchoan M, Mehta N, Heimbach JK, Dawson LA, Jou JH, Kulik LM, Agopian VG, Marrero JA, Mendiratta-Lala M, Brown DB, Rilling WS, Goyal L, Wei AC, Taddei TH. AASLD Practice Guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology. 2023;78:1922-1965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 900] [Cited by in RCA: 1114] [Article Influence: 371.3] [Reference Citation Analysis (23)] |
| 12. | Wang MD, Li C, Liang L, Xing H, Sun LY, Quan B, Wu H, Xu XF, Wu MC, Pawlik TM, Lau WY, Shen F, Yang T. Early and Late Recurrence of Hepatitis B Virus-Associated Hepatocellular Carcinoma. Oncologist. 2020;25:e1541-e1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 13. | Portolani N, Coniglio A, Ghidoni S, Giovanelli M, Benetti A, Tiberio GA, Giulini SM. Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg. 2006;243:229-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 706] [Cited by in RCA: 754] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 14. | Wu JC, Huang YH, Chau GY, Su CW, Lai CR, Lee PC, Huo TI, Sheen IJ, Lee SD, Lui WY. Risk factors for early and late recurrence in hepatitis B-related hepatocellular carcinoma. J Hepatol. 2009;51:890-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 368] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 15. | Fukumura D, Kloepper J, Amoozgar Z, Duda DG, Jain RK. Enhancing cancer immunotherapy using antiangiogenics: opportunities and challenges. Nat Rev Clin Oncol. 2018;15:325-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 745] [Cited by in RCA: 1517] [Article Influence: 189.6] [Reference Citation Analysis (0)] |
| 16. | Tsilimigras DI, Bagante F, Moris D, Hyer JM, Sahara K, Paredes AZ, Mehta R, Ratti F, Marques HP, Soubrane O, Lam V, Poultsides GA, Popescu I, Alexandrescu S, Martel G, Workneh A, Guglielmi A, Hugh T, Aldrighetti L, Endo I, Pawlik TM. Recurrence Patterns and Outcomes after Resection of Hepatocellular Carcinoma within and beyond the Barcelona Clinic Liver Cancer Criteria. Ann Surg Oncol. 2020;27:2321-2331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 17. | Nevola R, Ruocco R, Criscuolo L, Villani A, Alfano M, Beccia D, Imbriani S, Claar E, Cozzolino D, Sasso FC, Marrone A, Adinolfi LE, Rinaldi L. Predictors of early and late hepatocellular carcinoma recurrence. World J Gastroenterol. 2023;29:1243-1260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 103] [Cited by in RCA: 156] [Article Influence: 52.0] [Reference Citation Analysis (3)] |
| 18. | Kim JM, Joh JW, Yi NJ, Choi GS, Kim K, Lee KW, Suh KS. Predicting Hepatocellular Carcinoma Recurrence Beyond Milan Criteria After Liver Resection for Solitary Hepatocellular Carcinoma. J Gastrointest Surg. 2020;24:2219-2227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Hong SK, Jin XL, Suh S, Hong SY, Hong K, Han ES, Lee JM, Choi Y, Yi NJ, Lee KW, Suh KS. Different Risk Factors for Early and Late Recurrence After Curative Resection of Hepatocellular Carcinoma. World J Surg. 2022;46:197-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Zhang XY, Ou J, Chen JY, Li WW. Predicting early hepatocellular carcinoma recurrence after resection: A comment for moving forward. J Hepatol. 2019;70:567-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Yao LQ, Chen ZL, Feng ZH, Diao YK, Li C, Sun HY, Zhong JH, Chen TH, Gu WM, Zhou YH, Zhang WG, Wang H, Zeng YY, Wu H, Wang MD, Xu XF, Pawlik TM, Lau WY, Shen F, Yang T. Clinical Features of Recurrence After Hepatic Resection for Early-Stage Hepatocellular Carcinoma and Long-Term Survival Outcomes of Patients with Recurrence: A Multi-institutional Analysis. Ann Surg Oncol. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 22. | Gruttadauria S, Barbera F, Conaldi PG, Pagano D, Liotta R, Gringeri E, Miraglia R, Burgio G, Barbara M, Pietrosi G, Cammà C, Di Francesco F. Clinical and Molecular-Based Approach in the Evaluation of Hepatocellular Carcinoma Recurrence after Radical Liver Resection. Cancers (Basel). 2021;13:518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, Sugawara Y, Minagawa M, Takayama T, Kawasaki S, Makuuchi M. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1061] [Cited by in RCA: 1261] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 24. | Sun HC, Zhang W, Qin LX, Zhang BH, Ye QH, Wang L, Ren N, Zhuang PY, Zhu XD, Fan J, Tang ZY. Positive serum hepatitis B e antigen is associated with higher risk of early recurrence and poorer survival in patients after curative resection of hepatitis B-related hepatocellular carcinoma. J Hepatol. 2007;47:684-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 25. | Li T, Wang SK, Zhou J, Sun HC, Qiu SJ, Ye QH, Wang L, Fan J. Positive HBcAb is associated with higher risk of early recurrence and poorer survival after curative resection of HBV-related HCC. Liver Int. 2016;36:284-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Kim H, Park MS, Park YN, Kim H, Kim KS, Choi JS, Ahn SH, Han KH, Kim MJ, Kim KW. Preoperative radiologic and postoperative pathologic risk factors for early intra-hepatic recurrence in hepatocellular carcinoma patients who underwent curative resection. Yonsei Med J. 2009;50:789-795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Chan AWH, Zhong J, Berhane S, Toyoda H, Cucchetti A, Shi K, Tada T, Chong CCN, Xiang BD, Li LQ, Lai PBS, Mazzaferro V, García-Fiñana M, Kudo M, Kumada T, Roayaie S, Johnson PJ. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol. 2018;69:1284-1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 426] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 28. | Lee S, Kang TW, Song KD, Lee MW, Rhim H, Lim HK, Kim SY, Sinn DH, Kim JM, Kim K, Ha SY. Effect of Microvascular Invasion Risk on Early Recurrence of Hepatocellular Carcinoma After Surgery and Radiofrequency Ablation. Ann Surg. 2021;273:564-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 244] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 29. | Yoo S, Kim JY, Lim YS, Han S, Choi J. Impact of HBsAg seroclearance on late recurrence of hepatitis B virus-related hepatocellular carcinoma after surgical resection. J Hepatol. 2022;77:939-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 33] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 30. | Muñoz-Martínez S, Iserte G, Sanduzzi-Zamparelli M, Llarch N, Reig M. Current pharmacological treatment of hepatocellular carcinoma. Curr Opin Pharmacol. 2021;60:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 31. | Cheng SH, Chen B, Li TX. [Research developments of adjuvant therapies for hepatocellular carcinoma after resection]. Zhonghua Fangshe Zhongliuxue Zazhi. 2019;28:233-237. |
| 32. | Wang Z, Ren Z, Chen Y, Hu J, Yang G, Yu L, Yang X, Huang A, Zhang X, Zhou S, Sun H, Wang Y, Ge N, Xu X, Tang Z, Lau W, Fan J, Wang J, Zhou J. Adjuvant Transarterial Chemoembolization for HBV-Related Hepatocellular Carcinoma After Resection: A Randomized Controlled Study. Clin Cancer Res. 2018;24:2074-2081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 226] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 33. | Wei W, Jian PE, Li SH, Guo ZX, Zhang YF, Ling YH, Lin XJ, Xu L, Shi M, Zheng L, Chen MS, Guo RP. Adjuvant transcatheter arterial chemoembolization after curative resection for hepatocellular carcinoma patients with solitary tumor and microvascular invasion: a randomized clinical trial of efficacy and safety. Cancer Commun (Lond). 2018;38:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 120] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 34. | Hirokawa F, Komeda K, Taniguchi K, Asakuma M, Shimizu T, Inoue Y, Kagota S, Tomioka A, Yamamoto K, Uchiyama K. Is Postoperative Adjuvant Transcatheter Arterial Infusion Therapy Effective for Patients with Hepatocellular Carcinoma who Underwent Hepatectomy? A Prospective Randomized Controlled Trial. Ann Surg Oncol. 2020;27:4143-4152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 35. | Luo L, Shan R, Cui L, Wu Z, Qian J, Tu S, Zhang W, Xiong Y, Lin W, Tang H, Zhang Y, Zhu J, Huang Z, Li Z, Mao S, Li H, Hu Z, Peng P, He K, Li Y, Liu L, Shen W, He Y. Postoperative adjuvant transarterial chemoembolisation improves survival of hepatocellular carcinoma patients with microvascular invasion: A multicenter retrospective cohort. United European Gastroenterol J. 2023;11:228-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Bai S, Yang P, Liu J, Xue H, Xia Y, Liu F, Yang Z, Zhang L, Wu Y, Shen F, Wang K. Surgical Margin Affects the Long-Term Prognosis of Patients With Hepatocellular Carcinoma Undergoing Radical Hepatectomy Followed by Adjuvant TACE. Oncologist. 2023;28:e633-e644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 37. | He J, Chen XM. [Applications and advances of hepatic arterial infusion chemotherapy in surgical treatment of hepatocellular carcinoma]. Zhonghua Gandan Waike Zazhi. 2021;27:390-392. [DOI] [Full Text] |
| 38. | Sindram D, Lau KN, Martinie JB, Iannitti DA. Hepatic tumor ablation. Surg Clin North Am. 2010;90:863-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 39. | Shiina S, Tateishi R, Arano T, Uchino K, Enooku K, Nakagawa H, Asaoka Y, Sato T, Masuzaki R, Kondo Y, Goto T, Yoshida H, Omata M, Koike K. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol. 2012;107:569-77; quiz 578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 484] [Cited by in RCA: 587] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 40. | Francica G, Saviano A, De Sio I, De Matthaeis N, Brunello F, Cantamessa A, Giorgio A, Scognamiglio U, Fornari F, Giangregorio F, Piscaglia F, Gualandi S, Caturelli E, Roselli P, Rapaccini GL, Pompili M. Long-term effectiveness of radiofrequency ablation for solitary small hepatocellular carcinoma: a retrospective analysis of 363 patients. Dig Liver Dis. 2013;45:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 41. | Niemeyer DJ, Simo KA, Iannitti DA, McKillop IH. Ablation therapy for hepatocellular carcinoma: past, present and future perspectives. Hepat Oncol. 2014;1:67-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | Zhu XD, Li KS, Sun HC. Adjuvant therapies after curative treatments for hepatocellular carcinoma: Current status and prospects. Genes Dis. 2020;7:359-369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 43. | Wang L, Qiu L, Ke Q, Ji H, Wu J. Systematic review of adjuvant external beam radiotherapy for hepatocellular carcinoma following radical hepatectomy. Radiother Oncol. 2022;175:101-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 44. | Rangamuwa K, Leong T, Weeden C, Asselin-Labat ML, Bozinovski S, Christie M, John T, Antippa P, Irving L, Steinfort D. Thermal ablation in non-small cell lung cancer: a review of treatment modalities and the evidence for combination with immune checkpoint inhibitors. Transl Lung Cancer Res. 2021;10:2842-2857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 45. | Tong Y, Yang H, Xu X, Ruan J, Liang M, Wu J, Luo B. Effect of a hypoxic microenvironment after radiofrequency ablation on residual hepatocellular cell migration and invasion. Cancer Sci. 2017;108:753-762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 46. | Chen W, Chiang CL, Dawson LA. Efficacy and safety of radiotherapy for primary liver cancer. Chin Clin Oncol. 2021;10:9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 47. | Garcia A, Mathew SO. Racial/Ethnic Disparities and Immunotherapeutic Advances in the Treatment of Hepatocellular Carcinoma. Cancers (Basel). 2024;16:2446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 48. | Su F, Chen K, Liang Z, Qu S, Li L, Chen L, Yang Y, Wu C, Liang X, Zhu X. Survival benefit of higher fraction dose delivered by three-dimensional conformal radiotherapy in hepatocellular carcinoma smaller than 10 cm in size. Cancer Manag Res. 2019;11:3791-3799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 49. | Sun J, Wang Z, Sheng Y, Ming X, Jiang GL, Wang W. Indications of IMRT, PRT and CIRT for HCC from comparisons of dosimetry and normal tissue complication possibility. Strahlenther Onkol. 2022;198:361-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 50. | Wang PM, Hsu WC, Chung NN, Chang FL, Fogliata A, Cozzi L. Radiotherapy with volumetric modulated arc therapy for hepatocellular carcinoma patients ineligible for surgery or ablative treatments. Strahlenther Onkol. 2013;189:301-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 51. | Wahl DR, Stenmark MH, Tao Y, Pollom EL, Caoili EM, Lawrence TS, Schipper MJ, Feng M. Outcomes After Stereotactic Body Radiotherapy or Radiofrequency Ablation for Hepatocellular Carcinoma. J Clin Oncol. 2016;34:452-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 434] [Article Influence: 39.5] [Reference Citation Analysis (0)] |
| 52. | Llovet JM, Montal R, Sia D, Finn RS. Molecular therapies and precision medicine for hepatocellular carcinoma. Nat Rev Clin Oncol. 2018;15:599-616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1487] [Cited by in RCA: 1457] [Article Influence: 182.1] [Reference Citation Analysis (0)] |
| 53. | Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9016] [Cited by in RCA: 10501] [Article Influence: 583.4] [Reference Citation Analysis (9)] |
| 54. | Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S, Kim JS, Luo R, Feng J, Ye S, Yang TS, Xu J, Sun Y, Liang H, Liu J, Wang J, Tak WY, Pan H, Burock K, Zou J, Voliotis D, Guan Z. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2009;10:25-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3854] [Cited by in RCA: 4731] [Article Influence: 262.8] [Reference Citation Analysis (0)] |
| 55. | Bruix J, Qin S, Merle P, Granito A, Huang YH, Bodoky G, Pracht M, Yokosuka O, Rosmorduc O, Breder V, Gerolami R, Masi G, Ross PJ, Song T, Bronowicki JP, Ollivier-Hourmand I, Kudo M, Cheng AL, Llovet JM, Finn RS, LeBerre MA, Baumhauer A, Meinhardt G, Han G; RESORCE Investigators. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2160] [Cited by in RCA: 2822] [Article Influence: 313.6] [Reference Citation Analysis (1)] |
| 56. | Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng AL. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4432] [Cited by in RCA: 4076] [Article Influence: 509.5] [Reference Citation Analysis (5)] |
| 57. | Qin S, Chan SL, Gu S, Bai Y, Ren Z, Lin X, Chen Z, Jia W, Jin Y, Guo Y, Hu X, Meng Z, Liang J, Cheng Y, Xiong J, Ren H, Yang F, Li W, Chen Y, Zeng Y, Sultanbaev A, Pazgan-Simon M, Pisetska M, Melisi D, Ponomarenko D, Osypchuk Y, Sinielnikov I, Yang TS, Liang X, Chen C, Wang L, Cheng AL, Kaseb A, Vogel A; CARES-310 Study Group. Camrelizumab plus rivoceranib versus sorafenib as first-line therapy for unresectable hepatocellular carcinoma (CARES-310): a randomised, open-label, international phase 3 study. Lancet. 2023;402:1133-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 453] [Article Influence: 151.0] [Reference Citation Analysis (2)] |
| 58. | Bruix J, Takayama T, Mazzaferro V, Chau GY, Yang J, Kudo M, Cai J, Poon RT, Han KH, Tak WY, Lee HC, Song T, Roayaie S, Bolondi L, Lee KS, Makuuchi M, Souza F, Berre MA, Meinhardt G, Llovet JM; STORM investigators. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 2015;16:1344-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 558] [Cited by in RCA: 828] [Article Influence: 75.3] [Reference Citation Analysis (0)] |
| 59. | Zhang W, Zhao G, Wei K, Zhang Q, Ma W, Song T, Wu Q, Zhang T, Kong D, Li Q. Adjuvant sorafenib reduced mortality and prolonged overall survival and post-recurrence survival in hepatocellular carcinoma patients after curative resection: a single-center experience. Biosci Trends. 2014;8:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 60. | Bai S, Hu L, Liu J, Sun M, Sun Y, Xue F. Prognostic Nomograms Combined Adjuvant Lenvatinib for Hepatitis B Virus-related Hepatocellular Carcinoma With Microvascular Invasion After Radical Resection. Front Oncol. 2022;12:919824. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 61. | Sun HC, Zhu XD, Zhou J, Gao Q, Shi YH, Ding ZB, Huang C, Qiu SJ, Ren N, Shi GM, Sun J, Ye QH, Huang XW, Yang XR, Fan J. Adjuvant apatinib treatment after resection of hepatocellular carcinoma with portal vein tumor thrombosis: a phase II trial. Ann Transl Med. 2020;8:1301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 62. | Zhou J, Sun H, Huang Z, Liu L, Wen T, Zhu X, Shi Y, Gao Q, Qiu S, Ding Z, Wang Z, Ye Q, Huang X, Huang C, Peng Y, Shi G, Wang X, Fan J. Adjuvant lenvatinib after radical resection in patients with hepatocellular carcinoma (HCC): Preliminary analysis of a prospective, multi-center, single-arm study. J Clin Oncol. 2022;40:e16158-e16158. [RCA] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 63. | Huang Y, Kim BYS, Chan CK, Hahn SM, Weissman IL, Jiang W. Improving immune-vascular crosstalk for cancer immunotherapy. Nat Rev Immunol. 2018;18:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 421] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 64. | Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3297] [Cited by in RCA: 5011] [Article Influence: 385.5] [Reference Citation Analysis (1)] |
| 65. | Kudo M, Ueshima K, Nakahira S, Nishida N, Ida H, Minami Y, Nakai T, Wada H, Kubo S, Ohkawa K, Morishita A, Nomi T, Ishida K, Kobayashi S, Umeda M, Tsurusaki M, Chiba Y, Yoshimura K, Sakai K, Nishio K. Final results of adjuvant nivolumab for hepatocellular carcinoma (HCC) after surgical resection (SR) or radiofrequency ablation (RFA) (NIVOLVE): A phase 2 prospective multicenter single-arm trial and exploratory biomarker analysis. J Clin Oncol. 2022;40:416-416. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 66. | Zhang WQ, Zhang Q, Tan L, Guan ZF, Tian F, Tang HT, He K, Chen WQ. Postoperative adjuvant immunotherapy for high-risk hepatocellular carcinoma patients. Front Oncol. 2023;13:1289916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 67. | Wang K, Xiang YJ, Yu HM, Cheng YQ, Liu ZH, Qin YY, Shi J, Guo WX, Lu CD, Zheng YX, Zhou FG, Yan ML, Zhou HK, Liang C, Zhang F, Wei WJ, Lau WY, Li JJ, Liu YF, Cheng SQ. Adjuvant sintilimab in resected high-risk hepatocellular carcinoma: a randomized, controlled, phase 2 trial. Nat Med. 2024;30:708-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 81] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 68. | Xu X, Wang MD, Xu JH, Fan ZQ, Diao YK, Chen Z, Jia HD, Liu FB, Zeng YY, Wang XM, Wu H, Qiu W, Li C, Pawlik TM, Lau WY, Shen F, Lv GY, Yang T. Adjuvant immunotherapy improves recurrence-free and overall survival following surgical resection for intermediate/advanced hepatocellular carcinoma a multicenter propensity matching analysis. Front Immunol. 2023;14:1322233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 69. | Xu WB, Qi F, Jiao RD, Zheng LZ, Zhang YH, Hou DH, Liu Y, Kang ZJ. Prognostic and clinicopathological value of high expression of TIM‐3 in different cancer types: A meta‐analysis. Precis Med Sci. 2020;9:31-42. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 70. | Lu C, Rong D, Zhang B, Zheng W, Wang X, Chen Z, Tang W. Current perspectives on the immunosuppressive tumor microenvironment in hepatocellular carcinoma: challenges and opportunities. Mol Cancer. 2019;18:130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 318] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 71. | Fu J, Xu D, Liu Z, Shi M, Zhao P, Fu B, Zhang Z, Yang H, Zhang H, Zhou C, Yao J, Jin L, Wang H, Yang Y, Fu YX, Wang FS. Increased regulatory T cells correlate with CD8 T-cell impairment and poor survival in hepatocellular carcinoma patients. Gastroenterology. 2007;132:2328-2339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 598] [Cited by in RCA: 711] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 72. | Ren Z, Xu J, Bai Y, Xu A, Cang S, Du C, Li Q, Lu Y, Chen Y, Guo Y, Chen Z, Liu B, Jia W, Wu J, Wang J, Shao G, Zhang B, Shan Y, Meng Z, Wu J, Gu S, Yang W, Liu C, Shi X, Gao Z, Yin T, Cui J, Huang M, Xing B, Mao Y, Teng G, Qin Y, Wang J, Xia F, Yin G, Yang Y, Chen M, Wang Y, Zhou H, Fan J; ORIENT-32 study group. Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): a randomised, open-label, phase 2-3 study. Lancet Oncol. 2021;22:977-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 765] [Article Influence: 153.0] [Reference Citation Analysis (1)] |
| 73. | Cheng AL, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Lim HY, Kudo M, Breder V, Merle P, Kaseb AO, Li D, Verret W, Ma N, Nicholas A, Wang Y, Li L, Zhu AX, Finn RS. Updated efficacy and safety data from IMbrave150: Atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J Hepatol. 2022;76:862-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 1142] [Article Influence: 285.5] [Reference Citation Analysis (0)] |
| 74. | Qin S, Chen M, Cheng AL, Kaseb AO, Kudo M, Lee HC, Yopp AC, Zhou J, Wang L, Wen X, Heo J, Tak WY, Nakamura S, Numata K, Uguen T, Hsiehchen D, Cha E, Hack SP, Lian Q, Ma N, Spahn JH, Wang Y, Wu C, Chow PKH; IMbrave050 investigators. Atezolizumab plus bevacizumab versus active surveillance in patients with resected or ablated high-risk hepatocellular carcinoma (IMbrave050): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2023;402:1835-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 304] [Article Influence: 101.3] [Reference Citation Analysis (0)] |
| 75. | Xia Y, Tang W, Qian X, Li X, Cheng F, Wang K, Zhang F, Zhang C, Li D, Song J, Zhang H, Zhao J, Yao A, Wu X, Wu C, Ji G, Liu X, Zhu F, Qin L, Xiao X, Deng Z, Kong X, Li S, Yu Y, Xi W, Deng W, Qi C, Liu H, Pu L, Wang P, Wang X. Efficacy and safety of camrelizumab plus apatinib during the perioperative period in resectable hepatocellular carcinoma: a single-arm, open label, phase II clinical trial. J Immunother Cancer. 2022;10:e004656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 151] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 76. | Wang X, Cao W, Qiu Y, Ji H, Yuan J, Wu W, Liu F, Feng L, Ding R, Li X, Tao K. Clinical efficacy and safety evaluation of camrelizumab plus lenvatinib in adjuvant therapy after hepatocellular carcinoma surgery. Front Oncol. 2023;13:1174999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 77. | Huang H, Liao W, Zhang K, Wang H, Cheng Q, Mei B. Adjuvant Transarterial Chemoembolization Plus Immunotherapy for Huge Hepatocellular Carcinoma: A Propensity Score Matching Cohort Study. J Hepatocell Carcinoma. 2024;11:721-735. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 78. | Liang L, Xu ZD, Lu WF, Du CF, Gao ZY, Huang XK, Wang KD, Ye TW, Dai MG, Liu SY, Shen GL, Liu JW, Zhang CW, Huang DS. Survival benefit from adjuvant TACE combined with lenvatinib for patients with hepatocellular carcinoma and microvascular invasion after curative hepatectomy. Asian J Surg. 2024;47:5106-5112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 79. | Song X, Li Y, Zhang H, Yang Q. The anticancer effect of Huaier (Review). Oncol Rep. 2015;34:12-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 80. | Schepetkin IA, Quinn MT. Botanical polysaccharides: macrophage immunomodulation and therapeutic potential. Int Immunopharmacol. 2006;6:317-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 871] [Cited by in RCA: 903] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 81. | Bao H, Liu P, Jiang K, Zhang X, Xie L, Wang Z, Gong P. Huaier polysaccharide induces apoptosis in hepatocellular carcinoma cells through p38 MAPK. Oncol Lett. 2016;12:1058-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 82. | Hu Z, Yang A, Su G, Zhao Y, Wang Y, Chai X, Tu P. Huaier restrains proliferative and invasive potential of human hepatoma SKHEP-1 cells partially through decreased Lamin B1 and elevated NOV. Sci Rep. 2016;6:31298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 83. | Chen Q, Shu C, Laurence AD, Chen Y, Peng BG, Zhen ZJ, Cai JQ, Ding YT, Li LQ, Zhang YB, Zheng QC, Xu GL, Li B, Zhou WP, Cai SW, Wang XY, Wen H, Peng XY, Zhang XW, Dai CL, Bie P, Xing BC, Fu ZR, Liu LX, Mu Y, Zhang L, Zhang QS, Jiang B, Qian HX, Wang YJ, Liu JF, Qin XH, Li Q, Yin P, Zhang ZW, Chen XP. Effect of Huaier granule on recurrence after curative resection of HCC: a multicentre, randomised clinical trial. Gut. 2018;67:2006-2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 171] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 84. | Zhai XF, Liu XL, Shen F, Fan J, Ling CQ. Traditional herbal medicine prevents postoperative recurrence of small hepatocellular carcinoma: A randomized controlled study. Cancer. 2018;124:2161-2168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 85. | Chang HH, Hsieh KY, Yeh CH, Tu YP, Sheu F. Oral administration of an Enoki mushroom protein FVE activates innate and adaptive immunity and induces anti-tumor activity against murine hepatocellular carcinoma. Int Immunopharmacol. 2010;10:239-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 86. | Kawata A, Une Y, Hosokawa M, Wakizaka Y, Namieno T, Uchino J, Kobayashi H. Adjuvant chemoimmunotherapy for hepatocellular carcinoma patients. Adriamycin, interleukin-2, and lymphokine-activated killer cells versus adriamycin alone. Am J Clin Oncol. 1995;18:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 87. | Xie L, Pang R, Jin Y, Xiang S, Li H. [Effects of hepatic artery chemotherapeutic embolization combined with perfusing LAK cells into hepatic artery after radical operation of liver cancer]. Zhonghua Gan Zang Bing Za Zhi. 2000;8:142-143. [PubMed] |
| 88. | Takayama T, Makuuchi M. Prevention of hepatocellular carcinoma recurrence: actuality and perspectives. Hepatogastroenterology. 2002;49:87-90. [PubMed] |
| 89. | Zhao H, Zheng M, Wang K, Wang L, He H, Wang M, Shi Y, Huang S, Ji F, Li X, Zhu H, Wang L, Zhang X, Shi X, Zhao S, Fu B, Wu T. A meta-analysis of adoptive immunotherapy in postoperative hepatocellular carcinoma. J Cancer Res Ther. 2018;14:807-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 90. | Lee JH, Lee JH, Lim YS, Yeon JE, Song TJ, Yu SJ, Gwak GY, Kim KM, Kim YJ, Lee JW, Yoon JH. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology. 2015;148:1383-91.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 401] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 91. | Yu X, Zhao H, Liu L, Cao S, Ren B, Zhang N, An X, Yu J, Li H, Ren X. A randomized phase II study of autologous cytokine-induced killer cells in treatment of hepatocellular carcinoma. J Clin Immunol. 2014;34:194-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |