Published online May 27, 2025. doi: 10.4254/wjh.v17.i5.104646
Revised: March 25, 2025
Accepted: April 22, 2025
Published online: May 27, 2025
Processing time: 148 Days and 13 Hours
It is well known that in case of high initial strictures of bile ducts surgical treatment is associated with a high risk of damage to the hepatoduodenal liga
To compare the long-term outcomes of different surgical treatment options for patients with high-grade benign biliary strictures.
From 2012 to 2022, 193 patients were treated at the A.V. Vishnevsky Surgical Center. All of them had different levels of strictures according to Bismuth-Strasberg classification: Type E1-2 in 32 patients, type E3 - 99, type E4 – 62.123 pa
Long-term results were available for 192 (99%) patients with a follow-up of 4.7 ± 1.6 years after reconstructive surgery; 3.0 ± 1.4 years after percutaneous interventions. Excellent and good results (according to Terblanche classification) were achieved in 35% (42/122) of patients after open reconstructive surgery and in 13% (9/70) of patients after percutaneous transhepatic interventions (P-value < 0.05).
Technically, the most difficult bile duct strictures for reconstructive and percutaneous transhepatic interventions with a high recurrence rate are Bismuth-Strasberg type E4 and E5. The comparative analysis of long-term results of percutaneous and open procedures showed a statistically significant advantage of percutaneous procedures compared to open reconstructive procedures.
Core Tip: Percutaneous transhepatic biliary drainage (PTBD) are an effective and safe way to treat patients with high benign biliary strictures. The first step is to consider PTBD in cases of high benign biliary strictures. Only when minimally invasive procedures are ineffective should reconstructive procedures be considered.
- Citation: Trifonov S, Kovalenko Y, Gurmikov B, Varava A, Vodeiko V, Pakhtushkin E, Vishnevsky V, Zharikov Y. Reconstructive surgery and percutaneous balloon dilation for the treatment of benign biliary strictures: A retrospective study. World J Hepatol 2025; 17(5): 104646
- URL: https://www.wjgnet.com/1948-5182/full/v17/i5/104646.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i5.104646
Currently, the incidence of bile duct injuries is not decreasing. For example, injuries and benign strictures of bile ducts after cholecystectomy occur in 0.1%-0.8% of cases[1-4], after liver resection and transplantation in 4%-32%[5,6], after pancreaticoduodenal resection in 1.2%-27.4%[7]. Considering that the number of cholecystectomies performed in the Russian Federation in 2019 will be about 160 thousand operations[8], the predicted number of injuries will be about a thousand per year.
Nowadays, there are three main methods of treatment for patients with benign strictures of bile ducts: Endoscopic, percutaneous biliary and surgical. A meta-analysis of publications, conducted by a group of Hungarian specialists led by Huszár et al[9], showed no static differences in the long-term results of cicatricial benign stricture treatment by different methods. Surgical interventions were considered successful in 84% of cases, endoscopic interventions in 79%, and percutaneous biliary interventions in 75%. However, it should be noted that all the articles analyzed were retrospective and there was no randomization[9].
It is well known that in the case of high bile duct strictures (at the level of the confluence and above), surgical treatment is associated with a high risk of damage to the hepatoduodenal ligament elements, often involving coarse scarring, and with a significant risk of stricture recurrence (especially in the case of intraparenchymal location of bile duct strictures)[10-12]. Endoscopic management of such strictures is extremely complicated, as the vast majority of these patients have undergone early Roux-en-Y hepatojejunostomy[13,14].
Percutaneous transhepatic biliary drainage (PTBD) of the bile ducts is an alternative to surgical treatment of high benign biliary strictures. This procedure is associated with an insignificant number of usually mild complications according to the Clavien-Dindo classification (up to 10%), proven long-term efficacy (64%-97%); a number of works with observation period of more than 10 years. This method is also effective in intrahepatic (sectoral and segmental) strictures, when traditional resection procedures (such as hepatectomy) are associated with a high risk of complications and mortality. At the same time, this treatment method has a number of disadvantages, primarily related to the need for prolonged drainage, which reduces quality of life, as well as the need for repeated hospitalizations for staged treatment[15-19].
It is likely that all of the above problems will be eliminated or minimized in the future with the introduction of biodegradable stents into widespread clinical practice and the development of accelerated treatment protocols[17,20].
A retrospective analysis of the treatment results of 193 patients with bile duct strictures treated at the A.V. Vishnevsky National Medical Research Center of Surgery from January 2012 to December 2022 was performed. There were 144 (74%) women, 49 (26%) men. The mean age of patients was 52.9 ± 12.2 years. Most of the strictures 175 (90.7%) developed after bile duct injury during cholecystectomy, in 3 patients after severe combined injury, in 10 patients–after liver resection. In another 5 patients, the cause of stricture was unknown.
MR-cholangiopancreatography was the gold standard of diagnosis and was performed in all patients. In the presence of biliary drainage, partial and complete biliary fistula, fistulocholangiography was performed. Computed tomography was performed in cases of suspected vascular injury.
According to Bismuth–Strasberg classification 32 patients with stricture type E1-2, type E3-99, type E4-62 were included in the study. Of the 193 patients who underwent cholecystectomy, 5 (2.5%) had combined damage to vessels and bile ducts. Of these, three patients had damage to the right hepatic artery, one to the left hepatic artery, and one patient had simultaneous damage to the right hepatic artery and portal vein.
Clinical features of the presence of biliary structures were obstructive jaundice with pruritus 16 (8.3%), chronic recurrent cholangitis 44 (22.8%), complete and partial biliary fistula 50 (25.9%). In two patients cholangitis was combined with multiple miliary abscesses of the liver, in 56 (29%) patients there was a combination of these symptoms.
Before admission to A.V. Vishnevskiy NMRC of surgery 92 patients (47.7%) underwent reconstructive interventions on bile ducts; 88 (45.6%) patients underwent hepatojejunostomy, two patients hepaticoduodenostomy. After bile duct injury 58 (30.1%) patients underwent drainage operations (PTBD and laparotomy drainage of bile ducts), four patients underwent reconstructive operations (suturing of bile duct on drainage), four patients endoscopic stenting.
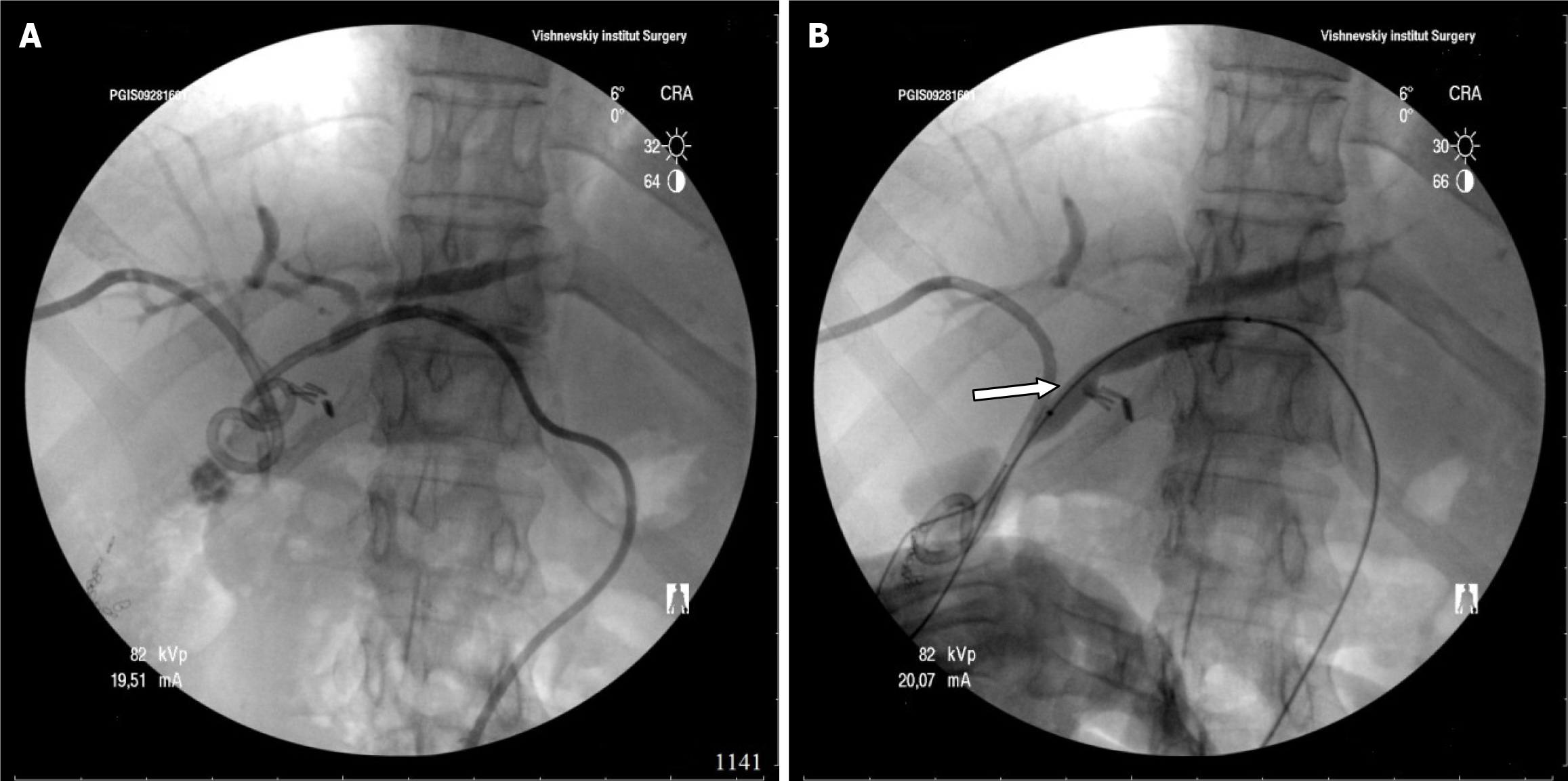
We performed bile duct puncture and drainage under radiologic and ultrasound control. Balloon dilatation of strictures was performed with catheters of 6-10 mm diameter, maximum pressure was 14 atmospheres. The maximum diameter of the drainage was 14 French.
The study complied with the norms of the Declaration of Helsinki and was fully approved by the Local Ethics Committee of the A.V. Vishnevsky National Medical Research Center of Surgery under protocol No. 08-19 on May 6, 2019. All participants gave informed consent prior to the study.
Descriptive statistics were used to compare the characteristics of patients with and without postoperative development of cholangitis and stricture. The following variables were included in this comparison: Age, sex, preoperative procedures. Differences in proportions were evaluated by Pearson's χ2 test. Univariate analyses, including χ2 test and t-tests, were performed to evaluate significant differences between patients who developed cholangitis/stricture and those who did not. Cumulative incidence curves (Kaplan-Meier curve) were calculated to determine the time to diagnosis in patients who developed cholangitis and/or stricture. Patients were censored if they died or were lost to follow-up and did not develop cholangitis and were no longer at risk.
In the first phase, 111 of 193 patients (57.5%) underwent PTBD for resolution of obstructive jaundice and/or treatment of acute cholangitis. The nature of the procedures is shown in Table 1. Technical success of external-internal biliary drainage and balloon dilatation of strictures was achieved in 70 (63.1%) patients (Figure 1). The reason for failure was the presence of complete stricture of the hepaticocholedochal duct or lobular, segmental bile duct in 33 patients, complete stricture of the hepatojejunostomy in 8 patients.
| Procedure | Distribution of strictures according to Bismuth-strasberg type | |||
| Type E2 | Type E3 | Type E 4 | Total | |
| External bile duct drainage | 4 | 12 | 16 | 32 |
| External-internal drainage of bile ducts | 11 | 14 | 30 | 70 |
| Combined bile duct drainage | - | - | 9 | 9 |
Out of 70 patients who underwent PTBD was abandoned in 4 patients because of large multiple cholangiolithiasis. In one patient-because of stricture of hepaticoduodenostomy. Thus, we performed stage percutaneous transhepatic treatment in 70 patients. The duration of biliary tract drainage ranged from 3 to 50 months (median 17.4 months). The number of balloon dilatations ranged from 1 to 12, the median number was 5 procedures.
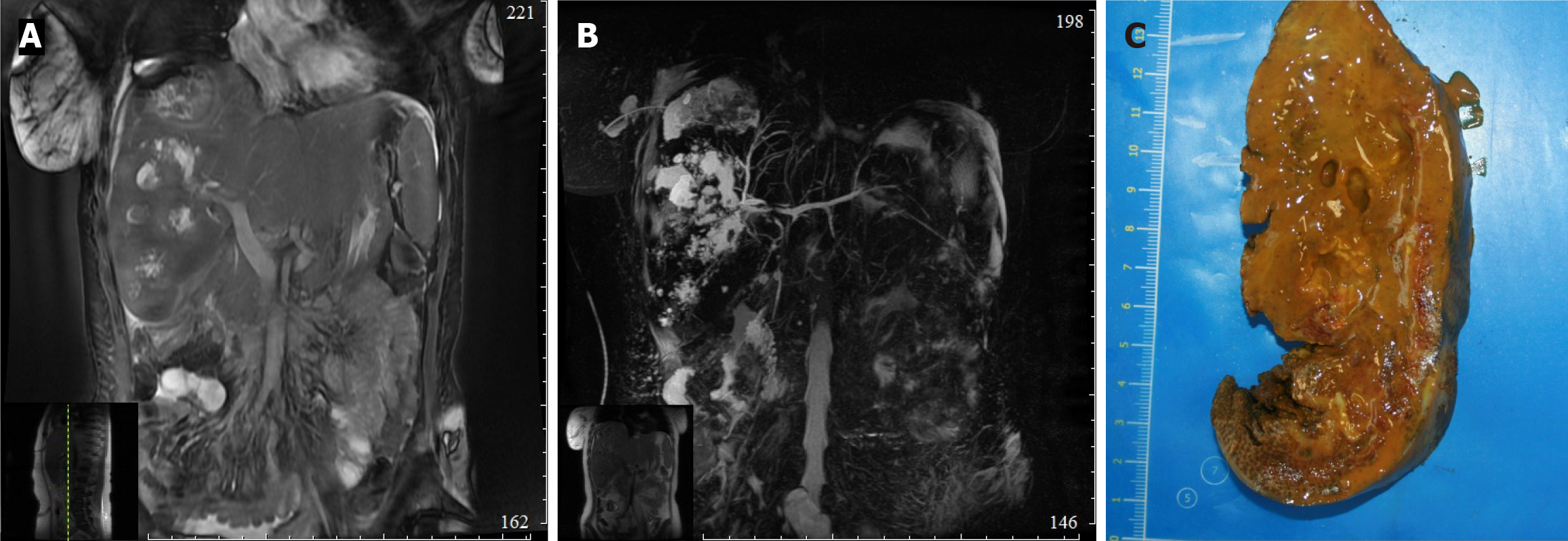
In one patient reconstructive surgery was refused due to severe somatic pathology, therefore combined (external and external-internal) PTBD was performed. Due to stenosis extending to intrahepatic bile ducts, 14 patients underwent hepatojejunostomy combined with liver resection of different volume (right-sided hepatectomy 4, left-sided hepatectomy 3, anatomical resection of II, III liver segments 7). Two out of 14 patients who underwent liver resection had previously diagnosed hepatic artery injury (Figure 2).
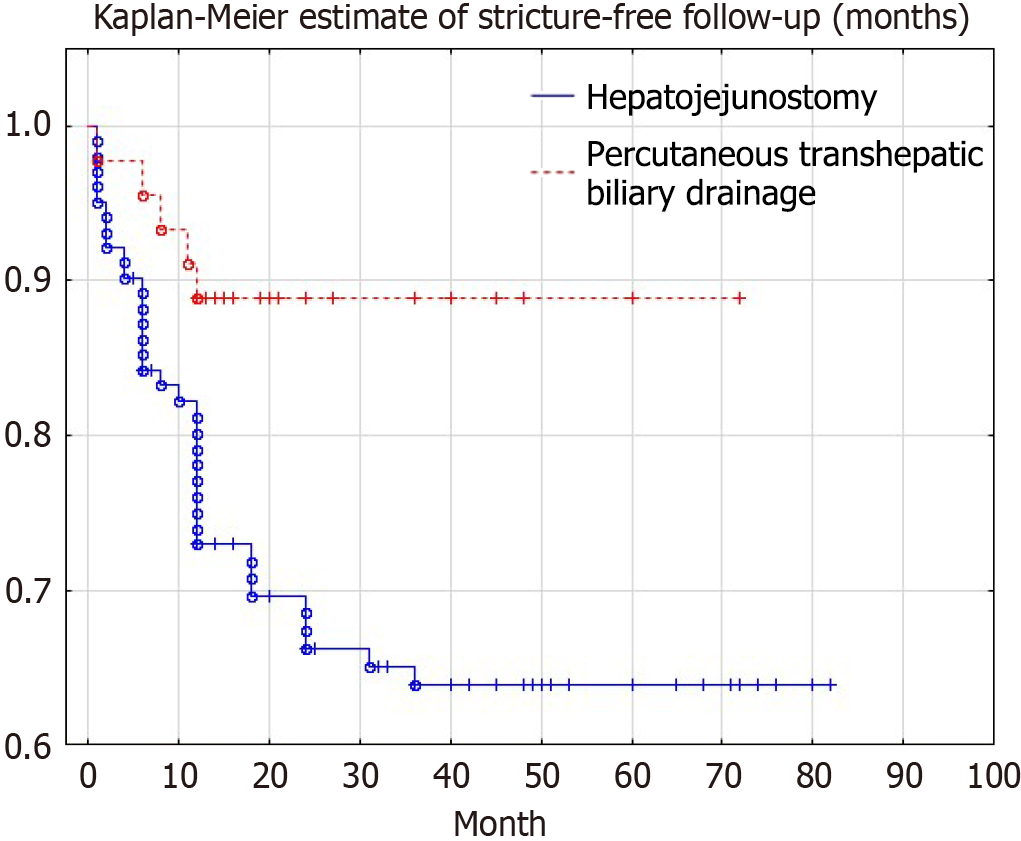
Long-term results were evaluated according to the Terblanche scale. Excellent and good results were defined as no more than 2-3 episodes of chronic cholangitis per year, absence of jaundice and instrumental signs of bile duct stricture (time to stricture according to Kaplan-Meier curve, Figure 3).
Analysis of long-term treatment results showed that in patients after PTBD the number of stricture recurrences was 12.9% (9/70), after hepatojejunostomy 34.4% (42/122) (relative risk 0.373, 95%СI: 0.194-0.721, P-value < 0.05). Long-term results were observed in 192 (99%) patients, with a follow-up of 4.7 ± 1.6 years after reconstructive surgery; 3.0 ± 1.4 years after percutaneous interventions. It should be noted that in 75% of cases, stricture recurrence occurred in the first year after surgery. After stricture recurrence, 35 patients underwent PTBD (32 were successfully treated), three patients underwent liver transplantation for secondary biliary cirrhosis.
An analysis of publications over the last two decades shows a trend towards the use of minimally invasive procedures. Its advantages are undeniable, especially in the treatment of biliary strictures with lobular bile duct separation. Even with excellent long-term results (9.6% restriction in 312 patients) after reconstructive procedures in the article by Mercado et al[21], a significant number of postoperative complications (more than 50%), including bilomas and biliary fistulas (13(4%) and 32(10%), respectively), draw attention[21]. It should be noted that in the article by Mercado et al[21]. It should be noted that we also obtained similar data in our patients 4 (6%) and 9 (14%) patients developed biloma and hepatojejunostomy failure, respectively.
Stilling et al[22] cites data from the Danish registry of patients with bile duct injuries. Thus, after 139 hepatojejunostomy, strictures occurred in 42 (30%) patients. It should be noted that hepatojejunostomy were formed at the earliest time after the injury, and 19% of them were accompanied by vascular wounds. Obviously, this fact explains the significant frequency of recurrences after primary surgery. Reoperations performed in patients with recurrent hepatojejunostomy strictures had significantly better results: 39 out of 42 (93%) were successful, with 19 (45%) patients undergoing re-hepatojejunostomy and 23 (55%) patients undergoing PTBD with balloon dilatation[22]. In addition, the authors do not specify the criteria that guided their choice of intervention.
The experience of our clinic shows that the best results of open reconstructive interventions were observed in E1-2 Bismuth–Strasberg strictures 92% of successful interventions, when it was possible to excise all scar tissue and create the widest possible anastomosis. In contrast, in E3 and E4 Bismuth–Strasberg strictures, only successful interventions were performed, and these were associated with a significant number of complications. Therefore, in our opinion, percutaneous transhepatic interventions are reasonable in this group of patients.
The quality of life of patients after PTBD is reduced, although they can perform physical work, but it does not allow them to return to a full life. Adequate postoperative care of PTBD could help improve the quality of life[23]. Currently, there are no studies comparing the cost-effectiveness of PTBD and reconstructive interventions, as a rule, the choice of treatment method is associated with the availability and experience of specialists in the center. In the conditions of insurance medicine in Russia, a reliable analysis of the treatment of our patients is impossible. Patients in PTBD group had shorter hospital stay and lower initial and total costs than the surgical group. Early complications of PTBD group was significantly lower than surgical group.
Unfortunately, there is currently no uniform approach to PTBD in biliary scar strictures, which makes it difficult to evaluate long-term results and to select the optimal technique. There are also a number of limitations to the application of this treatment option: Multiple cholangiolithiasis, narrow bile ducts, technical impossibility to pass the guidewire behind the stricture[16,18,24]. Reconstructive surgery for E3 and E4 strictures remains the option of choice, but in some cases can only be successful if extensive and sectoral liver resections are performed[15]. An important role in such surgeries is assigned to the resection of the IV-V liver segments, which provides sufficient access to the lobular and sectoral ducts[25,26].
In case of combined damage of hepatic arteries and bile ducts, further treatment tactics depend on the degree of hepatocyte ischemia and bile duct necrosis[12]. The course of such pathological process can have two scenarios: Development of acute sterile necrosis of the liver parenchyma with transition to atrophy of the affected liver segments or, in case of infection-development of multiple abscesses, sepsis. Both conditions are associated with liver failure of varying severity depending on the volume of liver parenchyma affected. The risk of bacterial infection of the necrotic liver is higher in patients who have undergone endoscopic or percutaneous biliary procedures[27,28]. In the presence of widespread infection, resection procedures have been performed, whereas in its absence, only reconstructive procedures have been performed.
PTBD are an effective and safe method of treatment for patients with highly benign biliary strictures. Reconstructive procedures should be performed only when minimally invasive procedures are ineffective. If it is impossible to create adequate bile flow from the affected liver segments, resection procedures should be performed.
The authors would like to thank André Pontes-Silva, a scientist and a highly qualified professional of the Federal University of São Carlos (UFSCar, Brasil), for his scientific assistance.
| 1. | Emeljanov SI, Panchenkov DN, Mamalygina LA, Tokin AN, Chistjakov AA, Khandulaev ShM. Surgical treatment of intraoperative extrahepatic bile duct injuries. Ann HPB Surg. 2005;3:55-61. |
| 2. | Nichitajlo ME, Skums AB, Galochka IP. Injury to the bile duct during laparoscopic cholecystectomy. Ann HPB Surg. 2005;2:30-35. |
| 3. | Nuzzo G, Giuliante F, Giovannini I, Ardito F, D'Acapito F, Vellone M, Murazio M, Capelli G. Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg. 2005;140:986-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 267] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 4. | Gal'perin EI, Chevokin AY. "Fresh" injury to the bile ducts. Hirurgiya. Zhurnal im. N.I. Pirogova. 2010;10:4-10. |
| 5. | Park JK, Yang JI, Lee JK, Park JK, Lee KH, Lee KT, Joh JW, Kwon CHD, Kim JM. Long-term Outcome of Endoscopic Retrograde Biliary Drainage of Biliary Stricture Following Living Donor Liver Transplantation. Gut Liver. 2020;14:125-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (37)] |
| 6. | Bagante F, Ruzzenente A, Beal EW, Campagnaro T, Merath K, Conci S, Akgül O, Alexandrescu S, Marques HP, Lam V, Shen F, Poultsides GA, Soubrane O, Martel G, Iacono C, Guglielmi A, Pawlik TM. Complications after liver surgery: a benchmark analysis. HPB (Oxford). 2019;21:1139-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (37)] |
| 7. | Ito T, Sugiura T, Okamura Y, Yamamoto Y, Ashida R, Aramaki T, Endo M, Matsubayashi H, Ishiwatari H, Uesaka K. Late benign biliary complications after pancreatoduodenectomy. Surgery. 2018;163:1295-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (37)] |
| 8. | Revishvili AS, Oloviannyi VE, Sazhin VP, Anishchenko MM. [Surgical care in the Russian Federation during the pandemic - the main results of 2020]. Khirurgiia (Mosk). 2021;5-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (37)] |
| 9. | Huszár O, Kokas B, Mátrai P, Hegyi P, Pétervári E, Vincze Á, Pár G, Sarlós P, Bajor J, Czimmer J, Mosztbacher D, Márta K, Zsiborás C, Varjú P, Szücs Á. Meta-Analysis of the Long Term Success Rate of Different Interventions in Benign Biliary Strictures. PLoS One. 2017;12:e0169618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Pitt HA, Miyamoto T, Parapatis SK, Tompkins RK, Longmire WP Jr. Factors influencing outcome in patients with postoperative biliary strictures. Am J Surg. 1982;144:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 137] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Blumgart LH, Kelley CJ, Benjamin IS. Benign bile duct stricture following cholecystectomy: critical factors in management. Br J Surg. 1984;71:836-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 110] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Pellegrini CA, Thomas MJ, Way LW. Recurrent biliary stricture. Patterns of recurrence and outcome of surgical therapy. Am J Surg. 1984;147:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 138] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Vitale GC, Tran TC, Davis BR, Vitale M, Vitale D, Larson G. Endoscopic management of postcholecystectomy bile duct strictures. J Am Coll Surg. 2008;206:918-23; discussion 924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Skinner M, Popa D, Neumann H, Wilcox CM, Mönkemüller K. ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy. 2014;46:560-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 161] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 15. | Pekolj J, Yanzón A, Dietrich A, Del Valle G, Ardiles V, de Santibañes E. Major liver resection as definitive treatment in post-cholecystectomy common bile duct injuries. World J Surg. 2015;39:1216-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Kulezneva YV, Melekhina OV, Kurmanseitova LI, Efanov MG, Tsvirkun VV, Alikhanov RB, Patrushev IV. [X-ray surgical treatment of benign biliary anastomotic strictures: Issues for discussion]. Ann HPB Surg. 2017;22:45-54. [DOI] [Full Text] |
| 17. | Lindquester WS, Prologo JD, Krupinski EA, Peters GL. Structured Protocol for Benign Biliary Anastomotic Strictures: Impact on Long-Term Clinical Effectiveness. AJR Am J Roentgenol. 2018;210:447-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Weber A, Rosca B, Neu B, Rösch T, Frimberger E, Born P, Schmid RM, Prinz C. Long-term follow-up of percutaneous transhepatic biliary drainage (PTBD) in patients with benign bilioenterostomy stricture. Endoscopy. 2009;41:323-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Kirkpatrick DL, Hasham H, Collins Z, Johnson P, Lemons S, Shahzada H, Hunt SL, Walter C, Hill J, Fahrbach T. The Utility of a Benign Biliary Stricture Protocol in Preventing Symptomatic Recurrence and Surgical Revision. J Vasc Interv Radiol. 2018;29:688-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (37)] |
| 20. | Mauri G, Michelozzi C, Melchiorre F, Poretti D, Pedicini V, Salvetti M, Criado E, Falcò Fages J, De Gregorio MÁ, Laborda A, Sonfienza LM, Cornalba G, Monfardini L, Panek J, Andrasina T, Gimenez M. Benign biliary strictures refractory to standard bilioplasty treated using polydoxanone biodegradable biliary stents: retrospective multicentric data analysis on 107 patients. Eur Radiol. 2016;26:4057-4063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 21. | Mercado MA, Orozco H, de la Garza L, López-Martínez LM, Contreras A, Guillén-Navarro E. Biliary duct injury: partial segment IV resection for intrahepatic reconstruction of biliary lesions. Arch Surg. 1999;134:1008-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Stilling NM, Fristrup C, Wettergren A, Ugianskis A, Nygaard J, Holte K, Bardram L, Sall M, Mortensen MB. Long-term outcome after early repair of iatrogenic bile duct injury. A national Danish multicentre study. HPB (Oxford). 2015;17:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 23. | Subramani VN, Avudaiappan M, Yadav TD, Kumar H, Sharma V, Mandavdhare H, Gorsi U, Singh H. Outcome Following Percutaneous Transhepatic Biliary Drainage (PTBD) in Carcinoma Gallbladder: a Prospective Observational Study. J Gastrointest Cancer. 2022;53:543-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (37)] |
| 24. | Li C, Wen T. Surgical management of hepatolithiasis: A minireview. Intractable Rare Dis Res. 2017;6:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (37)] |
| 25. | Mercado MA, Domínguez I. Classification and management of bile duct injuries. World J Gastrointest Surg. 2011;3:43-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Strasberg SM, Picus DD, Drebin JA. Results of a new strategy for reconstruction of biliary injuries having an isolated right-sided component. J Gastrointest Surg. 2001;5:266-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 65] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | Kim KM, Park JW, Lee JK, Lee KH, Lee KT, Shim SG. A Comparison of Preoperative Biliary Drainage Methods for Perihilar Cholangiocarcinoma: Endoscopic versus Percutaneous Transhepatic Biliary Drainage. Gut Liver. 2015;9:791-799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 28. | Dilek ON, Atay A. Dealing with hepatic artery traumas: A clinical literature review. World J Clin Cases. 2021;9:8425-8440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (39)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/