Published online Mar 27, 2024. doi: 10.4254/wjh.v16.i3.344
Peer-review started: December 11, 2023
First decision: December 29, 2023
Revised: January 8, 2024
Accepted: March 1, 2024
Article in press: March 1, 2024
Published online: March 27, 2024
Processing time: 107 Days and 5.3 Hours
Succinylation is a highly conserved post-translational modification that is processed via enzymatic and non-enzymatic mechanisms. Succinylation exhibits strong effects on protein stability, enzyme activity, and transcriptional regulation. Protein succinylation is extensively present in the liver, and increasing evidence has demonstrated that succinylation is closely related to hepatic metabolism. For instance, histone acetyltransferase 1 promotes liver glycolysis, and the sirtuin 5-induced desuccinylation is involved in the regulation of the hepatic urea cycle and lipid metabolism. Therefore, the effects of succinylation on hepatic glucose, amino acid, and lipid metabolism under the action of various enzymes will be discussed in this work. In addition, how succinylases regulate the progression of different liver diseases will be reviewed, including the desuccinylation activity of sirtuin 7, which is closely associated with fatty liver disease and hepatitis, and the actions of lysine acetyltransferase 2A and histone acetyltransferase 1 that act as succinyltransferases to regulate the succinylation of target genes that influence the de
Core Tip: Succinylation is the process of transferring succinyl groups through enzymatic and non-enzymatic means using succinyl CoA as a direct substrate. The succinylation degree could be promoted by succinyltransferases (e.g., lysine acetyltransferase 2A, histone acetyltransferase 1, α-ketoglutarate dehydrogenase complex, and carnitine palmitoyltransferase 1A). Desuccinylases including CobB, sirtuin 5, and sirtuin 7 negatively regulate protein succinylation. Several proteins and enzymes in glucose, amino acid, and lipid metabolisms are succinylated in the liver. Succinylation is associated with the progression of several liver diseases. Proteins with varied levels of succinylation may be potential targets for the treatment of fatty liver, hepatitis, and hepatocellular carcinoma.
- Citation: Liu S, Li R, Sun YW, Lin H, Li HF. Protein succinylation, hepatic metabolism, and liver diseases. World J Hepatol 2024; 16(3): 344-352
- URL: https://www.wjgnet.com/1948-5182/full/v16/i3/344.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i3.344
Post-translational modification is an important mechanism that affects protein function, integrating metabolism with physiological and pathological processes. Succinylation is an important post-translational modification of proteins via both enzymatic and non-enzymatic manners[1].
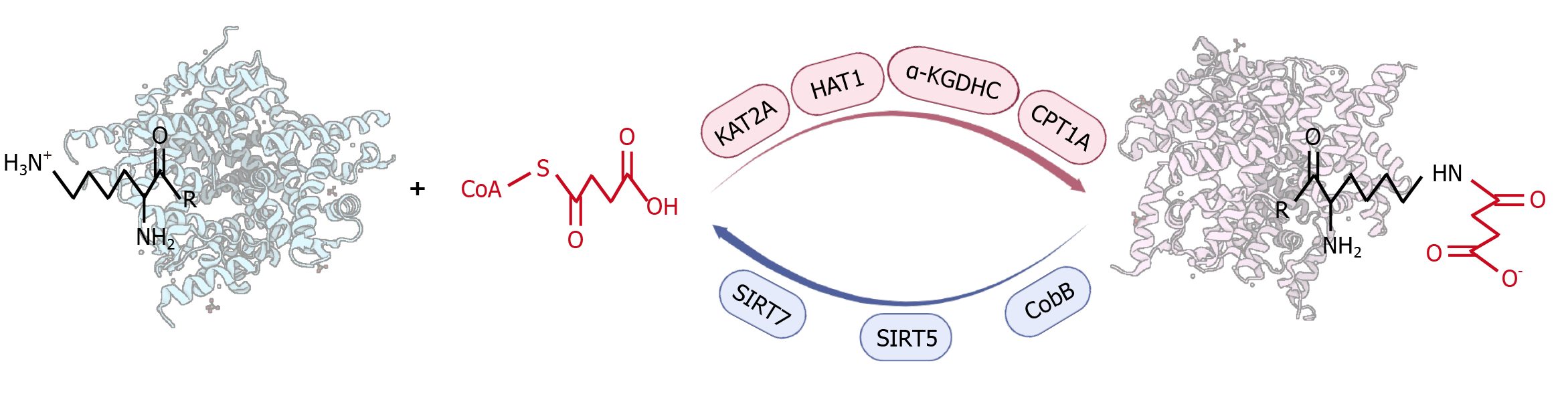
Process of succinyl modification: Succinylation is the process by which a succinyl donor transfers a negatively charged four-carbon succinyl group to the amine of lysine residues by enzymatic or non-enzymatic means[2,3] (Figure 1). The succinyl group binding to the lysine residue has a relatively larger molecular weight (approximately 100.02 Da), which significantly changes the protein structure. Additionally, the charge carried by the lysine residues changes from +1 to -1, resulting in alterations to the physical and chemical properties as well as the functions of the proteins[1-4].
Succinyl modification is widespread in both the cytoplasm and nucleus[5]. In the cytoplasm, succinylation is highly concentrated in mitochondria and may be involved in regulating the tricarboxylic acid cycle, amino acid metabolism, and fatty acid metabolism[6-9]. In the nucleus, lysine succinylation is present in more than one-third of nucleosomes, and the succinylation sites are mainly enriched in the gene promoter region, suggesting that succinylation may be involved in the transcriptional regulation of genes[6,8,9]. Succinylated lysine residues have greater structural changes and charge differences than other typical covalent lysine modification groups such as acetyl and dimethyl[1,5]. Therefore, the influence and mechanism of succinylation on the target proteins and its potential application for the treatment of metabolic diseases have received increasing research attention.
Mechanisms for succinylation: On one hand, succinylation could be processed via non-enzymatic manners, which relies on succinyl-CoA or succinate from mitochondrial and peroxisome sources[4,5,10-14]. Succinylation would occur if provided with sufficient succinyl-CoA[10]. It has been established that mixing succinyl-CoA with albumin or isocitrate dehydrogenase increases succinylation and mitochondrial pH in a pH-dependent and dose-dependent manner[4,5]. Sreedhar et al[11] showed that nicotinamide adenine dinucleotide phosphate-specific isocitrate dehydrogenase mutation results in a 280% increase in cellular succinyl-CoA levels and mitochondrial hyper-succinylation. Succinate dehydrogenase inactivation induces excessive succinylation via increasing the accumulation of succinyl-CoA[12]. Notably, tissues with high levels of succinyl-CoA also show a strong extent of succinyl modification, such as in the heart and liver[13]. Succinate entering the cells could be converted to succinyl-CoA to enhance lysine succinylation[1]. A study has shown that dietary succinate increases the succinylation of intestinal and hepatic proteins with a molecular weight of 25-35 kD in zebrafish[14].
On the other hand, the extent of succinylation could be positively regulated by several enzymes that play succinyl-writer roles (Figure 1)[15-19], even though no specific succinyltransferases have been identified to date. For example, lysine acetyltransferase 2A (KAT2A) was found to be a succinyltransferase[15,16], which can reportedly upregulate H3K79 succinylation and β-catenin stabilization, thereby promoting glycolysis[20]. Zhou et al[21] confirmed that KAT2A promotes the succinylation of K46 and K280 of C-terminal binding protein 1 and mediates the transcription-suppressing activity. In addition, histone acetyltransferase 1 (HAT1) was identified as a succinyltransferase of both histone and non-histone proteins[17,22]. HAT1 mediates the succinylation of histones, and quantitative proteomic analysis revealed five succinylation sites on 45 histones[17]. Research has shown that HAT1 is necessary for the regulation of epigenetic and gene expression by H3K122 succinylation[17].
Wang et al[22] and Yang et al[17] demonstrated that phosphoglycerate mutase 1 (PGAM1), a critical enzyme in glycolysis, is succinylated by HAT1 at K99. The later report also mentioned that aspirin downregulates HAT1 by targeting NF-kappaB to induce PGAM1 K99 desuccinylation, which suppresses the glycolytic process[22]. Furthermore, the α-ketoglutarate dehydrogenase complex (α-KGDHC) regulates succinylation either by regulating succinyl-CoA levels or by directly catalyzing succinylation[4,18]. Inhibition of α-KGDHC reduces succinylation levels of both cytoplasmic matrix and mitochondrial proteins[4]. The E2k subunit of α-KGDHC was demonstrated to be essential for its trans-succinylase activity. The absence of the E2k subunit reduces succinylation, while the presence of alpha-ketoglutaric acid increases succinylation[4].
Another lysine succinyltransferase in mammalian cells is carnitine palmitoyltransferase 1A (CPT1A)[19]. Kurmi et al[19] demonstrated that CPT1A can play the role of a succinyltransferase both in vivo and in vitro to regulate substrate proteins and related metabolic processes. Wang et al[23] discovered that CPT1A-mediated succinylation of S100A10 (a protein that is overexpressed in gastric cancer) increases human gastric cancer invasion. Moreover, CPT1A promotes the succinylation of mitochondrial fission factor at K302 and enhances the development of ovarian cancer[24].
In addition, significant progress has been made in the exploration of desuccinylases that negatively regulate succinylation (Figure 1). CobB was the first desuccinylase discovered in prokaryotes with both deacetylation and desuccinylation activities[25]. A high-performance liquid chromatography assay showed that CobB could deacetylate and desuccinylate a histone H3K9 peptide with similar efficiency, whereas the desuccinylation activity of CobB might be induced when cells are treated with succinate[25].
Sirtuin 5 (SIRT5) and sirtuin 7 (SIRT7) are currently known as important desuccinylases in eukaryotes[26-32]. SIRT5 acts in all cell compartments. The activity of SIRT5 is dependent on NAD+, which is influenced by the availability of NAD+ (substrate) and the amount of nicotinamide (product)[26]. In SIRT5 knockouts, more than 80% of proteins are succinylated in the tricarboxylic acid cycle to enhance cell respiration, and 60% of proteins in fatty acid metabolism are succinylated[27]. At least 2565 succinylation sites on 779 proteins in mammalian fibroblasts and liver tissues were found to be regulated by SIRT5[27]. Novel targets for SIRT5 in regulating the mitochondrial lysine succinylome such as uncoupling protein 1 in mouse brown adipose tissue were recently identified[28,29].
SIRT7 is a member of the sirtuin family proteins that are described as NAD (+)-dependent class III histone deacetylases[30,31]. Research indicated that SIRT7 catalyzed the desuccinylation of H3K122, which promoted chromatin condensation and DNA double-strand break repair[30]. Yu et al[31] showed that SIRT7 restricted chronic hepatitis B virus (HBV) transcription and replication through catalyzing desuccinylation of H3K122 that is associated with covalently closed circular (ccc) DNA minichromosome. SIRT7 mediates the desuccinylation of arginine methyltransferase 5 (PRMT5) K387, which is involved in lipid reprogramming, tumor growth, and metastasis[32].
Collectively, succinylation is the process of transferring negatively charged four-carbon succinyl groups to amines of lysine residues through enzymatic and non-enzymatic manners using succinyl-CoA as a direct substrate. The succinylation degree could be promoted by succinyltransferases, such as KAT2A, HAT1, α-KGDHC, and CPT1A. Meanwhile, desuccinylases, including CobB, SIRT5, and SIRT7 negatively regulate the extent of protein succinylation. To date, the characterization of succinyltransferases and desuccinylases, their target specificity, the function of succinylation, and their clinical application still need to be further investigated, given their significance for proteomic analysis.
The liver is a crucial metabolic organ through which major metabolic processes including glucose, amino acid, and lipid metabolisms occur[33]. The overall abundance of lysine succinylation in the liver is higher relative to other tissues, with proteins and enzymes in several metabolic pathways being succinylated[34].
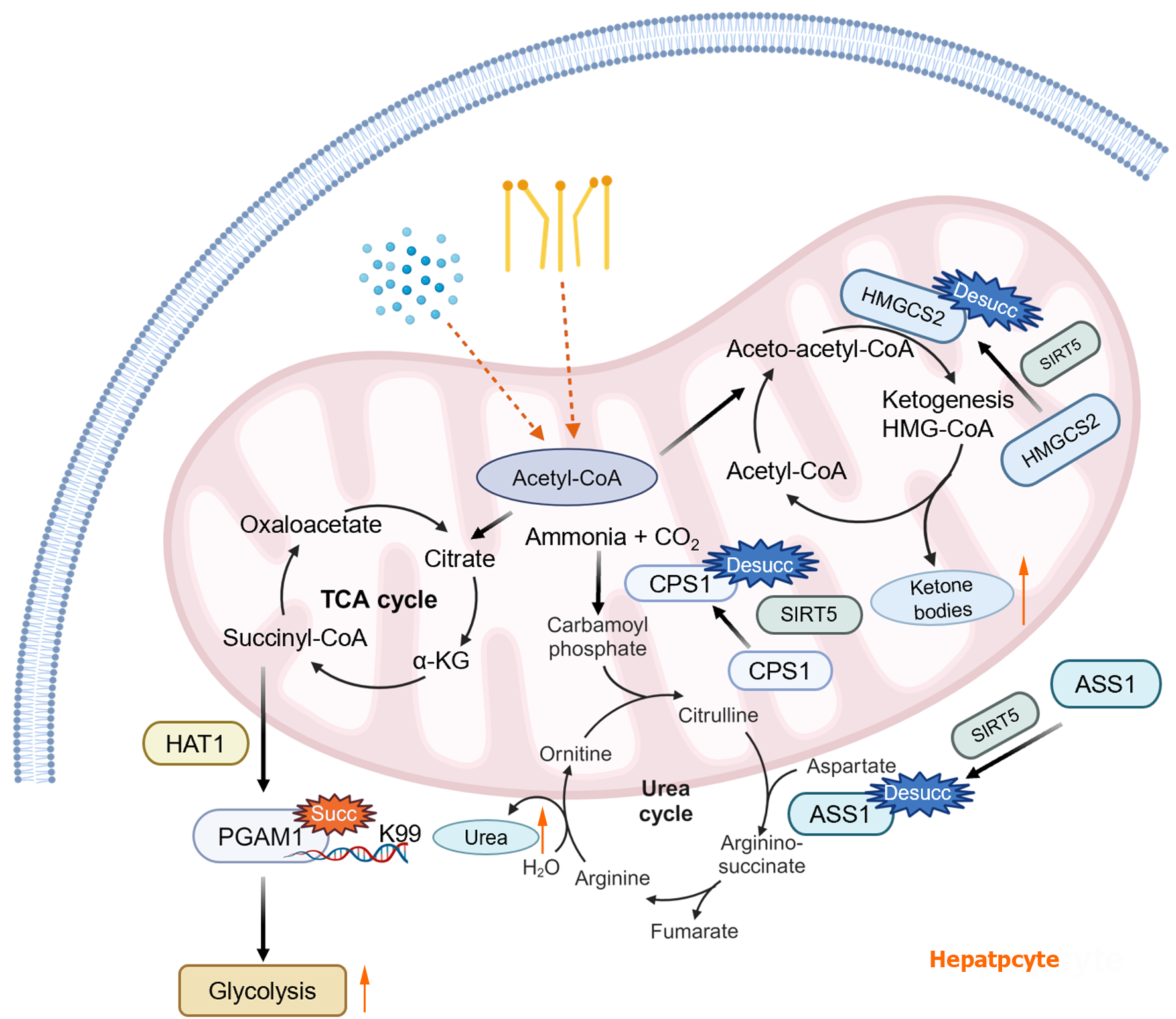
Influence of protein succinylation on glucose and amino acid metabolism: Glucose homeostasis is largely regulated by hepatic glycogen synthesis, gluconeogenesis, and glycolysis[35,36]. Enhancement of glycolysis contributes to the growth of tumor cells. Yang et al[17] performed a Kyoto Encyclopedia of Genes and Genomes pathway enrichment analysis on HAT1-targeted non-histone proteins and found that HAT1 mediates the succinylation of glycolytic-related proteins, including seven key enzymes including GPI, TPI, GAPDH, PGK, PGAM, enolase, and PKM. The authors further demonstrated that the HAT1-induced K99 succinylation of PGAM1 increased its activity, which further promoted tumorigenesis[17]. Wang et al[22] showed that aspirin reduced HAT1 expression, which decreased the K99 succinylation level of PGAM1, thereby restricting PGAM1 activity and inhibiting glycolysis in liver cancer (Figure 2).
The liver is also a major tissue for the conversion of ammonia[37], which is a toxic metabolite derived from amino acid metabolism under physiological conditions[38]. For the conversion of ammonia to non-toxic urea via the urea cycle, carbamoyl phosphate synthase 1 (CPS1) is the first enzyme that is highly abundant in mitochondria, and it is expressed mainly in hepatocytes[39]. Polletta et al[40] demonstrated that mitochondrial SIRT5 not only promotes ammonia detoxification by catalyzing desuccinylation of CPS1, but it also regulates glutamine homeostasis and ammonia levels by inhibiting glutaminase activity to reduce ammonia release and the conversion of glutamine to glutamate (Figure 2). Additionally, Zhang et al[41] conducted stoichiometry of lysine succinylation in mouse liver and found several highly succinylated lysine sites in arginine succinate synthetase (ASS1-a key enzyme in the urea cycle), which were regulated by SIRT5. Metabolomic analysis confirmed that SIRT5 deficiency reduced liver urea cycle activity, and more importantly, SIRT5 deficiency affected ammonia tolerance.
Influence of protein succinylation on lipid metabolism: The liver serves as an important regulator of lipid homeostasis[42], which includes lipid uptake, lipogenesis, fatty acid oxidation, ketogenesis, and lipid secretion[43]. When lipid synthesis exceeds lipolysis or export, it causes the accumulation of lipids in hepatocytes, ultimately leading to hepatic steatosis[32,44]. PRMT5 is a type II arginine methyltransferase that affects a variety of metabolites including phospholipids, fatty acids, and steroid hormones. Yuan et al[32] demonstrated that SIRT7-mediated desuccinylation of PRMT5 at K387 increases its methyltransferase activity, thereby upregulating lipid metabolism-related factors, such as sterol-regulatory element binding protein 1a (SREBP1a), FASN, ACACA, PPARγ, SCD, etc. Moreover, SIRT5 is also involved in the regulation of fatty acid β-oxidation[45]. When SIRT5 is deficient, fatty acid β-oxidation is reduced, which leads to fat accumulation in the liver[13].
Ketone bodies, which are comprised of acetoacetic acid, β-hydroxybutyrate, and acetone[46], are produced by the liver through fatty acid catabolism during glucose deficiency[47,48]. Mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthetase 2 (HMGCS2) is a key enzyme required for ketogenic biosynthesis, which is regulated by succinylation[49]. Early studies on ketogenic regulation have shown that the accumulation of succinyl-CoA is the main process leading to enzyme inactivation in the liver. It was reported that glucagon drastically reduced succinyl-CoA levels and HMGCS2 succinylation, which led to strong ketogenic activation[4]. SIRT5 induces desuccinylation of HMGCS2 and promotes ketone body formation (Figure 2). Among the 15 succinylated lysine residues identified on HMGCS2, several sites appear to be highly targeted by SIRT5 including K83, K310, K350, K354, and K358[50]. Studies have shown that lysine adjacent to the HMGCS2 substrate binding site was strongly succinylated, suggesting that succinyl-CoA may interact with lysine residues around the catalytic pocket, resulting in non-enzymatic modification of these lysines[51,52].
At present, the discovery that various enzymes involved in liver glucose, amino acid, and lipid metabolisms were regulated by succinylation is only the tip of the iceberg, and whether other enzymes in the liver are modulated by succinylation remains to be ascertained.
Influence of succinylation on hepatic glucose metabolism: Under the stimulation of succinyl-CoA, HAT1 causes the K99 site of PGAM1 to be succinylated and promotes its enzyme activity, thus promoting glycolysis. The influence of succinylation on hepatic amino acid metabolism is shown by SIRT5 promotion of urea production by regulating the desuccinylation of ASS1 and CPS1. The influence of succinylation on hepatic lipid metabolism is shown by SIRT5-induced desuccinylation of HMGCS2 that promotes ketone body formation.
Several studies have established that succinylation is strongly associated with the progression of liver diseases, primarily for fatty liver disease, hepatitis, and hepatocellular carcinoma (HCC). Succinylation not only regulates fat deposition and thus fatty liver degeneration[45,53], but it also promotes HBV transcription and replication[31]. In addition, succinylation stimulates immune escape and tumor growth in HCC[54]. Therefore, the specific roles of succinylation in liver diseases are discussed herein.
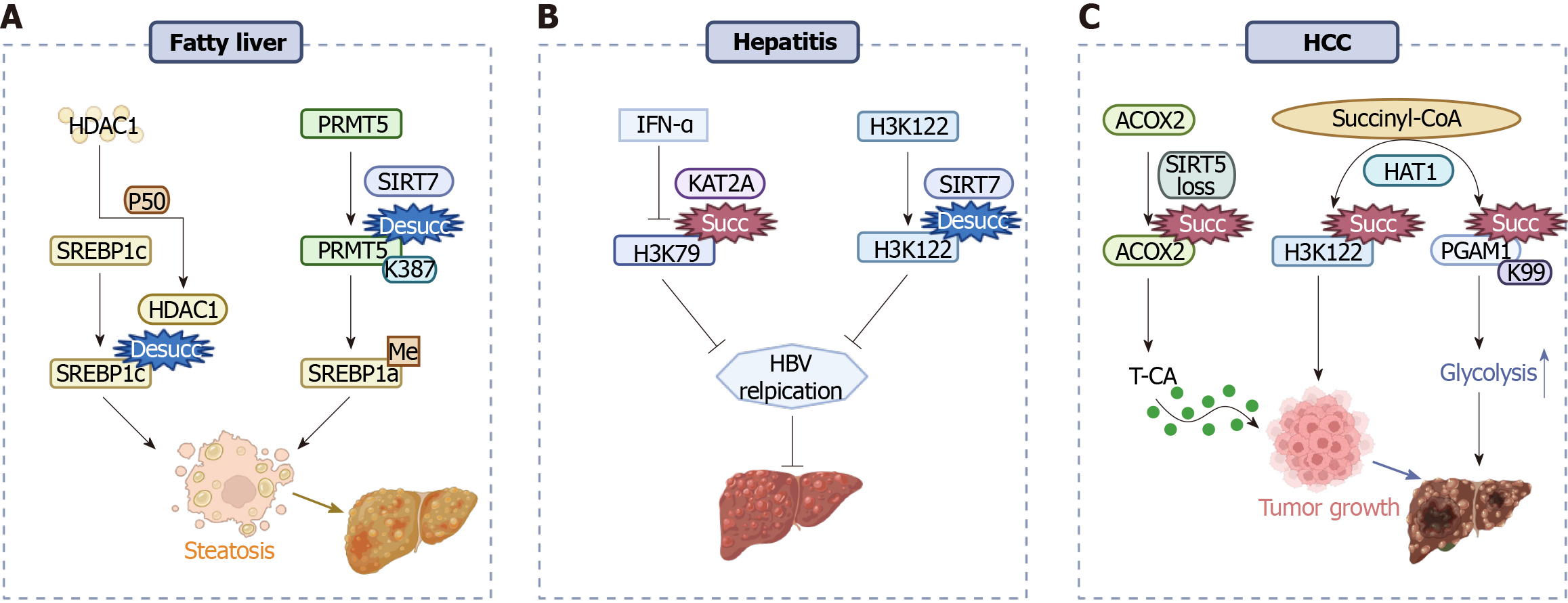
Succinylation is involved in fatty liver disease: Fatty liver, which is caused initially by excessive fat accumulation in the liver, is a common chronic disease with a high prevalence worldwide[55,56]. As one of the metabolism-related post-translational modifications, the succinylation degree is enhanced in fatty liver samples[45,57]. Cheng et al[57] conducted quantitative succinylated proteome analysis using the livers of nonalcoholic fatty liver disease (NAFLD) rat models and identified 178 differentially succinylated proteins, which were involved in various metabolic and cellular processes and could promote the progression of NAFLD to varying degrees. Another study[45] also indicated that overexpression of SIRT5 in the liver resulted in decreased succinylation, enhanced fatty acid oxidation, and attenuated fatty liver degen
Succinylation promotes hepatitis virus replication: Viral hepatitis is an infectious disease threatening human health, with a growing number of incidences in recent years[59]. HBV is a hepatotropic DNA virus that encodes multiple gene products for viral replication[60-62]. cccDNA plays an important role as a template for HBV transcription[63]. In the nucleus of HBV-infected cells, SIRT7 catalyzes the desuccinylation of cccDNA-bound histone H3K122, thereby limiting HBV transcription and replication[31]. KAT2A is identified as an important host factor for HBV replication[16]. Wang et al[15] confirmed that KAT2A is coupled to nuclear α-KGDHC, which acts as a histone H3 succinyltransferase. Later research[64] found that KAT2A can bind to cccDNA by interacting with the HBV core protein and catalyzing the succinylation of H3K79 on cccDNA (Figure 3B), thus promoting cccDNA transcription. Interestingly, Yuan et al[65] discovered that IFN-α restrains HBV cccDNA by downregulating KAT2A-mediated histone H3K79 succinylation. Collectively, targeting succinyl-modification enzymes and the succinylated proteins may provide new perspectives for the treatment of HBV.
Succinylation degree is associated with the progression of HCC: HCC is a common and highly lethal cancer, which ranks fourth in cancer incidence and second in cancer mortality[66,67]. In liver cancer patients, the expression of SIRT7 is significantly higher than that in normal liver tissues, and this initially increases at the first and middle stages of HCC but tends to decrease at the later stages[68]. Moreover, deficiency of SIRT5 promotes HCC and is associated with oxidative damage response[54]. Sun et al[54] showed that SIRT5 depletion led to increased lysine succinylation of acyl-CoA oxidase 2 (ACOX2) (Figure 3C), resulting in the synthesis of primary bile acids, which further promoted immune escape and tumor growth in HCC. In addition, Yang et al[17] confirmed that HAT1 promoted cell proliferation in HCC by catalyzing H3K122 succinylation (Figure 3C). Aspirin inhibits the succinylation level of PGAM1 at K99 by downregulating the expression of HAT1 and decreasing the level of glucose consumption and lactic acid production in liver cancer cells, thereby attenuating the glycolytic pathway in HCC[22,69]. In view of the complex roles of the succinylation signaling pathway in HCC, further studies are necessary to distinguish the pleiotropic effects of succinylation for its application in treating liver cancers.
Through delineating the pleiotropic relationships between succinylation and hepatic metabolism, protein succinylation is involved in various physiological and pathological processes in the liver. Despite the significant progress in understanding this kind of post-translational modification, many issues remain unresolved, providing opportunities for future studies.
Succinylation is site-specific, and some proteins have several succinylation sites to make the substrate perform varied biological functions. Research has found that the 252 identified succinylated proteins have 1190 SuK sites and a total of 6579 lysines, with at least 18% of lysines on these proteins being modified by succinylation[49]. Whether these lysine succinylation sites overlap with known enzyme active sites may be an important sign to examine the function of succinylation regulation. Therefore, further research on the exact influences and mechanisms for succinylation on different proteins and/or different lysine sites of one target protein is of great importance.
Some specific succinylases regulate glycolysis and amino acid and lipid metabolisms by modifying the succinylation degree of critical enzymes. Are there other succinylases that are crucial for hepatic metabolism? Histone deacetylase 1 maintains SREBP1c activity through desuccinylation and promotes hepatic steatosis[53]. Similarly, some succinylation-modifying enzymes also exert other enzymatic activities. For instance, the demalonylation activity of SIRT5[27] and the acetylation activity of KAT2A are likely to contribute to regulating the biological processes of the liver. This suggests that some enzymes with other functions can also exert succinylation or desuccinylation activity, and some identified succi
In addition, succinylation-regulated metabolic processes could affect the progression of fatty liver, hepatitis, and HCC. In some cases, the effect of succinylation on disease development may not be common between histone and non-histone proteins. For instance, Yuan et al[32] verified that SIRT7-mediated desuccinylation of PRMT5 at K387 promoted fatty liver. Meanwhile, SIRT7 catalyzes the desuccinylation of cccDNA-bound histone H3K122, thereby limiting HBV transcription and replication[16]. This indicates that the roles of succinyltransferase/desuccinylase are not consistent with different metabolic environments or reactions. Therefore, we ask that the following scientific questions be resolved. What are the differences in succinylation levels and regulatory mechanisms during the occurrence and development of various metabolic diseases at different stages? How can we modulate more succinylation-related pathways in target tissues to improve human health?
In conclusion, the in-depth study of these issues would greatly enhance our understanding of protein succinylation, which further supports the theoretical basis for the treatment of metabolic diseases and the development of related drugs.
| 1. | Zhang Z, Tan M, Xie Z, Dai L, Chen Y, Zhao Y. Identification of lysine succinylation as a new post-translational modification. Nat Chem Biol. 2011;7:58-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 775] [Cited by in RCA: 804] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 2. | Hirschey MD, Zhao Y. Metabolic Regulation by Lysine Malonylation, Succinylation, and Glutarylation. Mol Cell Proteomics. 2015;14:2308-2315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 346] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 3. | Yang Y, Gibson GE. Succinylation Links Metabolism to Protein Functions. Neurochem Res. 2019;44:2346-2359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 166] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 4. | Gibson GE, Xu H, Chen HL, Chen W, Denton TT, Zhang S. Alpha-ketoglutarate dehydrogenase complex-dependent succinylation of proteins in neurons and neuronal cell lines. J Neurochem. 2015;134:86-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 114] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 5. | Weinert BT, Schölz C, Wagner SA, Iesmantavicius V, Su D, Daniel JA, Choudhary C. Lysine succinylation is a frequently occurring modification in prokaryotes and eukaryotes and extensively overlaps with acetylation. Cell Rep. 2013;4:842-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 484] [Cited by in RCA: 632] [Article Influence: 48.6] [Reference Citation Analysis (0)] |
| 6. | Smestad J, Erber L, Chen Y, Maher LJ 3rd. Chromatin Succinylation Correlates with Active Gene Expression and Is Perturbed by Defective TCA Cycle Metabolism. iScience. 2018;2:63-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 118] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 7. | Papanicolaou KN, O'Rourke B, Foster DB. Metabolism leaves its mark on the powerhouse: recent progress in post-translational modifications of lysine in mitochondria. Front Physiol. 2014;5:301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Kumar S, Lombard DB. Generation and Purification of Catalytically Active Recombinant Sirtuin5 (SIRT5) Protein. Methods Mol Biol. 2016;1436:241-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Chinopoulos C. The Mystery of Extramitochondrial Proteins Lysine Succinylation. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (2)] |
| 10. | Bharathi SS, Zhang Y, Gong Z, Muzumdar R, Goetzman ES. Role of mitochondrial acyl-CoA dehydrogenases in the metabolism of dicarboxylic fatty acids. Biochem Biophys Res Commun. 2020;527:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Sreedhar A, Wiese EK, Hitosugi T. Enzymatic and metabolic regulation of lysine succinylation. Genes Dis. 2020;7:166-171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 12. | Li F, He X, Ye D, Lin Y, Yu H, Yao C, Huang L, Zhang J, Wang F, Xu S, Wu X, Liu L, Yang C, Shi J, Liu J, Qu Y, Guo F, Zhao J, Xu W, Zhao S. NADP(+)-IDH Mutations Promote Hypersuccinylation that Impairs Mitochondria Respiration and Induces Apoptosis Resistance. Mol Cell. 2015;60:661-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 193] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 13. | Sadhukhan S, Liu X, Ryu D, Nelson OD, Stupinski JA, Li Z, Chen W, Zhang S, Weiss RS, Locasale JW, Auwerx J, Lin H. Metabolomics-assisted proteomics identifies succinylation and SIRT5 as important regulators of cardiac function. Proc Natl Acad Sci U S A. 2016;113:4320-4325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 295] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 14. | Ding Q, Lu C, Hao Q, Zhang Q, Yang Y, Olsen RE, Ringo E, Ran C, Zhang Z, Zhou Z. Dietary Succinate Impacts the Nutritional Metabolism, Protein Succinylation and Gut Microbiota of Zebrafish. Front Nutr. 2022;9:894278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 15. | Wang Y, Guo YR, Liu K, Yin Z, Liu R, Xia Y, Tan L, Yang P, Lee JH, Li XJ, Hawke D, Zheng Y, Qian X, Lyu J, He J, Xing D, Tao YJ, Lu Z. KAT2A coupled with the α-KGDH complex acts as a histone H3 succinyltransferase. Nature. 2017;552:273-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 419] [Article Influence: 46.6] [Reference Citation Analysis (0)] |
| 16. | Wang Y, Guo YR, Xing D, Tao YJ, Lu Z. Supramolecular assembly of KAT2A with succinyl-CoA for histone succinylation. Cell Discov. 2018;4:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 17. | Yang G, Yuan Y, Yuan H, Wang J, Yun H, Geng Y, Zhao M, Li L, Weng Y, Liu Z, Feng J, Bu Y, Liu L, Wang B, Zhang X. Histone acetyltransferase 1 is a succinyltransferase for histones and non-histones and promotes tumorigenesis. EMBO Rep. 2021;22:e50967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 124] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 18. | Dobolyi A, Bago A, Palkovits M, Nemeria NS, Jordan F, Doczi J, Ambrus A, Adam-Vizi V, Chinopoulos C. Exclusive neuronal detection of KGDHC-specific subunits in the adult human brain cortex despite pancellular protein lysine succinylation. Brain Struct Funct. 2020;225:639-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Kurmi K, Hitosugi S, Wiese EK, Boakye-Agyeman F, Gonsalves WI, Lou Z, Karnitz LM, Goetz MP, Hitosugi T. Carnitine Palmitoyltransferase 1A Has a Lysine Succinyltransferase Activity. Cell Rep. 2018;22:1365-1373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 136] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 20. | Tong Y, Guo D, Yan D, Ma C, Shao F, Wang Y, Luo S, Lin L, Tao J, Jiang Y, Lu Z, Xing D. KAT2A succinyltransferase activity-mediated 14-3-3ζ upregulation promotes β-catenin stabilization-dependent glycolysis and proliferation of pancreatic carcinoma cells. Cancer Lett. 2020;469:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 84] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 21. | Zhou J, Yan X, Liu Y, Yang J. Succinylation of CTBP1 mediated by KAT2A suppresses its inhibitory activity on the transcription of CDH1 to promote the progression of prostate cancer. Biochem Biophys Res Commun. 2023;650:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 22. | Wang YF, Zhao LN, Geng Y, Yuan HF, Hou CY, Zhang HH, Yang G, Zhang XD. Aspirin modulates succinylation of PGAM1K99 to restrict the glycolysis through NF-κB/HAT1/PGAM1 signaling in liver cancer. Acta Pharmacol Sin. 2023;44:211-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 23. | Wang C, Zhang C, Li X, Shen J, Xu Y, Shi H, Mu X, Pan J, Zhao T, Li M, Geng B, Xu C, Wen H, You Q. CPT1A-mediated succinylation of S100A10 increases human gastric cancer invasion. J Cell Mol Med. 2019;23:293-305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 24. | Zhu Y, Wang Y, Li Y, Li Z, Kong W, Zhao X, Chen S, Yan L, Wang L, Tong Y, Shao H. Carnitine palmitoyltransferase 1A promotes mitochondrial fission by enhancing MFF succinylation in ovarian cancer. Commun Biol. 2023;6:618. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 25. | Colak G, Xie Z, Zhu AY, Dai L, Lu Z, Zhang Y, Wan X, Chen Y, Cha YH, Lin H, Zhao Y, Tan M. Identification of lysine succinylation substrates and the succinylation regulatory enzyme CobB in Escherichia coli. Mol Cell Proteomics. 2013;12:3509-3520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 226] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 26. | Buler M, Aatsinki SM, Izzi V, Uusimaa J, Hakkola J. SIRT5 is under the control of PGC-1α and AMPK and is involved in regulation of mitochondrial energy metabolism. FASEB J. 2014;28:3225-3237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 27. | Park J, Chen Y, Tishkoff DX, Peng C, Tan M, Dai L, Xie Z, Zhang Y, Zwaans BM, Skinner ME, Lombard DB, Zhao Y. SIRT5-mediated lysine desuccinylation impacts diverse metabolic pathways. Mol Cell. 2013;50:919-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 807] [Article Influence: 62.1] [Reference Citation Analysis (0)] |
| 28. | Wang G, Meyer JG, Cai W, Softic S, Li ME, Verdin E, Newgard C, Schilling B, Kahn CR. Regulation of UCP1 and Mitochondrial Metabolism in Brown Adipose Tissue by Reversible Succinylation. Mol Cell. 2019;74:844-857.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 164] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 29. | Zhang C, He X, Sheng Y, Xu J, Yang C, Zheng S, Liu J, Li H, Ge J, Yang M, Zhai B, Xu W, Luo Y, Huang K. Allicin Regulates Energy Homeostasis through Brown Adipose Tissue. iScience. 2020;23:101113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 30. | Li L, Shi L, Yang S, Yan R, Zhang D, Yang J, He L, Li W, Yi X, Sun L, Liang J, Cheng Z, Shang Y, Yu W. SIRT7 is a histone desuccinylase that functionally links to chromatin compaction and genome stability. Nat Commun. 2016;7:12235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 302] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 31. | Yu HB, Cheng ST, Ren F, Chen Y, Shi XF, Wong VKW, Law BYK, Ren JH, Zhong S, Chen WX, Xu HM, Zhang ZZ, Hu JL, Cai XF, Hu Y, Zhang WL, Long QX, He L, Hu ZW, Jiang H, Zhou HZ, Huang AL, Chen J. SIRT7 restricts HBV transcription and replication through catalyzing desuccinylation of histone H3 associated with cccDNA minichromosome. Clin Sci (Lond). 2021;135:1505-1522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 32. | Yuan HF, Zhao M, Zhao LN, Yun HL, Yang G, Geng Y, Wang YF, Zheng W, Yuan Y, Song TQ, Niu JQ, Zhang XD. PRMT5 confers lipid metabolism reprogramming, tumour growth and metastasis depending on the SIRT7-mediated desuccinylation of PRMT5 K387 in tumours. Acta Pharmacol Sin. 2022;43:2373-2385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 33. | Shi B, Feng ZQ, Li WB, Zhang HY. Low G preconditioning reduces liver injury induced by high +Gz exposure in rats. World J Gastroenterol. 2015;21:6543-6549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Zhang Y, Bharathi SS, Rardin MJ, Lu J, Maringer KV, Sims-Lucas S, Prochownik EV, Gibson BW, Goetzman ES. Lysine desuccinylase SIRT5 binds to cardiolipin and regulates the electron transport chain. J Biol Chem. 2017;292:10239-10249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 35. | Arias-Loste MT, García-Unzueta MT, Llerena S, Iruzubieta P, Puente A, Cabezas J, Alonso C, Cuadrado A, Amado JA, Crespo J, Fábrega E. Plasma betatrophin levels in patients with liver cirrhosis. World J Gastroenterol. 2015;21:10662-10668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Abdollahi M, Marandi SM, Ghaedi K, Safaeinejad Z, Kazeminasab F, Shirkhani S, Sanei MH, Rezvanian P, Nasr-Esfahani MH. Insulin-Related Liver Pathways and the Therapeutic Effects of Aerobic Training, Green Coffee, and Chlorogenic Acid Supplementation in Prediabetic Mice. Oxid Med Cell Longev. 2022;2022:5318245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 37. | O'Connell TM, Golzarri-Arroyo L, Pin F, Barreto R, Dickinson SL, Couch ME, Bonetto A. Metabolic Biomarkers for the Early Detection of Cancer Cachexia. Front Cell Dev Biol. 2021;9:720096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 38. | Nakagawa T, Lomb DJ, Haigis MC, Guarente L. SIRT5 Deacetylates carbamoyl phosphate synthetase 1 and regulates the urea cycle. Cell. 2009;137:560-570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 649] [Cited by in RCA: 627] [Article Influence: 36.9] [Reference Citation Analysis (0)] |
| 39. | Kwan R, Chen L, Park MJ, Su Z, Weerasinghe SVW, Lee WM, Durkalski-Mauldin VL, Fontana RJ, Omary MB. The Role of Carbamoyl Phosphate Synthetase 1 as a Prognostic Biomarker in Patients With Acetaminophen-induced Acute Liver Failure. Clin Gastroenterol Hepatol. 2023;21:3060-3069.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 40. | Polletta L, Vernucci E, Carnevale I, Arcangeli T, Rotili D, Palmerio S, Steegborn C, Nowak T, Schutkowski M, Pellegrini L, Sansone L, Villanova L, Runci A, Pucci B, Morgante E, Fini M, Mai A, Russo MA, Tafani M. SIRT5 regulation of ammonia-induced autophagy and mitophagy. Autophagy. 2015;11:253-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 278] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 41. | Zhang R, Xie X, Carrico C, Meyer JG, Wei L, Bons J, Rose J, Riley R, Kwok R, Kumaar PA, He W, Nishida Y, Liu X, Locasale JW, Schilling B, Verdin E. Regulation of urea cycle by reversible high stoichiometry lysine succinylation. bioRxiv. 2022;. [DOI] [Full Text] |
| 42. | Frayn KN, Kingman SM. Dietary sugars and lipid metabolism in humans. Am J Clin Nutr. 1995;62:250S-261S; discussion 261S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 100] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 43. | Mostofa MG, Tran M, Gilling S, Lee G, Fraher O, Jin L, Kang H, Park YK, Lee JY, Wang L, Shin DJ. MicroRNA-200c coordinates HNF1 homeobox B and apolipoprotein O functions to modulate lipid homeostasis in alcoholic fatty liver disease. J Biol Chem. 2022;298:101966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 44. | Xu M, Wu H, Li M, Wen Y, Yu C, Xia L, Xia Q, Kong X. DJ-1 Deficiency Protects Hepatic Steatosis by Enhancing Fatty Acid Oxidation in Mice. Int J Biol Sci. 2018;14:1892-1900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Du Y, Hu H, Qu S, Wang J, Hua C, Zhang J, Wei P, He X, Hao J, Liu P, Yang F, Li T, Wei T. SIRT5 deacylates metabolism-related proteins and attenuates hepatic steatosis in ob/ob mice. EBioMedicine. 2018;36:347-357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 46. | Hwang CY, Choe W, Yoon KS, Ha J, Kim SS, Yeo EJ, Kang I. Molecular Mechanisms for Ketone Body Metabolism, Signaling Functions, and Therapeutic Potential in Cancer. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 70] [Reference Citation Analysis (0)] |
| 47. | Laffel L. Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev. 1999;15:412-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 48. | Veneti S, Grammatikopoulou MG, Kintiraki E, Mintziori G, Goulis DG. Ketone Bodies in Diabetes Mellitus: Friend or Foe? Nutrients. 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 49. | Hegardt FG. Mitochondrial 3-hydroxy-3-methylglutaryl-CoA synthase: a control enzyme in ketogenesis. Biochem J. 1999;338 ( Pt 3):569-582. [PubMed] |
| 50. | Rardin MJ, He W, Nishida Y, Newman JC, Carrico C, Danielson SR, Guo A, Gut P, Sahu AK, Li B, Uppala R, Fitch M, Riiff T, Zhu L, Zhou J, Mulhern D, Stevens RD, Ilkayeva OR, Newgard CB, Jacobson MP, Hellerstein M, Goetzman ES, Gibson BW, Verdin E. SIRT5 regulates the mitochondrial lysine succinylome and metabolic networks. Cell Metab. 2013;18:920-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 604] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 51. | Ali HR, Michel CR, Lin YH, McKinsey TA, Jeong MY, Ambardekar AV, Cleveland JC, Reisdorph R, Reisdorph N, Woulfe KC, Fritz KS. Defining decreased protein succinylation of failing human cardiac myofibrils in ischemic cardiomyopathy. J Mol Cell Cardiol. 2020;138:304-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 52. | Jebb D, Hiller M. Recurrent loss of HMGCS2 shows that ketogenesis is not essential for the evolution of large mammalian brains. Elife. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 53. | Guo Y, Zhang X, Zhao Z, Lu H, Ke B, Ye X, Wu B, Ye J. NF- κ B/HDAC1/SREBP1c pathway mediates the inflammation signal in progression of hepatic steatosis. Acta Pharm Sin B. 2020;10:825-836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 54. | Sun R, Zhang Z, Bao R, Guo X, Gu Y, Yang W, Wei J, Chen X, Tong L, Meng J, Zhong C, Zhang C, Zhang J, Sun Y, Ling C, Tong X, Yu FX, Yu H, Qu W, Zhao B, Guo W, Qian M, Saiyin H, Liu Y, Liu RH, Xie C, Liu W, Xiong Y, Guan KL, Shi Y, Wang P, Ye D. Loss of SIRT5 promotes bile acid-induced immunosuppressive microenvironment and hepatocarcinogenesis. J Hepatol. 2022;77:453-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 112] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 55. | Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021;397:2212-2224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 461] [Cited by in RCA: 1944] [Article Influence: 388.8] [Reference Citation Analysis (33)] |
| 56. | Tilg H, Adolph TE, Moschen AR. Multiple Parallel Hits Hypothesis in Nonalcoholic Fatty Liver Disease: Revisited After a Decade. Hepatology. 2021;73:833-842. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 285] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 57. | Cheng Y, Hou T, Ping J, Chen G, Chen J. Quantitative succinylome analysis in the liver of non-alcoholic fatty liver disease rat model. Proteome Sci. 2016;14:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 58. | Giandomenico V, Simonsson M, Grönroos E, Ericsson J. Coactivator-dependent acetylation stabilizes members of the SREBP family of transcription factors. Mol Cell Biol. 2003;23:2587-2599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 193] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 59. | Thornton J. Hepatitis Fund aims to accelerate viral hepatitis elimination. Lancet. 2023;401:1414-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 60. | Polaris Observatory Collaborators. Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol. 2018;3:383-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1260] [Cited by in RCA: 1261] [Article Influence: 157.6] [Reference Citation Analysis (6)] |
| 61. | Seto WK, Lo YR, Pawlotsky JM, Yuen MF. Chronic hepatitis B virus infection. Lancet. 2018;392:2313-2324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 391] [Article Influence: 48.9] [Reference Citation Analysis (2)] |
| 62. | Jeng WJ, Papatheodoridis GV, Lok ASF. Hepatitis B. Lancet. 2023;401:1039-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 350] [Article Influence: 116.7] [Reference Citation Analysis (0)] |
| 63. | Martinez MG, Boyd A, Combe E, Testoni B, Zoulim F. Covalently closed circular DNA: The ultimate therapeutic target for curing HBV infections. J Hepatol. 2021;75:706-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 128] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 64. | Qin YP, Yu HB, Yuan SY, Yang Z, Ren F, Wang Q, Li F, Ren JH, Cheng ST, Zhou YJ, He X, Zhou HZ, Zhang Y, Tan M, Yang ML, Zhang DP, Wen X, Dong ML, Zhang H, Liu J, Li ZH, Chen Y, Huang AL, Chen WX, Chen J. KAT2A Promotes Hepatitis B Virus Transcription and Replication Through Epigenetic Regulation of cccDNA Minichromosome. Front Microbiol. 2021;12:795388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 65. | Yuan Y, Yuan H, Yang G, Yun H, Zhao M, Liu Z, Zhao L, Geng Y, Liu L, Wang J, Zhang H, Wang Y, Zhang XD. IFN-α confers epigenetic regulation of HBV cccDNA minichromosome by modulating GCN5-mediated succinylation of histone H3K79 to clear HBV cccDNA. Clin Epigenetics. 2020;12:135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 66. | Zheng R, Qu C, Zhang S, Zeng H, Sun K, Gu X, Xia C, Yang Z, Li H, Wei W, Chen W, He J. Liver cancer incidence and mortality in China: Temporal trends and projections to 2030. Chin J Cancer Res. 2018;30:571-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 240] [Cited by in RCA: 252] [Article Influence: 31.5] [Reference Citation Analysis (2)] |
| 67. | de Martel C, Maucort-Boulch D, Plummer M, Franceschi S. World-wide relative contribution of hepatitis B and C viruses in hepatocellular carcinoma. Hepatology. 2015;62:1190-1200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 348] [Cited by in RCA: 395] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 68. | Yanai M, Kurata M, Muto Y, Iha H, Kanao T, Tatsuzawa A, Ishibashi S, Ikeda M, Kitagawa M, Yamamoto K. Clinicopathological and molecular analysis of SIRT7 in hepatocellular carcinoma. Pathology. 2020;52:529-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 69. | Yuan Y, Yuan HF, Geng Y, Zhao LN, Yun HL, Wang YF, Yang G, Zhang XD. Aspirin modulates 2-hydroxyisobutyrylation of ENO1K281 to attenuate the glycolysis and proliferation of hepatoma cells. Biochem Biophys Res Commun. 2021;560:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Pădureanu V, Romania; Sukocheva OA, Australia S-Editor: Qu XL L-Editor: Filipodia P-Editor: Zheng XM