Published online Dec 27, 2024. doi: 10.4254/wjh.v16.i12.1493
Revised: October 11, 2024
Accepted: October 28, 2024
Published online: December 27, 2024
Processing time: 147 Days and 13.2 Hours
Liver transplantation (LT) has demonstrated favorable efficacy in managing end-stage alveolar echinococcosis. Nevertheless, the current research focal points and advancement trends remain ambiguous.
To map the research landscape to underscore critical areas of focus, influential studies, and future directions of LT for echinococcosis treatment.
Publications on LT for echinococcosis treatment published between 1900 and 2023 were searched in the Web of Science database and analyzed using bibliometrics.
A total of 14 countries/regions, 75 institutions, and 499 authors have published research articles, with China, Turkey, and France being the three most productive countries. The four institutions with the most contributions were Sichuan University, Xinjiang Medical University, the University de Franche Comte, and Inonu University. The three authors who contributed the most were Wen Hao, Wang Wentao, and Bresson Hadni Solange. The four most common keywords were alveolar echinococcosis, LT, ex-vivo liver resection and autotransplantation, and echinococcosis multilocularies.
Our study found that the treatment of complications after LT for echinococcosis treatment and the preoperative surgical plan based on the anatomical relationship between the lesion and the blood vessel are early research hotspots. Recent research focuses on the treatment of complications after ex-vivo liver resection and autotransplantation, especially vascular complications.
Core Tip: While numerous studies have reports on liver transplantation for echinococcosis, few have delved into its historical context and emerging trends. This study underscored the importance of comprehending historical and trend-based dimensions to anticipate future research hotspots in this domain. Consequently, the study aimed to conduct a bibliometric analysis to map the research landscape, highlight influential works, and identify potential future research directions.
- Citation: Mamuti A, Tulading A, Zhang YF, Azhati Y, Tuersunmaimaiti A, Maimaiti M, Lv CH, Wu J, Yao G, Aierken A, Tuxun T. Insight into the history and trends of liver transplantation for echinococcosis: A bibliometric analysis. World J Hepatol 2024; 16(12): 1493-1504
- URL: https://www.wjgnet.com/1948-5182/full/v16/i12/1493.htm
- DOI: https://dx.doi.org/10.4254/wjh.v16.i12.1493
Echinococcosis is a globally distributed zoonotic disease caused by the parasites Echinococcus granulosus (E. granulosus) and Echinococcus multilocularis (E. multilocularis), which are responsible for cystic echinococcosis (CE) and alveolar echinococcosis (AE), respectively[1]. This disease poses a significant threat to human health and imposes substantial economic burdens on global development. Both CE and AE are predominantly prevalent in pastoral and semi-pastoral regions, including areas such as western China, the eastern Mediterranean, southern and eastern Europe, North Africa, South America, and Central Asia[2]. Despite the considerable similarity between E. granulosus and E. multilocularis, these species exhibit distinct biological growth patterns, leading to the formation of fluid-filled cystic lesions in CE and infiltrative growth lesions in AE.
The World Health Organization Informal Working Group on Echinococcosis recommends radical resection combined with oral albendazole as the first-line treatment for these conditions[3]. The insidious growth of the parasites and progression of the disease, coupled with a general lack of awareness among patients, as well as significant involvement of major vasculature and compromised hepatic function, often results in the majority of cases being unresectable at the time of diagnosis, particularly in instances of AE. Consequently, the mortality rate for these patients is high, and liver transplantation (LT) is reserved as a last resort to preserve life. Currently, patients with end-stage hepatic AE and CE are considered candidates for LT, which is routinely performed in specialized centers within endemic regions, albeit in limited numbers.
The inaugural case of LT for echinococcosis treatment dates back to 1986, when a patient with end-stage hepatic AE successfully underwent deceased donor LT (DDLT)[4]. Nevertheless, LT in patients with echinococcosis remains uncommon due to technical challenges, donor shortages, and associated complications. It was not until 2009 that the first cases of living donor LT (LDLT) were performed on 2 patients with end-stage AE[5]. In contrast, patients with CE seldom require LT unless they develop Budd-Chiari syndrome, which leads to liver failure. A case of LT in a CE patient has been documented[6].
Ex-vivo liver resection and autotransplantation (ELRA) was initially introduced in 2010 by Wen Hao as a treatment for end-stage echinococcosis. Since then, it has gradually become the preferred option for unresectable cases, primarily due to its advantages of not requiring an organ donor, eliminating the need for immunosuppression, and having a relatively low recurrence rate[7]. Given that LT for echinococcosis treatment is considered an orphan procedure and is performed only sporadically in a limited number of centers within endemic regions, a comprehensive analysis could offer valuable insights into the historical and current trends of LT in the context of echinococcosis, potentially informing future developments in this field.
Bibliometrics involves the quantitative analysis of extensive collections of publications within specific research domains, utilizing visualization tools alongside mathematical and statistical methods to elucidate current research topics and predict future trends[8]. Our investigation revealed an absence of publications in the global database that examined LT for the treatment of echinococcosis through bibliometric analysis. This study analyzed the countries, institutions, authors, references, and keywords associated with LT for echinococcosis treatment from 1900 to 2023 by bibliometrics to elucidate the current status and forecast potential future research directions.
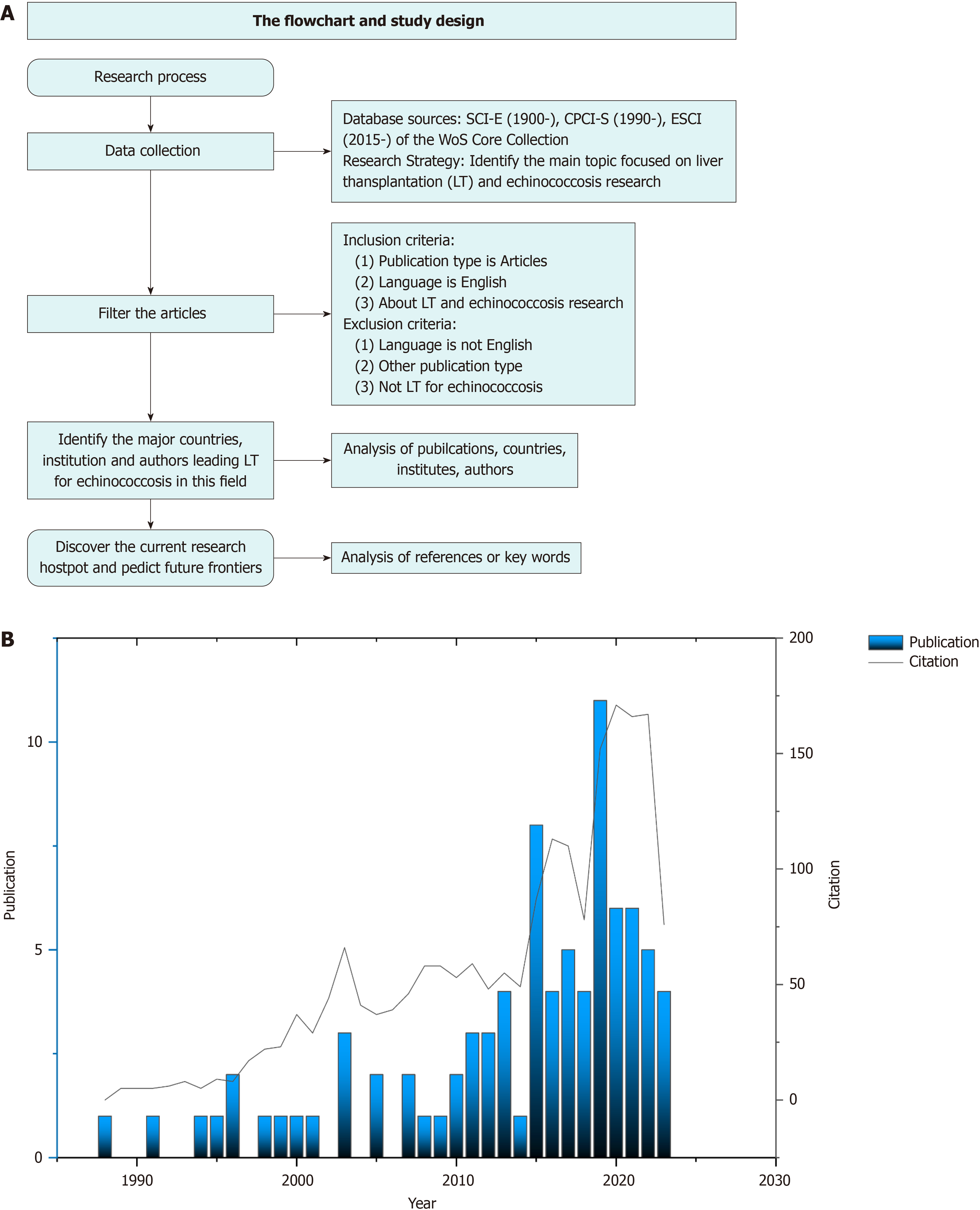
The Web of Science Core Collection (WoSCC) was selected as the primary database of our study. We searched articles of LT for echinococcosis treatment published between 1900 and 2023 with the following formula: TS = (Echinococc* OR Hydatid* OR cystic echinococc* OR alveococcosis OR alveolar echinococc* OR Multilocular echinococc*) AND TS = (graft* OR transplant* OR Liver* transplant* OR Hepatic* transplant* OR Autotransplant* OR Ex-vivo liver* resection OR ex-vivo resection). The entire WoSCC records, including the cited references, were downloaded in TEXT format within 1 day on December 26, 2023 to minimize possible deviations caused by database updates. The flowchart of data collection and analysis was illustrated in Figure 1A.
The bibliometric tools used in this paper were VOSviewer (version 1.6.18) and CiteSpace (version 5.7.R5 Advanced). VOSviewer was used to conduct collaborative network analysis of countries, institutions, authors, co-occurrence network, and density analysis of keywords. CiteSpace could provide citation burst analysis, supporting the identification of research trends and hotspots in the field. Origin 2021 is a scientific drawing and data analysis software developed by OriginLab (Northampton, MA, United States). It is used for data statistics and annual publication mapping in this study. Microsoft Office Excel 2016 was used for descriptive statistical analysis and chart generation. Scimago Graphica (version 1.0.24) was used to process image data and beautify images.
A total of 85 publications on LT for echinococcosis treatment published in the WoSCC database from January 1, 1900 to December 26, 2023 were included in this study. The number of publications and citations related to LT for echinococcosis treatment has increased steadily since 1988. Since 2011, the number of publications has gradually increased, and the annual citation growth of publications has been consistent with the growth trend of publications, reflecting that LT has gradually become an indispensable part of research in this field (Figure 1B).
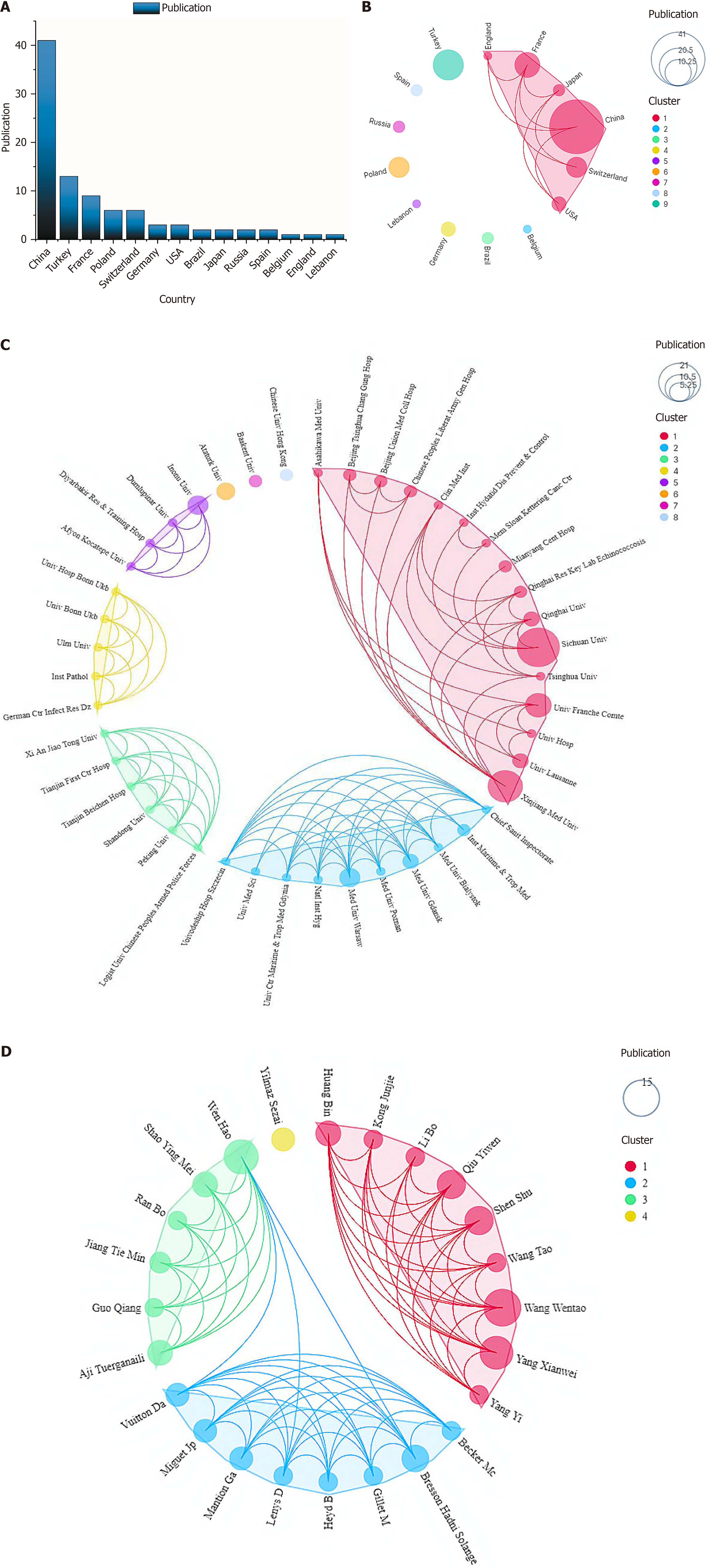
Countries/regions: The results showed that a total of 14 countries/regions contributed to the treatment of LT for echinococcosis treatment. The top three countries in terms of the number of publications were China (n = 41, 48.2%), Turkey (n = 13, 15.3%), and France (n = 9, 10.6%) (Figure 2A). The intensity of cooperation between these countries is relatively weak, among which France has cooperative relations with China, Switzerland, and other countries (Figure 2B).
Institutions: The institution with the largest volume of publications was Sichuan University (n = 21, 205 citations), followed by Xinjiang Medical University (n = 14, 233 citations) and University de Franche Comte (n = 8, 586 citations), Warsaw Medical University (n = 5, 97 citations), and Inonu University (n = 5, 69 citations). The top 10 production institutions in terms of the number of publications were centralized in China, Turkey, France, and other major producing countries (Table 1). The University de Franche Comte located in France, has close cooperation with many institutions (Figure 2C). Combined with Figure 2B and C, it was found that the cooperation between the main producing countries was not as good as the cooperation between domestic institutions.
| Rank | Institutions | Country | Documents | Citations |
| 1 | Sichuan University | China | 21 | 205 |
| 2 | Xinjiang Medical University | China | 14 | 233 |
| 3 | University de Franche Comte | France | 8 | 586 |
| 4 | Inonu University | Turkey | 5 | 69 |
| 5 | Medical University of Warsaw | Poland | 5 | 97 |
| 6 | Ataturk University | Turkey | 4 | 60 |
| 7 | Medical University of Gdansk | Poland | 3 | 75 |
| 8 | Qinghai University | China | 3 | 0 |
| 9 | University of Lausanne | Switzerland | 3 | 176 |
| 10 | Baskent University | Turkey | 2 | 39 |
Authors: In this study, the number of publications and citations on LT for echinococcosis treatment ranked among the top 10 authors (Table 2). Wang Wentao had the most publications (n = 15), followed by Wen Hao (n = 13) and Yang Xianwei (n = 12). Among them seven authors were from China, and the remaining three authors were from France or Turkey. In China, there is a close cooperation between Wang Wentao and Wen Hao (Figure 2D), and Wen Hao’s articles have been cited in the top second in this field. Bresson Hadni Solange from France has published articles with the highest citations, making great contributions to the development of this field.
| Rank | Author | Country | Documents | Total citations | Rank | Author | Country | Citations | TLS |
| 1 | Wang Wentao | China | 15 | 49 | 1 | Bresson Hadni Solange | France | 126 | 665 |
| 2 | Wen Hao | China | 13 | 30 | 2 | Wen Hao | China | 60 | 311 |
| 3 | Yang Xianwei | China | 12 | 43 | 3 | Kern P | USA | 57 | 353 |
| 4 | Qiu Yiwen | China | 9 | 37 | 4 | Vuitton Da | France | 40 | 314 |
| 5 | Shen Shu | China | 9 | 38 | 5 | Koch Sp | Germany | 31 | 198 |
| 6 | Bresson Hadni Solange | France | 8 | 35 | 6 | Gottstein B | Switzerland | 26 | 208 |
| 7 | Aji Tuerganaili | China | 7 | 27 | 7 | Brunetti E | Italy | 24 | 170 |
| 8 | Huang Bin | Turkey | 7 | 34 | 8 | Ammann Rw | Switzerland | 22 | 195 |
| 9 | Shao Ying Mei | China | 7 | 27 | 9 | Yang Xw | China | 22 | 123 |
| 10 | Mantion Ga | France | 6 | 32 | 10 | Mcmanus Dp | Australia | 20 | 127 |
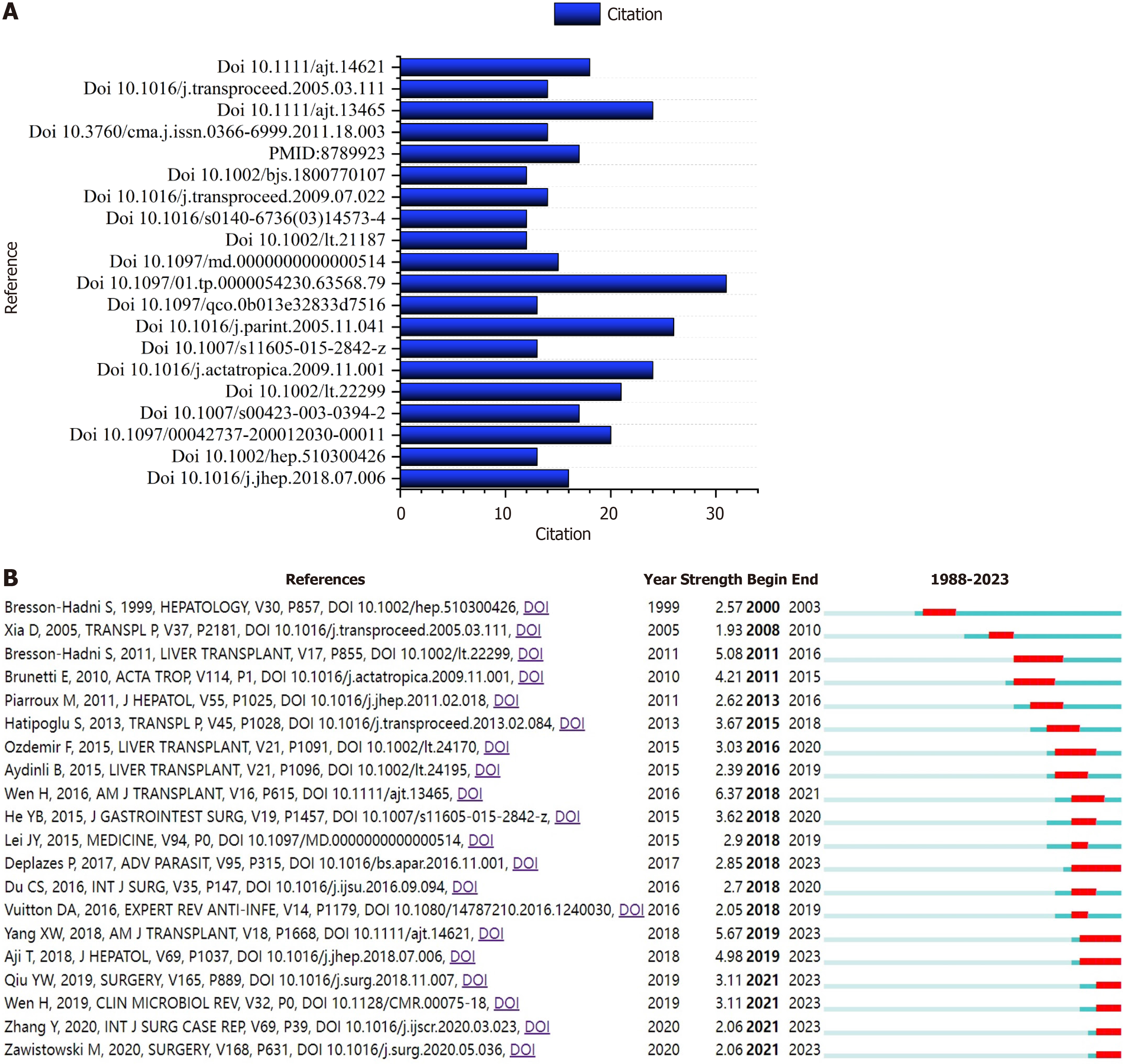
Analysis of co-cited references: Our analysis of co-cited references yielded 1081 records. Figure 3A shows the top 20 co-cited references. The top 10 co-cited references are shown in Supplementary Table 1 and 2. Among them, the paper entitled, “Experience of LT for incurable AE: A 45-case European collaborative report” has received the greatest number of co-citations (n = 31)[9]. The paper entitled, “Expert consensus for the diagnosis and treatment of cystic and AE in humans” ranked second (n = 26)[10]. Most of the top 10 co-cited articles were published in the last 20 years. The top 20 with the strongest citation burst were shown in Figure 3B, with the red bar indicating high citation frequency and the blue bar indicating fewer citations. Supplementary Table 2 shows the references that are kept in a state of burst[11-17].
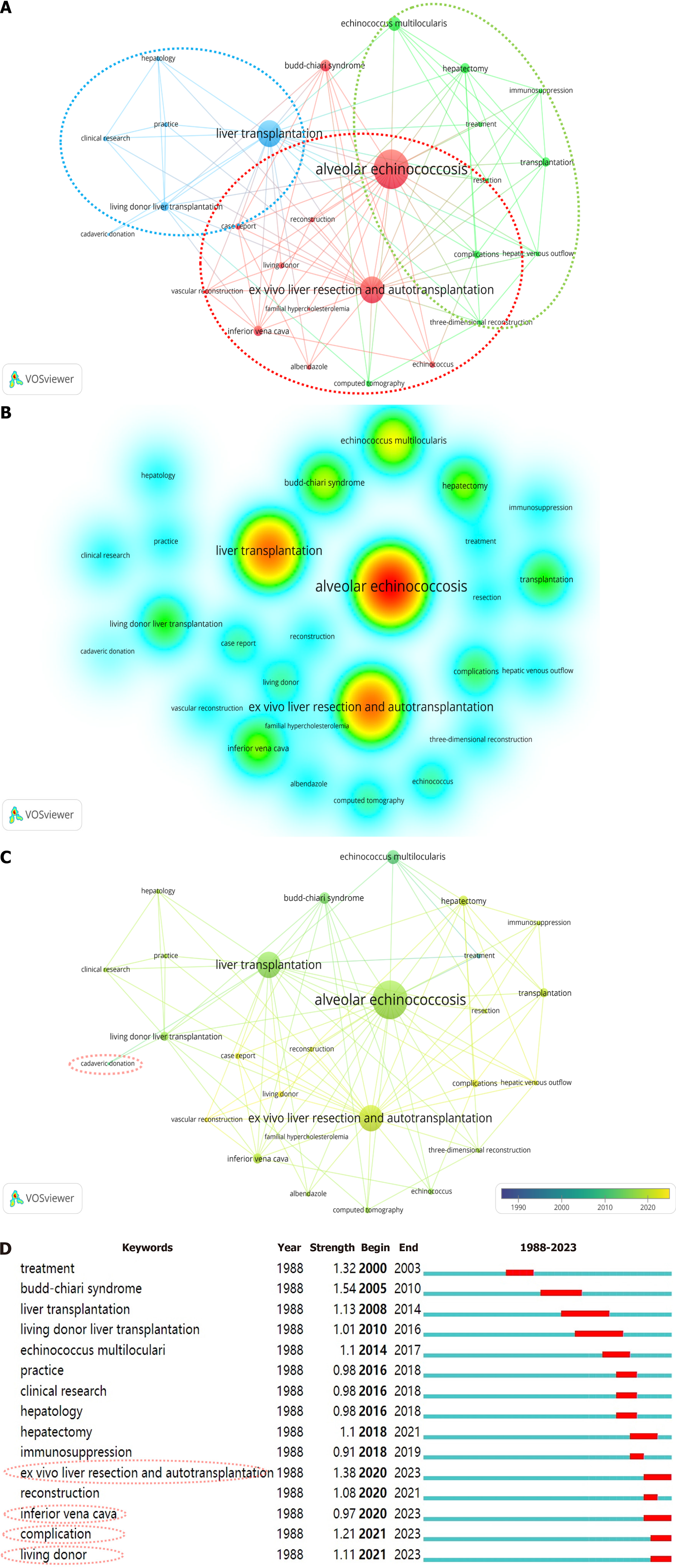
Analysis of keywords: We studied the keyword co-occurrence network diagram showing four different clusters (Figure 4A). Cluster 1 (red) included AE, ELRA, Budd-Chiari syndrome, and inferior vena cava (IVC). Cluster 2 (green) contained hepatectomy, echinococcus multilocularis, transplantation, and complications. Cluster 3 (blue) focused on liver transplantation, LDLT, and cadaver donation. The above commonly used keywords showed high density in the density view (Figure 4B), indicating that these keywords are currently popular and have great potential in the field of LT for echinococcosis treatment. Keyword analysis was used to explore the changing trends of research topics, predict emerging topics, and reveal potential research hotspots in this field. Recent keywords included complications, vascular re
To the best of our knowledge, our study is the inaugural bibliometric analysis on LT in patients with echinococcosis, providing a comprehensive overview of the historical development and trends of various LT techniques in this context. Our analysis encompassed 85 pertinent research articles originating from 14 countries, 75 institutions, and involving 449 authors globally.
Since the initial efforts to treat end-stage hepatic AE with LT[4], approximately 300 cases have been documented worldwide, mostly from China, France, and Turkey. The limited reporting of allotransplantation can be attributed to the low incidence of the orphan disease[9], surgical techniques in the endemic region[9], immune rejection[18], and concerns regarding postoperative recurrence[9]. The ELRA technique originated in France and expanded significantly in China, driven by the high incidence of echinococcosis, particularly AE, in northwest China. Since 2011, the ELRA technique has gained rapid global recognition and has become increasingly pivotal in the management of AE, as demonstrated by the substantial rise in related publications and citations (Figure 1B).
A total of 14 countries have predominantly contributed articles to this field. Notably, China has produced the highest volume and quality of publications, followed by France and Turkey. Since 2011, there has been a rapid increase in the number of publications, a trend closely associated with the advent of ELRA. In this study, we concluded that Sichuan University and Xinjiang Medical University in China were ranked first and second, respectively, in terms of publication output. The remaining institutions in the top 10 were located in France, Turkey, Poland, and Switzerland. As tertiary centers and World Health Organization collaborating centers, the hospitals affiliated with Sichuan and Xinjiang Medical Universities were responsible for nearly 90% of the transplantation procedures for AE patients in China. Additionally, a significant number of patients from other endemic regions, including the Qinghai-Tibetan Plateau, were referred to these centers[19] . The primary focus of these institutions was on the surgical techniques and safety associated with ELRA. Meanwhile, the University of Franche-Comté reported the first and a majority of DDLT cases. In the aspect of publication output, Inonu University and Warsaw Medical University are ranked fourth and fifth, respectively, with their research predominantly focusing on the surgical indications and safety of allotransplantation.
The study showed that Wang Wentao and Wen Hao have made the most significant contributions in publication volume, while Bresson Hadni Solange articles had garnered the highest number of citations. Despite the relatively recent experience of Chinese researchers with LT for echinococcosis treatment, China leads in the number of publications. The field of LT for echinococcosis treatment continues to expand and holds substantial potential for future advancements, particularly concerning ELRA. Furthermore, the findings indicated that the frequency of cooperation is insufficient from a global standpoint. It is imperative to enhance collaboration among countries, institutions, and authors through multicenter research initiatives, international conferences, and the exchange of expertise. Such efforts are essential to advancing the worldwide dissemination of LT for echinococcosis treatment, ultimately benefiting a greater number of patients in need.
To gain a deeper understanding of notable achievements within this specific field, an analysis of co-cited references was performed. The 10 most frequently cited references in this study were clinical series published in reputable scholarly journals, as indicated in Supplementary Table 2. In 2000, Bresson-Hadni et al[20] proposed that benzimidazole (BMZ) treatment is generally administered to patients with unresectable parasites or recurrent AE following surgery, with LT being necessary if deterioration persists. In 2003, Bresson-Hadni et al[21] documented five fatalities among 47 AE patients who underwent LT, with three of these deaths potentially attributable to excessive immunosuppression and inappropriate BMZ treatment post-transplant. The aforementioned findings suggest that BMZ effectively inhibits both the recurrence and progression of echinococcosis. Conversely, inappropriate application of immunosuppressive treatment strategies may exacerbate the progression of extrahepatic echinococcosis.
According to research findings[9], the 5-year survival rate post-allotransplantation for patients with AE is 71%, with a recurrence-free survival rate of 58%. It is imperative to evaluate the presence of distant metastasis in these patients and to restrict the use of immunosuppressive medications before surgery. Kern et al[3] developed a PNM system classification based on a cohort of 222 patients with AE. This classification functions as an internationally acknowledged standard for disease staging and assists in identifying appropriate candidates for LT. The 2010 edition of the consensus guidelines on the diagnosis and management of human CE and AE[10] recommended that post-LT therapy with BMZs should be administered for a minimum duration of 2 years, with ongoing surveillance extending for at least 10 years[22]. In their 2011 study, Bresson-Hadni et al[23] reported on 5 patients with AE who underwent LT followed by postoperative treatment with BMZs. The authors suggested that LT may serve as a viable option for patients who are unable to undergo radical resection or who experience postoperative metastasis and recurrence during critical periods. They further indicated that BMZ therapy could effectively manage residual disease following transplantation and mitigate the risk of AE recurrence.
In 2015, Jianyong et al[24] documented successful outcomes without recurrence using the autologous vein for IVC replacement in ELRA, thereby suggesting it as a valuable surgical option for advanced AE. In a 2016 study by Wen et al[25], it was documented that 15 patients with end-stage hepatic AE underwent treatment with ELRA, resulting in a mortality rate of 6.7% (1/15) and a major complication incidence of 20% (3/15). Additionally, another study involving 31 AE patients treated with ELRA reported a mortality rate of 6.5%, with severe infection and disease recurrence identified as the primary causes of death[16]. In 2018, the research team led by Wen Hao documented a cohort of 69 patients with AE who underwent ELRA. The study emphasized the meticulous adherence to surgical indications, made the preoperative prediction of the size and quality of the future residual liver volume (RLV), and the prevention of postoperative complications, including liver failure. The publication exerted a substantial influence within the academic community, as demonstrated by its frequent citations and enduring relevance.
Our findings indicated that cadaver donation emerged as a significant research topic around 2010, with ELRA becoming the predominant focus in the field since 2011 (Figure 4C). During the past 5 years, newly emerged research areas, including complications and vascular reconstruction, have gained prominence as critical areas of investigation. These results are correlated with the early implementation of DDLT and LDLT, in contrast to the relatively later introduction of ELRA. Since 2011, a substantial body of research has emerged, broadening the scope of the previous topic. Concurrently, the focus of research has shifted from surgical safety to the management of complications. The constrained advancement of DDLT can be ascribed to the necessity for extended immunosuppressive therapy, a scarcity of donors, postoperative complications, and a high recurrence rate. Key terms relevant to the current heightened interest in this area include ELRA, complications, living donors, and the IVC (Figure 4D). Keywords for the current elevated outbreak status included: ELRA; complications; living donors; and IVC (Figure 4D). Among them, ELRA is currently in an explosive state, with a high intensity and longer duration of the outbreak. ELRA was first seen in the keyword overlay diagram in 2011.
In 2011, Wen Hao’s team[7] reported the first case of an operation for end-stage AE employing ELRA, indicating a potentially innovative surgical approach for this condition, as evidenced by the successful procedure and favorable postoperative outcome of the patient. By 2015, 4 years after the initial case, a total of 15 patients had undergone ELRA treatment, yielding a mortality rate of 6.6% and a major complication rate of 20%[25]. The previously mentioned groundbreaking discovery has progressively enhanced the application of ELRA in managing end-stage AE, promoted the advancement of related scientific research, and contributed to an increase in scholarly publications in this field (Figure 1B).
In 2018, Yang X’s study on ELRA for AE involving 31 patients indicated that an RLV/standard liver volume (SLV) ratio greater than 35% could serve as a new criterion for the surgery. However, further research is necessary due to the limited follow-up and absence of a control group in the study[16]. The increasing utilization of ELRA techniques has led to an increased number of individuals being accepted for ELRA procedures. A study by Aji et al[12] in 2018 documented the successful treatment of 69 patients with end-stage AE using ELRA, with no reported cases of recurrence during the follow-up period. The study found that the 30-day mortality rate was 7.24% (5/69), while the overall mortality rate was 11.5% (8/69).
Research conducted by Shen et al[18] on ELRA revealed that patients undergoing this procedure exhibited a 100% survival rate at 1-year, 3-year, and 5-year follow-up intervals. In contrast, the study reported that the overall survival rates for patients undergoing LDLT were 100% at 1 year, 83.3% at 3 years, and 66.7% at 5 years. These findings suggest that ELRA may represent a more advantageous treatment option. Furthermore, research indicates that an RLV/SLV ratio of less than 40% does not adversely affect patient prognosis following ELRA. However, it is crucial that the potential impact of postoperative hepatic vein obstruction to the residual liver[26].
The aforementioned research has demonstrated the safety and feasibility of ELRA in managing end-stage AE, underscoring its advantages over DDLT and LDLT. Moreover, an RLV/SLV range of 35% to 40% is considered a surgical indication for ELRA. Qiu et al[27] performed an analysis comparing the prognostic outcomes of end-stage AE between ELRA and nonsurgical treatment modalities. Meanwhile, it also indicated a significantly higher 5-year survival rate of 82.1% in the ELRA cohort, in contrast to only 19.1% in the group receiving palliative care. These results imply that ELRA may substantially improve survival rates for patients with end-stage AE. To date, the largest number of ELRA cases reported originates from the authors’ institution, encompassing 114 patients with AE[28]. The most recent study conducted by Qiu et al[29] documented 91 patients with end-stage AE who underwent ELRA, with a complication rate of 33% (30/91).
This study acknowledged certain limitations that needs to be addressed. Given the widespread use of English globally, a significant number of publications on LT for echinococcosis treatment are available in English. Nonetheless, this study may have overlooked high-quality publications in other languages. Additionally, the study exclusively utilized publications from the WoSCC database, thereby excluding other databases and potentially introducing selection bias. Furthermore, bibliometric analysis predominantly depends on the volume of publications and the total number of citations, with the accrual of citations being a protracted process. Our findings revealed that a considerable proportion of the highly ranked co-cited articles were published 10 years ago, indicating that these publications exert substantial influence and may in some degree reflect the current research landscape.
Our study found that since 2011, the number of publications on LT for echinococcosis treatment has increased rapidly. At present, the cooperation between countries or institutions around the world in this field is not close enough, and it is necessary to further strengthen cooperation and exchange experience. The study also found that the treatment of complications after LT and the development of surgical plans based on echinococcosis and vascular anatomy are early research hotspots. The future research trend is the treatment of vascular complications in ERLA, and vascular complications may be related to vascular repair methods or materials.
The author thanks Xinjiang Medical University for all the administrative assistance during the implementation of the project.
| 1. | McManus DP, Gray DJ, Zhang W, Yang Y. Diagnosis, treatment, and management of echinococcosis. BMJ. 2012;344:e3866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 269] [Article Influence: 19.2] [Reference Citation Analysis (1)] |
| 2. | Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 710] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 3. | Kern P, Wen H, Sato N, Vuitton DA, Gruener B, Shao Y, Delabrousse E, Kratzer W, Bresson-Hadni S. WHO classification of alveolar echinococcosis: principles and application. Parasitol Int. 2006;55 Suppl:S283-S287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 227] [Article Influence: 10.8] [Reference Citation Analysis (1)] |
| 4. | Gillet M, Miguet JP, Mantion G, Bresson-Hadni S, Becker MC, Rouget C, Christophe JL, Roullier M, Landecy G, Guerder L. Orthotopic liver transplantation in alveolar echinococcosis of the liver: analysis of a series of six patients. Transplant Proc. 1988;20:573-576. [PubMed] |
| 5. | Moray G, Shahbazov R, Sevmis S, Karakayali H, Torgay A, Arslan G, Savas N, Yilmaz U, Haberal M. Liver transplantation in management of alveolar echinococcosis: two case reports. Transplant Proc. 2009;41:2936-2938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Moreno-González E, Loinaz Segurola C, García Ureña MA, García García I, Gómez Sanz R, Jiménez Romero C, González Pinto I, Corral Sanchez MA, Palma Carazo F. Liver transplantation for Echinococcus granulosus hydatid disease. Transplantation. 1994;58:797-800. [PubMed] [DOI] [Full Text] |
| 7. | Wen H, Dong JH, Zhang JH, Zhao JM, Shao YM, Duan WD, Liang YR, Ji XW, Tai QW, Aji T, Li T. Ex vivo liver resection followed by autotransplantation for end-stage hepatic alveolar echinococcosis. Chin Med J (Engl). 2011;124:2813-2817. [PubMed] |
| 8. | Ninkov A, Frank JR, Maggio LA. Bibliometrics: Methods for studying academic publishing. Perspect Med Educ. 2022;11:173-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 478] [Article Influence: 119.5] [Reference Citation Analysis (0)] |
| 9. | Koch S, Bresson-Hadni S, Miguet JP, Crumbach JP, Gillet M, Mantion GA, Heyd B, Vuitton DA, Minello A, Kurtz S; European Collaborating Clinicians. Experience of liver transplantation for incurable alveolar echinococcosis: a 45-case European collaborative report. Transplantation. 2003;75:856-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 107] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 10. | Brunetti E, Kern P, Vuitton DA; Writing Panel for the WHO-IWGE. Expert consensus for the diagnosis and treatment of cystic and alveolar echinococcosis in humans. Acta Trop. 2010;114:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1638] [Cited by in RCA: 1416] [Article Influence: 88.5] [Reference Citation Analysis (0)] |
| 11. | Deplazes P, Rinaldi L, Alvarez Rojas CA, Torgerson PR, Harandi MF, Romig T, Antolova D, Schurer JM, Lahmar S, Cringoli G, Magambo J, Thompson RC, Jenkins EJ. Global Distribution of Alveolar and Cystic Echinococcosis. Adv Parasitol. 2017;95:315-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 685] [Article Influence: 76.1] [Reference Citation Analysis (1)] |
| 12. | Aji T, Dong JH, Shao YM, Zhao JM, Li T, Tuxun T, Shalayiadang P, Ran B, Jiang TM, Zhang RQ, He YB, Huang JF, Wen H. Ex vivo liver resection and autotransplantation as alternative to allotransplantation for end-stage hepatic alveolar echinococcosis. J Hepatol. 2018;69:1037-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 85] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 13. | Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, Zhang W, McManus DP. Echinococcosis: Advances in the 21st Century. Clin Microbiol Rev. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 704] [Article Influence: 100.6] [Reference Citation Analysis (0)] |
| 14. | Qiu Y, Yang X, Shen S, Huang B, Wang W. Vascular infiltration-based surgical planning in treating end-stage hepatic alveolar echinococcosis with ex vivo liver resection and autotransplantation. Surgery. 2019;165:889-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (2)] |
| 15. | Zhang Y, Lai ECH, Yang C, Yang H, Liu J, Zhou G, Xian D, Deng S, Lau WY. In situ reconstruction of vascular inflow/outflow to left lateral liver section, ex-vivo liver resection and autologous liver transplantation of remaining liver remnant for hepatic alveolar echinococcosis. Int J Surg Case Rep. 2020;69:39-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Yang X, Qiu Y, Huang B, Wang W, Shen S, Feng X, Wei Y, Lei J, Zhao J, Li B, Wen T, Yan L. Novel techniques and preliminary results of ex vivo liver resection and autotransplantation for end-stage hepatic alveolar echinococcosis: A study of 31 cases. Am J Transplant. 2018;18:1668-1679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 17. | Zawistowski M, Nowaczyk J, Jakubczyk M, Domagała P. Outcomes of ex vivo liver resection and autotransplantation: A systematic review and meta-analysis. Surgery. 2020;168:631-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (1)] |
| 18. | Shen S, Kong J, Qiu Y, Zhang S, Qin Y, Wang W. Ex vivo liver resection and autotransplantation versus allotransplantation for end-stage hepatic alveolar echinococcosis. Int J Infect Dis. 2019;79:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Craig P. Echinococcus multilocularis. Curr Opin Infect Dis. 2003;16:437-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 111] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Bresson-Hadni S, Vuitton DA, Bartholomot B, Heyd B, Godart D, Meyer JP, Hrusovsky S, Becker MC, Mantion G, Lenys D, Miguet JP. A twenty-year history of alveolar echinococcosis: analysis of a series of 117 patients from eastern France. Eur J Gastroenterol Hepatol. 2000;12:327-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 125] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Bresson-Hadni S, Koch S, Miguet JP, Gillet M, Mantion GA, Heyd B, Vuitton DA; European group of clinicians. Indications and results of liver transplantation for Echinococcus alveolar infection: an overview. Langenbecks Arch Surg. 2003;388:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 69] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Reuter S, Jensen B, Buttenschoen K, Kratzer W, Kern P. Benzimidazoles in the treatment of alveolar echinococcosis: a comparative study and review of the literature. J Antimicrob Chemother. 2000;46:451-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 115] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Bresson-Hadni S, Blagosklonov O, Knapp J, Grenouillet F, Sako Y, Delabrousse E, Brientini MP, Richou C, Minello A, Antonino AT, Gillet M, Ito A, Mantion GA, Vuitton DA. Should possible recurrence of disease contraindicate liver transplantation in patients with end-stage alveolar echinococcosis? A 20-year follow-up study. Liver Transpl. 2011;17:855-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 24. | Jianyong L, Jingcheng H, Wentao W, Lunan Y, Jichun Z, Bing H, Ding Y. Ex vivo liver resection followed by autotransplantation to a patient with advanced alveolar echinococcosis with a replacement of the retrohepatic inferior vena cava using autogenous vein grafting: a case report and literature review. Medicine (Baltimore). 2015;94:e514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 25. | Wen H, Dong JH, Zhang JH, Duan WD, Zhao JM, Liang YR, Shao YM, Ji XW, Tai QW, Li T, Gu H, Tuxun T, He YB, Huang JF. Ex Vivo Liver Resection and Autotransplantation for End-Stage Alveolar Echinococcosis: A Case Series. Am J Transplant. 2016;16:615-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 26. | Shen S, Qiu Y, Yang X, Wang W. Remnant Liver-to-Standard Liver Volume Ratio Below 40% is Safe in Ex Vivo Liver Resection and Autotransplantation. J Gastrointest Surg. 2019;23:1964-1972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Qiu Y, Huang B, Yang X, Wang T, Shen S, Yang Y, Wang W. Evaluating the Benefits and Risks of Ex Vivo Liver Resection and Autotransplantation in Treating Hepatic End-stage Alveolar Echinococcosis. Clin Infect Dis. 2022;75:1289-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Maimaitinijiati Y, AJi T, Jiang TM, Ran B, Shao YM, Zhang RQ, Guo Q, Wang ML, Wen H. Approaches to reconstruction of inferior vena cava by ex vivo liver resection and autotransplantation in 114 patients with hepatic alveolar echinococcosis. World J Gastroenterol. 2022;28:4351-4362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 29. | Qiu Y, Yang X, Huang B, Wei G, Chen Y, Yang K, Wang W. Outcomes of inferior vena cava reconstruction using artificial or autologous materials in ex vivo liver resection and autotransplantation. Asian J Surg. 2023;46:213-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/