Published online Jun 27, 2023. doi: 10.4254/wjh.v15.i6.850
Peer-review started: April 8, 2023
First decision: May 4, 2023
Revised: May 22, 2023
Accepted: May 31, 2023
Article in press: May 31, 2023
Published online: June 27, 2023
Processing time: 77 Days and 17.4 Hours
Sepsis is a severe medical condition that occurs when the body's immune system overreacts to an infection, leading to life-threatening organ dysfunction. The "Third international consensus definitions for sepsis and septic shock (Sepsis-3)" defines sepsis as an increase in sequential organ failure assessment score of 2 points or more, with a mortality rate above 10%. Sepsis is a leading cause of intensive care unit (ICU) admissions, and patients with underlying conditions such as cirrhosis have a higher risk of poor outcomes. Therefore, it is critical to recognize and manage sepsis promptly by administering fluids, vasopressors, steroids, and antibiotics, and identifying and treating the source of infection.
To conduct a systematic review and meta-analysis of existing literature on the management of sepsis in cirrhotic patients admitted to the ICU and compare the management of sepsis between cirrhotic and non-cirrhotic patients in the ICU.
This study is a systematic literature review that followed the PRISMA statement's standardized search method. The search for relevant studies was conducted across multiple databases, including PubMed, Embase, Base, and Cochrane, using predefined search terms. One reviewer conducted the initial search, and the eligibility criteria were applied to the titles and abstracts of the retrieved articles. The selected articles were then evaluated based on the research objectives to ensure relevance to the study's aims.
The study findings indicate that cirrhotic patients are more susceptible to infections, resulting in higher mortality rates ranging from 18% to 60%. Early identification of the infection source followed by timely administration of antibiotics, vasopressors, and corticosteroids has been shown to improve patient outcomes. Procalcitonin is a useful biomarker for diagnosing infections in cirrhotic patients. Moreover, presepsin and resistin have been found to be reliable markers of bacterial infection in patients with decompensated liver cirrhosis, with similar diagnostic performance compared to procalcitonin.
This review highlights the importance of early detection and management of infections in cirrhosis patients to reduce mortality. Therefore, early detection of infection using procalcitonin test and other biomarker as presepsin and resistin, associated with early management with antibiotics, fluids, vasopressors and low dose corticosteroids might reduce the mortality associated with sepsis in cirrhotic patients.
Core Tip: Sepsis is a severe condition encountered in the intensive care unit (ICU), and when it occurs in cirrhotic patients, it often leads to high mortality due to impaired immunity and multiorgan failure. To diagnose and monitor sepsis in cirrhotic patients, various scoring systems have been developed, including the Sequential Organ Failure Assessment (SOFA) score, the Chronic Liver Failure-Sequential Organ Failure Assessment (CLIF-SOFA) score, quick SOFA (qSOFA), Model for End-Stage Liver Disease (MELD), and MELD-Na score. Although the proposed current management of sepsis in cirrhotic patients might follow the guidelines proposed by the Surviving Sepsis Campaign, this approach has might not cause significant improvement in patient outcomes. Therefore, early recognition of infection and its source is critical, followed by timely initiation of antibiotic therapy, fluid resuscitation with albumin (5% or 20%), vasopressors, and low-dose corticosteroids such as hydrocortisone. Studies have shown that this approach reduces mortality in the ICU. In addition to pharmacological interventions, interventions to control the source of infection, such as surgical drainage, may also be necessary. Finally, procalcitonin levels can be used as a diagnostic biomarker in cirrhotic patients with sepsis, helping to guide antibiotic therapy and improve patient outcomes. In conclusion, timely recognition and management of sepsis in cirrhotic patients in the ICU is crucial, and early initiation of appropriate interventions, including antibiotics, fluids, and corticosteroids, may improve patient outcomes.
- Citation: Ndomba N, Soldera J. Management of sepsis in a cirrhotic patient admitted to the intensive care unit: A systematic literature review. World J Hepatol 2023; 15(6): 850-866
- URL: https://www.wjgnet.com/1948-5182/full/v15/i6/850.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i6.850
Physiologically, sepsis is viewed as a proinflammatory and procoagulant response to invading pathogens with three recognized stages in the inflammatory response, with a progressively increased risk of end-organ failure and death[1]. Evidence shows that sepsis in cirrhotic patients causes a marked imbalance of cytokine response, known as a "cytokine storm," which converts responses that are normally beneficial for fighting infections into excessive, damaging inflammation. Therefore, the three recognized stages are sepsis, severe sepsis, and septic shock, and cirrhotic patients are prone to developing sepsis-induced organ failure and death[1]. Severe sepsis in cirrhotic patients is associated with high production of proinflammatory cytokines that play a role in the worsening of liver function and development of organ or system failure such as shock, acute lung injury, acute respiratory distress syndrome, coagulopathy, renal failure, or hepatic encephalopathy[1]. Furthermore, cirrhotic patients with severe sepsis can develop sepsis-induced hyperglycemia, defective arginine-vasopressin secretion, adrenal insufficiency, or compartmental syndrome[2].
Sepsis is a severe condition characterized by a deregulation of the body's response to infection and can lead to life-threatening organ dysfunction. As one of the leading causes of admission to intensive care units (ICUs), sepsis has been found to have poorer outcomes in patients with comorbidities such as cirrhosis, as stated in the "Third International Consensus Definitions for Sepsis and Septic Shock"[1-3]. Organ dysfunction in sepsis is measured by an increase of two points or more in the Sequential Organ Failure Assessment (SOFA) score, which is associated with a mortality rate greater than 10%[4-5]. The SOFA score comprises six sub-scores, including liver failure, which has been found to be associated with higher mortality. The other sub-scores include respiratory, coagulation, cardiovascular, central nervous system, and renal. Each sub-score is rated on a scale of 0 to 4 and summed up to a final score from 0 to 24. Systematic Inflammatory Response Syndrome occurs when two or more criteria, such as body temperature > 38 ℃ or < 36 ℃, tachycardia > 90/min, hyperventilation, and abnormal white blood cell count, are met[2].
Septic shock is a subset of sepsis that leads to profound circulatory and cellular metabolism abnormalities, resulting in substantially increased mortality[4]. To identify septic shock, one should look for hypotension that requires vasopressor therapy and a mean arterial pressure (MAP) of less than 65 mmHg despite adequate fluid resuscitation and systolic blood pressure. Additionally, signs of tissue hypoperfusion such as low urinary output, acidosis, and worsening mental status, along with evidence of systemic inflammatory response syndrome, including a body temperature above 38 or below 36 ºC, tachycardia, tachypnea, leukocytosis, and documented infection, are also considered[5].
Elevated lactate levels reflect cellular dysfunction in sepsis, and multiple factors contribute to their elevation, including insufficient tissue oxygen delivery, impaired aerobic respiration, acceleration of aerobic glycolysis, and reduced hepatic clearance[1]. However, defining sepsis and septic shock poses inherent challenges[3].
The acute change in total SOFA score of more than 2 points due to an infection is identified as organ dysfunction. In patients with a SOFA score of 2 or more, the overall mortality risk is approximately 10%, which is higher than the overall mortality rate of ST-segment elevation myocardial infarction. This score also identifies a 2-25 fold increased risk of dying compared to patients with a SOFA score less than 2. However, this score is not used as a tool for managing septic patients in the ICU but rather to characterize them clinically. SOFA has greater predictive validity in patients suspected of sepsis in an ICU[3,4].
There are several risk factors associated with sepsis, including patient factors such as immunosuppression, comorbidity, or therapy, microbe factors such as the presence of multi-resistant or virulent bacteria, and procedural risks such as surgery, indwelling catheters, or implantable devices[6]. Cirrhosis, which is the end-stage of most chronic liver diseases, has two clinical phases: Compensated and decompensated. The compensated phase is defined as the period between the onset of cirrhosis with minor or no symptoms and the first major complication, while the decompensated phase is when the patient first presents with ascites, variceal hemorrhage, hepatic encephalopathy, spontaneous bacterial peritonitis, and hepatorenal syndrome. This period is associated with a short survival time. Cirrhosis may be diagnosed by liver biopsy or by signs of chronic liver disease with documented portal hypertension. Cirrhotic patients have a reduced capacity of the reticuloendothelial system to clear bacteria from the gut, resulting in a higher rate of infections and a worse prognosis[7].
Cirrhosis is an irreversible condition caused by several factors or conditions, such as viral hepatitis, alcoholic liver disease, and non-alcoholic fatty liver disease. According to the World Health Organization, cirrhosis was the 9th leading cause of death in the west in 2015[8]. Studies have shown that mortality among cirrhotic patients with sepsis in the ICU ranges from 18%-66%, with mechanical ventilation being an independent predictor of mortality. The MELD and MELD-Na scores are used for the prediction of 90-day mortality and for organ allocation in liver transplantation. A cohort study by Baudry et al[9] found that mortality of cirrhotic patients with sepsis ranges from 18%-66%. WHO estimates cirrhosis as the 12th cause of mortality in the world, with deaths exceeding 1 million per year. ICUs provide specialized treatment and monitoring for critically ill patients.
The aim of the present paper is to determine the optimal current management of sepsis in cirrhotic patients admitted to the ICU.
This systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA-P) protocol[10] and examines published papers on the management of sepsis in cirrhotic patients admitted to the ICU.
Inclusion criteria were cirrhotic patients over 18 years old, admitted to the ICU with sepsis. The study analyzed the management and prognosis of cirrhotic patients with sepsis, as well as compared the management of sepsis in cirrhotic patients to those without cirrhosis. Only English-language randomized controlled trials (RCTs), retrospective cohort studies, and prospective cohort studies were included.
The analyzed outcomes include survival, length of ICU stay, and the overall prognosis of cirrhotic patients with sepsis admitted to the ICU.
Searches were conducted on PubMed, Google Scholar, Embase, and Cochrane databases. Retrieved papers were initially filtered based on their titles and abstracts, and the full text of selected papers were then retrieved and analyzed. Only papers that met the inclusion criteria were included and analyzed. The search strategy is described in Appendix 1 and the critical appraisal of the papers is presented in Appendix 2.
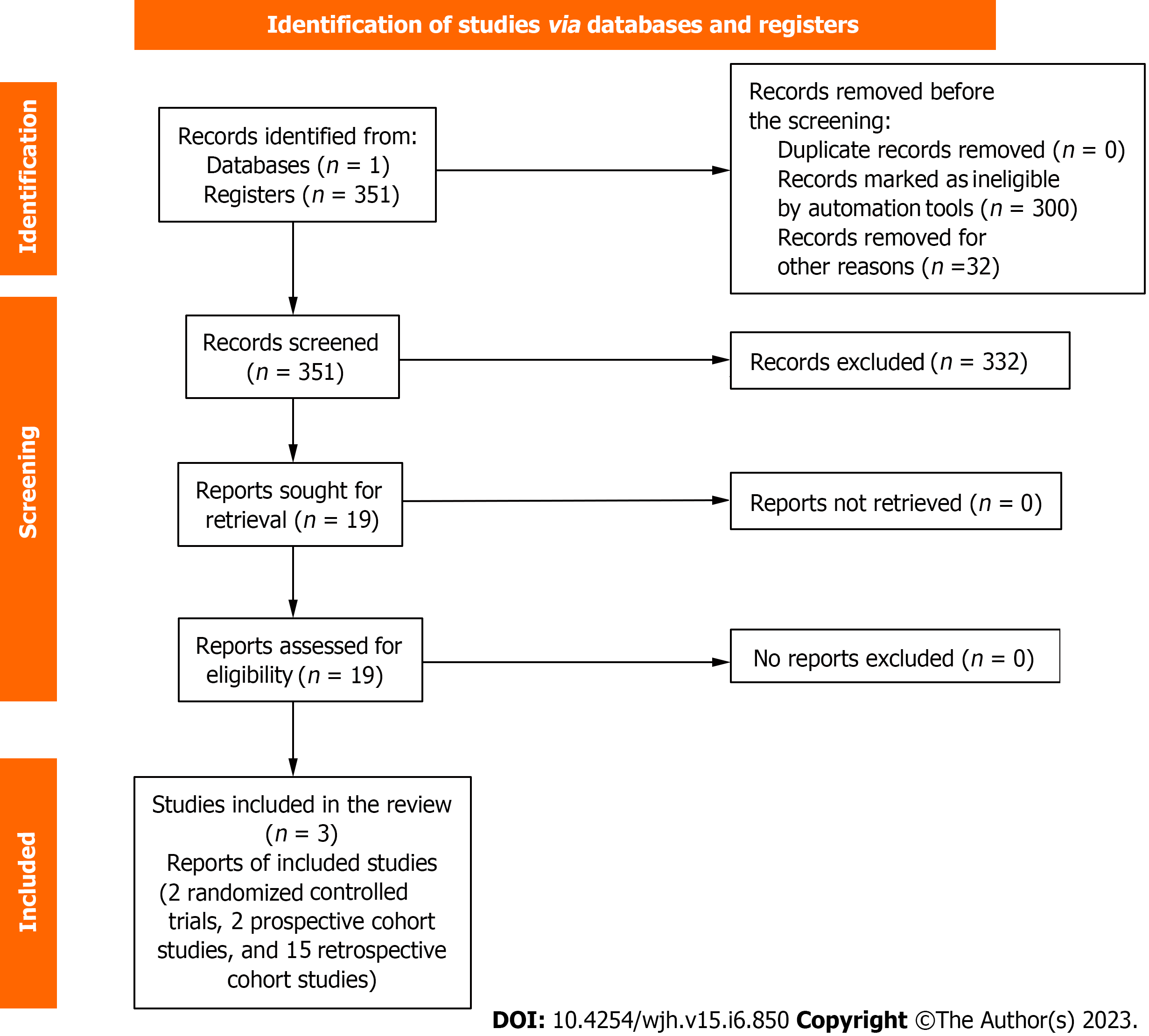
Figure 1 illustrates the selection process following the PRISMA-P protocol. Initially, 351 search results were retrieved, out of which 284 were excluded after screening the titles, 46 were excluded after the abstract, and 3 were excluded after full articles. A total of 19 papers met the inclusion criteria and were included for full-text review. The primary outcome of all reviewed papers was the survival of cirrhosis patients with sepsis in the ICU. The review also analyzed the prognostic value of scores such as Child-Turcotte-Pugh, Model for End-Stage Liver Disease (MELD), Model for End-Stage Liver Disease Sodium (MELD-Na), and SOFA scores for cirrhotic patients with sepsis. The summarized data is available on Table 1 for randomized controlled trials, Table 2 for prospective cohort studies, Table 3 for retrospective cohort studies and Table 4 for selected studies.
| Ref. | Purpose | Type of study | Sample size | Conclusion | Setting |
| Philips et al[11] | Assessed the use of 5% human fluid for the resuscitation of cirrhotic patients with sepsis | Three hundred-eight patients were divided into two groups | 5% human albumin was safe and more beneficial in correcting hypotension than normal saline | ICU | |
| Arabi et al[13] | Assess the use of a low dose of hydrocortisone in cirrhotic patients with sepsis | RCT | 140 patients were 65 excluded, and 39 received hydrocortisone and 36 placeboes | That study did not find mortality improvement with corticosteroids despite hemodynamic improvement. The treatment proposed: Hemodynamic monitoring and management, laboratory test culture, stress ulcer prophylaxis as histamine H2 receptor antagonists, norepinephrine as vasopressors, and empiric antibiotic. The outcome was 28 days of all-cause mortality | ICU |
| Ref. | Purpose | Type of study | Sample size | Conclusion | Setting |
| Rinaldi et al[5] | The aim was to evaluate the effect of adherence to evidence-based guidelines of the Surviving Sepsis Campaign (SSC) on the outcome of cirrhotic patients with shock admitted to the ICU. Resuscitation of sepsis with hydrocortisone | Prospective cohort | 38 patients | ICU | |
| Thierry et al[23] | Assess the use of echocardiography in assessing the LVEF on cirrhotic patients with septic shock | The prospective cohort single-center study | 34 patients compared | Echocardiography in a cirrhotic patient with septic shock show hyperdynamic syndrome with high LVEF | ICU |
| Ref. | Purpose | Type of study | Sample size | Conclusion | Setting |
| Guo et al[26] | Assessment of VCS parameter for evaluation of sepsis in cirrhotic patients | Retrospective analysis of prospective data | 257 patients | Proposed management was collection of blood culture, white cell volume determination, procalcitonin, and interleukin -6, sCD163 laboratory tests. Conclusion VCS parameters have the potential to be used to evaluate and predict early infections in patients with cirrhosis, and VCS can increase sensitivity and specificity in the diagnosis of sepsis and cirrhosis patients | ICU |
| Villarreal et al[15] | Assessing the usefulness of procalcitonin for diagnosing infection in cirrhotic patients | Retrospective cohort study | 66 patients of 255 admitted had procalcitonin tests. Patients with infection suspicion had a serum procalcitonin (PCT) test within the first 12 h | Septic patients with cirrhosis had elevated procalcitonin. As PCT has a sensitivity of 83% and specificity of 75% is an effective tool for diagnosing infection in patients with liver cirrhosis. Excellent tool for differentiating infectious disease in cirrhotic patients | ICU |
| Galbois et al[27] | Assess whether the mottling score and tissue oxygen saturation (StO2) may be used as early death predictors on cirrhotic patients with septic shock. Hemodynamic parameters at 6 h in patients with liver cirrhosis according to their survival status at 14 days | 42 out of 46 patients admitted with cirrhosis and septic shock were analyzed | There is systemic vasodilation and increased mortality in cirrhosis patients with sepsis. Patients with increased mottling died, and those with decreased survived. Mottling score and knee StO2 measures 6 h after starting vasopressors are excellent predictors of 14-day mortality | ICU | |
| Piccolo Serafim et al[14] | The study evaluates the use of steroids in a patient with septic shock and cirrhosis | A retrospective cohort study (2007-2017) | 56 patients out of 179 admitted with septic shock received steroids during ICU | The use of steroids did not show significant differences in mortality. Vasopressor requirement and is not associated with decreased mortality | ICU |
| Chang et al[17] | aimed to determine whether septic patients with liver cirrhosis had worse survival than patients without liver cirrhosis | Retrospective cohort | 776 patients, 64 had sepsis with cirrhosis, 712 sepsis without cirrhosis | Cirrhotic patients with sepsis had a poor outcome, and the survival of sepsis and cirrhosis after matching was not inferior to those without cirrhosis | ICU |
| Sauneuf et al[18] | Assess the use of albumin as an adjuvant to vasopressors in managing septic shock in cirrhotic patients | Retrospective cohort single center and observational overdone over 14 years studied done from 1997 to 2004 and 2005 to 2010 | During the period 2005 to 2010, 42, cirrhotic patients with septic shock in ICU were included | In conclusion, the survival rate of septic shock in cirrhosis remains low, and current shock management could benefit cirrhotic patients. Treatment use is: Vasopressors used is norepinephrine, epinephrine, and dobutamine; mechanical ventilation was used in the case of ARDS, and a protective strategy with a low tidal volume of 6 m/kg of body weight, and the plateau was kept below 30 cmH2O, small -dose of corticosteroids (200 mg hydrocortisone per day, insulin therapy, The main sites of infections were: Pneumonia, spontaneous or secondary peritonitis, and urinary tract infection. There were gram-positive and negative. Septic shock represent a severe complication of cirrhosis with very low survival rates. Sepsis in a cirrhotic patient has a poor prognosis. Hydrocortisone did not reduce mortality and was associated with adverse effects such as shock relapse and gastrointestinal bleeding. Cirrhotic patients are commonly perceived as poor candidates for `ICU admission because of the very high mortality | ICU |
| Umgelter et al[21] | Assess the outcome of the continuous low dose of TP in a septic shock patient | Small cohort study | 2004-2007: 12 patients, 8 males, and 4 females were included with sepsis due to spontaneous bacterial peritonitis, pneumonia, and cholangitis | TP is currently used in treating cirrhotic patients with hepatorenal syndrome and as an adjunct to NE in a cirrhotic patient with septic shock and kidney failure; TP dose 2 ug/kg if a patient was started NE in the first 24 h. 11 patients had RRT, TP increased SVR index and NE doses needed to obtain target MAP decreased while the CI remained stable. Despite hemodynamic improvement, 11 out of 12 patients died. The author concluded that TP was effective as a vasopressor in septic cirrhotic patients at a low dose in combination with NE, and there was no dramatic decrease in CI. TP has a role in the early treatment of septic shock, and the author recommends a controlled study with TP in a cirrhotic patient with sepsis | ICU |
| Durst et al[20] | The study aimed to evaluate the use of vasopressor in septic shock with cirrhosis and without cirrhosis | single-center, retrospective cohort, 18 years | 122 patients included were 61 with cirrhosis and 61 non-cirrhosis with sepsis, and septic with cirrhosis | ICU | |
| Maimone et al[12] | Compare the 20% albumin to plasmolytes in managing cirrhosis and sepsis in the intensive care unit | Retrospective cohort study | 100 patients with cirrhosis and sepsis-induced hypotension | ICU | |
| Bal et al[24] | The aim is to predict 50 days in hospital mortality in decomposed cirrhosis patients with SBP | A single-centre study prospective study | 218 were admitted to ICU from 2013-2014 with cirrhosis and spontaneous bacterial peritonitis | ICU | |
| Chebl et al[22] | Assess the outcome and mortality predictor of cirrhosis patients with sepsis | A single-center retrospective cohort study | 200 patients | The study revealed an increased risk of sepsis in cirrhotic patients and sepsis-induced organ failure and related death in cirrhosis. The management of shock is to keep MAP above 65 mmgh with vasopressors; the aggressive fluid hydration may worsen the outcome as there is low oncotic pressure in a cirrhotic patient, which may lead to oedema with aggressive fluid hydration, so it is good to start with vasopressors early in the treatment of septic cirrhosis patients to avoid complications, a cirrhotic patient has higher lactate than the non-cirrhotic because of decreased lactate clearance by the liver | ICU |
| Chen et al[25] | A single-center, retrospective cohort study from 2015 to 2018 | 104 patients with cirrhosis and bacteremia were subdivided into afebrile (55) and febrile (49) | The cirrhotic patient is prone to infection. Cirrhotic patients with bacterial infections present with atypical manifestations such as normothermia. Scoring systems focused on organ dysfunction, such as quick sequential organ failure assessment (qSOFA) score or chronic liver failure sequential organ failure assessment (CLIF-SOFA) score, have better predictor ability | In the emergency department | |
| Sasso et al[19] | Assess the prediction of mortality in a cirrhotic patient | Prospective cohort | 113 patients mechanically ventilator cirrhotic from 2014-2018 | Conclude that cirrhotic patients requiring mechanical ventilation have an extremely poor prognosis, and the vasopressor requirement was strongly a predictor of mortality in mechanical ventilation cirrhosis with sepsis | ICU |
| Fischer et al[12] | Assess the use of presepsin and resistin as markers of bacterial infections in cirrhotic patients with sepsis | Conclusion: Both presepsin and resistin may be reliable markers of bacterial infections in patients with decompensated liver cirrhosis and have similar diagnostic performance for bacterial infection and sepsis compared to C-reactive protein (CRP) and PCT. The best cut-off level of presepsin for diagnosis of sepsis was 1444 pg/mL. Conclusion PCT, CRP, Presepsin, and resistin had similar accuracy in diagnosing infection and sepsis in decompensated cirrhosis | ICU | ||
| Baudry et al[9] | Assess the prognosis of sepsis in cirrhotic patients | A Retrospective cohort study from 2002-2013 | 7644 patients were admitted, where 149 were | ICU |
| Ref. | Year | Aim | Setting | Results | Conclusion |
| Philips et al[11] | 2021 | Assessed the use of 5% human fluid for the resuscitation of cirrhotic patients with sepsis | ICU | Found that primary, the two groups were different, with P values of less than 0.05, which is statistically significant. Study was done among 300 patients with sepsis with hypotension and cirrhosis 123 (n = 154, 79.8% receive albumin, and 131 (154, 85.1%) receive normal saline. Outcome related to MAP. measurement only 7.5 (n = 23) show reversal hypotension MAP > 65 at the end of the first hours of the resuscitation period; after 3 h, it was 11.7% (n = 18) and 32% (n = 5) in albumin and saline groups respectively (P = 0.008); Secondary outcome related to MAP, in the first hours while the study group, 62 patients (20.1%, n = 308) fluid resuscitation and sustained at 2 h in 42 (13.6%) patients improved MAP more than 65 mmHgf was seen in 25.3 (n = 39). In the albumin group at the end of the first hour compared to 14.9% (n = 23) patients in the saline group (P = 0.03). In second hour 17.5% (n = 27) in albumin group compare 9.7% (in = 15, P = 0.06) in saline group 5% albumin showed better improvement of MAP hemodynamic response compared to saline with P < 0.001 that is statistically significant. First hour, HA vs NS: 99.5 ± 7.9 vs 101.7 ± 8.8, P = 0.02; Second hour 97.9 ± 5.5 vs 103.4 ± 6.7, P < 0.001); Third hour 96.6 ± 3.6 vs 103.1 ± 5.9, P < 0.001 | Found 5% human albumin correcting hypotension in sepsis with cirrhosis patients. Data were analyzed using IBM SPSS 22.0 statistic window. Quantitative variables were presented as mean ± SD and presented as number and percentage, the Chi-square or Fischer's exact test was used for categorical data, and continuous data were analyzed using the students' test or Mann-Whitney U test, Kaplan-Meier used for survival curves |
| Arabi et al[13] | 2010 | Assess the use of a low dose of hydrocortisone in cirrhotic patients with sepsis | ICU | 140 patients screened 75 enrolled in the study. 60 (80%) with shock within 24 h and 71 (95%) with shock within 48 h. Twenty-eight days mortality with hydrocortisone treatment compared to its placebo 33 (85%) vs 26 (72%) relative risk (RR) 1.17, 95% confidence interval 0.92-1.49, P = 0.19). There was relative adrenal insufficiency in cirrhosis patients presenting with septic shock. Hydrocortisone show significant hemodynamic improvement. The 28-day mortality 33 (85) P = 0.19 and ICU mortality 24 (62) P = 0.64. Hemodynamic response was shock reversal 24 (62) P = 0.05 statistically significant | Found that corticosteroids improve hemodynamic status of the patient but do not change mortality |
| Rinaldi et al[5] | 2013 | The aim was to evaluate the effect of adherence to evidence-based guidelines of the surviving sepsis campaign (SSC) on the outcome of cirrhotic patients with shock admitted to the ICU | ICU | 30 day-mortality of cirrhotic patients with septic shock in ICU is extremely high, and the application of SSC guidelines did not seem to improve the survival rate in this population. In addition, approximately 40% of cirrhotic patients developed an infection. 30 days mortality of 31 (81.6%) patients, 13 (86.6) with the bundle completed and 18 (78.2%) with the bundle not completed. This difference was not statistically significant | Hydrocortisone was associated with shock resolution but no survival modification. Chang et al[17], (2022) show that sepsis in cirrhotic patients has poor outcome than sepsis without Cirrhosis. And Sauneuf et al[18], (2013) found also that sepsis in cirrhotic patient survival remain low despite current management. Bal et al[24], 2016 found that mortality in 50 days in septic with cirrhosis patients was 43% |
| Thierry et al[23] | 2007 | Assess the use of echocardiography in assessing the LVEF on cirrhotic patients with septic shock | ICU | Show clinical and echocardiographic hemodynamic parameters between patients with Cirrhosis and without Cirrhosis; Cirrhosis had higher. Without Cirrhosis, Cirrhosis had higher values for the CI (3.69+/-1 vs 2.86+/-0.81/min/m2, P = 0.02. SI (37.5 ± 8 vs 32.4 ± 7 mL/m2, P = 0.04); LVEF (67 ± 7 vs 55.9 ± 12%, P = 0.005 and lower value for the SVR (1636.1 ± 523 vs 2136.6+/-633 dynes/cm5 m2, P = 0.04). The MELD score was not significantly correlated with the CI (R = 0.20, P = 0.49, or S (r = 0.15, P = 0.6). Mortality in ICU was 53% overall (64% vs 45%, P = 0.27), not statistically different from the patient without Cirrhosis | Show that echocardiography is of important help in the management of Cirrhosis with sepsis, showing hyperdynamic syndrome with high LVEF |
| Guo et al[26] | 2019 | Assessment of VCS parameter for evaluation of sepsis in cirrhotic patients | ICU | 52% of positive culture in septic patients with Cirrhosis, with traditional infection markers (PCT, IL-6) and sCD163 between the two groups significantly different (P < 0.001). VCS parameters WBC range from 1.4 to 18.3 in sepsis, and leucocytes range from 1.6 to 19.2 in patients with infection no difference in the two groups for WBC. Test sensitivity was 75.9%, and a specificity of 73% was achieved | Reviewed the management of cirrhosis patients with sepsis and proposed: Blood vulture collection, white cell volume determination, procalcitonin and interleukin -6 and sCD163 test, and he concluded that VCS parameters predict the presence of infection early in cirrhotic patients |
| Villareal et al[15] | 2016 | Assessing the usefulness of procalcitonin for diagnosing infection in cirrhotic patients | ICU | Found that the mean scores as mean child-Pugh score 9.5 ± 2 and MELD score 23 ± 8 with P = 0.14 and P = 0.33, respectively, and there were not statistically significant for Cirrhosis with and without infection, and the mortality was high 62.9%. Procalcitonin (PCT) as biomarkers was found to be higher in a patient with infection than those without infection 4.20 (1.4-10.2) vs 0.16 (0.1-0.23) through statistically significant differences were not reached P = 0.53, severe sepsis or septic shock was associated with higher PCT | Procalcitonin as biomarker might help with infection diagnosis in cirrhotic patients, and P. Fischer et al. (2019) found that both presepsin and resistin may be reliable markers of bacterial infection in patients with decompensated liver cirrhosis and have similar diagnostic performance compared to PCT |
| Chen et al[25] | 2019 | ICU | Find that the mean time of initiation of the antibiotic treatment was 3.5 h in the patient (afebrile: 4.3 h, febrile 2.8 h P = 0.23 high incidence of the afebrile group admitted in ICU (43.6% vs 20.4% P = 0.01) and higher 30 days mortality in afebrile group 40% vs 18.4%) P = 0.02) and endotracheal intubation 27.3% vs 10.2%, P = 0.03) infection | Found that the cirrhotic patient has an atypical presentation, and the qSOFA score or CLIF-SOFA score has a better predictor ability | |
| Umgelter et al[21] | 2008 | Assess the outcome of the continuous low dose of terlipressin (TP) in a septic shock patient | ICU | Find that ICU admission patients had a mean age of 58 ± 85 mean Child-Pugh score of 13.8 ± 0.8, and a mean APACHE ii score of 31 ± 6 where TP decreases systemic vascular resistance index and norepinephrine (NE) doses needed to obtain the target MAP decreased, while cardiac index CI remained stable, median survival after initiating TP was ranging 5-15 days | Found that TP at a dose of 2 ug/kg can be used as an adjunct to NE in a cirrhotic patient with sepsis for hemodynamic improvement |
| Durst et al[20] | 2021 | The study aimed to evaluate the use of vasopressor in septic shock with cirrhosis and without cirrhosis | ICU | state that sepsis in cirrhosis was more likely to occur than in non-cirrhotic 34 (55.7%) versus 23(37.8%), P = 0.046, and received steroid 38.3% and 19.7%, respectively P = 0.024. The cirrhosis group requires increased median (IQR) total vasopressor dosage when compared to non-cirrhotic [71.5 (15.5-239.5)] vs 24.7 (5.3-77.9) mg NE equivalent, P = 0.003 and required a significantly higher total number of vasopressor agents 3 (1-4) vs 2 (1-3) agents P = 0.03. The length of ICU stays 7.0 (3.6-11.4) vs 5.0 (2.6-10.4) days P = 0.146 no statistically significant and MAP goal greater than baseline BP was 3 (4.9%) | Found that for sepsis and Cirrhosis needing vasopressors, MAP should be maintained above 60 mmgh, and blood culture and antibiotic should be started early as a survival campaign guideline |
| Galbois et al[27] | 2015 | Assessment of VCS parameter for evaluation of sepsis in cirrhotic patients | ICU | Found that cirrhosis patients with sepsis admitted to ICU were child-Pugh c without mottling, and mortality at 14 days was 71% (at day 28:78% in ICU: 76% in hospital: 82%). Hemodynamic parameters at 6 h were: MAP more than 65mmgh that was 88%, CVP more than 8mmgh: was 90%, ScvO2 more than 81%, Urine output more than 0.5 mL/kg/h: 24%. Thenar and knee Sto2 at H6 to predict the outcome. Thenar Sto2 levels measured at H0 and H6 were not different in survivors and non-survivors. [H0: 77% (72-87) vs 84% (79-90), P = 0.11, H6:84% (79-89) vs 83% (71-92), P = 0.89]. Mottling score changes during the first 24 h of septic shock in a patient with and without Cirrhosis; in survivors, the proportion of patients with a mottling score of more than 2 decreased over time in both groups. in non-survivors, the proportion of patients with severe mottling score (4-5) increased over time in both groups. In non-survivors, the proportion of patients with a mottling score (0-1) was higher in patients with Cirrhosis than in patients without at H0 P = 0.001) and at H6 (P = 0.02), but was not significantly later | Described that mottling score and knee StO2 measurement at 6 h after vasopressors have excellent 14 days mortality prediction |
| Piccolo Serafim et al[14] | 2021 | The study evaluates the use of steroids in a patient with septic shock and Cirrhosis | ICU | Found that patients who received steroids received a higher total of vasopressors (91.2 mg vs 39.1 mg, P = 0.04) and lower of lactate (1.8 mmol/L vs 2.6 mmol/L, P = 0.007) | Show that steroids did not improve mortality despite hemodynamic changes |
| Chebl et al[22] | 2021 | Assess the outcome and mortality predictor of cirrhosis patients with sepsis | ICU | found that cirrhotic patients were more likely to get intubated than non-cirrhotic patients (72.49% vs 61.62%, P = 0.001), and there was no statistically significant difference in mechanical ventilation duration or ICU LOS among survivors. Cirrhotic patients have higher hospital mortality than non-cirrhotic patients (64.79% vs 31.54% P = 0.001) and higher ICU mortality (47.47% vs 18.05% P = 0.001) | proposed as management of cirrhotic patient with sepsis to keep MAP > 65 mmgh with vasopressors, and start vasopressors early because of reduced oncotic pressure and risk of pulmonary oedema, avoid aggressive fluid resuscitation, cirrhotic patients have higher lactate levels |
| Maimone et al[12] | 2022 | Compare the 20% albumin to plasmolytes in managing Cirrhosis and sepsis in the intensive care unit. | ICU | Found that sepsis and septic shock in cirrhotic patient was the leading cause of acute decompensation or acute, chronic liver failure and had a poor prognosis and increased mortality | Show that albumin 20% increases MAP above 65 mmgh 3 h after infusion compared with plasmolyte and restores hemodynamic status rapidly but induce pulmonary oedema; why is it important to close monitoring with ultrasound so early detection of pulmonary oedema and management |
| Bal et al[24] | 2013 | The aim is to predict 50 days in hospital mortality in decomposed cirrhosis patients with SBP | ICU | Bal et al[24] study show that 50 days mortality in ICU was 43.11% of the patient admitted | Show that patients admitted to intensive care units with sepsis and Cirrhosis have poor prognoses and are a poor candidate for ICU |
| Baudry et al[9] | 2019 | Assess the prognosis of sepsis in cirrhotic patients. | ICU | ||
| Sauneuf et al[18] | 2013 | Assess the use of albumin as an adjuvant to vasopressors in managing septic shock in cirrhotic patients. | ICU | Find from 2005 to 2010, 40.5% were discharged from ICU, and 26% were alive six months after discharge. IV albumin was frequently given (57.1% vs 8.5%, P < 0.001), and crystalloid infusion was reduced at the same time [3 (1.7-4.5) L vs 6 (3-8,9) L, P = 0.08]. The ventilatory management with a smaller tidal volume 8.6 vs 7ml/kg, P = 0.001). Intensive insulin therapy and low-dose glucocorticoids were also used frequently during the second period, 83.3% vs 31.9% P < 0.001 and 81% vs 44.7, P < 0.001, respectively. Marked survival improvement in ICU as compared 1997-2004 period (40% vs 17%, P = 0.02, and 29% vs 6%, P = 0.009, respectively) | |
| Sasso et al[19] | 2020 | Assess the Prediction of mortality in a cirrhotic patient | ICU | Study shows changes in SOFA score median (IQR) in a cirrhotic patient. 24 h post admission 2.5 (0.75 to 5, P = 0.122 and 48 h post admission 1(0 to 4) P = 0.269. End of vasopressor therapy 0 (-3.5 to 21, P = 0.963, that is not statistically significant. But the duration of vasopressor in (hour) median (IQR) 86 (42.0-164.5) P = 0.003. MAP goal decreased during vasopressor course n (%) 13 (21.3) P = 0.041 statistically significant | Concluded that mechanically ventilated cirrhotic patients with sepsis have an extremely poor prognosis, and vasopressor use was strongly a predictor of mortality |
| Chang et al[17] | (2022) | The study aimed to determine whether septic patients with liver cirrhosis had worse survival than patients without liver cirrhosis | ICU | Found that liver cirrhosis was more common in male patients with 48% median range APACHE II was 25.5%, 27% of ICU mortality, sepsis with compensated liver cirrhosis mechanical ventilation 24% P value 0.179 and 4% (P = 0.842) needed for renal replacement therapy | |
| Fischer et al[16] | 2019 | Assess the use of presepsin and resistin as markers of bacterial infections in cirrhotic patients with sepsis | ICU | Found that 63% of the aetiology of Cirrhosis was alcoholism, 46% was bacterial infection (SBP), as infection markers presepsin, resistin, CRP, and PCT for predicting 28 days survival were AUROC = 0.74 (95% VI: 0.64-0.84) (P < 0.001), 0.68 (95%CI: 0.57-0.82) (P = 0.006, 0.74 (95%CI: 0.64-0.84)(P < 0.001) and 0.70 (95%CI: 0.59-0.81) (P = 0.001) respectively |
Albumin: Philips et al[11] found that 5% human albumin corrected hypotension in sepsis with cirrhosis (Table 1). Maimone et al[12] found that albumin 20% increased MAP above 65 mmHg 3 h after infusion compared to plasmolyte, but with a risk of inducing pulmonary edema (Table 3).
Corticosteroids: Arabi et al[13] concluded that corticosteroids improved the hemodynamic status of the patient but did not change mortality (Table 1). Rinaldi et al[5] and Piccolo Serafim et al[14] found similar results to Arabi et al[13] (Tables 2 and 3).
Infection diagnosis: Villarreal et al[15] concluded that procalcitonin as a biomarker helped with infection diagnosis in cirrhotic patients. Fischer et al[16] found that both presepsin and resistin may be reliable markers of bacterial infection in patients with decompensated liver cirrhosis and have similar diagnostic performance compared to procalcitonin (Table 3).
Prognosis: Baudry et al[9], Fischer et al[16], Chang et al[17], and Sauneuf et al[18], found that the prognosis is poor in ICU for cirrhosis patients with sepsis (Table 3). Sasso et al[19] found that mechanically ventilated cirrhotic patients with sepsis have an extremely poor prognosis, and vasopressor use was strongly a predictor of mortality (Table 3).
Vasopressors: Durst et al[20] found that norepinephrine is the best vasopressor to use in cirrhotic patients with sepsis to maintain MAP above 60 mmHg. Umgelter et al[21] concluded that terlipressin is effective as a vasopressor in septic cirrhotic patients in combination with norepinephrine to correct hypotension. Chebl et al[22] recommend starting vasopressors early to avoid aggressive fluid resuscitation and maintain MAP > 65 mmHg (Table 3).
Hyperdynamic syndrome: Thierry et al[23] found that echocardiography helps diagnose hyperdynamic syndrome with high LVEF in septic patients (Table 3).
Mortality: Bal et al[24] found 50-day mortality to be about 43.11%. Baudry et al[9] found that the mortality of cirrhotic patients with sepsis ranges from 18%-66%, which is close to the WHO finding that estimates cirrhosis as the 12th cause of mortality in the world, with death exceeding 1 million a year (Table 3).
Scoring system: Chen et al[25] concluded that the qSOFA (Quick SOFA) criteria, consisting of 3 variables, are a better predictor of adverse outcomes associated with sepsis. The presence of two or more abnormalities in patients with suspected infection identifies a higher risk of developing adverse outcomes.
Hemodynamic monitoring: Administer antibiotics within the first hour and monitor physiological parameters like urine output and lactate clearance to prevent end-organ dysfunction[7]. In advanced cirrhosis, elevated cardiac index, low systemic vascular resistance, low MAP, and higher central venous oxygen saturation may be present. Lactate levels should be carefully evaluated as they may take a while to lower down to normal levels. Serum lactate measurement is still recommended in these patients[7]. Skin mottling score and tissue oxygenation saturation assessed with laser Doppler can also be used as hypoxia of the tissue markers in cirrhosis[7].
Fluid resuscitation: Aggressive intravenous fluid resuscitation is recommended in any patient with hypotension or elevated serum lactate. However, the choice of fluid between crystalloid or colloid remains controversial[6,11,12]. The SAFE study concluded that albumin improves hemodynamic status and may reduce mortality, while the VISEP study found that pentastarch colloids can cause acute kidney injury in sepsis and increase 90-day mortality[6,11]. Human albumin is the fluid of choice in cirrhotic patients with sepsis, as it corrects hypotension more effectively than crystalloid[12]. Early goal-directed therapy can help reduce mortality, but the methodology of the Rivers study has been questioned. The recommended fluid should be one that sustains an increase in intravascular volume and contains a chemical composition similar to that of extracellular fluid[6]. Hydroxyethyl starch is not recommended in cirrhosis patients as it increases nephrotoxicity, while albumin is associated with dose-dependent acute kidney injury[6]. An albumin dose of 50-100 g/day is used over crystalloid for initial fluid resuscitation in cirrhosis patients, but no strong evidence exists[6].
Sepsis bundle protocol: According to the Surviving Sepsis Campaign (SSC) guidelines, the sepsis bundle protocol did not improve survival in cirrhotic patients with sepsis[7].
Vasopressors: Vasopressors are frequently indicated to maintain a MAP of at least 65 mmHg in persistently hypotensive patients. Norepinephrine is widely used in distributive shock for its predominantly alpha-adrenoceptor agonism and vasoconstrictive effect[21]. Cirrhotic patients with sepsis and cirrhosis needing vasopressors should have a goal of maintaining the MAP above 60 mmHg. Blood culture and antibiotics should be started as early as possible according to the SCC guidelines[20]. SSC international guideline does not recommend vasopressors as monotherapy or the first line for septic shock treatment, and a randomized trial shows the benefit of angiotensin II for refractory vasodilatory shock treatment[7].
Corticosteroids: Corticosteroids are commonly used for unsatisfactory responses to vasopressors. It helps hasten shock resolution, decreases the required dose of vasopressors, and improves the 90-day survival in septic shock patients, and it might increase shock recurrence. Nevertheless, its use in liver cirrhosis remains controversial[7]. Hydrocortisone improves the hemodynamic status of the patient without a relevant change in mortality[13,14,18]. Hydrocortisone is associated with better shock resolution, although without an impact on survival[5]. Low-dose corticosteroid is recommended to be administered early in patients with severe septic shock to patients who are not responding to vasopressors, but this is still controversial[6].
Antibiotics: Broad-spectrum empirical antimicrobial therapy should be commenced early after obtaining blood for culture and microscopy. Many studies have shown mortality improvement when the antibiotic is administered within 1 h of the recognition of sepsis and hypotension[6]. The selection of the antimicrobial agents considers antifungal, antiviral, or antiparasitic agents that are directed by the clinical finding, knowledge of the common local pathogens and their antibiotic resistance profiles, and consideration of the patient's potential predisposition to a specific infection, for example, immunosuppression as for Cirrhosis[6]. Avoid prolonged therapy with broad-spectrum antimicrobials because it promotes the evolution of resistant organisms, which can lead to the failure of the treatment[6]. Sepsis in cirrhotic patients requires a high grade of suspicion so that empiric antibiotics might be started as early as possible. Each hour delay in the starting the antimicrobial increases mortality by 1.86 times. Broad-spectrum antibiotics should be considered in patients at risk for resistant bacteria[6,7]. Early antibiotic start and intravenous administration of albumin 5% or 20% decrease the risk of renal failure development and improve survival in a cirrhotic patient with sepsis[2].
Procalcitonin: Procalcitonin is used as a biomarker for the risk of severe bacterial infection and for stopping antimicrobial therapy, but its role in cirrhotic patients has not been established yet[7]. In contrast, Villarreal et al[15] found that procalcitonin might be helpful in identifying bacterial infections in cirrhotic patients. Fischer et al[16] by Fischer et al[16] concludes that both presepsin and resistin are reliable markers of bacterial infection in patients with decompensated liver cirrhosis and have similar diagnostic performance to procalcitonin.
Liver transplantation: Liver transplantation is the definitive treatment for cirrhotic patients[7]. Cirrhotic patients are prone to bacterial infections and have higher mortality. Early therapeutic management of sepsis in the cirrhotic patient is crucial, and treatment should focus on correcting hypotension and avoiding aggressive fluid resuscitation[22]. Echocardiography can help diagnose hyperdynamic syndrome with high LVEF in cirrhotic patients with sepsis. Blood tests and VCS parameters can predict the presence of infection early in cirrhotic patients[23,26]. Mottling score and knee score and tissue oxygen saturation measurement six hours after vasopressors have an excellent 14-day mortality prediction[27]. Sepsis in cirrhotic patients has a poor outcome compared to sepsis without cirrhosis. Vasopressors, mechanical ventilation, and corticosteroids are suggested treatments, but mortality in 50 days in cirrhosis patients with sepsis was 43%. Mechanically ventilated cirrhotic patients with sepsis have an extremely poor prognosis, and vasopressor use was a predictor of mortality[17,18,19,24]. Cirrhotic patients have atypical presentations, and the qSOFA score or CLIF-SOFA score has better predictive ability[25].
Renal-replacement therapy and liver-support system: The use of hemofiltration in patients with sepsis has the potential benefit of alleviating the systemic inflammation of sepsis by removing circulating inflammatory mediators. However, two RCTs did not demonstrate significant reduction in inflammatory mediators nor patients' outcomes. Therefore, hemofiltration should not be recommended for routine management of patients with severe sepsis[1,6]. For liver support in the management of cirrhosis, it is recommended to treat the grade of ascites that are grade1 (mild) or grade 2 (moderate) where it is managed out of the ICU with restricted dietary sodium intake, start antidiuretic and monitor urea and electrolyte. For grade 3 that have a large volume of ascites with respiratory implication, paracentesis is recommended followed by dietary sodium restriction and diuretic therapy. Antibiotic prophylaxis should be used to prevent severe sepsis in a cirrhotic patient with ascites, gastrointestinal bleeding, or with more than one episode of spontaneous bacterial infection[4].
Glucose control: Hyperglycemia and insulin resistance are common in sepsis, and hyperglycemia may act as a procoagulant, impair neutrophil function, and increase the risk of death. Therefore, it is recommended to monitor and control glucose levels in patients with sepsis[1].
Infection source control: Source control in sepsis involves physical measures for removing the focus of infection. It is essential to identify and manage the source of infection promptly in the ICU[6].
The management of sepsis in cirrhosis patients is crucial to decrease the high mortality rate associated with this condition. In recent years, research has aimed to find the most effective therapeutic management for sepsis in cirrhosis patients. Interestingly, current therapeutic strategies for sepsis in cirrhosis patients are similar to the SSC international guidelines accepted for the general population.
Despite current management strategies, mortality remains high in cirrhosis patients with sepsis. Mortality rates are currently around 38%, with 30% of deaths due to infection[28]. Liver-specific scores, such as the CLIF-SOFA, CLIF-C Acute-on-Chronic Liver Failure (ACLF), and CLIF-C acute decom
As the cirrhotic liver patient is prone to bacterial infection and impaired immunity status, which triggers complications related to cirrhosis such as hepatic encephalopathy, ascites, variceal bleeding, or hepatorenal syndrome[30-33] that further impaired prognosis[34]. The SSC guideline recommends early detection of the source of infection, early initiation of antibiotics, fluid resuscitation, vasopressors, and corticosteroids[11,12].
Several studies have investigated the effectiveness of different therapeutic strategies for sepsis in cirrhosis patients. The use of human albumin 5% and 20% has been found to be beneficial for correcting hypotension and maintaining MAP above 65 instead of crystalloid[11,12]. Furthermore, norepinephrine has been found to be the best vasopressor for correcting hypotension in cirrhosis patients with sepsis, and combination therapy with terlipressin and norepinephrine has also been found to be effective[20,22].
One interesting finding is that early vasopressor administration may be more beneficial than aggressive fluid administration in cirrhotic patients with sepsis. Chebl et al[22] found that early use of vasopressors was associated with better outcomes in cirrhosis patients. However, the use of corticosteroids did not show a decrease in mortality in cirrhotic patients with sepsis[9,18,19].
The management of sepsis in cirrhosis patients requires early detection and intervention with antibiotics, fluid resuscitation, vasopressors, and corticosteroids. While current management strategies are similar to those recommended in the SSC international guideline[36], studies have shown that the use of human albumin and norepinephrine or combination therapy with terlipressin and norepi
The use of EASL-CLIF criteria on ACLF and CLIF-SOFA for prognostication of sepsis in cirrhotic patients admitted to the ICU has gained significant attention[8,38]. These scoring systems have been developed to assess the severity of liver disease and predict mortality in severely decompensated cirrhosis patients[39-42]. By incorporating organ failure parameters, such as cardiovascular, renal, respiratory, neurological, hematological, and hepatic dysfunction, these criteria provide a comprehensive evaluation of the patient's condition. In the context of sepsis, the EASL-CLIF criteria can help identify cirrhotic patients at higher risk of poor outcomes and guide clinicians in making informed decisions regarding treatment strategies and resource allocation[8,38]. The CLIF-SOFA score, in particular, has shown promise in predicting short-term mortality and facilitating risk stratification in this vulnerable population[29,43-45]. By utilizing these criteria, healthcare professionals can enhance their ability to prognosticate sepsis in cirrhotic patients, thereby improving patient care and potentially reducing mortality rates. Further research and validation studies are warranted to optimize the use of EASL-CLIF criteria for prognostication and guide personalized interventions in this challenging clinical scenario[8,38].
The studies included in this systematic review provide valuable insights into the management of sepsis in patients with cirrhosis. However, these studies also have several limitations that need to be acknowledged. One of the major limitations of these studies is the absence of complete guidelines on the management of sepsis in patients with cirrhosis[37]. Although different therapeutic steps were proposed, these studies do not provide a comprehensive guide for managing these patients.
Moreover, most of the studies included in this systematic review were RCTs and cohort prospective and retrospective studies. While these studies provide strong and moderate evidence, they also have limitations in terms of generalizability. This is because most of these studies were conducted on single centers with small sample sizes. For instance, studies by Rinaldi et al[5], Philips et al[11], Maimone et al[12], Arabi et al[13], Sauneuf et al[18], Durst et al[20], Thierry et al[23] Bal et al[24], Chen et al[25], Galbois et al[27] were conducted on small sample sizes, which limits the generalizability of their findings.
Furthermore, the prospective nature of some studies can also affect the results due to missing information. For example, studies by Rinaldi et al[5], Baudry et al[9], Philips et al[11], Maimone et al[12], Arabi et al[13], Piccolo Serafim et al[14], Chang et al[17], Sauneuf et al[18] Sasso et al[19] Durst et al[20], Chebl et al[22], Thierry et al[23], Bal et al[24], and Chen et al[25], and Galbois et al[27] were conducted prospectively and some information was missing, which can affect the accuracy of the results.
Moreover, retrospective studies have their limitations as well, as not all information was present. For instance, Rinaldi et al[5], Baudry et al[9], Philips et al[11], Maimone et al[12], Arabi et al[13], Piccolo Serafim et al[14], Villarreal et al[15], Fischer et al[16] Chang et al[17], Sauneuf et al[18], Durst et al[20], Umgelter et al [21] Chebl et al[22], Thierry et al[23], Bal et al[24], Chen et al[25], Guo et al[26] and Galbois et al[27], all suffered from selection bias and missing information bias.
In addition, it is important to acknowledge that this review has certain limitations. Although we made efforts to gather relevant sources, we were unable to conduct an exhaustive search, leading to some sources remaining unexplored. This constraint resulted from the time limitations imposed during the review process. Consequently, the review may not encompass the full breadth and depth of available literature on the management of cirrhosis patients with sepsis admitted to the ICU. Furthermore, it is worth noting that a substantial proportion of the included research papers were retrospective studies with occasional missing information. To enhance the understanding and enhance outcomes in cirrhotic patients with sepsis, further research endeavors are warranted.
In conclusion, sepsis in cirrhotic patients is a complex and challenging clinical scenario. Our systematic review of the literature revealed that there is no standardized approach to the management of sepsis in cirrhotic patients admitted to the ICU. Although there is evidence to support early identification of infection, prompt administration of antibiotics, and aggressive resuscitation with fluids and vasopressors, the optimal management of these patients remains unclear. Furthermore, the studies included in this review were limited by small sample sizes, single-center designs, and missing data, highlighting the need for larger, multicenter trials to establish best practices for managing sepsis in cirrhotic patients.
Despite these limitations, our review suggests that using prognostic scores such as SOFA, MELD, and MELD-Na can help identify high-risk patients and guide clinical decision-making. Furthermore, improving outcomes in septic cirrhotic patients will require a multidisciplinary approach, including collaboration between intensivists, hepatologists, infectious disease specialists, and other healthcare providers. With the growing burden of cirrhosis and sepsis worldwide, further research is urgently needed to clarify the optimal management of this complex patient population and improve outcomes for these critically ill patients.
The background of the study lies in the physiological response of sepsis, characterized by a dysregulated inflammatory reaction to infection, which can progress to organ failure and death. Cirrhotic patients are particularly susceptible to sepsis-induced organ failure and have higher mortality rates. The imbalance of cytokine response, known as a "cytokine storm," plays a significant role in the worsening of liver function and the development of organ/system failure in severe sepsis. The severity of sepsis in cirrhotic patients is associated with increased production of proinflammatory cytokines. Additionally, cirrhotic patients with severe sepsis can experience complications such as shock, acute lung injury, coagulopathy, renal failure, or hepatic encephalopathy. Understanding the background and significance of sepsis in cirrhosis is crucial for effective management and improved outcomes.
The motivation behind this research is to address the impact of sepsis in cirrhotic patients and the associated challenges in managing this complex condition. Sepsis is a major cause of admission to intensive care units (ICUs), and its outcomes are worse in patients with comorbidities like cirrhosis. Organ dysfunction in sepsis, measured by the Sequential Organ Failure Assessment (SOFA) score, including liver failure, is linked to higher mortality rates. Defining sepsis and septic shock accurately remains challenging. Given the high mortality and complexity of sepsis in cirrhosis, understanding the key problems and finding effective solutions is crucial. Solving these problems not only improves patient outcomes but also contributes to future research in this field by providing insights into personalized interventions, risk stratification, and resource allocation.
The main objectives of this study are to determine the optimal management of sepsis in cirrhotic patients admitted to the ICU and to explore strategies for improving outcomes in this population. Realizing these objectives has significant implications for future research in this field. By identifying effective management approaches, personalized interventions can be developed to address the specific needs of cirrhotic patients with sepsis. Furthermore, understanding the impact of different interventions on mortality and organ failure rates provides valuable insights for risk stratification and resource allocation. The successful realization of these objectives contributes to the advancement of knowledge and practices in managing sepsis in cirrhotic patients, ultimately improving patient care and outcomes in this challenging clinical scenario.
This study utilized a systematic review methodology following the PRISMA-P protocol to investigate the management of sepsis in cirrhotic patients admitted to the ICU. The inclusion criteria comprised cirrhotic patients over 18 years old with sepsis in the ICU, and the analysis focused on sepsis management and prognosis in this population. English-language randomized controlled trials, retrospective cohort studies, and prospective cohort studies were considered. The outcomes assessed included survival, ICU length of stay, and overall prognosis. Searches were conducted on PubMed, Google Scholar, Embase, and Cochrane databases, with filtering based on titles and abstracts. Relevant papers underwent full-text analysis, and only those meeting the inclusion criteria were included. This systematic review offers valuable insights into sepsis management and prognosis in cirrhotic patients admitted to the ICU, utilizing a comprehensive approach to assess existing literature.
The study conducted a systematic review to investigate the management of sepsis in cirrhotic patients admitted to the ICU. The researchers selected 19 papers that met the inclusion criteria, focusing on survival and prognostic factors for this patient population. The findings indicated that albumin administration corrected hypotension in sepsis with cirrhosis, while corticosteroids improved hemodynamic status without affecting mortality. Procalcitonin was found to be helpful in diagnosing bacterial infections in cirrhotic patients, and vasopressors such as norepinephrine and terlipressin were recommended to maintain mean arterial pressure above specific thresholds. The prognosis was generally poor for cirrhotic patients with sepsis, especially for mechanically ventilated patients or those requiring vasopressors. The use of fluid resuscitation, particularly with human albumin, was recommended, and early antibiotic administration within the first hour showed improved outcomes. The qSOFA criteria were identified as a better predictor of adverse outcomes in sepsis, and echocardiography aided in diagnosing hyperdynamic syndrome. Liver transplantation was highlighted as the definitive treatment for cirrhotic patients. The study also mentioned the potential benefits and limitations of renal replacement therapy and liver support systems in sepsis management. Source control and glucose control were emphasized as essential aspects of sepsis management.
The study proposes that the current therapeutic strategies for sepsis in cirrhosis patients, which are similar to the Surviving Sepsis Campaign guidelines for the general population, may not be sufficient in reducing mortality rates in this specific patient group. It highlights the need for further research and development of comprehensive management guidelines for sepsis in cirrhosis patients. The study suggests that the use of human albumin and norepinephrine, as well as combination therapy with terlipressin and norepinephrine, may be effective in correcting hypotension and improving outcomes in cirrhosis patients with sepsis. Additionally, it indicates that early administration of vasopressors could be more beneficial than aggressive fluid administration in this patient population. However, the use of corticosteroids did not show a decrease in mortality.
Future research should focus on developing standardized management guidelines specifically tailored for sepsis in cirrhosis patients. These guidelines should encompass early detection of infection, appropriate antibiotic therapy, fluid resuscitation, vasopressor selection, and corticosteroid use. There is a need for larger, multicenter trials to validate the findings of existing studies and establish best practices for managing sepsis in cirrhosis patients. These studies should have larger sample sizes and address the limitations of previous research, such as single-center designs and missing data. Prognostic scores, such as SOFA, Model for End-Stage Liver Disease (MELD), and MELD-Na, should be further evaluated and incorporated into the management of sepsis in cirrhosis patients to identify high-risk individuals and guide treatment decisions. A multidisciplinary approach involving intensivists, hepatologists, infectious disease specialists, and other healthcare providers is essential for improving outcomes in septic cirrhotic patients. Collaboration and coordination among these specialties should be emphasized in future research and clinical practice.
We would like to extend our sincere appreciation to the Acute Medicine MSc program at the University of South Wales for their invaluable assistance in our work. We acknowledge and commend the University of South Wales for their commitment to providing advanced problem-solving skills and life-long learning opportunities for healthcare professionals.
| 1. | Gustot T, Durand F, Lebrec D, Vincent JL, Moreau R. Severe sepsis in cirrhosis. Hepatology. 2009;50:2022-2033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 331] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 2. | Gustot T, Felleiter P, Pickkers P, Sakr Y, Rello J, Velissaris D, Pierrakos C, Taccone FS, Sevcik P, Moreno C, Vincent JL; EPIC II Group of Investigators. Impact of infection on the prognosis of critically ill cirrhotic patients: results from a large worldwide study. Liver Int. 2014;34:1496-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 18772] [Article Influence: 1877.2] [Reference Citation Analysis (4)] |
| 4. | Lambden S, Laterre PF, Levy MM, Francois B. The SOFA score-development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23:374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 377] [Cited by in RCA: 608] [Article Influence: 86.9] [Reference Citation Analysis (0)] |
| 5. | Rinaldi L, Ferrari E, Marietta M, Donno L, Trevisan D, Codeluppi M, Busani S, Girardis M. Effectiveness of sepsis bundle application in cirrhotic patients with septic shock: a single-center experience. J Crit Care. 2013;28:152-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Gantner D, Nichol AD. Treatment of severe sepsis. Anaesthesia and Intensive Care Medicine. 13:199-203. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Simonetto DA, Piccolo Serafim L, Gallo de Moraes A, Gajic O, Kamath PS. Management of Sepsis in Patients With Cirrhosis: Current Evidence and Practical Approach. Hepatology. 2019;70:418-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Rashed E, Soldera J. CLIF-SOFA and CLIF-C scores for the prognostication of acute-on-chronic liver failure and acute decompensation of cirrhosis: A systematic review. World J Hepatol. 2022;14:2025-2043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (2)] |
| 9. | Baudry T, Hernu R, Valleix B, Jahandiez V, Faucher E, Simon M, Cour M, Argaud L. Cirrhotic Patients Admitted to the ICU With Septic Shock: Factors Predicting Short and Long-Term Outcome. Shock. 2019;52:408-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 10. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3:e123-e130. [PubMed] |
| 11. | Philips CA, Maiwall R, Sharma MK, Jindal A, Choudhury AK, Kumar G, Bhardwaj A, Mitra LG, Agarwal PM, Sarin SK. Comparison of 5% human albumin and normal saline for fluid resuscitation in sepsis induced hypotension among patients with cirrhosis (FRISC study): a randomized controlled trial. Hepatol Int. 2021;15:983-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 12. | Maimone S, Tripodi VF, Mazzeo AT. Response to: A randomized-controlled trial comparing 20% albumin to plasmalyte in patients with cirrhosis and sepsis-induced hypotension [ALPS trial]. J Hepatol. 2022;77:1731-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Arabi YM, Aljumah A, Dabbagh O, Tamim HM, Rishu AH, Al-Abdulkareem A, Knawy BA, Hajeer AH, Tamimi W, Cherfan A. Low-dose hydrocortisone in patients with cirrhosis and septic shock: a randomized controlled trial. CMAJ. 2010;182:1971-1977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 14. | Piccolo Serafim L, Simonetto DA, Anderson AL, Choi DH, Weister TJ, Hanson AC, Kamath PS, Gajic O, Gallo de Moraes A. Clinical Effect of Systemic Steroids in Patients with Cirrhosis and Septic Shock. Shock. 2021;56:916-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Villarreal E, Vacacela K, Gordon M, Calabuig C, Alonso R, Ruiz J, Kot P, Babiloni D, Ramírez P. [Usefulness of procalcitonin for diagnosing infection in critically ill patients with liver cirrhosis]. Med Intensiva. 2016;40:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Fischer P, Grigoras C, Bugariu A, Nicoara-Farcau O, Stefanescu H, Benea A, Hadade A, Margarit S, Sparchez Z, Tantau M, Ionescu D, Procopet B. Are presepsin and resistin better markers for bacterial infection in patients with decompensated liver cirrhosis? Dig Liver Dis. 2019;51:1685-1691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Chang YC, Fang YT, Chen HC, Lin CY, Chang YP, Tsai YH, Chen YM, Huang KT, Chang HC, Wang CC, Lin MC, Fang WF. The Survival of Septic Patients with Compensated Liver Cirrhosis Is Not Inferior to That of Septic Patients without Liver Cirrhosis: A Propensity Score Matching Analysis. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Sauneuf B, Champigneulle B, Soummer A, Mongardon N, Charpentier J, Cariou A, Chiche JD, Mallet V, Mira JP, Pène F. Increased survival of cirrhotic patients with septic shock. Crit Care. 2013;17:R78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Sasso R, Lauzon S, Rockey DC. Cirrhotic Patients on Mechanical Ventilation Have a Low Rate of Successful Extubation and Survival. Dig Dis Sci. 2020;65:3744-3752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Durst MM, Eitzen EA, Benken ST. Comparison of Vasopressor Duration in Septic Shock Patients With and Without Cirrhosis. Ann Pharmacother. 2021;55:970-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Umgelter A, Reindl W, Schmid RM, Huber W. Continuous terlipressin infusion in patients with persistent septic shock and cirrhosis of the liver. Intensive Care Med. 2008;34:390-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Chebl RB, Tamim H, Sadat M, Qahtani S, Dabbagh T, Arabi YM. Outcomes of septic cirrhosis patients admitted to the intensive care unit: A retrospective cohort study. Medicine (Baltimore). 2021;100:e27593. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 23. | Thierry S, Giroux Leprieur E, Lecuyer L, Brocas E, Van de Louw A. Echocardiographic features, mortality, and adrenal function in patients with cirrhosis and septic shock. Acta Anaesthesiol Scand. 2008;52:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Bal CK, Daman R, Bhatia V. Predictors of fifty days in-hospital mortality in decompensated cirrhosis patients with spontaneous bacterial peritonitis. World J Hepatol. 2016;8:566-572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Chen HY, Hsu YC. Afebrile Bacteremia in Adult Emergency Department Patients with Liver Cirrhosis: Clinical Characteristics and Outcomes. Sci Rep. 2020;10:7617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 26. | Guo F, Feng YC, Zhao G, Wu HL, Xu L, Zhao J, Lv J, Han ST, Huang YC, Ma XM. The Leukocyte VCS Parameters Compared with Procalcitonin, Interleukin-6, and Soluble Hemoglobin Scavenger Receptor sCD163 for Prediction of Sepsis in Patients with Cirrhosis. Dis Markers. 2019;2019:1369798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Galbois A, Bigé N, Pichereau C, Boëlle PY, Baudel JL, Bourcier S, Maury E, Guidet B, Ait-Oufella H. Exploration of skin perfusion in cirrhotic patients with septic shock. J Hepatol. 2015;62:549-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Fagiuoli S, Colli A, Bruno R, Burra P, Craxì A, Gaeta GB, Grossi P, Mondelli MU, Puoti M, Sagnelli E, Stefani S, Toniutto P. Management of infections in cirrhotic patients: report of a consensus conference. Dig Liver Dis. 2014;46:204-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 29. | Jacques ROC, Massignan LS, Winkler MS, Balbinot RS, Balbinot RA, Balbinot SS, Soldera J. Liver-specific scores as predictors of mortality in spontaneous bacterial peritonitis. GastroHep. 2020;2:224-231. [DOI] [Full Text] |
| 30. | Yuan LT, Chuah SK, Yang SC, Liang CM, Wu CK, Tai WC, Hung TH, Nguang SH, Wang JW, Tseng KL, Ku MK, Hsu PI, Wu DC, Hsu CN. Multiple bacterial infections increase the risk of hepatic encephalopathy in patients with cirrhosis. PLoS One. 2018;13:e0197127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Hung TH, Tseng CW, Tsai CC, Lee HF. Effect of proton pump inhibitors on mortality of cirrhotic patients with pneumonia. PLoS One. 2019;14:e0216041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Christou L, Pappas G, Falagas ME. Bacterial infection-related morbidity and mortality in cirrhosis. Am J Gastroenterol. 2007;102:1510-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 149] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 33. | Piano S, Tonon M, Angeli P. Changes in the epidemiology and management of bacterial infections in cirrhosis. Clin Mol Hepatol. 2021;27:437-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 34. | Lan P, Wang SJ, Shi QC, Fu Y, Xu QY, Chen T, Yu YX, Pan KH, Lin L, Zhou JC, Yu YS. Comparison of the predictive value of scoring systems on the prognosis of cirrhotic patients with suspected infection. Medicine (Baltimore). 2018;97:e11421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Choudhury A, Kedarisetty CK, Vashishtha C, Saini D, Kumar S, Maiwall R, Sharma MK, Bhadoria AS, Kumar G, Joshi YK, Sarin SK. A randomized trial comparing terlipressin and noradrenaline in patients with cirrhosis and septic shock. Liver Int. 2017;37:552-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 36. | Terres AZ, Balbinot RS, Muscope ALF, Longen ML, Schena B, Cini BT, Luis Rost G Jr, Balensiefer JIL, Eberhardt LZ, Balbinot RA, Balbinot SS, Soldera J. Evidence-based protocol for diagnosis and treatment of hepatorenal syndrome is independently associated with lower mortality. Gastroenterol Hepatol. 2022;45:25-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 37. | Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M, Prescott HC, Schorr C, Simpson S, Wiersinga WJ, Alshamsi F, Angus DC, Arabi Y, Azevedo L, Beale R, Beilman G, Belley-Cote E, Burry L, Cecconi M, Centofanti J, Coz Yataco A, De Waele J, Dellinger RP, Doi K, Du B, Estenssoro E, Ferrer R, Gomersall C, Hodgson C, Møller MH, Iwashyna T, Jacob S, Kleinpell R, Klompas M, Koh Y, Kumar A, Kwizera A, Lobo S, Masur H, McGloughlin S, Mehta S, Mehta Y, Mer M, Nunnally M, Oczkowski S, Osborn T, Papathanassoglou E, Perner A, Puskarich M, Roberts J, Schweickert W, Seckel M, Sevransky J, Sprung CL, Welte T, Zimmerman J, Levy M. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47:1181-1247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 295] [Cited by in RCA: 2810] [Article Influence: 562.0] [Reference Citation Analysis (0)] |
| 38. | Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, Durand F, Gustot T, Saliba F, Domenicali M, Gerbes A, Wendon J, Alessandria C, Laleman W, Zeuzem S, Trebicka J, Bernardi M, Arroyo V; CANONIC Study Investigators of the EASL–CLIF Consortium. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144:1426-1437, 1437.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1720] [Cited by in RCA: 2269] [Article Influence: 174.5] [Reference Citation Analysis (6)] |
| 39. | Grochot RM, Luz LB, Garcia R, Balbinot RÂ, Balbinot SS, Soldera J. Acute–on–chronic liver failure data from a teaching hospital in Brazil. A Historical Cohort. Inter J Sci Res. 2020;9:1-6. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Reference Citation Analysis (0)] |
| 40. | Silva PE, Fayad L, Lazzarotto C, Ronsoni MF, Bazzo ML, Colombo BS, Dantas-Correa EB, Narciso-Schiavon JL, Schiavon LL. Single-centre validation of the EASL-CLIF consortium definition of acute-on-chronic liver failure and CLIF-SOFA for prediction of mortality in cirrhosis. Liver Int. 2015;35:1516-1523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 41. | Terres AZ, Balbinot RS, Muscope ALF, Longen ML, Schena B, Cini BT, Rost Jr GL, Leichtweis Balensiefer JI, Eberhardt LZ, Balbinot RA, Balbinot SS, Soldera J. Acute-on-chronic liver failure is independently associated with higher mortality for cirrhotic patients with acute esophageal variceal hemorrhage: Retrospective cohort study. World J Clin Cases. 2023;11:4003-4018. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (2)] |
| 42. | Jacques ROC, Massignan LDS, Winkler MS, Balbinot RS, Balbinot SS, Soldera J. Acute-on-Chronic Liver Failure is Independently Associated With Lower Survival in Patients with Spontaneous Bacterial Peritonitis. Arq Gastroenterol. 2021;58:344-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Reference Citation Analysis (0)] |
| 43. | Grochot RM, Luz LB, Garcia R, Balbinot RA, Balbinot SS, Soldera J. CLIF-SOFA is superior to other liver-specific scores for predicting mortality in acute-on-chronic liver failure and decompensated cirrhosis. Austin J Gastroenterol. 2019;6:1105. |
| 44. | Terres AZ, Balbinot RS, Muscope ALF, Longen ML, Schena B, Cini BT, Rost Jr GL, Leichtweis Balensiefer JI, Eberhardt LZ, Balbinot RA, Balbinot SS, Soldera J. Predicting mortality for hepatorenal syndrome with liver-specific scores. GastroHep. 2020;2:336-343. [DOI] [Full Text] |
| 45. | Terres AZ, Balbinot RS, Muscope ALF, Eberhardt LZ, Balensiefer JIL, Cini BT, Luis Rost G Jr, Longen ML, Schena B, Balbinot RA, Balbinot SS, Soldera J. Predicting mortality for cirrhotic patients with acute oesophageal variceal haemorrhage using liver-specific scores. GastroHep. 2021;3:236-246. [DOI] [Full Text] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Federação Brasileira De Gastroenterologia; Sociedade Brasileira de Hepatologia.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Thomson M, United States; Xie Q, China S-Editor: Ma YJ L-Editor: A P-Editor: Cai YX