Published online Feb 27, 2023. doi: 10.4254/wjh.v15.i2.123
Peer-review started: August 29, 2022
First decision: November 17, 2022
Revised: November 19, 2022
Accepted: January 31, 2023
Article in press: January 31, 2023
Published online: February 27, 2023
Processing time: 178 Days and 20.5 Hours
An international panel recently proposed an update to the terminology and diagnostic criteria for fatty liver disease. The experts proposed a change in the nomenclature from non-alcoholic fatty liver disease (NAFLD) to metabolic (dysfunction)-associated fatty liver disease (MAFLD). This single-letter change, we believe, heralds the dawn of a new era in clinical practice and in clinical and basic research as well. The new nomenclature with the easily applicable approach has stimulated the enthusiasm of the researchers worldwide, resulting in a large number of publications over the past two years. Several recent studies have provided tremendous evidence of the superiority of the MAFLD criteria over the NAFLD criteria. Many studies in different geographic areas of the world incl
Core Tip: An international panel recently proposed an update to the terminology and diagnostic criteria for fatty liver disease. The authors proposed a change in the nomenclature from non-alcoholic fatty liver disease (NAFLD) to metabolic (dysfunction)-associated fatty liver disease (MAFLD). Several studies have been published recently, and showed tremendous evidence of the superiority of MAFLD criteria over NAFLD criteria. Consequently, many societies, physician and nurse groups, health stakeholders, representatives of regulatory sciences, and others endorsed the new nomenclature.
- Citation: Fouad Y. Metabolic-associated fatty liver disease: New nomenclature and approach with hot debate. World J Hepatol 2023; 15(2): 123-128
- URL: https://www.wjgnet.com/1948-5182/full/v15/i2/123.htm
- DOI: https://dx.doi.org/10.4254/wjh.v15.i2.123
The World Health Organization (WHO) has motivated scientists, doctors, and healthcare providers to use the appropriate medical terms and change the terms according to the patient's interest and the medical care provided. This call by the WHO was to overcome the stigmas and inaccuracies that may confer upon people, regions, and economies[1].
In the recent medical history, renaming of the diseases involved primary biliary cirrhosis, schizophrenia, epilepsy, autism, and others with ongoing trials to change the term ‘’noncommunicable diseases’’ to a better positive name to gain more medical support by governments, societies, and stakeholders[2].
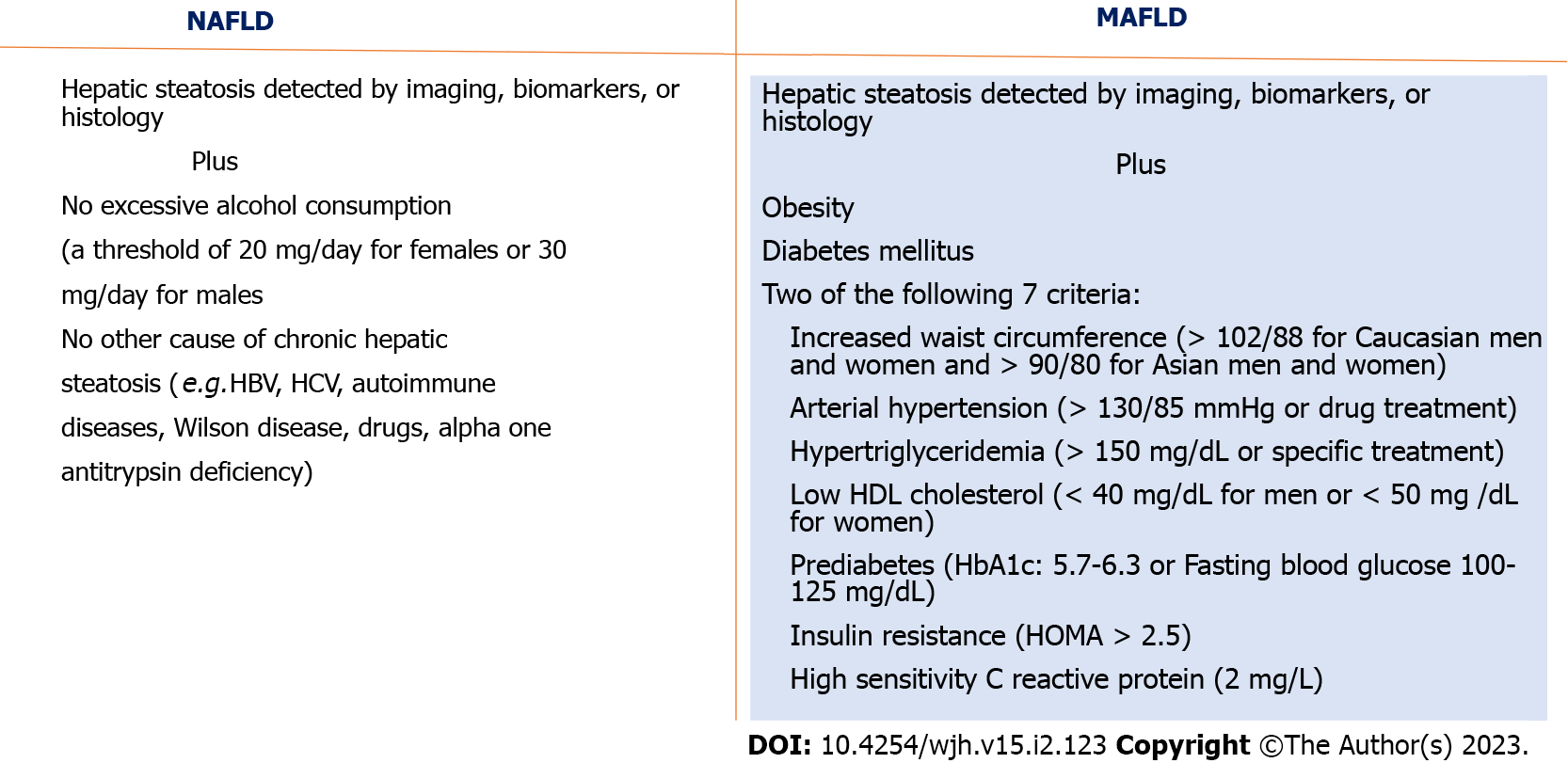
Since 1980 when the non-alcoholic fatty liver disease (NAFLD) was introduced[3], several trials have been carried out to rename the disease by different scientists and societies for different reasons. In 2019, Eslam et al[4] proposed changing the traditional NAFLD to metabolic dysfunction-associated liver disease (MAFLD). The single-letter change means a lot for researchers, physicians, and patients. The authors explained their vision of new nomenclature by linking the fatty liver to the metabolic syndrome which is the most common and most serious etiology of fatty liver diseases and under-evaluated when using the older nomenclature. Moreover, the new nomenclature gives the clinical community a chance to avoid the stigma of alcohol intake, avoid the negativity of NAFLD nomenclature, and overcomes trivialization[2]. The simplified criteria for diagnosis of MAFLD were put forward by consensus of an international panel of hepatologists in 2020[5]. These criteria pave the way for easy diagnosis of fatty liver diseases because of easy applicability. The consensus considered the diagnosis of MAFLD based on the presence of steatosis by imaging or histopathology in addition to the presence of diabetes mellitus or obesity/overweight or two out of seven metabolic dysfunction criteria (Figure 1). The new nomenc
The new nomenclature with the easily applicable approach stimulated the enthusiasm of researchers worldwide, resulting in a large number of publications over the last two years. Several studies have been published recently, showing tremendous evidence of the superiority of MAFLD criteria over NAFLD criteria. Many studies in different geographic areas of the world including the United States (US), Europe, and Asia on a large number of patients proved that the utility of MAFLD criteria was higher than that of the NAFLD criteria in different aspects of fatty liver diseases.
Among the many important findings, MAFLD criteria could better identify patients at risk of liver fibrosis than the NAFLD criteria in the American population[6]. High diagnostic ability of fatty liver index in the detection of steatosis was seen in patients with MAFLD[7]. Fibrosis-4 index and NAFLD fibrosis score could confidently be used to exclude advanced fibrosis in overweight, obese, and severely obese patients with MAFLD[8]. MAFLD is associated with a higher incidence of hepatocellular carcinoma[9]. MAFLD (not NAFLD) predicts extrahepatic malignancy[10]. MAFLD was better than NAFLD in identifying patients at high risk of renal diseases[11]. In a recent meta-analysis, MAFLD was associated with increased severity of COVID-19[12]. Renaming to MAFLD increases awareness of the disease among primary care providers and physicians in other specialties[13]. Change to MAFLD has a positive impact on clinical trials[14,15] MAFLD identifies the severity of the coexistence of fatty liver disease with other liver diseases[16,17].
Being convinced by the reasons for changing nomenclature, evidence of the superiority of the new name MAFLD, and the benefits of the new nomenc
| Type of endorsement | Endorsed by | Ref. |
| Guidelines | APASL | [25] |
| Guidelines | Egyptian EMRG group | [26] |
| Consensus statement | Middle East and North Africa group | [27] |
| View point (perspectives) | International nurse and allied health groups | [28] |
| Position statement | ALEH | [29] |
| Position statement | The Chinese Society of Hepatology | [30] |
| Position statement | ISTP | [31] |
| Position statement | Arabic Association for the Study of Diabetes and Metabolism | [32] |
| Consensus statement | Malaysian Society of Gastroenterology and Hepatology | [33] |
| Viewpoint (perspectives) | International leaders in regulatory science and drug development | [34] |
| Position statement | International representatives of patient advocacy groups | [35] |
| Letter of endorsement | Global multi-stakeholder from more than 135 countries worldwide | [36] |
| Editorial of endorsement | Spanish Society of Gastroenterology | [37] |
Two major hepatology societies, The European Association for Study of the Liver and The American Association for the Study of Liver Diseases, have not endorsed the new name yet till writing this editorial. The debate from these societies focused mainly on the prematurity of change[18]. One of the main debates is about non-metabolic or lean NAFLD. Evidence proved that the non-metabolic NAFLD group seems to be comparable to subjects with no fatty liver in terms of cardiovascular-related mortality as well as all-cause mortality. Moreover, the non-metabolic NAFLD group seems to be at a very low risk of fibrosis (0.8%)[19]. Another concern was about pediatric NAFLD. In a recent study involving 1446 US adolescents aged 12–18 years from the National Health and Nutrition Examination Survey III, MAFLD criteria were met by most of these US adolescents with elastographic evidence of steatosis[20]. Additional debate was about clinical trials. In a recently published paper, a group of researchers declared that the new name and approach with positive inclusion criteria lead to easier recruitment of patients and are more likely to give positive results[21]. Being in the era of evidence-based medicine, we believe that the need for an evidence-based debate is mandatory. Once again, the MAFLD conceptual framework removes the concept that there is no alcohol involvement, links the liver disease which is commonly seen in metabolic dysregulation with its systemic effects, and performs better in patient identification, risk stratification, disease awareness, and networking with metabolic disease physicians[22,23].
The important question in the current situation is why some experts do not change their attitude toward the new nomenclature despite the obvious conspicuous evidence. The answer is not clear although, pleasingly, since the very beginning, the weight of evidence appears to have led to the persuasion of an ever-increasing number of stakeholders on the increasing benefits. Another important issue is that experts who advocate against the redefinition despite the robust evidence should explain to the hepatology community how and why we discard the rapidly progressive growing body of new literature[24].
In summary, we have a redefinition of a very prevalent disease worldwide. The new nomenclature MAFLD is simple, with superior utility, and is supported by a tremendous amount of evidence. It is endorsed by many societies and full global adoption is a matter of time.
| 1. | Gladstonemay R. WHO urges more care in naming diseases. New York, NY: New York Times. [Internet] [accessed 8 May 2015]. Available from: https://www.seattletimes.com/nation-world/who-urges-more-care-in-naming-diseases/. |
| 2. | Fouad Y, Waked I, Bollipo S, Gomaa A, Ajlouni Y, Attia D. What's in a name? Liver Int. 2020;40:1254-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 217] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 3. | Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434-438. [PubMed] |
| 4. | Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology. 2020;158:1999-2014.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2367] [Cited by in RCA: 2427] [Article Influence: 404.5] [Reference Citation Analysis (4)] |
| 5. | Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, Zelber-Sagi S, Wai-Sun Wong V, Dufour JF, Schattenberg JM, Kawaguchi T, Arrese M, Valenti L, Shiha G, Tiribelli C, Yki-Järvinen H, Fan JG, Grønbæk H, Yilmaz Y, Cortez-Pinto H, Oliveira CP, Bedossa P, Adams LA, Zheng MH, Fouad Y, Chan WK, Mendez-Sanchez N, Ahn SH, Castera L, Bugianesi E, Ratziu V, George J. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73:202-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2883] [Cited by in RCA: 3199] [Article Influence: 533.2] [Reference Citation Analysis (2)] |
| 6. | Wang X, Wu S, Yuan X, Chen S, Fu Q, Sun Y, Lan Y, Hu S, Wang Y, Lu Y, Qu S, Wang L. Metabolic Dysfunction-associated Fatty Liver Disease and Mortality Among Chinese Adults: a Prospective Cohort Study. J Clin Endocrinol Metab. 2022;107:e745-e755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 7. | Kim D, Konyn P, Sandhu KK, Dennis BB, Cheung AC, Ahmed A. Metabolic dysfunction-associated fatty liver disease is associated with increased all-cause mortality in the United States. J Hepatol. 2021;75:1284-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 327] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 8. | Eren F, Kaya E, Yilmaz Y. Accuracy of Fibrosis-4 index and non-alcoholic fatty liver disease fibrosis scores in metabolic (dysfunction) associated fatty liver disease according to body mass index: failure in the prediction of advanced fibrosis in lean and morbidly obese individuals. Eur J Gastroenterol Hepatol. 2022;34:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 9. | Lin YP, Wang PM, Chuang CH, Yong CC, Liu YW, Huang PY, Yao CC, Tsai MC. Metabolic Risks Are Increasing in Non-B Non-C Early-Stage Hepatocellular Carcinoma: A 10-Year Follow-Up Study. Front Oncol. 2022;12:816472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, Wu Y, Wang X, Zhu Y. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40:2082-2089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 411] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 11. | Liang Y, Chen H, Liu Y, Hou X, Wei L, Bao Y, Yang C, Zong G, Wu J, Jia W. Association of MAFLD With Diabetes, Chronic Kidney Disease, and Cardiovascular Disease: A 4.6-Year Cohort Study in China. J Clin Endocrinol Metab. 2022;107:88-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 149] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 12. | Pan L, Huang P, Xie X, Xu J, Guo D, Jiang Y. Metabolic associated fatty liver disease increases the severity of COVID-19: A meta-analysis. Dig Liver Dis. 2021;53:153-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 63] [Article Influence: 12.6] [Reference Citation Analysis (1)] |
| 13. | Fouad Y, Gomaa A, Semida N, Ghany WA, Attia D. Change from NAFLD to MAFLD increases the awareness of fatty liver disease in primary care physicians and specialists. J Hepatol. 2021;74:1254-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 14. | Pan Z, Fan JG, Eslam M. An update on drug development for the treatment of metabolic (dysfunction) associated fatty liver disease: Progress and opportunities. Curr Opin Pharmacol. 2021;60:170-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Eslam M, George J. MAFLD: Now is the time to capitalize on the momentum. J Hepatol. 2021;74:1262-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Mak LY, Yuen MF, Seto WK. Letter regarding "A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement". J Hepatol. 2020;73:1573-1574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 17. | van Kleef LA, Choi HSJ, Brouwer WP, Hansen BE, Patel K, de Man RA, Janssen HLA, de Knegt RJ, Sonneveld MJ. Metabolic dysfunction-associated fatty liver disease increases risk of adverse outcomes in patients with chronic hepatitis B. JHEP Rep. 2021;3:100350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 77] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 18. | Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z, Cohen DE, Loomba R. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology. 2021;73:1194-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 307] [Article Influence: 61.4] [Reference Citation Analysis (0)] |
| 19. | Tsutsumi T, Kawaguchi T, Nakano D, Torimura T. Atherosclerotic cardiovascular disease in non-metabolic nonalcoholic fatty liver disease. Hepatol Res. 2022;52:317-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Ciardullo S, Carbone M, Invernizzi P, Perseghin G. Impact of the new definition of metabolic dysfunction-associated fatty liver disease on detection of significant liver fibrosis in US adolescents. Hepatol Commun. 2022;6:2070-2078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 21. | Eslam M, Ahmed A, Després JP, Jha V, Halford JCG, Wei Chieh JT, Harris DCH, Nangaku M, Colagiuri S, Targher G, Joshi S, Byrne CD, Khunti K, Nguyen MH, Gish RG, George J. Incorporating fatty liver disease in multidisciplinary care and novel clinical trial designs for patients with metabolic diseases. Lancet Gastroenterol Hepatol. 2021;6:743-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 22. | Méndez-Sánchez N, Díaz-Orozco L, Córdova-Gallardo J. Redefinition of fatty liver disease from NAFLD to MAFLD raised disease awareness: Mexican experience. J Hepatol. 2021;75:221-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 23. | Eslam M, Ratziu V, George J. Yet more evidence that MAFLD is more than a name change. J Hepatol. 2021;74:977-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 24. | Fouad Y, Dufour JF, Zheng MH, Bollipo S, Desalegn H, Grønbaek H, Gish RG. The NAFLD-MAFLD debate: Is there a Consensus-on-Consensus methodology? Liver Int. 2022;42:742-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 25. | Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, Zheng MH, Shiha G, Yilmaz Y, Gani R, Alam S, Dan YY, Kao JH, Hamid S, Cua IH, Chan WK, Payawal D, Tan SS, Tanwandee T, Adams LA, Kumar M, Omata M, George J. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 617] [Article Influence: 102.8] [Reference Citation Analysis (3)] |
| 26. | Fouad Y, Esmat G, Elwakil R, Zakaria S, Yosry A, Waked I, El-Razky M, Doss W, El-Serafy M, Mostafa E, Anees M, Sakr MA, AbdelAty N, Omar A, Zaki S, Al-Zahaby A, Mahfouz H, Abdalla M, Albendary M, Hamed AK, Gomaa A, Hasan A, Abdel-Baky S, El Sahhar M, Shiha G, Attia D, Saeed E, Kamal E, Bazeed S, Mehrez M, Abdelaleem S, Gaber Y, Abdallah M, Salama A, Tawab DA, Nafady S. The egyptian clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Saudi J Gastroenterol. 2022;28:3-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 27. | Shiha G, Alswat K, Al Khatry M, Sharara AI, Örmeci N, Waked I, Benazzouz M, Al-Ali F, Hamed AE, Hamoudi W, Attia D, Derbala M, Sharaf-Eldin M, Al-Busafi SA, Zaky S, Bamakhrama K, Ibrahim N, Ajlouni Y, Sabbah M, Salama M, Anushiravani A, Afredj N, Barakat S, Hashim A, Fouad Y, Soliman R. Nomenclature and definition of metabolic-associated fatty liver disease: a consensus from the Middle East and north Africa. Lancet Gastroenterol Hepatol. 2021;6:57-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 118] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 28. | Clayton M, Fabrellas N, Luo J, Alghamdi MG, Hafez A, Qadiri TA, Owise N, Attia D. From NAFLD to MAFLD: Nurse and allied health perspective. Liver Int. 2021;41:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 29. | Mendez-Sanchez N, Arrese M, Gadano A, Oliveira CP, Fassio E, Arab JP, Chávez-Tapia NC, Dirchwolf M, Torre A, Ridruejo E, Pinchemel-Cotrim H, Castellanos Fernández MI, Uribe M, Girala M, Diaz-Ferrer J, Restrepo JC, Padilla-Machaca M, Dagher L, Gatica M, Olaechea B, Pessôa MG, Silva M. The Latin American Association for the Study of the Liver (ALEH) position statement on the redefinition of fatty liver disease. Lancet Gastroenterol Hepatol. 2021;6:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 30. | Nan Y, An J, Bao J, Chen H, Chen Y, Ding H, Dou X, Duan Z, Fan J, Gao Y, Han T, Han Y, Hu P, Huang Y, Jia J, Jiang J, Jiang Y, Li J, Li R, Li S, Li W, Li Y, Lin S, Liu J, Liu S, Lu L, Lu Q, Luo X, Ma X, Rao H, Ren H, Ren W, Shang J, Shi L, Su M, Wang B, Wang R, Wei L, Wen Z, Wu B, Wu J, Xin S, Xing H, Xu J, Yan M, Yang J, Yang L, Yang Y, Yu Y, Zhang L, Zhang X, Zhang Y, Zhao J, Zhao S, Zheng H, Zhou Y, Zhuang H, Zuo W, Xu X, Qiao L. The Chinese Society of Hepatology position statement on the redefinition of fatty liver disease. J Hepatol. 2021;75:454-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 100] [Article Influence: 20.0] [Reference Citation Analysis (3)] |
| 31. | El-Shabrawi M, Memon I, Attia D, El-Koofy NM. The International Society of Tropical Paediatrics (ISTP) endorses the redefinition of fatty liver disease. J Hepatol. 2022;76:738-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Shaltout I, Alkandari H, Fouad Y, Hamed AE. Arabic Association for the Study of Diabetes and Metabolism (AASD) endorsing the MAFLD definition of fatty liver disease. J Hepatol. 2022;76:739-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Chan WK, Tan SS, Chan SP, Lee YY, Tee HP, Mahadeva S, Goh KL, Ramli AS, Mustapha F, Kosai NR, Raja Ali RA. Malaysian Society of Gastroenterology and Hepatology consensus statement on metabolic dysfunction-associated fatty liver disease. J Gastroenterol Hepatol. 2022;37:795-811. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 34. | Fouad Y, Palmer M, Chen M, Regev A, Banerjee R, Myers R, Riccio R, Torstenson R, Younes R, Arora PS, Landgren H, Karsdal MA, Blake M, Shapiro DA, Gruss HJ, Sheikh MY, Attia D, Bollipo S, Smith AD, Freilich B, Gish RG, Schuppan D. Redefinition of Fatty Liver Disease from NAFLD to MAFLD through the Lens of Drug Development and Regulatory Science. J Clin Transl Hepatol. 2022;10:374-382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 35. | Shiha G, Korenjak M, Eskridge W, Casanovas T, Velez-Moller P, Högström S, Richardson B, Munoz C, Sigurðardóttir S, Coulibaly A, Milan M, Bautista F, Leung NWY, Mooney V, Obekpa S, Bech E, Polavarapu N, Hamed AE, Radiani T, Purwanto E, Bright B, Ali M, Dovia CK, McColaugh L, Koulla Y, Dufour JF, Soliman R, Eslam M. Redefining fatty liver disease: an international patient perspective. Lancet Gastroenterol Hepatol. 2021;6:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 149] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 36. | Méndez-Sánchez N, Bugianesi E, Gish RG, Lammert F, Tilg H, Nguyen MH, Sarin SK, Fabrellas N, Zelber-Sagi S, Fan JG, Shiha G, Targher G, Zheng MH, Chan WK, Vinker S, Kawaguchi T, Castera L, Yilmaz Y, Korenjak M, Spearman CW, Ungan M, Palmer M, El-Shabrawi M, Gruss HJ, Dufour JF, Dhawan A, Wedemeyer H, George J, Valenti L, Fouad Y, Romero-Gomez M, Eslam M; Global multi-stakeholder consensus on the redefinition of fatty liver disease. Global multi-stakeholder endorsement of the MAFLD definition. Lancet Gastroenterol Hepatol. 2022;7:388-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 195] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 37. | Romero-Gómez M, Ampuero J. Looking for a new name for non-alcoholic fatty liver disease in Spanish: esteatosis hepática metabólica (EHmet). Rev Esp Enferm Dig. 2021;113:161-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: European Association for the Study of the Liver, 14229; Asian Pacific Association for the Study of the Liver, 2217.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ko HL, Singapore; Kocak A, Turkey; Li HL, China S-Editor: Liu GL L-Editor: Wang TQ P-Editor: Liu GL