Published online Dec 27, 2021. doi: 10.4254/wjh.v13.i12.2128
Peer-review started: June 29, 2021
First decision: August 18, 2021
Revised: August 24, 2021
Accepted: November 15, 2021
Article in press: November 15, 2021
Published online: December 27, 2021
Processing time: 181 Days and 3.4 Hours
Alcoholic liver cirrhosis (ALC) is a chronic liver disease with varying disease severity. Readmissions of ALC are associated with poor outcomes.
To identify and assess trends of readmissions for ALC over an eight-year period.
This retrospective interrupted trend study analysed 30-d readmissions of ALC in the United States from 2010 to 2018 using the National Readmissions Database. Hospitalization for ALC was the reason for index admission obtained using the International Classification of Diseases codes (571.2 and K70.3X). Biodemographic characteristics and hospitalization trends were highlighted over time. A multivariate regression analysis model was used to calculate the trend for risk-adjusted odds of 30-d all-cause ALC readmissions, ALC specific readmission rate, ALC readmission proportion, inpatient mortality, mean length of stay (LOS) and mean total hospital cost (THC) following adjustments for age, gender, grouped Charlson Comorbidity Index, insurance, mean household income, and hospital characteristics.
There was a trend towards increasing total 30-d readmissions of ALC from 7660 in 2010 to 15085 in 2018 (P < 0.001). Patients readmitted for ALC were noted to have an increasing comorbidity burden over time. We noted a rise in the risk-adjusted 30-d all-cause readmission of ALC from 24.9% in 2010 to 29.9% in 2018 (P < 0.001). ALC-specific readmission rate increased from 6.3% in 2010 to 8.4% in 2018 (P < 0.001) while ALC readmission proportion increased from 31.4% in 2010 to 36.3% in 2018 (P < 0.001). Inpatient mortality for 30-d readmissions of ALC declined from 10.5% in 2010 to 8.2% in 2018 (P = 0.0079). However, there was a trend towards increasing LOS from 5.6 d in 2010 to 6.3 d in 2018 (P < 0.001) and increasing THC from 13790 dollars in 2010 to 17150 dollars in 2018 (P < 0.001). The total days of hospital stay attributable to 30-d readmissions of ALC increased by 119.2% while the total attributable hospital costs increased by 149% by the end of 2018.
There was an increase in the 30-d readmission rate and comorbidity burden for ALC; however, inpatient mortality declined. Additionally, there was a trend towards increasing LOS and THC for these readmissions.
Core Tip: This retrospective interrupted trend study analysed 30-d readmissions of alcoholic liver cirrhosis (ALC) in the United States from 2010-2018. There was a trend towards increasing 30-d all-cause readmission rate and ALC-specific readmission rate for the study period. However, inpatient mortality was noted to have a declining trend from 10.5% in 2010 to 8.2% in 2018 (P = 0.0079). The total days of hospital stay attributable to ALC readmissions increased by 119.2% and total attributable hospital costs increased by 149% during the study period.
- Citation: Kichloo A, El-Amir Z, Dahiya DS, Wani F, Singh J, Solanki D, Edigin E, Eseaton P, Mehboob A, Shaka H. Trends of alcoholic liver cirrhosis readmissions from 2010 to 2018: Rates and healthcare burden associated with readmissions. World J Hepatol 2021; 13(12): 2128-2136
- URL: https://www.wjgnet.com/1948-5182/full/v13/i12/2128.htm
- DOI: https://dx.doi.org/10.4254/wjh.v13.i12.2128
Alcohol use disorders are known to affect millions worldwide, and alcohol consumption is directly associated with liver disease mortality. Alcoholic liver disease varies in severity and prognosis based on several factors, including the pattern of alcohol consumption, duration of alcohol consumption, amount of alcohol consumption, the presence or absence of liver inflammation, nutritional status, genetic predisposition, and diet[1]. Alcoholic liver cirrhosis (ALC) is closely associated not only with the duration of alcohol consumption, but also the amount of undiluted alcohol consumed[1]. Although many patients with significant alcohol consumption develop fatty liver disease, not all patients with alcoholic liver disease progress to liver cirrhosis. It has also been postulated that genetic and environment factors may also play a key role in the development of ALC. Liver cirrhosis is reported to have significant mortality, morbidity, and reduced life expectancy. In fact, the median survival of patients with advanced ALC is reported to be around 1-2 years. Additionally, patients with decompensated cirrhosis who abstain from alcohol use have a reported 5-year survival rate of 60%, compared to the 30% survival rate in patients who continue with alcohol consumption[1]. It has previously been reported that a high proportion of patients with liver cirrhosis are readmitted within 30 d or 90 d, underscoring the risk of readmission in these patients[2].
While data on the morbidity and mortality of ALC has been reported in literature, there is paucity of information on the trends of readmissions after an index hospitalization for ALC. The purpose of this study was to identify the trends of readmissions, total hospital charges, and length of stay (LOS) over an eight-year study period while also examining changes in the demographic of ALC readmissions over time. Furthermore, as National Readmission Database (NRD) stores data on inpatient admissions in the form of International Classification of Diseases (ICD) codes, we used the codes 571.2 and K70.3X to include all patients with ALC in our study[3].
This was a retrospective interrupted trends study involving adult hospitalizations for ALC in in the United States from 2010-2018. Data was extracted from the NRD which is the largest, publicly available, all-payer, inpatient healthcare readmission database in the United States, drawn from the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases[3]. The NRD is an annual file constructed using one calendar year of discharge data. Discharges included in the NRD were treated at community hospitals (excluding rehabilitation or long-term acute care hospitals) and a majority of these discharges had patient linkage numbers that were verified and not questionable. Discharge weights were calculated using post-stratification for hospital characteristics (census region, urban-rural location, teaching status, bed size, and hospital control) and patient characteristics [sex and five age groups (0, 1-17, 18-44, 45-64, and 65 and older)]. The NRD contains discharge data from 28 geographically dispersed states accounting for 59.7% of the total United States population and 58.7% of all United States hospitalizations. It comprises both patient and hospital-level information. Up to 40 discharge diagnoses and 25 procedures are collected for each patient using the ICD-9 and ICD-10 codes. Diagnose were classified as principal diagnosis which was the reason for hospitalization, and secondary diagnosis which was any other discharge diagnosis. Hospitals were stratified according to ownership control, the number of beds, teaching status, urban/rural location, and geographic region. Furthermore, the NRD allows for weighted analysis to obtain 100% of the United States hospitalizations within a given year[3].
The study involved hospitalizations from NRD for 2010, 2012, 2014, 2016 and 2018 with ALC as the reason for index admission using ICD codes (571.2 and K70.3X). Individuals less than 18 years of age, December and elective hospitalizations were excluded from the study. Using unique hospitalization identifiers, index hospitalizations were identified and one subsequent hospitalization within 30 d was tagged as a readmission. Furthermore, traumatic admissions were excluded from the readmission data. December admissions were excluded when searching for index admissions as these hospitalizations would lack data for at least 30 d following discharge to determine if there was a readmission according to the study design. The comorbidity burden was assessed using Sundararajan’s adaptation of the modified Deyo’s Charlson Comorbidity Index[4].
The biodemographic and hospitalization trends of the studied populations were highlighted over time. The 30-d all-cause ALC readmission rate, the ALC specific readmission rate, ALC readmission proportion, trends in inpatient mortality rate, mean LOS and mean THC were calculated. Total hospital cost was obtained using the HCUP Cost-to-Charge Ratio files and adjusted for inflation using the Medical Expenditure Panel Survey index for hospital care with 2018 as the reference point[5,6].
Data analysis was performed using Stata® Version 16 software (StataCorp, Texas, United States). All analyses were conducted using the weighted samples for national estimates in adjunct with HCUP regulations for using the NRD database. A multivariate regression analysis was used to calculate the trends of risk-adjusted odds of 30-d all-cause ALC readmission rate, the ALC specific readmission rate, ALC readmission proportion, trends in inpatient mortality rate, mean LOS and mean THC following adjustment for age, sex, grouped Charlson Comorbidity Index, insurance type, mean household income, and hospital characteristics. All P values were 2 sided with 0.05 set as the threshold for statistical significance.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. As the NRD does not include patient-specific and hospital-specific identifiers, this study was exempt from the Institutional Review Boards as per guidelines put forth by the IRB for research on database studies.
The NRD is a large publicly available all-payer inpatient care database in the United States, containing data on more than 18 million hospital stays per year[3]. Its large sample size provides sufficient data for analysis across hospital types and the study of readmissions for relatively uncommon disorders and procedures.
Details of characteristics of readmissions for ALC within the included years for the study are shown in Table 1. There has been a yearly increase in the total number of 30-d readmissions for ALC from 7660 in 2010 to 15085 in 2018 (P < 0.001). Most readmissions were noted for men but there was a decreasing trend in the proportion of male readmissions (P < 0.001). Patients readmitted for ALC had an increasing comorbidity burden with time. We also noted a rising trend of readmissions for small bed-sized and metropolitan teaching hospitals.
| Variable | Year | ||||
| 2010 | 2012 | 2014 | 2016 | 2018 | |
| Number of readmissions | 7660 | 8211 | 8753 | 13278 | 15085 |
| Mean age (yr) | 53.5 ± 0.5 | 53.6 ± 0.4 | 53.6 ± 0.4 | 54.0 ± 0.3 | 54.2 ± 0.3 |
| Male (%) | 72.5 | 73.1 | 72.2 | 68.3 | 67.4 |
| Charlson comorbidity | |||||
| Index (CCI) Score (%) | |||||
| 0 | 2.8 | 2.4 | 2.2 | 0.6 | 0.6 |
| 1 | 15.7 | 15.1 | 13.0 | 1.4 | 13.2 |
| 2 | 7.5 | 6.5 | 6.9 | 7.3 | 6.3 |
| ≥ 3 | 74.0 | 76.0 | 78.0 | 78.4 | 79.8 |
| Insurance type | |||||
| Medicare | 27.6 | 28.2 | 29.3 | 30.0 | 30.5 |
| Medicaid | 40.5 | 42.0 | 42.1 | 41.6 | 40.6 |
| Private | 21.4 | 20.0 | 20.4 | 22.5 | 21.8 |
| Uninsured | 10.5 | 9.7 | 8.3 | 6.0 | 7.2 |
| Household income | |||||
| Quartile (%) | |||||
| 1 | 34.6 | 36.2 | 34.0 | 34.2 | 33.2 |
| 2 | 23.8 | 25.6 | 28.3 | 27.4 | 29.2 |
| 3 | 23.4 | 22.4 | 22.0 | 23.5 | 22.6 |
| 4 | 18.2 | 15.8 | 15.6 | 14.8 | 15.0 |
| Hospital characteristics | |||||
| Hospital bed size (%) | |||||
| Small | 9.3 | 9.0 | 12.4 | 11.6 | 14.3 |
| Medium | 22.3 | 22.7 | 26.4 | 25.9 | 25.9 |
| Large | 68.4 | 68.2 | 61.2 | 62.5 | 59.8 |
| Teaching status (%) | |||||
| Metropolitan non-teaching | 40.4 | 39.1 | 28.0 | 26.1 | 20.5 |
| Metropolitan teaching | 52.6 | 53.7 | 66.8 | 69.5 | 75.4 |
| Non-metropolitan | 7.0 | 7.3 | 5.2 | 4.3 | 4.1 |
| Hospital Volume (Quintiles) | |||||
| Q1 | 2.4 | 2.3 | 2.2 | 1.9 | 1.5 |
| Q2 | 6.6 | 5.8 | 6.0 | 5.2 | 5.5 |
| Q3 | 12.6 | 12.5 | 12.0 | 10.6 | 11.3 |
| Q4 | 21.8 | 22.0 | 20.1 | 20.1 | 20.7 |
| Q5 | 56.6 | 57.4 | 59.7 | 62.2 | 61.1 |
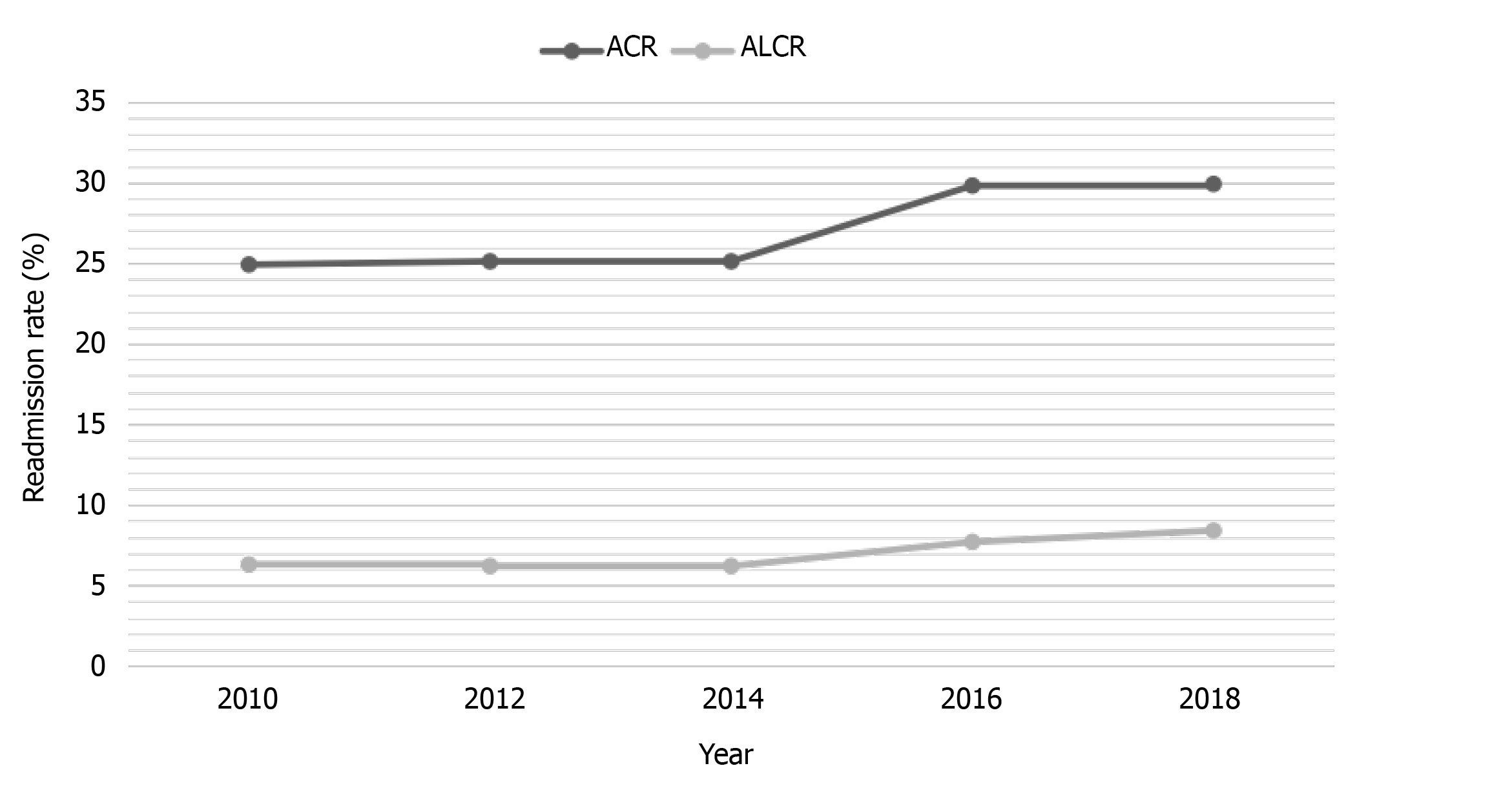
There was a steady rise in the rate of risk-adjusted 30-d all-cause ALC readmissions from 24.9% in 2010 to 29.9% in 2018 (P < 0.001). We also noted increasing risk-adjusted 30-d ALC specific readmission rate from 6.3% in 2010 to 8.4% in 2018 (P < 0.001) and increasing ALC readmission proportion from 31.4% in 2010 to 36.3% in 2018 (P < 0.001) (Table 1 and Figure 1). In-patient mortality for 30-d readmissions of ALC showed a decreasing trend from 10.5% in 2010 to 8.2% in 2018 (P = 0.0079). However, there was a trend towards increasing LOS from 5.6 d in 2010 to 6.3 d in 2018 (P < 0.001) and increasing THC from 13790 dollars in 2010 to 17150 dollars in 2018 (P < 0.001) (Table 2).
| Outcomes | Year | P value1 | ||||
| 2010 | 2012 | 2014 | 2016 | 2018 | ||
| All-cause readmission rate (%) | 24.9 | 25.1 | 25.1 | 29.8 | 29.9 | < 0.0011 |
| ALC specific readmission rate (%) | 6.3 | 6.2 | 6.2 | 7.7 | 8.4 | < 0.0011 |
| ALC readmission proportion (%) | 31.4 | 30.9 | 30.7 | 33.5 | 36.3 | < 0.0011 |
| Inpatient mortality (%) | 10.5 | 9.7 | 9.2 | 8.3 | 8.2 | 0.0081 |
| Mean length of stay (d) | 5.6 | 5.6 | 5.6 | 6.4 | 6.3 | 0.0011 |
| Mean total hospital cost (USD) | 13790 | 14206 | 13612 | 17602 | 17150 | < 0.0011 |
The total days of hospital stay attributable to 30-d readmissions of ALC increased by 119.2% from 43244 d in 2010 to 94789 d in 2018, while the total attributable hospital costs increased by 149% from 104 million dollars in 2010 to over 259 million dollars by the end of 2018.
There has been a yearly increase in the total number of 30-d readmissions of ALC in the United States. This may be due to rising alcohol use, high-risk drinking habits and DSM-IV alcohol use disorders[7]. Prior research has established a strong positive co-relation between rising alcohol use disorders and alcoholic liver disease such as ALC. In our study, most 30-d ALC readmissions were for males, but a decreasing trend was noted in the proportion of male readmissions. A study examining privately insured individuals with alcoholic cirrhosis noted that 32% of patients with alcoholic cirrhosis were women[8]. Our findings may reflect a rise in alcohol use, alcohol use disorders, and high-risk drinking behaviours in women, which is consistent with findings in current the literature[7].
Recent reports have also indicated that women with alcohol use disorder may experience more barriers to treatment than men. Additionally, women are less likely to access treatment for alcohol use disorders than men. The reasons for these differences in treatment across genders are numerous and include low perception for the need of treatment, feelings of shame and guilt, concurrent disorders, economic disparities, insurance disparities, and employment status[9]. The rise of alcohol use disorders and rising consumption of alcohol by women along with differences in treatment between genders may, in part, explain the down trend noted in males over the eight-year study period. Targeted treatments plans or treatment plan elements that aim to address gaps in the treatment for alcohol use disorders may help prevent ALC and help in the management of ALC patients with alcohol use disorders. Research also suggests that treatment outcomes for women are best when given in women-only programs that have women-specific content focus[9]. Thus, creating targeted treatment programs for women may be an effective way of reducing ALC readmissions and promoting abstinence from alcohol use, a key component of ALC treatment strategies[10].
Patients readmitted for ALC had increasing comorbidity burden with time. Comorbidities are known to increase mortality and affect the overall prognosis in patients with liver cirrhosis, but it is important to recognize complications and distinguish them from comorbidities in cirrhotics[11]. Previous reports have indicated that increased alcohol consumption, high-risk consumption behaviours and increased alcohol use disorders in the United States not only constitute a public health crisis, but also increase the risk of numerous comorbidities associated with alcohol use. Alcohol use disorders and increased alcohol consumption are well known risk factors for morbidity and mortality in patients with hypertension, cardiovascular disease, stroke, cirrhosis, certain cancers, type 2 diabetes mellitus, infections, and injuries. Moreover, alcohol use disorders and high-risk alcohol consumption are both associated with numerous psychiatric disorders[7]. As previous studies have indicated, understanding the impact of comorbidities on cirrhosis can help generate tailored treatment regimens for patients with ALC[11]. The rising comorbidity burden with time may also reflect the need for increased interventions specifically based on comorbid conditions.
There was a steady rise in the risk-adjusted 30-d all-cause ALC readmission rate. We also noted increasing risk-adjusted 30-d ALC specific readmission rate and ALC readmission proportion. A study investigating patients with ALC found that these patients were more likely to be disproportionately sicker at presentation and were readmitted more often than their non-ALC counterparts[8]. Additionally, hospital readmissions have been reported to occur more frequently in patients with cirrhosis. In general, research noted that early readmission reflects poor quality of care, and previous studies have reported a pooled rate of 26% for 30-d readmissions for cirrhosis. These readmissions negative impact inpatient mortality. The rising rate of readmissions in patients with ALC suggests that there may be room for improvement in caring for patients with ALC with the hope of reducing readmissions as has been suggested in previous cirrhosis-related readmissions studies[12]. Previous studies have also found that initial ALC admissions have most often resulted in readmissions secondary to acute complications from cirrhosis and substance abuse, while in patients without ALC, readmissions were most commonly due to acute cirrhosis complications and complications from cancer[2]. The rise in ALC-related readmissions found in our study may reflect increased alcohol use, closely related to the amount of undiluted alcohol consumed and the duration of consumption[1]. This reflects the need for enrolment of patients with ALC into alcohol rehabilitation programs on index admission, extensive patient education, regular outpatient follow-ups and early effective alcohol use disorder treatments in the outpatient setting to prevent development and readmissions in ALC patients.
Inpatient mortality showed a decreasing trend in our study; however, there was a trend towards increasing LOS and THC. The total days of hospital stay attributable to ALC readmissions increased by 119.2%, and total attributable hospital costs increased by 149% from 104 dollars million in 2010 to over 259 million dollars by 2018. Inpatient charges for patients with liver cirrhosis are substantial and have been consistently increasing[13]. Cirrhosis has resulted in considerable resource utilization and expenditure, despite acceptable hospital survival. Critically ill patients with liver cirrhosis have historically been perceived as not only having a poor prognosis, but also substantial costs of care, which is elucidated by our findings[14]. Alcohol liver diseases such as ALC are reportedly account for more than half of the charges associated with liver cirrhosis. This significant cost associated with ALC is driven by the volume of both admissions and readmissions of the same patients. Previous reports have suggested that effective alcohol use disorder interventions can help reduce costs related to inpatient cirrhosis management[13]. Treatments that have been proven to be cost-effective and in some cases cost-saving for ALC include one-on-one physician counselling and medication-assisted therapies[15]. These have been shown to improve outcomes in patients with compensated ALC[15].
This study has several strengths that can be appreciated. The population used for this study is drawn from the NRD, which is believed to be a large, multi-ethnic hospital-based registry in the United States. This study also examines eight-year data and numerous demographic characteristics of ALC hospitalizations, offering a comprehensive, thorough, and contemporary overview of ALC readmissions in the United States. However, as with any study, there are limitations that should be noted. Data from the NRD is subject to all biases associated with retrospective studies. Additionally, the NRD does not contain data on the hospital course and treatment aspects of the disease. Moreover, the NRD reports information on hospitalizations rather than from individual patients. Thus, patients with numerous readmissions would be included more than once in the data set. The database also uses ICD codes to store information and therefore may have coding errors. Finally, the NRD does not include information about the severity of ALC at the time of admission.
Despite these limitations, the large sample size, outcomes of the study, and analysis techniques make for a study that provides a current perspective on a major healthcare burden while aiming to encourage further discourse and future controlled prospective studies on ALC hospitalizations and readmissions.
ALC is a chronic liver disease with a known healthcare and economic burden, morbidity, and mortality with the potential to result in readmissions. This retrospective, interrupted trends study examined adult hospitalizations for ALC in in the United States. We found a yearly increase in the total number of 30-d readmissions for ALC and an increasing comorbidity burden with time which may reflect the rise in alcohol use disorders and comorbid conditions in patients with ALC. There was a steady rise in the risk-adjusted 30-d all-cause ALC readmission rate, risk-adjusted 30-d ALC-specific readmission rate and 30-d ALC readmission proportion. This may reflect the need for better management of ALC in an outpatient setting. Medication-assisted therapies and counselling may be highly cost-effective ways to reduce ALC readmissions. Inpatient mortality notably showed a decreasing trend for the study period. However, there was a trend towards increasing LOS and THC. Ultimately, improved management of ALC and associated conditions like alcohol use disorder and high-risk alcohol consumption may help reduce readmissions and resultant healthcare burdens associated with readmissions.
Readmissions of alcoholic liver cirrhosis (ALC) are associated with poor outcomes.
There is paucity of data on the trends of 30-d readmissions of ALC in the United States despite it being a significant healthcare burden.
The primary objective of this study was to identify and assess trends of 30-d readmissions of ALC in the United States over an eight-year period.
This retrospective interrupted trend study used the National Readmissions Database to identify all 30-d readmissions of ALC. Multivariate regression analysis was used to calculate the trend for risk-adjusted odds of 30-d all-cause ALC readmissions, ALC specific readmission rate, ALC readmission proportion, mortality, mean length of stay (LOS) and mean total hospital cost (THC).
There was a trend towards increasing total 30-d readmissions of ALC, risk-adjusted 30-d all-cause ALC readmission, ALC specific readmission rate, and ALC readmission proportion. However, inpatient mortality declined from 10.5% in 2010 to 8.2% in 2018. The total days of hospital stay attributable to 30-d readmissions of ALC increased by 119.2% while the total attributable hospital costs increased by 149% by the end of 2018.
The total number of 30-d readmissions of ALC increased; however, inpatient mortality declined. There was a trend towards increasing LOS and THC for these readmissions.
Future studies are needed to investigate the treatment aspects of ALC in an inpatient setting. Additionally, the impact of early enrollment of patients into alcohol rehabilitation programs, patient education, regular outpatient follow-up and early effective alcohol use disorder treatments in the outpatient setting to prevent readmissions of ALC in is yet to be determined.
| 1. | Bruha R, Dvorak K, Petrtyl J. Alcoholic liver disease. World J Hepatol. 2012;4:81-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (2)] |
| 2. | Tapper EB, Halbert B, Mellinger J. Rates of and Reasons for Hospital Readmissions in Patients With Cirrhosis: A Multistate Population-based Cohort Study. Clin Gastroenterol Hepatol. 2016;14:1181-1188.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 178] [Article Influence: 17.8] [Reference Citation Analysis (1)] |
| 3. | Agency for Healthcare Research and Quality. Overview of the Nationwide Readmissions Database (NRD). 2018. [cited 20 May 2021]. Available from: https://www.hcup-us.ahrq.gov/nrdoverview.jsp. |
| 4. | Sundararajan V, Quan H, Halfon P, Fushimi K, Luthi JC, Burnand B, Ghali WA; International Methodology Consortium for Coded Health Information (IMECCHI). Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med Care. 2007;45:1210-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 214] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 5. | Agency for Healthcare Research and Quality. Cost-to-Charge Ratio Files. [cited 20 May 2021]. Available from: https://www.hcup-us.ahrq.gov/db/ccr/costtocharge.jsp. |
| 6. | Dunn A, Grosse SD, Zuvekas SH. Adjusting Health Expenditures for Inflation: A Review of Measures for Health Services Research in the United States. Health Serv Res. 2018;53:175-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 387] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 7. | Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B, Jung J, Zhang H, Fan A, Hasin DS. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74:911-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 761] [Cited by in RCA: 1078] [Article Influence: 119.8] [Reference Citation Analysis (0)] |
| 8. | Mellinger JL, Shedden K, Winder GS, Tapper E, Adams M, Fontana RJ, Volk ML, Blow FC, Lok ASF. The high burden of alcoholic cirrhosis in privately insured persons in the United States. Hepatology. 2018;68:872-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 173] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 9. | McCrady BS, Epstein EE, Fokas KF. Treatment Interventions for Women With Alcohol Use Disorder. Alcohol Res. 2020;40:08. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 10. | Walsh K, Alexander G. Alcoholic liver disease. Postgrad Med J. 2000;76:280-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 74] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Jepsen P. Comorbidity in cirrhosis. World J Gastroenterol. 2014;20:7223-7230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Orman ES, Ghabril M, Emmett TW, Chalasani N. Hospital Readmissions in Patients with Cirrhosis: A Systematic Review. J Hosp Med. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Barritt AS 4th, Jiang Y, Schmidt M, Hayashi PH, Bataller R. Charges for Alcoholic Cirrhosis Exceed All Other Etiologies of Cirrhosis Combined: A National and State Inpatient Survey Analysis. Dig Dis Sci. 2019;64:1460-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Shawcross DL, Austin MJ, Abeles RD, McPhail MJW, Yeoman AD, Taylor NJ, Portal AJ, Jamil K, Auzinger G, Sizer E, Bernal W, Wendon JA. The impact of organ dysfunction in cirrhosis: survival at a cost? J Hepatol. 2012;56:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 15. | Avanceña ALV, Miller N, Uttal SE, Hutton DW, Mellinger JL. Cost-effectiveness of alcohol use treatments in patients with alcohol-related cirrhosis. J Hepatol. 2021;74:1286-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Michalak A, Samadder S S-Editor: Liu M L-Editor: A P-Editor: Liu M