Published online Jun 27, 2019. doi: 10.4254/wjh.v11.i6.542
Peer-review started: March 12, 2019
First decision: April 10, 2019
Revised: May 16, 2019
Accepted: June 17, 2019
Article in press: June 17, 2019
Published online: June 27, 2019
Processing time: 108 Days and 20.5 Hours
An ideal staging system for hepatocellular carcinoma (HCC) should rely on the hepatic reserve function and tumor burden. With the improvement in diagnostic and treatment strategies for HCC, in addition to recent treatment of viral hepatitis, finding a suitable assessment tool for hepatic reserve has become mandatory.
To validate a recently proposed modified albumin-bilirubin-TNM (mALBI-T) grade as a prognostic model for patients with HCC in Egypt.
For patients diagnosed with HCC, Child-Turcotte-Pugh (CTP) score, Barcelona Clinic Liver Cancer (BCLC) stage, albumin-bilirubin (ALBI), plateltet-albumin–bilirubin (PALBI), ALBI-based BCLC, ALBI-T and mALBI-T grades were estimated. Patients were followed from time of diagnosis to date of death or date of data collection if they remained alive. Overall survival and received treatments were determined. Survival data were analyzed.
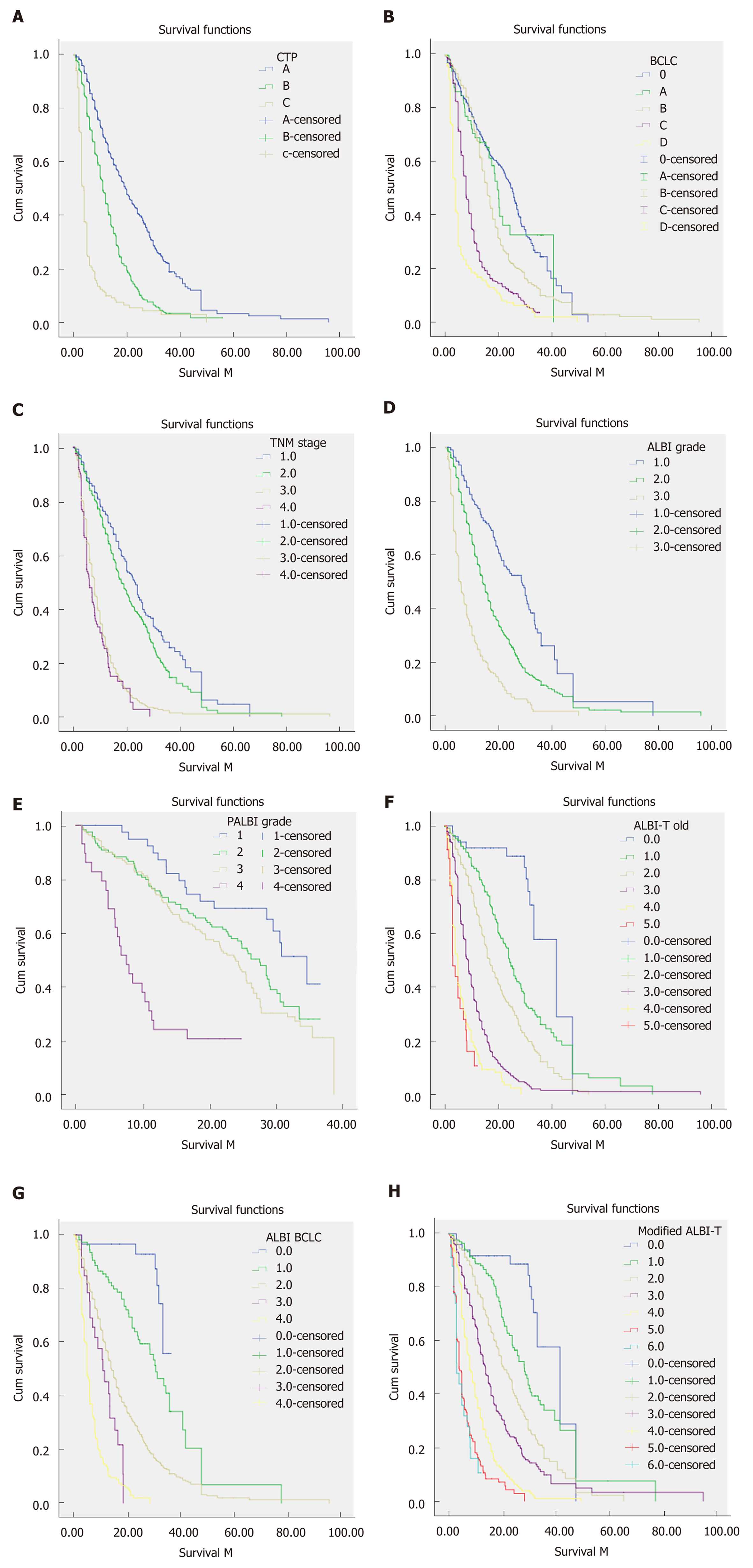
A total of 1910 patients were included (mean age, 57 years; 1575 males). At presentation, 50.6% had CTP A, 36.1% had CTP B and 13.4 % had CTP C; 12% had ALBI grade 1, 62.3% had ALBI grade 2 and 24.7% had ALBI grade 3. Overall median survival was 13 mo; survival was better in patients with ALBI 1 than in those with ALBI 2 and 3 (28.6 vs 14 and 5.8 mo, respectively, P < 0.001). Patients with ALBI-T grades 0 and 1 had better survival than those with ALBI-T grades 2, 3, 4 and 5 (P < 0.001). The modified ALBI-T showed better stratification and significant improvement in prediction of survival.
ALBI-T grade is a superior prognostic tool that selects patients with HCC who have better liver reservoir and tumor stage. mALBI-T is a better prognostic model in patients with HCC.
Core tip: In this study, we validated the modified version of the albumin-bilirubin-TNM grade (mALBI-T) in a retrospective Egyptian cohort. In addition, this study offered a comparative analysis of eight different established and novel scoring systems. We concluded that the modified ALBI-T score is superior to the other scoring systems and offers a better prognostic tool.
- Citation: Elshaarawy O, Alkhatib A, Elhelbawy M, Gomaa A, Allam N, Alsebaey A, Rewisha E, Waked I. Validation of modified albumin-bilirubin-TNM score as a prognostic model to evaluate patients with hepatocellular carcinoma. World J Hepatol 2019; 11(6): 542-552
- URL: https://www.wjgnet.com/1948-5182/full/v11/i6/542.htm
- DOI: https://dx.doi.org/10.4254/wjh.v11.i6.542
Hepatocellular carcinoma (HCC) accounts for > 5% of all human cancers and is a major health problem worldwide, being the fifth most common malignancy in men and the eighth in women. The estimated annual incidence of HCC exceeds 840000, and it is the third most common cause of cancer-related death in the world[1].
It is widely perceived that survival in HCC depends on tumor stage, underlying liver function, and the performance status of the patient[2]. The Child-Turcotte-Pugh (CTP) classification of liver function relies on individual parameters scored based on arbitrarily defined, predetermined cutoff points that lead to misjudging of the liver condition of the patients[3]. This was an incentive for the development of a novel scoring system, the Albumin-Bilirubin(ALBI) grade by Johnson et al[4] incorporating albumin and bilirubin only, which are numerical parameters readily available in the basic investigations for patients with liver disease. ALBI grade does not comprise the subjective parameters which are included in CTP classification, for example, grading of ascites and encephalopathy. The cut-off points of the predictive equation of ALBI grade allocate patients according to the calculated score as follows: score of -2.60 or less is ALBI grade 1, those with a score more than -1.39 is ALBI grade 3, while those in between are classified as ALBI grade 2. Nevertheless, patients with ALBI grade 2 had a wide range of hepatic function, the same drawback of Child-Pugh class B. So, other grades based on ALBI grade were proposed[5-8]. Hiraoka et al[8] proposed the ALBI-T grade which icorporated TNM staging system (LCSG fifth edition) into the previously discussed ALBI grading system. It showed better performance and superiority as a prognostic scoring system regarding survival prediction in HCC patients.
Hiraoka et al[9] proposed to divide ALBI grade into four levels, namely, the modified ALBI (mALBI) grade, using an additional cut-off value for ALBI score (–2.270), based on an indocyanine green retention test (ICG-R15) of 30%, which is statistically defined as the cut-off value for minimal anatomical surgical resection for HCC in Makuuchi criteria. In the current work, the prognostic value of the modified albumin-bilirubin-TNM (mALBI-T) grade proposed by Hiraoka et al[9] was evaluated as a tool to predict survival in HCC patients and compared to other ALBI-based grades.
All patients diagnosed with HCC according to the AASLD guidelines[10] with complete data and contact details, from the HCC clinic at National Liver Institute, Menoufia University, were included in this study. The study was granted ethical committee approval prior to data retrieval. We had access to a data set of a cohort of 1910 patients diagnosed with HCC who fulfilled the inclusion criteria.
The diagnosis of HCC was based on the presence of an arterial hypervascular focal lesion > 2 cm with rapid wash-out with a single imaging modality (triphasic spiral computed tomography (CT), magnetic resonance imaging or angiography) or two imaging modalities demonstrating the before mentioned feature for lesions < 2 cm[10]. All patients included in the study were subjected to history taking and complete clinical examination with special emphasis on the etiology of liver disease, history of ascites or encephalopathy, performance status based on the Eastern Co-operative Oncology Group (ECOG) performance scale, demographic data and contact details. Laboratory investigations included serum albumin, total bilirubin, alpha fetoprotein (AFP) and international normalized ratio (INR). Ultrasound and multislice triphasic CT of the abdomen with contrast were done to detect the number of nodules, nodule type (unifocal, multifocal, or diffuse), maximum tumor diameter (cm), location (right/left/both lobes), portal vein thrombosis (PVT) and extrahepatic or lymph node metastasis. Any patient with incomplete data or inaccessible contact was excluded from the analysis.
The following staging and grading systems were estimated at the time of HCC diagnosis: CTP score, Barcelona Clinic Liver Cancer (BCLC) stage and TNM stage[4,10-12]. During data preparation and analysis, the following scores were estimated based on baseline data using the following formulas.
ALBI grade[4]: The cut points of this linear predictor place patients with a calculated score of -2.60 or less into ALBI grade 1, those with a score higher than -1.39 into ALBI grade 3, and those in between into ALBI grade 2. The equation for the linear predictor is (log10 bilirubin x 0.66) + (albumin x -0.085), where bilirubin is in mcmol/L and albumin is in g/L[5].
PALBI grade[6]: ALBI score was calculated as [2.02*Log10 bilirubin] + [-0.37*[log10 bilirubin]2] + [-0.04*albumin] + [-3.48* log10 platelets] + [1.01 *(log10 platelets2)]. PALBI grade was assigned based on 50% and 85% Cox cut points: PALBI 1, ≤ -2.53; PALBI 2, -2.53 to -2.09; PALBI 3, >-2.09[7].
ALBI-BCLC grade[7]: It was calculated by replacing the CTP grades A, B and C used in the BCLC system with the ALBI grades 1, 2 and 3 respectively[8].
ALBI-T grade[8]: ALBI-T score was obtained by adding the TNM stage from the LCSGJ 5th edition to the ALBI grade and then subtracting 2. Patients were graded from 0 to 5[9].
mALBI-T grade[9]: The mALBI-T score was proposed by Hiraoka et al[9] as they added a new cut-off point for ALBI grade 2 at -2.27 based on an ICG-R15 of 30%, resulting in four stages of ALBI grade. This modification was introduced to ALBI-T grade where TNM stage was added to modified ALBI grade and subtracting 2. This led to mALBI-T stages from 0 to 6. Consequently, patients were followed from the time of diagnosis to the date of death or date of data collection if they remained alive.
Statistical analyses were performed using SPSS Statistics version 25.0 (IBM, United States). Overall survival and the received treatment were determined. Survival data were analyzed using Kaplan Meir Survival curves and log rank test, then the area under the receiver operating characteristic curve (AUC) was determined for each staging and scoring system. Results were considered statistically significant when P-values were lower than 0.05. P-values less than 0.01 were considered highly significant. Of note, all reported P-values are uncorrected and two-tailed.
A total of 1910 patients with HCC were included, of whom 1575 (82.5%) were male. The mean age of the patients was 57 years. The underlying cause of cirrhosis was hepatitis C virus infection in 71.6% of cases. The right lobe was the site of HCC in about 1204 (63%) patients. PVT was detected in 345 (18%) patients, and extra-hepatic metastasis was detected in (7.74%) 148. EGOG performance status was zero in 1154 (60.3%) patients. The baseline clinical features of the included patients are shown in Table 1.
| Variable | Patients |
| n = 1912 | |
| Male gender, n (%) | 1575 (82.4) |
| Age (yr, mean ± SD) | 57(± 7.2) |
| Etiology | |
| Hepatitis C | 1369 (71.6) |
| Hepatitis B | 468 (24.5) |
| Other | 75 (3.9) |
| Albumin (g/L, mean ± SD) | 31.4(± 4.6) |
| Bilirubin [µmol/L, median (IQR)] | 24.5 (13.9-29.1) |
| Platelet count (x 109/L, mean ± SD) | 96 (± 37.4) |
| AFP [µg/L, median (IQR)] | 43 (10-184.3) |
| Tumor size [cm, median (IQR)] | 5.6 (1.8-8.4) |
| Solitary tumor, n (%) | 369 (19.3) |
| PVT | 345 (18) |
| Metastasis | 148 (7.7) |
| ECOG grade 0, n (%) | 1154 (60.4) |
| Treatment | |
| Liver resection | 67 (3.5) |
| Liver transplantation | 43 (2.3) |
| Ablative procedures (PEI, RFA and microwave) | 249 (13.1) |
| TACE | 1036 (54.1) |
| Combined treatment (TACE + ablation) | 8 (0.4) |
| Systemic therapy | 40 (2.1) |
| Conservative | 469 (24.5) |
| Overall survival, months (95%CI) | 17.9 (12.1-13.8) |
| Overall deaths, n (%) | 1219 (63.8) |
Among these basic features, we can see that hepatitis B virus infection as an etiology is a predictor of poor survival in the multivariate analysis (Table 2). Also, single tumor and good liver function (e.g., low bilirubin and high albumin) were good predictors of survival in our cohort (Table 2).
| Variable | Hazard ratio (95%CI) | P-value |
| Tumour number | ||
| Solitary | 1 | |
| Multiple | 1.456 (1.236, 1.750) | <0.01 |
| Log10 tumour size (cm) | 3.517 (2.678, 4.567) | <0.001 |
| Baseline log10 AFP | 1.302 (1.208, 1.411) | <0.001 |
| Baseline albumin | 0.993 (0.966, 0.998) | 0.031 |
| Baseline log10 bilirubin | 1.581 (1.139, 2.194) | <0.001 |
| Vascular invasion | ||
| No | 1 | |
| Yes | 1.612 (1.251, 2.045) | 0.001 |
| Aetiology | ||
| Hepatitis C virus | 1 | |
| hepatitis B virus | 1.260 (1.020, 1.407) | <0.05 |
| Others | 0.914 (0.887, 0.991) | 0.043 |
Patients were classified according to CTP class, ALBI grade, PALBI, TNM, BCLC staging system, ALBI-based BCLC, ALBI-T and mALBI-T (Table 3).
| Staging/grading system | Stage/grade | Percentage of patients | Median survival (mo) | P-value |
| CTP | A | 50.6 | 19 | < 0.001 |
| B | 36.1 | 11 | ||
| C | 13.4 | 3.8 | ||
| BCLC | 0 | 3.6 | 25.4 | < 0.001 |
| A | 27.5 | 19.8 | ||
| B | 26.6 | 16 | ||
| C | 28.9 | 8 | ||
| D | 13.4 | 4 | ||
| TNM | I | 19.5 | 23 | < 0.001 |
| II | 36.6 | 18 | ||
| III | 35.4 | 8 | ||
| IV | 8.5 | 6 | ||
| ALBI | 1 | 12 | 28.6 | < 0.001 |
| 2 | 63.2 | 14 | ||
| 3 | 24.7 | 5.8 | ||
| PALBI | 1 | 10.1 | 34.6 | < 0.001 |
| 2 | 29 | 27.5 | ||
| 3 | 33.9 | 23.9 | ||
| 4 | 27 | 7.5 | ||
| ALBI-based BCLC | 0 | 1.5 | Undefined | < 0.001 |
| A | 5.9 | 30.8 | ||
| B | 67.2 | 14.2 | ||
| C | 2.2 | 11 | ||
| D | 23.2 | 5 | ||
| ALBI-T | 0 | 2.6 | 42 | < 0.001 |
| 1 | 18.1 | 28.9 | ||
| 2 | 30.4 | 17 | ||
| 3 | 31.1 | 8 | ||
| 4 | 16 | 5 | ||
| 5 | 1.8 | 3 | ||
| Modified ALBI-T | 0 | 2.6 | 42 | < 0.001 |
| 1 | 9.1 | 28.9 | ||
| 2 | 18.5 | 20 | ||
| 3 | 27.9 | 14 | ||
| 4 | 25.5 | 8 | ||
| 5 | 14.6 | 5 | ||
| 6 | 1.8 | 3 |
Each of the investigated scoring systems showed significant stratification of the median survival across its different grades. The overall median survival was 13 mo for the whole cohort. The median survival for CTP A patients were 19 mo, better than that for patients with CTP B and C (11 and 3.8 mo, respectively) (P < 0.001). Indeed, the median survival was better in patients with ALBI grade 1 than in those with ALBI grades 2 and 3 (28.6, 14 and 5.8 mo, respectively, P < 0.001). Also, patients with PALBI grade 1 had a better median survival (34.6 mo) than in those with PALBI grades 2, 3 and 4 (27.5, 23.9 and 7.5 mo, respectively, P < 0.001).
The ALBI-based BCLC system showed better performance to stratify the included patients (Table 3). The median survival was [undefined (mean = 33.8 mo), 30.8, 14.2, 11 and 5 mo, P < 0.001] for stages 0, A, B, C and D compared to (25.4, 19.8, 16, 8 and 4 mo, P < 0.001) for stages 0, A, B, C and D, respectively, in the CTP-based BCLC staging system.
Incorporating TNM staging into ALBI grade (ALBI-T) provided better performance and ability to discriminate median survival of patients across different stages (P < 0.001). Furthermore, ALBI-T grades 0 and 1 patients had better median survival than those with ALBI-T grades 2, 3, 4 and 5 (42, 28.9, 17, 8, 5 and 3 mo, respectively P < 0.001). Notably, the mALBI-T showed significant improvement in the median survival in patients with ALBI-T grades. Also, mALBI-T grades 2, 3 and 4 showed improved survival (20, 14 and 8 mo, respectively, P < 0.001), as shown in Figure 1. However, other stages remained the same as they were not affected by the sub-classification of ALBI grade 2.
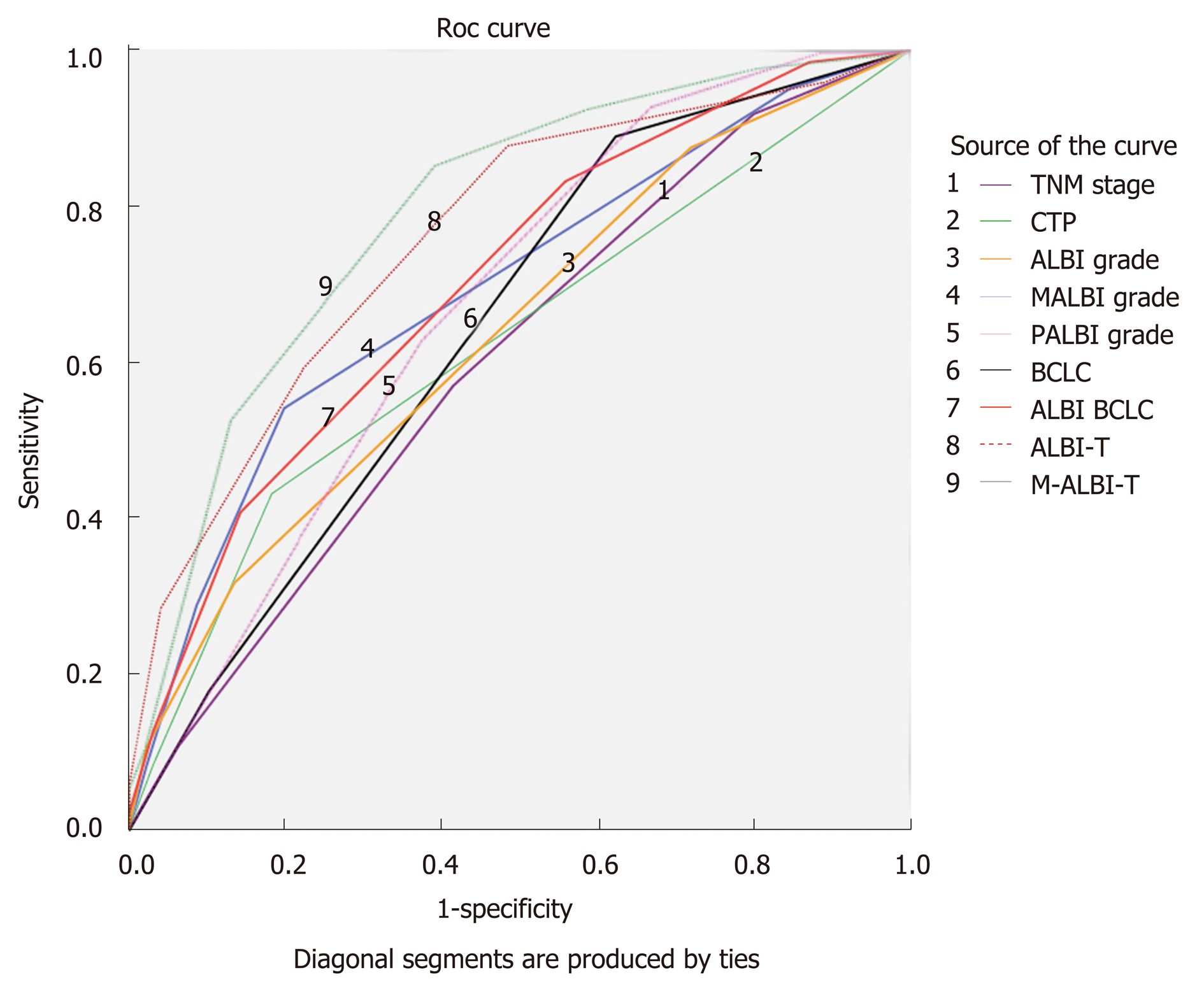
The AUC was determined for each grade (Figure 2). Of note, the ALBI-based BCLC had significantly higher AUC in comparison to CTP-based BCLC (AUC = 0.749 vs 0.713, respectively). However, the mALBI-T grade showed the highest AUC compared to all other studied scoring systems (AUC = 0.848, P < 0.001).
The most widely used staging system for stratifying patients with HCC is the BCLC system. It was proposed according to the recommendations of many randomized controlled trials and cohort studies which precisely included the tumor stage, patient’s performance status, and liver function into an algorithm which allocates patients to different treatment plans according to the evidence-based results[11]. The BCLC system helps to allocate treatment modalities and properly identify suitable patients for clinical trials. However, it is important to know that the liver function is assessed in the BCLC system according to the subjective CTP grade which is considered one of the limitations of this widely used staging system[10].
Residual hepatic function plays an important role in predicting the outcome of patients with HCC. On this premise, Johnson et al[4] conducted the pioneer study that coined the term ALBI grade on 6000 patients from Europe, Japan, China and the United States with various stages of HCC. Simply, this model depended on two laboratory variables (bilirubin and albumin) and omitted the subjective CTP variables ascites and hepatic encephalopathy. Questions have been raised regarding INR inclusion in ALBI grade. However, INR as a parameter is considered a source of bias in patients taking oral anti-coagulants, but it is impossible to stop treatment just to calculate a score. Since residual hepatic function plays an important role in predicting the outcome of patients with HCC, six models evaluating the severity of cirrhosis (CTP, ALBI, PALBI, ALBI-based BCLC and ALBI-T grading systems) were investigated in this study in addition to the recently proposed modification of ALBI-T.
Patients with CTP class A had a significantly better median survival than those with CTP classes B and C. This is in agreement with several reports[12-14]. Similarly, patients with ALBI grade 1 had a significantly better median survival than those with ALBI grades 2 and 3 in this study, in accordance with other reports[15,16]. ALBI grade has become a core for further prognostic models, and Roayaie et al[6] proposed PALBI grade, where they added the platelet count in a new linear predictive equation to the ALBI grade parameters. In this study, patients with PALBI grade 1 had significantly better median survival than those with PALBI grade 2, 3 and 4 (P < 0.001).
Both ALBI and PALBI grades showed precise ability to stratify HCC patients into different stages according to their survival. The PALBI grade was superior to CTP classification and ALBI grade in terms of mortality prediction (AUC = 0.734, 0.643 and 0.709, respectively). For CTP grade A patients, the PALBI grade had significantly higher AUC in comparison to ALBI grade at 1-year and 3-years intervals (Table 4). This is in line with the endpoints reported by Roayaie et al[6] who concluded that PALBI was independently associated with survival when controlled for age, tumor related factors and performance status, and can stratify patients with HCC undergoing curative therapies more precisely than CTP class[6]. Other studies reported the same results using different treatment modalities for HCC[17,18]. PALBI grade was found to perform better than ALBI grade, as incorporating platelet count reflects the role of portal hypertension. However, not all HCC patients have portal hypertension and some fallacies may result from platelet counting, as pseudo thrombocytopenia resulting from adding EDITA to blood samples that lead to aggregate formation inside automated cell counters. In addition, thrombocytosis can be found as a paraneoplastic event in patients with HCC and can affect the results of the score.
| Grade | 1-yr AUROC | 3-yr AUROC | Overall AUROC |
| TNM | 0.639 | 0.626 | 0.620 |
| CTP | 0.672 | 0.649 | 0.643 |
| ALBI | 0.741 | 0.728 | 0.709 |
| Modified ALBI | 0.755 | 0.732 | 0.719 |
| PALBI | 0.753 | 0.741 | 0.734 |
| BCLC | 0.758 | 0.743 | 0.713 |
| ALBI-based BCLC | 0.762 | 0.751 | 0.749 |
| ALBI-T | 0.822 | 0.809 | 0.801 |
| Modified ALBI-T | 0.851 | 0.848 | 0.848 |
ALBI grade succeeded to overcome the weaknesses of CTP classification, and this led to further trials to substitute CTP score in the BCLC staging system by Chan et al[7] or incorporating it to the TNM staging system to result in ALBI-T which was proposed by Hiraoka et al[8]. The ALBI-based BCLC staging system showed more prognostic power than CTP-based BCLC in the studied cohort. The ALBI-based BCLC had significantly higher AUC compared with CTP-based BCLC (AUC = 0.749 vs 0.713, respectively). In contrast, an international multicenter study found that the ALBI-based BCLC system yields the same prognostic discrimination as the CTP-based BCLC system, regardless of treatment modalities. The authors concluded that the substitution of CTP class by ALBI grade does not improve the overall prognostic performance of the BCLC system[7]. However, other authors found that the ALBI grade can estimates objective hepatic reserve across each BCLC stage[19].
ALBI-T grade was proposed through evaluation of the prognosis of 2,584 Japanese patients with HCC and validated in a nationwide survey of 46,681 patients in Japan[8,9]. In this study, patients with ALBI-T grade 0 had a median survival of 42 mo and patients with ALBI-T grade 1 was found to have a better median survival (28.9 mo) than those with ALBI-T grades 2, 3, 4 and 5 (17, 8, 5 and 3 mo, respectively). Comparable results were reported by other investigators[9,20-22].
ALBI-T grade was able to percisely predict survival in comparison to other scoring systems, due to its incorporation of TNM stage, which is suitable for assessment of small HCC tumors, and ALBI grade, which is an accurate objective tool for assessment of liver function. This could be emphasized by the multivariate Cox regression analysis showing that the parameters of the ALBI score performed well and it was a good predictor of survival (Table 2). Future scores would perform better if they include other parameters that evolved in our analsysis as a good predictor of survival such as vascular invasion and etiology.
The mALBI-T grade showed more detailed stratification ability and better predictive value for prognosis of Egyptian patients with HCC, compared to those shown by other staging and scoring systems including ALBI-T. When comparing the modified model to other staging systems, the mALBI-T had the highest AUC (0.848), while the AUC for ALBI-T was 0.801.
The retrospective nature and the short follow-up period are the main limitations to the present study. Despite this, the mALBI-T grade, with its detailed stratification of hepatic reserve function, may provide more accurate prediction of prognosis and overall survival of patients with HCC than other available grading systems.
It has been an urge to find a proper staging system for patients with hepatocellular carcinoma (HCC). The significance of this study is owed to comparing on a large scale a wide selection of scoring systems that included established [Child-Turcotte-Pugh (CTP), TNM and Barcelona Clinic Liver Cancer (BCLC)] and novel scoring systems (albumin-bilirubin (ALBI), plateltet-albumin–bilirubin (PALBI), ALBI-BCLC, ALBI-T and modified albumin-bilirubin-TNM (mALBI-T)].
Linear predictive equations based scoring systems (such as ALBI and PALBI) offer better performance than those based on predetermined cut-off points (CTP, TNM and BCLC). The best scoring system would be a linear function that incorporates liver function paramters and other tumor specific paramters such as alpha fetoprotein (AFP), tumor size and number.
We applied the tested scoring systems on our retrospective cohort and compared their performance using survival curves and AUROCS to predict survival in addition to patient stratification according to different scores.
Our findings proved that the modified version of ALBI-T score offered better stratification than the original score and is a better prognostic tool. It remains to be explored whether treatment modality specific scores would result in better performance than general scores or not and whether we need such specific scores or not.
This study offers a validation of the mALBI-T score in a large scale Egyptian cohort. mALBI-T performs better than the other investigated scoring systems such as ALBI and BCLC.
The best model for HCC patients should assess liver function, tumor number, size and other tumor specific paramters such as AFP. We suggest developing scores that include treatment response such as mRECIST criteria or recurrence status. Linear equations based scores are more precise and future scores should abandon old techniques that use predetermined points.
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 56668] [Article Influence: 7083.5] [Reference Citation Analysis (135)] |
| 2. | Fattovich G, Pantalena M, Zagni I, Realdi G, Schalm SW, Christensen E; European Concerted Action on Viral Hepatitis (EUROHEP). Effect of hepatitis B and C virus infections on the natural history of compensated cirrhosis: a cohort study of 297 patients. Am J Gastroenterol. 2002;97:2886-2895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 247] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 3. | Cholongitas E, Papatheodoridis GV, Vangeli M, Terreni N, Patch D, Burroughs AK. Systematic review: The model for end-stage liver disease--should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Aliment Pharmacol Ther. 2005;22:1079-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O'Beirne J, Fox R, Skowronska A, Palmer D, Yeo W, Mo F, Lai P, Iñarrairaegui M, Chan SL, Sangro B, Miksad R, Tada T, Kumada T, Toyoda H. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1962] [Cited by in RCA: 2169] [Article Influence: 197.2] [Reference Citation Analysis (0)] |
| 5. | Ogasawara S, Chiba T, Ooka Y, Suzuki E, Kanogawa N, Saito T, Motoyama T, Tawada A, Kanai F, Yokosuka O. Liver function assessment according to the Albumin-Bilirubin (ALBI) grade in sorafenib-treated patients with advanced hepatocellular carcinoma. Invest New Drugs. 2015;33:1257-1262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Roayaie S, Jibara G, Tabrizian P, Park JW, Yang J, Yan L, Schwartz M, Han G, Izzo F, Chen M, Blanc JF, Johnson P, Kudo M, Roberts LR, Sherman M. The role of hepatic resection in the treatment of hepatocellular cancer. Hepatology. 2015;62:440-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 338] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 7. | Chan AW, Kumada T, Toyoda H, Tada T, Chong CC, Mo FK, Yeo W, Johnson PJ, Lai PB, Chan AT, To KF, Chan SL. Integration of albumin-bilirubin (ALBI) score into Barcelona Clinic Liver Cancer (BCLC) system for hepatocellular carcinoma. J Gastroenterol Hepatol. 2016;31:1300-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 8. | Hiraoka A, Kumada T, Michitaka K, Toyoda H, Tada T, Ueki H, Kaneto M, Aibiki T, Okudaira T, Kawakami T, Kawamura T, Yamago H, Suga Y, Miyamoto Y, Tomida H, Azemoto N, Mori K, Miyata H, Ninomiya T, Kawasaki H. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J Gastroenterol Hepatol. 2016;31:1031-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 207] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 9. | Hiraoka A, Michitaka K, Kumada T, Izumi N, Kadoya M, Kokudo N, Kubo S, Matsuyama Y, Nakashima O, Sakamoto M, Takayama T, Kokudo T, Kashiwabara K, Kudo M. Validation and Potential of Albumin-Bilirubin Grade and Prognostication in a Nationwide Survey of 46,681 Hepatocellular Carcinoma Patients in Japan: The Need for a More Detailed Evaluation of Hepatic Function. Liver Cancer. 2017;6:325-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 269] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 10. | Bruix J, Sherman M. Management of hepatocellular carcinoma: An update. Hepatology. Hepatology. 2011;53:1020–10222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5972] [Cited by in RCA: 6630] [Article Influence: 442.0] [Reference Citation Analysis (1)] |
| 11. | Forner A, Llovet JM, Bruix J. Seminar: Hepatocellular carcinoma. Lancet. 2012;379:1245-1255. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3249] [Cited by in RCA: 3629] [Article Influence: 259.2] [Reference Citation Analysis (12)] |
| 12. | Lee SS, Shin HS, Kim HJ, Lee SJ, Lee HS, Hyun KH, Kim YH, Kwon BW, Han JH, Choi H, Kim BH, Lee JH, Kang HY, Shin HD, Song IH. Analysis of prognostic factors and 5-year survival rate in patients with hepatocellular carcinoma: a single-center experience. Korean J Hepatol. 2012;18:48-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Lee JH, Han SY, Jo JH, Kim SK, Go BS. Prognostic factors for survival in patients with hepatocellular carcinoma after radiofrequency ablation. Korean J Gastroenterol. 2007;49:17-23. |
| 14. | Liem MS, Poon RT, Lo CM, Tso WK, Fan ST. Outcome of transarterial chemoembolization in patients with inoperable hepatocellular carcinoma eligible for radiofrequency ablation. World J Gastroenterol. 2005;11:4465-4471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Lei Q, Zhang Y, Ke C, Yan C, Huang P, Shen H, Lei H, Chen Y, Luo J, Meng Z. Value of the albumin-bilirubin score in the evaluation of hepatitis B virus-related acute-on-chronic liver failure, liver cirrhosis, and hepatocellular carcinoma. Exp Ther Med. 2018;15:3074-3079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Na SK, Yim SY, Suh SJ, Jung YK, Kim JH, Seo YS, Yim HJ, Yeon JE, Byun KS, Um SH. ALBI versus Child-Pugh grading systems for liver function in patients with hepatocellular carcinoma. J Surg Oncol. 2018;117:912-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 17. | Liu PH, Hsu CY, Hsia CY, Lee YH, Chiou YY, Huang YH, Lee FY, Lin HC, Hou MC, Huo TI. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD Era. J Gastroenterol Hepatol. 2017;32:879-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 136] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 18. | Hansmann J, Evers MJ, Bui JT, Lokken RP, Lipnik AJ, Gaba RC, Ray CE. Albumin-Bilirubin and Platelet-Albumin-Bilirubin Grades Accurately Predict Overall Survival in High-Risk Patients Undergoing Conventional Transarterial Chemoembolization for Hepatocellular Carcinoma. J Vasc Interv Radiol. 2017;28:1224-1231.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Pinato DJ, Sharma R, Allara E, Yen C, Arizumi T, Kubota K, Bettinger D, Jang JW, Smirne C, Kim YW, Kudo M, Howell J, Ramaswami R, Burlone ME, Guerra V, Thimme R, Ishizuka M, Stebbing J, Pirisi M, Carr BI. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J Hepatol. 2017;66:338-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 326] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 20. | Hiraoka A, Kumada T, Kudo M, Hirooka M, Tsuji K, Itobayashi E, Kariyama K, Ishikawa T, Tajiri K, Ochi H, Tada T, Toyoda H, Nouso K, Joko K, Kawasaki H, Hiasa Y, Michitaka K; Real-Life Practice Experts for HCC (RELPEC) Study Group and HCC 48 Group (hepatocellular carcinoma experts from 48 clinics). Albumin-Bilirubin (ALBI) Grade as Part of the Evidence-Based Clinical Practice Guideline for HCC of the Japan Society of Hepatology: A Comparison with the Liver Damage and Child-Pugh Classifications. Liver Cancer. 2017;6:204-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 175] [Article Influence: 19.4] [Reference Citation Analysis (2)] |
| 21. | Chan AW, Chong CC, Mo FK, Wong J, Yeo W, Johnson PJ, Yu S, Lai PB, Chan AT, To KF, Chan SL. Applicability of albumin-bilirubin-based Japan integrated staging score in hepatitis B-associated hepatocellular carcinoma. J Gastroenterol Hepatol. 2016;31:1766-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, Gudat F, Denk H, Desmet V, Korb G, MacSween RN. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696-699. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3521] [Cited by in RCA: 3836] [Article Influence: 123.7] [Reference Citation Analysis (2)] |
Manuscript source: Invited Manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Egypt
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
P-Reviewer: Yu XJ, Zhang Y S-Editor: Cui LJ L-Editor: Wang TQ E-Editor: Zhang YL