Published online Jun 27, 2018. doi: 10.4254/wjh.v10.i6.425
Peer-review started: December 22, 2018
First decision: March 8, 2018
Revised: March 13, 2018
Accepted: April 11, 2018
Article in press: April 11, 2018
Published online: June 27, 2018
Processing time: 132 Days and 4.2 Hours
To determine the readmission rate, its reasons, predictors, and cost of 30-d readmission in patients with cirrhosis and ascites.
A retrospective analysis of the nationwide readmission database (NRD) was performed during the calendar year 2013. All adults cirrhotics with a diagnosis of ascites, spontaneous bacterial peritonitis, or hepatic encephalopathy were identified by ICD-9 codes. Multivariate analysis was performed to assess predictors of 30-d readmission and cost of readmission.
Of the 59597 patients included in this study, 18319 (31%) were readmitted within 30 d. Majority (58%) of readmissions were for liver related reasons. Paracentesis was performed in 29832 (50%) patients on index admission. Independent predictors of 30-d readmission included age < 40 (OR: 1.39; CI: 1.19-1.64), age 40-64 (OR: 1.19; CI: 1.09-1.30), Medicaid (OR: 1.21; CI: 1.04-1.41) and Medicare coverage (OR: 1.13; CI: 1.02-1.26), > 3 Elixhauser comorbidity (OR: 1.13; CI: 1.05-1.22), nonalcoholic cirrhosis (OR: 1.16; CI: 1.10-1.23), paracentesis on index admission (OR: 1.28; CI: 1.21-1.36) and having hepatocellular carcinoma (OR: 1.21; CI: 1.05; 1.39). Cost of index admission was similar in patients readmitted and not readmitted (P-value: 0.34); however cost of care was significantly more on 30 d readmission ($30959 ± 762) as compared to index admission ($12403 ± 378), P-value: < 0.001.
Cirrhotic patients with ascites have a 33% chance of readmission within 30-d. Younger patients, with public insurance, nonalcoholic cirrhosis and increased comorbidity who underwent paracentesis are at increased risk of readmission. Risk factors for unplanned readmission should be targeted given these patients have higher healthcare utilization.
Core tip: Cirrhotic patients with ascites have a 33% chance of 30-d readmission. Factors associated with 30-d readmission include age < 64 years, Medicaid and Medicare insurance, increased comorbidities, nonalcoholic cirrhosis, hepatocellular carcinoma and paracentesis during index admission. Based on identification of these predictors and significant cost involvement, there is need to find ways to counteract them and reduce 30-d readmission rate.
- Citation: Sobotka LA, Modi RM, Vijayaraman A, Hanje AJ, Michaels AJ, Conteh LF, Hinton A, El-Hinnawi A, Mumtaz K. Paracentesis in cirrhotics is associated with increased risk of 30-day readmission. World J Hepatol 2018; 10(6): 425-432
- URL: https://www.wjgnet.com/1948-5182/full/v10/i6/425.htm
- DOI: https://dx.doi.org/10.4254/wjh.v10.i6.425
The prevalence of cirrhosis in the United States has increased from 400000 to 600000 individuals in the past decade[1,2]. Approximately, 5%-7% of patients with compensated cirrhosis develop decompensation each year[3,4]. Decompensation of cirrhosis is marked by complications such as ascites, spontaneous bacterial peritonitis (SBP), hepatic encephalopathy, esophageal varices, and/or jaundice[2,3,5]. Patients with decompensated cirrhosis have worse outcomes with a median life expectancy of 2 years compared to 12 years in patients with compensated disease[3].
Ascites is one of the early signs of portal hypertension and decompensated cirrhosis[5]. The development of ascites is an ominous sign with a mortality rate of 50% in 2 years after initial development[6]. Patients with symptomatic, treatment refractory, or ascites complicated by SBP have an even higher mortality rate, estimated around 50% in 6 mo[7,8]. Paracentesis is a low risk procedure and recommended in all patients with refractory or symptomatic ascites on hospital admission to diagnose SBP and relieve symptoms[9,10]. Recent national studies have shown reduced inpatient short-term mortality in those who underwent paracentesis during hospitalization[10,11]. However, increased length of hospital stay and hospital charges were also reported in paracentesis group[10].
Given the economic burden of readmissions, the Patient Protection and Affordable Care Act instituted the Readmission Reduction Program that required the Centers for Medicare and Medicaid to reduce payment for hospitals with higher readmission rates[12]. Therefore, it is crucial to identify factors that predict 30-d readmissions in patients with decompensated cirrhosis and ascites given risk of frequent readmission and mortality. Readmission rates and mortality in cirrhotic patients have been reported in the North American Consortium for the Study of End-Stage Liver Disease cohort and insurance claim database[13,14]. Patients with decompensated cirrhosis and ascites are at higher risk of hospital readmission with recent studies reporting a readmission rate around 50%[13,14]. Moreover, presence of ascites and paracentesis was found to be independent predictors for readmission and increased 90 d and overall mortality[14]. However, there is no national report on the incidence of 30-d readmission rates and its predictors in patient population with ascites and/or HE. The aim of this study is to use Nationwide Readmission Database (NRD) to evaluate 30-d readmission rates, its reasons, predictors and cost of readmission.
A retrospective NRD study was performed from January 1st 2013 to December 1st 2013. NRD contains publically available data from 35 million hospitalizations over 21 geographically distributed states and offers insight into over 100 clinical and hospital variables[15]. National readmission rates from all payers and uninsured are provided in this analysis. The Ohio State University Data and Specimen Policy and Human Subjects Research Policy does not require informed consent for research conducted using public available data set as they do not involve “human subject.”
Utilizing International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, patients with a diagnosis of ascites (789.5, 789.69), SBP (567.23), or hepatic encephalopathy (572.2) and a diagnosis of cirrhosis (571.2, 571.5, 571.6) were included in this study. Patients were excluded from this study if they were under the age of 18, left against medical advice, transferred from a different facility, experienced mortality during the index admission, or were pregnant. Patients with missing length of stay between admissions were also excluded from this study. Moreover, if a patient was admitted more than once in 30 d, only the first readmission was included.
During index admission, multiple variables were evaluated to determine association with 30-d readmission. Patient demographics included age, gender, primary insurance payer, and annual income. Hospital demographics included size and type-urban-teaching, urban non-teaching and rural. Other variables of interest were identified using the appropriate ICD-9 codes and included comorbidities, evaluated by the Elixhauser co-morbidity scale and features of liver decompensation defined as the presence of esophageal varices, hepatorenal syndrome, and hepatocellular carcinoma. Etiology of cirrhosis was also determined by ICD-9 codes and was divided broadly as alcoholic vs non-alcoholic liver disease (Supplementary Appendix 1). Each patient was evaluated in order to determine if a paracentesis was performed on index admission. The procedure was identified using the proper procedural code (Supplementary Appendix 1).
We studied the 30-d readmission rate, reasons for readmission, predictors of 30-d readmission and cost with an emphasis on the effect of paracentesis in patients with cirrhosis and ascites. Reasons for readmission were divided into liver vs non-liver related based on the primary diagnosis on the 30-d readmission then we specifically evaluated the top 10 liver related reasons for readmission. We also studied the length of stay, cost during index admission and the difference of cost of index admission and readmission at 30 d.
All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, United States) on weighted data and accounted for the complex survey design. Chi-square test was used to compare proportions and t-test was used to compare means. A multivariate logistic regression model was fit to identify independent predictors for 30-d readmission where results are presented as odds ratios (OR) with 95% confidence intervals (CI). Variables included in the model were determined through stepwise selection where paracentesis, age, gender, type of insurance, income, Elixhauser comorbidity score, hospital size and type, etiology of cirrhosis and features of liver decompensation were eligible for inclusion.
There were 59597 patients included in this study with 18319 (33%) readmitted within 30 d. Mean age of patients in our study group was 59 ± 0.12 years. On univariate analysis, patients’ ≤ 64 years (66% vs 65%, P value 0.004) were more likely to be readmitted within 30 d. Patients with 30-d readmission were also more likely to have Medicaid (24% vs 20%, P-value < 0.001) or Medicare (45% vs 44%, P-value < 0.001) as their primary insurance provider. Readmitted patients were more likely to have > 3 comorbidities (78% vs 76%, P-value 0.003), nonalcoholic cirrhosis (54% vs 48%, P-value < 0.001) and hepatocellular carcinoma (4% vs 3%, P-value 0.002). All other patient and hospital information including gender, income, features of decompensation, hospital size and type were not significantly different between patients that were readmitted within 30-d compared to patients that were not (Table 1).
| Overall | No readmission within 30 d | 30-day readmission | P-value | ||||
| n = 59597 | n = 41279 | n = 18319 | |||||
| Age (mean, SE) | 59.15 | 0.12 | 59.41 | 0.13 | 58.58 | 0.17 | < 0.001 |
| Age, yr | 0.004 | ||||||
| < 40 | 2636 | 4.42 | 1727 | 4.18 | 909 | 4.96 | |
| 40-64 | 38865 | 65.21 | 26798 | 64.92 | 12067 | 65.88 | |
| ≥ 65 | 18096 | 30.36 | 12754 | 30.90 | 5342 | 29.16 | |
| Gender | 0.679 | ||||||
| Male | 36582 | 61.38 | 25302 | 61.30 | 11280 | 61.58 | |
| Female | 23015 | 38.62 | 15976 | 38.70 | 7039 | 38.42 | |
| Type of insurance | < 0.001 | ||||||
| Medicare | 26282 | 44.18 | 18150 | 44.05 | 8132 | 44.48 | |
| Medicaid | 12784 | 21.49 | 8424 | 20.44 | 4360 | 23.85 | |
| Private | 11957 | 20.10 | 8383 | 20.34 | 3575 | 19.55 | |
| Other | 8465 | 14.23 | 6250 | 15.17 | 2216 | 12.12 | |
| Income (Zip Code) | 0.392 | ||||||
| 1-37999 | 18523 | 31.76 | 12722 | 31.49 | 5801 | 32.35 | |
| 38000-47999 | 16491 | 28.27 | 11394 | 28.20 | 5097 | 28.43 | |
| 48000-63999 | 13613 | 23.34 | 9542 | 23.62 | 4071 | 22.70 | |
| 64000+ | 9702 | 16.63 | 6740 | 16.68 | 2962 | 16.52 | |
| AHRQ-Elixhauser Index | 0.003 | ||||||
| < 3 | 13981 | 23.46 | 9923 | 24.04 | 4058 | 22.15 | |
| ≥ 3 | 45616 | 76.54 | 31356 | 75.96 | 14260 | 77.85 | |
| Hospital size | 0.646 | ||||||
| Small | 6345 | 10.65 | 4435 | 10.75 | 1910 | 10.43 | |
| Medium | 13725 | 23.03 | 9555 | 23.15 | 4169 | 22.76 | |
| Large | 39527 | 66.32 | 27288 | 66.11 | 12239 | 66.81 | |
| Type of hospital | 0.020 | ||||||
| Urban non-teaching | 22770 | 38.21 | 15896 | 38.51 | 6875 | 37.53 | |
| Urban teaching | 30504 | 51.18 | 20879 | 50.58 | 9625 | 52.54 | |
| Rural | 6322 | 10.61 | 4504 | 10.91 | 1819 | 9.93 | |
| Etiology of cirrhosis | < 0.001 | ||||||
| Alcoholic | 34242 | 57.45 | 24072 | 58.32 | 10170 | 55.52 | |
| Non-alcoholic | 25356 | 42.55 | 17207 | 41.68 | 8149 | 44.48 | |
| In-hospital procedures | |||||||
| Paracentesis | 29832 | 50.06 | 19914 | 48.24 | 9918 | 54.14 | < 0.001 |
| Features of liver decompensation | |||||||
| Esophageal varices | 272 | 0.46 | 201 | 0.49 | 71 | 0.39 | 0.313 |
| Portal hypertension | 22074 | 37.04 | 15264 | 36.98 | 6810 | 37.17 | 0.794 |
| Hepatorenal syndrome | 2734 | 4.59 | 1817 | 4.40 | 917 | 5.00 | 0.055 |
| Hepatocellular carcinoma | 2274 | 3.82 | 1471 | 3.56 | 803 | 4.38 | 0.002 |
| Index admission mortality1 | |||||||
| None | 59566 | 94.41 | -- | -- | -- | -- | |
| Mortality | 3526 | 5.59 | -- | -- | -- | -- | |
| Calendar year mortality | < 0.001 | ||||||
| None | 53603 | 89.97 | 38960 | 94.42 | 14643 | 79.95 | |
| Mortality | 5978 | 10.03 | 2304 | 5.58 | 3673 | 20.05 | |
| Length of stay (mean, SE) | 5.69 | 0.08 | 5.66 | 0.10 | 5.77 | 0.10 | 0.345 |
| Cost (mean, SE) | 12488 | 363 | 12403 | 378 | 12680 | 421 | 0.391 |
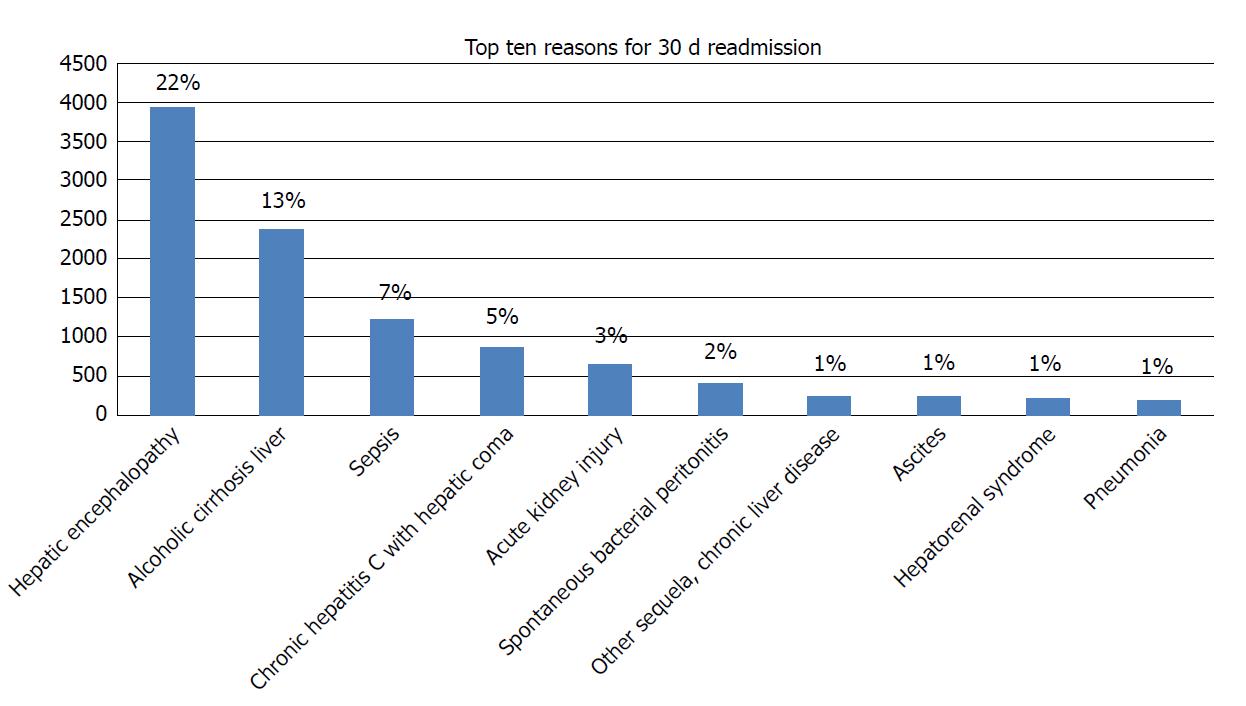
Reasons for 30-d readmission were grouped into liver related vs non liver related. Most readmissions (58%) were liver related with the number one reason for 30 d readmission being hepatic encephalopathy (Figure 1).
A total of 29832 (50%) patients underwent paracentesis during their index admission. Paracentesis during index admission was significantly higher in patients readmitted (n = 9918; 54%) as compared to those not readmitted within 30 d (n = 19914; 48%), P-value < 0.001 (Table 1).
On multivariate analysis, patients under the age of 40 years (OR: 1.39; CI: 1.19-1.64, P-value: < 0.001) and those between 40 and 64 (OR: 1.18; CI: 1.08 - 1.30, P-value: < 0.001) were more likely to be readmitted than patients ≥ 65 years (Table 2). Other independent predictors of 30-d readmission included: Medicaid (OR: 1.20; CI: 1.08-1.33; P-value: < 0.001) or Medicare insurance (OR: 1.13; CI: 1.02-1.26; P-value <0.001) vs private insurance, > 3 comorbidities on the Elixhauser comorbidity scale (OR: 1.13; CI: 1.05-1.22; P-value: 0.001), nonalcoholic cirrhosis (OR: 1.16; CI: 1.10-1.23; P-value: < 0.001) and hepatocellular carcinoma (OR: 1.21, CI: 1.05-1.39; P-value: 0.010). Most importantly, a paracentesis during index admission was also an independent predictor of 30-d readmission (OR: 1.28; CI: 1.21-1.36; P-value: < 0.001) (Table 2).
| OR (95%CI) | P-value | ||
| Age, yr | < 0.001 | ||
| < 40 | 1.42 | (1.22, 1.66) | |
| 40-64 | 1.19 | (1.09, 1.30) | |
| ≥ 65 | Reference | ||
| Type of insurance | < 0.001 | ||
| Private | Reference | ||
| Medicare | 1.13 | (1.02, 1.26) | |
| Medicaid | 1.20 | (1.08, 1.33) | |
| Other | 0.83 | (0.75, 0.92) | |
| AHRQ-elixhauser index | 0.001 | ||
| < 3 | Reference | ||
| ≥ 3 | 1.13 | (1.05, 1.22) | |
| Etiology of cirrhosis | < 0.001 | ||
| Alcoholic | Reference | ||
| Non-alcoholic | 1.16 | (1.10, 1.23) | |
| Paracentesis | 1.28 | (1.21, 1.36) | < 0.001 |
| Hepatocellular Carcinoma | 1.21 | (1.05, 1.39) | 0.010 |
The average length of stay during index admission was 5.69 ± 0.08 d. Length of stay was not significantly different between patients that were readmitted within 30 d (5.77 ± 0.10 d) and patients that were not (5.66 ± 0.10 d), P-value 0.34 (Table 1). Length of stay was also not an independent predictor of readmission on multivariate analysis (Table 2).
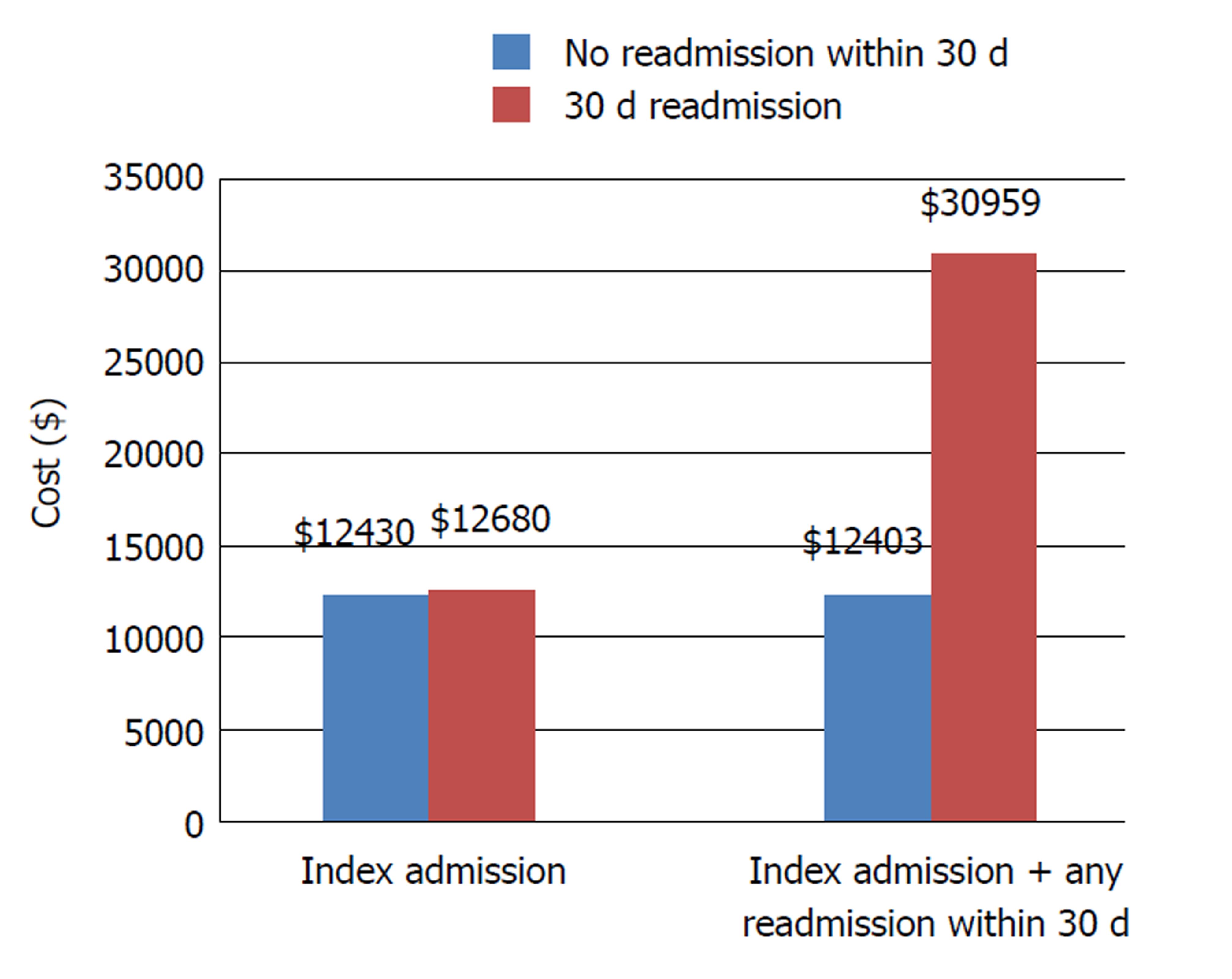
Cost of index hospitalization was similar (mean: $12403 ± 378 vs mean: $12680 ± 421, P-value = 0.391), however, cost of 30-d readmission (mean: $18120 ± 476) was higher than the cost of index admission (mean: $12403 ± 378), P-value: < 0.001). Cumulative total hospital cost for all admissions in calendar year was also significantly greater for patients readmitted within 30 d (mean: $51472 ± 1265) compared to patients not readmitted within 30 d (median: $23765 ± 595) (Figure 2).
In this study based on the Nationwide Readmission Database, approximately 1/3rd of patients with cirrhosis complicated by ascites and/or hepatic encephalopathy were readmitted within 30 d. Most patients were readmitted with liver related reasons. Half of the admitted patients underwent paracentesis. Independent predictors of 30-d readmission included younger age, Medicaid and Medicare insurance, encephalopathy cirrhosis, increased comorbidities, hepatocellular carcinoma and paracentesis during index admission. Patients that were readmitted within 30 d contributed to increased healthcare utilization. These predictors of 30-d readmission should be recognized in patients with decompensated cirrhosis and strategies designed to minimize readmissions as it has significant impact on healthcare utilization.
Diagnostic paracentesis to rule out SBP is part of quality indicators developed for the care of patients with cirrhosis admitted to the hospital with ascites and HE and is considered a safe procedure[16]. However, large volume paracentesis (LVP) is needed in certain situations for diagnostic and therapeutic purposes to relieve symptoms of tense ascites. Over the course of cirrhosis, patients may also require LVP when they develop diuretic refractory or diuretic resistant ascites, resulting in increased frequency of procedural intervention and rates of complication which could prompt readmission and increased cost[17]. Patients who undergo frequent LVP are subject to complications, such as post paracentesis circulatory dysfunction, which leads to faster re-accumulation of ascites, hyponatremia, renal impairment, and shorter survival. Given these complications, patients that undergo LVP would have higher rates of 30-d readmission and cost, which was noted in this study[18]. Despite these findings, it is important to note that performing a paracentesis is a quality indicator in cirrhotic patients with ascites or encephalopathy to evaluate for SBP; albeit paracentesis performance may be associated with increased 30-d readmission[10].
We identified that patients under the age of 64 were more likely to be readmitted within 30 d compared to older patients, which is consistent with previous studies[14]. This may seem counterintuitive, but reported in previous studies on patients with cirrhosis and in other chronic diseases, including chronic obstructive pulmonary disease (COPD)[19,20]. It is hypothesized that this is influenced by the “survivor effect” where younger patients admitted to the hospital typically have more severe disease compared to older patients[21]. Younger patients also tend to be better candidates for surgical intervention and the complications from these procedures may result in an increased risk of readmission[22].
Our results regarding Medicaid and Medicare as a predictor of 30-d readmission are in line with other studies showing a similar trend of increased readmission rates in patients with government funded insurances[21]. Multiple reasons for early readmission in Medicaid population are proposed including inability to schedule prompt hospital follow up, poor compliance with follow up appointment due to lack of support person or transportation, etc[23].
Other factors associated with readmission in patients with cirrhosis and ascites included higher number of comorbid conditions. Patients with multiple, complex medical conditions are more likely to return to medical care as they usually belong to a lower socioeconomic scale and are in poor general health[24].
Unplanned readmission at 30 d in patients with cirrhosis and ascites places a large financial burden on the healthcare system. This study shows that an unplanned readmission within 30 d increases the cost of management by more than 100%. In fact, unplanned 30 d readmission cost almost double the cost of index admission and the majority of the expense in the calendar year, further emphasizing the need to focus on modifiable factors that are associated with readmission in order to reduce cost of care[25,26]. Hospital readmission have been proven to be more expensive in previous literature as many of these patients are readmitted for hospital acquired infections, complications from previous admissions or poor discharge planning[27].
Recognizing factors associated with readmission and increased cost is crucial in order to reduce subsequent readmissions, hospital costs, morality, and ultimately improve quality of life. While age is a non-modifiable risk factors and insurance provider is challenging to modify, these patients should be targeted for interventions that are proven to reduce readmission rates, including a call from healthcare provider, early outpatient follow up and providing patients with enough supply of medications prior to discharge[28,29]. Patients that undergo frequent paracentesis should be evaluated early for other interventions, such as a transjugular intrahepatic portosystemic shunt (TIPS) or liver transplantation in order to prevent frequent readmission and costs associated with frequent large volume paracentesis[30]. Arrangement of outpatient clinic or day unit paracentesis may also be helpful in avoiding readmission. Further interventions to reduce readmission rates should be researched in order to improve hospital outcomes in this vulnerable and complicated patient population.
Utilizing the NRD provides a major advantage when evaluating factors associated with readmission and long-term outcomes, as this database allows individual/unique patients to be followed longitudinally over the course of a calendar year. This cannot be performed with the Nationwide Inpatient Sample database. Limitations of this study must be kept in mind while reviewing the results; NRD is an administrative database, which is dependent on ICD-9 coding; however, the validity of these codes has been determined in previous studies. Ascites is influenced by other factors such as hypoalbuminemia, portal hypertension, HCC with portal vein thrombosis; however laboratory results cannot be determined from the NRD and other factors are subject to the accuracy of ICD-9 codes. In addition, the indication for paracentesis could not be determined and we are unable to differentiate between diagnostic and large volume paracentesis as both have similar ICD-9 codes. In our clinical experience, most patients undergo a large volume paracentesis at the time of a diagnostic paracentesis; therefore we assume most patients in this study had a LVP. Disease severity in NRD is dependent on coding accuracy for features of decompensation rather than MELD score or Child turcotte Pugh score which limits the accuracy in predicting disease severity. Given that this study is based on administrative nature of database, we were unable to determine the causality of paracentesis with 30 d and subsequent readmission. In addition, this study only evaluates patients during hospitalization therefore, outpatient mortality is not included in this study.
The prevalence of cirrhosis and its complications such as ascites, encephalopathy, and SBP are ever-increasing with a large economic burden in the United States. A significant part of the burden is related to increased readmission rates in this vulnerable patient population with projected 30-d readmission rate around 33%. Though a paracentesis is indicated in this group of patients to rule out SBP and for symptomatic relief, paracentesis was also associated with increased 30-d readmission and cost; therefore, strategies in this patient population to minimize 30-d readmission and unnecessary cost should be designed. Further research should be conducted to determine ways to reduce readmission rates and cost in this population.
Patients with decompensated cirrhosis secondary to ascites or hepatic encephalopathy are at high risk of complication and readmission. Previous studies have determined that performing a paracentesis in these patients will improve inpatient mortality; however, the effect of performing a paracentesis on 30-d readmission has not been studied.
Given the economic burden of readmissions, we aimed to determine the readmission rate in patients with decompensated cirrhosis with ascites and encephalopathy. Identifying factors associated with readmission are crucial to preventing unnecessary hospital admission and healthcare spending.
The objective for this study included determining 30-d readmission rate in patients with cirrhosis with ascites or encephalopathy, reasons for readmission, factors associated with readmission and cost of readmission.
We performed a retrospective database analysis utilizing the Nationwide Readmission Database. All adult patients with a diagnosis of cirrhosis and ascites or encephalopathy were included. Multivariate analysis was performed to assess predictors of 30-d readmission and cost of readmission.
The 30 d readmission rate in patients with cirrhosis and ascites or encephalopathy was 31% and the majority of patients were readmitted for liver related issues (58%). Paracentesis was performed on 50% of patients during the index admission. Factors associated with readmission included age under 64, Medicaid or Medicare insurance provider, greater than 3 Elixhauser comorbidities, nonalcoholic cirrhosis, hepatocellular carcinoma and undergoing a paracentesis on index admission. Cost of index admission between patients that were readmitted within 30 d and those that were not readmitted were similar; however cost of care was significantly higher for the readmission compared to the index admission.
This study determined the readmission rate and economic burden of 30-d readmission in patient with cirrhosis and ascites or encephalopathy. We also highlighted multiple factors associated with readmission, specifically undergoing a paracentesis that were associated with 30 d readmission. Modifying factors associated with readmission during index admission could reduce unplanned readmissions, decrease the economic burden associated with readmission and decrease patient morbidity and mortality.
Further directions for this research include implementing intervention to modify factors associated with readmission in order to determine the effect on readmission, cost and patient mortality.
| 1. | Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371:838-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1686] [Cited by in RCA: 1608] [Article Influence: 89.3] [Reference Citation Analysis (0)] |
| 2. | Scaglione S, Kliethermes S, Cao G, Shoham D, Durazo R, Luke A, Volk ML. The Epidemiology of Cirrhosis in the United States: A Population-based Study. J Clin Gastroenterol. 2015;49:690-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 519] [Article Influence: 47.2] [Reference Citation Analysis (0)] |
| 3. | D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol. 2006;44:217-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1892] [Cited by in RCA: 2216] [Article Influence: 110.8] [Reference Citation Analysis (3)] |
| 4. | Samonakis DN, Koulentaki M, Coucoutsi C, Augoustaki A, Baritaki C, Digenakis E, Papiamonis N, Fragaki M, Matrella E, Tzardi M. Clinical outcomes of compensated and decompensated cirrhosis: A long term study. World J Hepatol. 2014;6:504-512. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Nusrat S, Khan MS, Fazili J, Madhoun MF. Cirrhosis and its complications: evidence based treatment. World J Gastroenterol. 2014;20:5442-5460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 128] [Cited by in RCA: 163] [Article Influence: 13.6] [Reference Citation Analysis (8)] |
| 6. | Moore KP, Aithal GP. Guidelines on the management of ascites in cirrhosis. Gut. 2006;55 Suppl 6:vi1-v12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 215] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 7. | Siqueira F, Kelly T, Saab S. Refractory Ascites: Pathogenesis, Clinical Impact, and Management. Gastroenterol Hepatol. 2009;5:647-656. |
| 8. | Ribeiro TC, Chebli JM, Kondo M, Gaburri PD, Chebli LA, Feldner AC. Spontaneous bacterial peritonitis: How to deal with this life-threatening cirrhosis complication? Ther Clin Risk Manag. 2008;4:919-925. [PubMed] |
| 9. | Sudulagunta SR, Sodalagunta MB, Bangalore Raja SK, Khorram H, Sepehrar M, Noroozpour Z. Clinical Profile and Complications of Paracentesis in Refractory Ascites Patients With Cirrhosis. Gastroenterology Res. 2015;8:228-233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Orman ES, Hayashi PH, Bataller R, Barritt AS 4th. Paracentesis is associated with reduced mortality in patients hospitalized with cirrhosis and ascites. Clin Gastroenterol Hepatol. 2014;12:496-503.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Gaetano JN, Micic D, Aronsohn A, Reddy G, Te H, Reau NS, Jensen D. The benefit of paracentesis on hospitalized adults with cirrhosis and ascites. J Gastroenterol Hepatol. 2016;31:1025-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Readmissions Reduction Program. Available from: https: //www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. |
| 13. | Bajaj JS, Reddy KR, Tandon P, Wong F, Kamath PS, Garcia-Tsao G, Maliakkal B, Biggins SW, Thuluvath PJ, Fallon MB. The 3-month readmission rate remains unacceptably high in a large North American cohort of patients with cirrhosis. Hepatology. 2016;64:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 200] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 14. | Scaglione SJ, Metcalfe L, Kliethermes S, Vasilyev I, Tsang R, Caines A, Mumtaz S, Goyal V, Khalid A, Shoham D. Early Hospital Readmissions and Mortality in Patients With Decompensated Cirrhosis Enrolled in a Large National Health Insurance Administrative Database. J Clin Gastroenterol. 2017;51:839-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | NRD Database Documentation. Available from: https: //www.hcup-us.ahrq.gov/db/nation/nrd/nrddbdocumentation.jsp. |
| 16. | Kanwal F, Kramer J, Asch SM, El-Serag H, Spiegel BM, Edmundowicz S, Sanyal AJ, Dominitz JA, McQuaid KR, Martin P. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010;8:709-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 17. | Annamalai A, Wisdom L, Herada M, Nourredin M, Ayoub W, Sundaram V, Klein A, Nissen N. Management of refractory ascites in cirrhosis: Are we out of date? World J Hepatol. 2016;8:1182-1193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Lindsay AJ, Burton J, Ray CE. Paracentesis-Induced Circulatory Dysfunction: A Primer for the Interventional Radiologist. Semin Intervent Rad. 2014;31:276-278. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Simmering JE, Polgreen LA, Comellas AP, Cavanaugh JE, Polgreen PM. Identifying Patients With COPD at High Risk of Readmission. Chronic Obstr Pulm Dis. 2016;3:729-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Ganesh S, Rogal SS, Yadav D, Humar A, Behari J. Risk factors for frequent readmissions and barriers to transplantation in patients with cirrhosis. PLoS One. 2013;8:e55140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Barrett ML, Wier LM, Jiang HJ, Steiner CA. All-Cause Readmissions by Payer and Age, 2009-2013: Statistical Brief #199. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality, United States. . [PubMed] |
| 22. | Patel MS, Mohebali J, Shah JA, Markmann JF, Vagefi PA. Readmission following liver transplantation: an unwanted occurrence but an opportunity to act. HPB (Oxford). 2016;18:936-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Kerr EA, Siu AL. Follow-up after hospital discharge: does insurance make a difference? J Health Care Poor Underserved. 1993;4:133-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Szekendi MK, Williams MV, Carrier D, Hensley L, Thomas S, Cerese J. The characteristics of patients frequently admitted to academic medical centers in the United States. J Hosp Med. 2015;10:563-568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 25. | Berman K, Tandra S, Forssell K, Vuppalanchi R, Burton JR Jr, Nguyen J, Mullis D, Kwo P, Chalasani N. Incidence and Predictors of 30-Day Readmission Among Patients Hospitalized for Advanced Liver Disease. Clin Gastroenterol Hepatol. 2011;9:254-259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 139] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 26. | Golabi P, Fazel S, Otgonsuren M, Sayiner M, Locklear CT, Younossi ZM. Mortality assessment of patients with hepatocellular carcinoma according to underlying disease and treatment modalities. Medicine (Baltimore). 2017;96:e5904. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 193] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 27. | Greco G, Shi W, Michler RE, Meltzer DO, Ailawadi G, Hohmann SF, Thourani VH, Argenziano M, Alexander JH, Sankovic K. Costs associated with health care-associated infections in cardiac surgery. J Am Coll Cardiol. 2015;65:15-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 28. | Morales BP, Planas R, Bartoli R, Morillas RM, Sala M, Casas I, Armengol C, Masnou H. HEPACONTROL. A program that reduces early readmissions, mortality at 60 days, and healthcare costs in decompensated cirrhosis. Dig Liver Dis. 2018;50:76-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Volk ML. Hospital readmissions for decompensated cirrhosis. Clinical Liver Disease. 2014;4:138-140. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Bai M, Qi XS, Yang ZP, Yang M, Fan DM, Han GH. TIPS improves liver transplantation-free survival in cirrhotic patients with refractory ascites: an updated meta-analysis. World J Gastroenterol. 2014;20:2704-2714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 127] [Cited by in RCA: 129] [Article Influence: 10.8] [Reference Citation Analysis (2)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P- Reviewer: Niu ZS, Shimizu Y, Sirin G S- Editor: Cui LJ L- Editor: A E- Editor: Huang Y