©2014 Baishideng Publishing Group Inc.
World J Hepatol. Nov 27, 2014; 6(11): 800-811
Published online Nov 27, 2014. doi: 10.4254/wjh.v6.i11.800
Published online Nov 27, 2014. doi: 10.4254/wjh.v6.i11.800
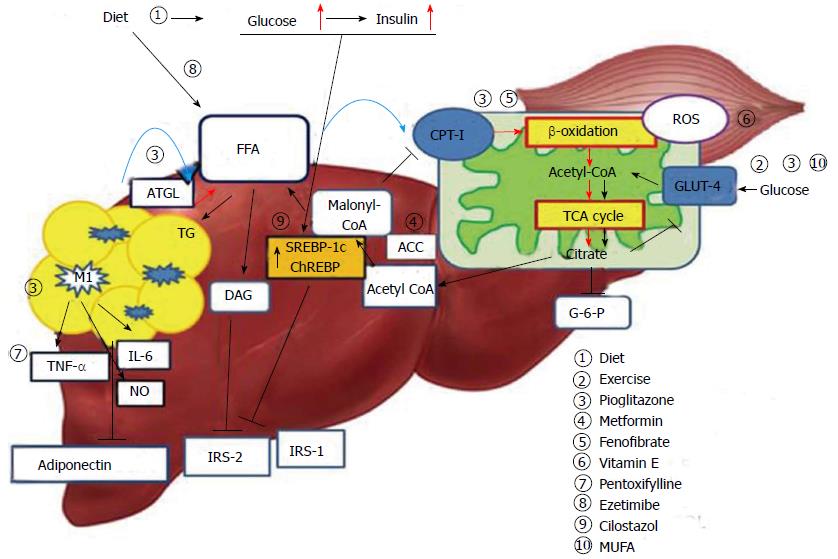
Figure 1 Mechanism of hepatic insulin resistance and the key pathway of drug action.
Delivery of FFAs to the liver and skeletal muscle is increased in insulin resistance conditions, and these are metabolized via mitochondrial β-oxidation. Consequently, hyperglycemia and increased hepatic FFA uptake reduce glucose uptake and oxidation in skeletal muscle. Diet and exercise are the main treatment strategies for this pathogenesis; insulin sensitizers and MUFA may contribute to reducing peripheral insulin resistance. Pioglitazone and fenofibrate act on β-oxidation of mitochondria and reduce hepatic steatosis. Accelerated β-oxidation also causes increased production of ROS. Vitamin E can reduce oxidative stress. Adipose tissue inflammation of the liver leads to inflammatory activation of hepatic Kupffer cells via classic response (M1) and produce inflammatory cytokines. This is also associated with decreased adiponectin levels and promotes hepatic steatohepatitis. Pentoxifylline inhibits TNF-α and alleviates steatohepatitis. Hyperglycemia caused by insulin resistance up-regulates lipogenic gene expression, such as SREBP-1c and ChREBP, and induces lipogenesis in hepatocytes. Cilostasol may inhibit SREBP-1c. FFA: Free fatty acid; TG: Triglyceride; CPT-I: Carnitine palmitoyltransferase-I; ACC: Acetyl-CoA carboxylase; ATGL: Adipose triglyceride lipase; ChREBP: Carbohydrate responsive element binding protein; SREBP-1c: Sterol regulatory element binding protein-1c; TCA: Tricarboxylic acid; ROS: Reactive oxygen species; IRS: Insulin receptor substrate; DAG: Diacylglycerol; G-6-P: Glucose 6-phosphate; TNF-α: Tumor necrosis factor- α; MUFA: Monosaturated fatty acids; M1: Kupffer cells activated via classic pathway.
- Citation: Yoon HJ, Cha BS. Pathogenesis and therapeutic approaches for non-alcoholic fatty liver disease. World J Hepatol 2014; 6(11): 800-811
- URL: https://www.wjgnet.com/1948-5182/full/v6/i11/800.htm
- DOI: https://dx.doi.org/10.4254/wjh.v6.i11.800