©The Author(s) 2025.
World J Hepatol. Oct 27, 2025; 17(10): 110412
Published online Oct 27, 2025. doi: 10.4254/wjh.v17.i10.110412
Published online Oct 27, 2025. doi: 10.4254/wjh.v17.i10.110412
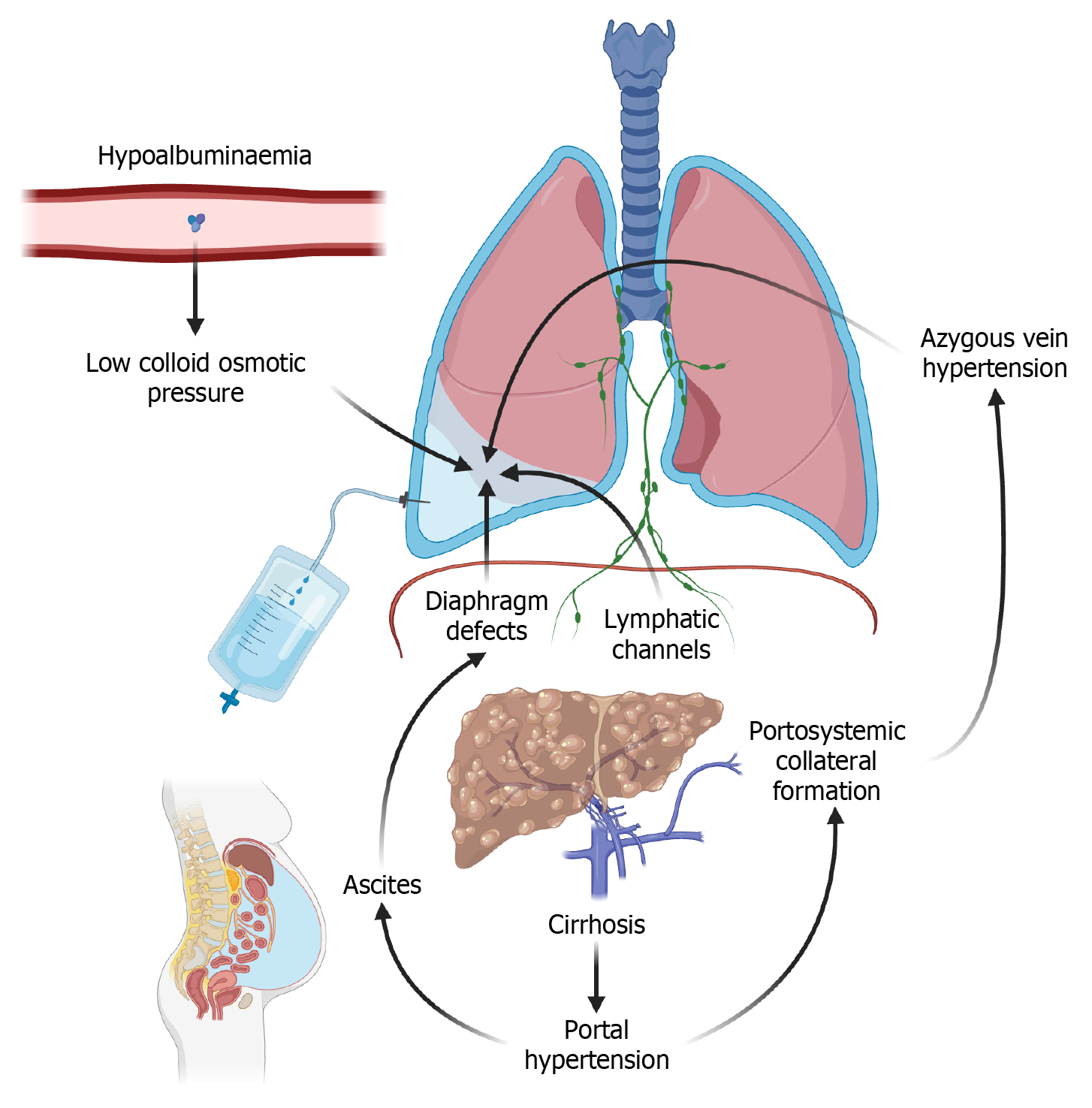
Figure 1 Proposed mechanisms of hepatic hydrothorax.
Among the proposed explanatory models for hepatic hydrothorax (HH) accumulation, migration of ascitic fluid through diaphragmatic defects is the most widely accepted. Progressive fibrosis and cirrhosis lead to portal hypertension and ascites. Long-standing and uncontrolled ascites forms blebs and fenestrations which permit direct communication between the peritoneal and pleural spaces. In addition, portal hypertension promotes the formation of portosystemic collaterals which in turn worsens azygous venous congestion. Impaired hepatic synthetic function results in hypoalbuminaemia and decreased colloid osmotic pressure. This exacerbates fluid accumulation and third spacing in potential spaces such as the pleural cavity. Finally, redistribution of interstitial fluid via lymphatic networks into the pleural space also contributes to HH accumulation.
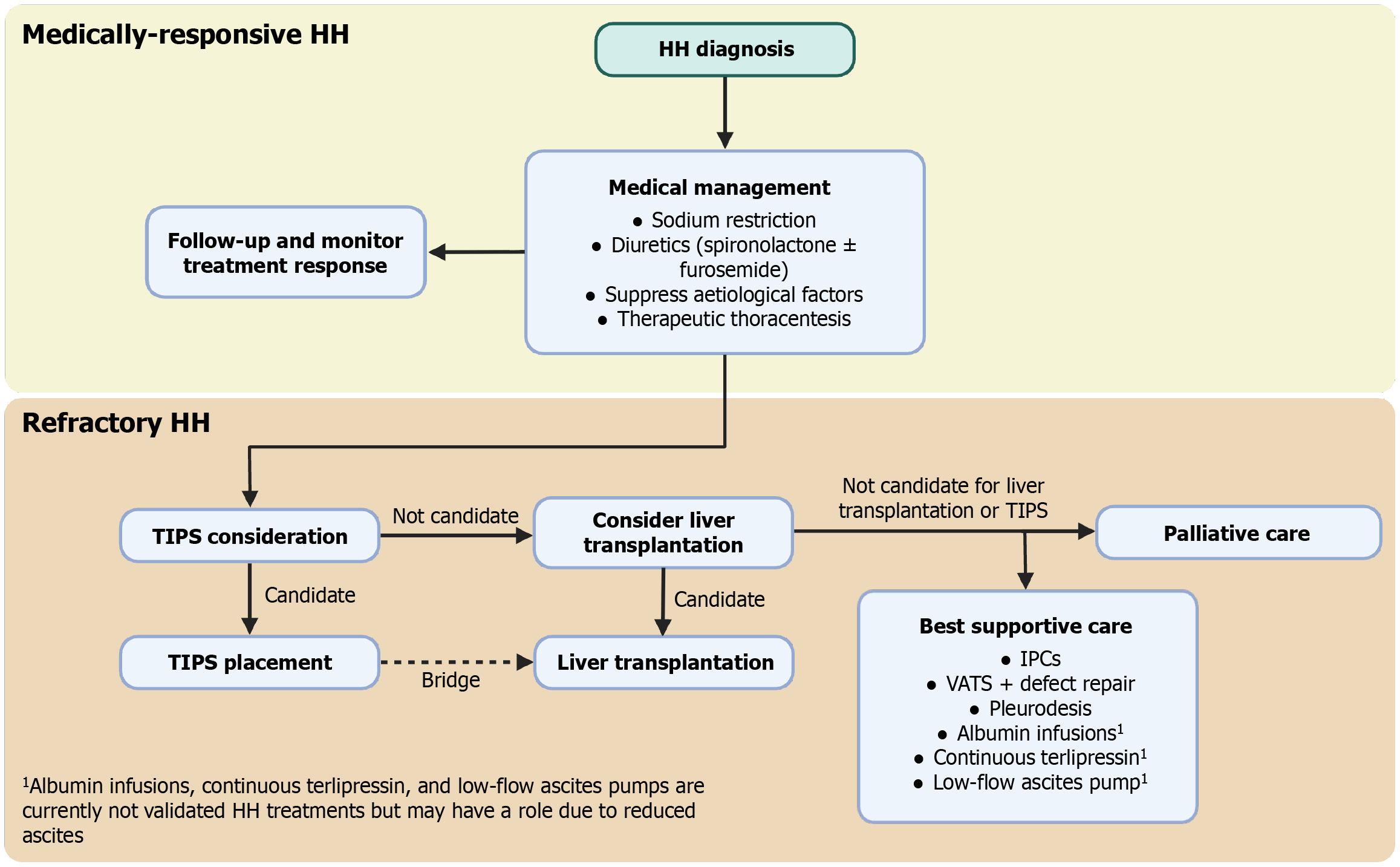
Figure 2 Management algorithm for hepatic hydrothorax.
Following hepatic hydrothorax (HH) diagnosis, medical management is initiated first. This includes dietary sodium restriction, diuresis, suppression of aetiological factors, and thoracentesis. If there is good response to medical therapy, patients should be followed-up and monitored closely. If patients remain symptomatic and/or demonstrate recurrent pleural effusions (e.g. radiographic or via pleural fluid aspirate) despite optimal medical therapy, this defines refractory HH. At this stage, transjugular intrahepatic portosystemic shunt (TIPS) eligibility should be considered in all patients. Successful TIPS placement may even serve as a bridge to liver transplantation. Eligibility for transplantation should be assessed particularly if the patient is not a TIPS candidate. If the patient is ineligible for TIPS or transplantation, best supportive or palliative care should be initiated. Treatment options for the former include indwelling pleural catheters and surgical approaches such as video-assisted thoracoscopic surgery or pleurodesis. Experimental treatments including a low-flow ascites pump device, albumin infusions, and continuous terlipressin are novel options which require validated trials in pure HH populations to support their use. HH: Hepatic hydrothorax; IPCs: Indwelling pleural catheters; TIPS: Transjugular intrahepatic portosystemic shunt; VATS: Video-assisted thoracoscopic surgery.
- Citation: Cilia BJ, Haridy J, Raj A, Hannah N. Hepatic hydrothorax as a manifestation of decompensated cirrhosis: An update on current management and future directions. World J Hepatol 2025; 17(10): 110412
- URL: https://www.wjgnet.com/1948-5182/full/v17/i10/110412.htm
- DOI: https://dx.doi.org/10.4254/wjh.v17.i10.110412