Published online May 15, 2003. doi: 10.3748/wjg.v9.i5.1086
Revised: November 14, 2002
Accepted: November 25, 2002
Published online: May 15, 2003
AIM: To introduce our latest innovation on technical manipulation of laparoscopic splenectomy.
METHODS: Under general anesthesia and carbon dioxide (CO2) pneumoperitoneum, 86 cases of laparoscopic splenectomy (LS) were performed. The patients were placed in three different operative positions: 7 cases in the lithotomic position, 31 cases in the right recumbent position and 48 cases in the right lateral position. An ultrasonic scissors was used to dissect the pancreaticosplenic ligament, the splenocolicum ligament, lienorenal ligament and the lienophrenic ligament, respectively. Lastly, the gastrosplenic ligament and short gastric vessels were dissected. The splenic artery and vein were resected at splenic hilum with Endo-GIA. The impact of different operative positions, spleen size and other events during the operation were studied.
RESULTS: The laparoscopic splenectomy was successfully performed on all 86 patients from August 1997 to August 2002. No operative complications, such as peritoneal cavity infection, massive bleeding after operation and adjacent organs injured were observed. There was no death related to the operation. The study showed that different operative positions could significantly influence the manipulation of LS. The right lateral position had more advantages than the lithotomic position and the right recumbent position in LS.
CONCLUSION: Most cases of LS could be accomplished successfully when patients are placed in the right lateral position. The right lateral position has more advantages than the conventional supine approach by providing a more direct view of the splenic hilum as well as other important anatomies. Regardless of operation positions, the major axis of spleen exceeding 15 cm by B-ultrasound in vitro will surely increase the difficulties of LS and therefore prolong the duration of operation. LS is a safe and feasible modality for splenectomy.
- Citation: Tan M, Zheng CX, Wu ZM, Chen GT, Chen LH, Zhao ZX. Laparoscopic splenectomy: the latest technical evaluation. World J Gastroenterol 2003; 9(5): 1086-1089
- URL: https://www.wjgnet.com/1007-9327/full/v9/i5/1086.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i5.1086
Endoscopic surgery has continued to gain popularity in almost all fields of general surgery. Since the first case of LS described by Delaitre and his colleagues[1] in 1991, more and more LS have been reported in the world[2-13]. LS has been proven to be a safe modality and become now the first choice of treatment for most patients requiring a splenectomy[12,14-19]. LS will be the best choice in laparoscopic surgery followed by the laparoscopic cholecystectomy[20,21]. However, we noticed that some anatomical and technical factors could significantly influence the outcome of LS. We herein report our latest results of 86 cases with LS.
From August 1997 to August 2002, there were 86 patients with various splenic disorders shown in Table 1 received LS. There were thirty-five males and fifty-one females, with the mean age of 41 years (range 16-71). The platelet count (PLT) of 47 patients, in this study, with immune thrombocytopenic purpura (ITP) ranged 12-77 × 109/L. The major axis of spleen by B-ultrasound in vitro preoperatively were less than 12 cm in fifty-four cases, 12-15 cm in twenty-one cases, 15-20 cm in eight cases and more than 20 cm in three cases. The patient with the largest spleen (23 cm) in this study was a case who suffered from portal hypertension, hypersplenism disease. Accessory spleen was detected in 6 cases with the size of 8 mm to 20 mm. The same surgeon performed all LSs.
| Diagnosis | Cases (percentage%) |
| Hematologic disorders | |
| ITP | 47 (54.7%) |
| Hereditary spherocytosis (HS) | 7 (8.1%) |
| Autoimmune hemolytic anemia | 4 (4.7%) |
| Aplastic anemia (AA) | 3 (3.5%) |
| Hodgkin’s lymphoma | 3 (3.5%) |
| Systemic lupus erythematosus (SLE) | 2 (2.3%) |
| Other disorders | |
| Hypersplenism | 12 (13.9%) |
| Multiple splenic cysts | 3 (3.5%) |
| Splenic tuberculosis | 3 (3.5%) |
| Splenic hemangioma | 2 (2.3%) |
| Total | 86 (100%) |
Patients with non-hematologic disorders were similar to those receiving traditional open splenectomy in preoperative management. Patients with ITP received an oral administration of prednisone 30-40 mg twice a day and high doses of immunoglobulin G (400 mg/kg per day) 3-5 days for at least one week prior to the operation to raise the platelet count to a mean value of 80 (range 14-110) × 109/L. Intravenous administration of prophylactic antibiotics and hydrocortisone 200-300 mg were needed immediately before operation. Prednisone should be given continuously after the operation and reduced in dose gradually according to clinical situations.
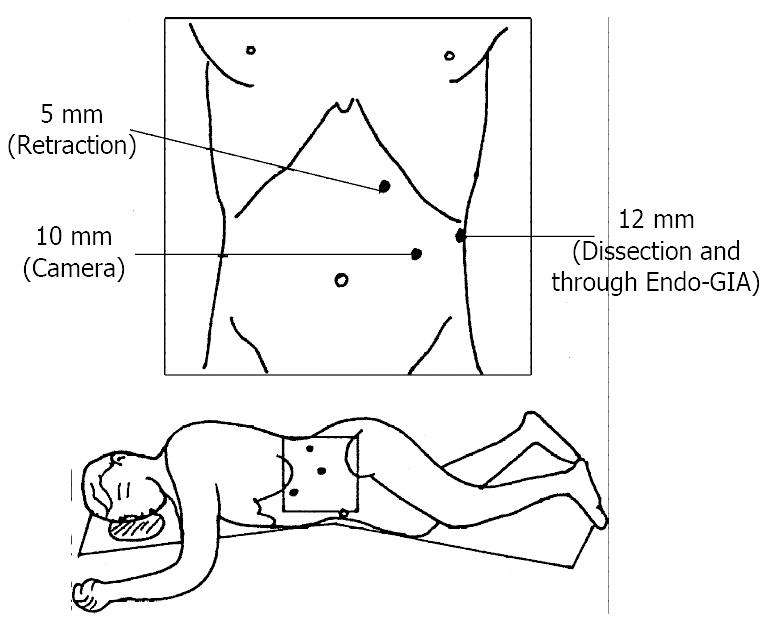
All patients received the general anesthesia and were placed in three different operative positions: 7 cases in the lithotomic position, 31 cases in the right recumbent position and 48 cases in the right lateral position. In the right recumbent position and the lateral position, three trocars were usually used to perform the LS (Figure 1). Once all ports were placed, a 30o telescope was introduced through the 10 mm trocar into the peritoneal cavity. Ultrasonic scissors were used to dissect the pancreaticosplenic ligament, splenocolicum ligament, lienorenal ligament and lienophrenic ligament, respectively. Lastly, the gastrosplenic ligament and short gastric vessels were dissected. The splenic artery and vein were resected at splenic hilum with Endo-GIA staplers (Autosuture CO; USA), which enabled safe vascular operation for larger vessels. Finally, the spleen was extracted in a plastic or nylon bag through a port wound which enlarged to about 3 cm.
No postoperative complications or mortality occurred in any patients with LS, All patients were hemodynamically stable during the perioperative period.
Eighty-six cases underwent a successful LS with a mean operating time of 110 minutes (range 50-270 minutes) except one case with extensive dense adhesion around the spleen due to severe perisplenitis, for whom it took nearly six hours to accomplish the operation. The situations of patients with operating time over 120 minutes were: the initial five cases of our patients being conducted LS and eleven cases with spleen major axis exceeding 15 cm. The case with 23 cm in major axis of spleen took 270 minutes to finish the LS. Blood loss was estimated between 50-800 ml during operation in all patients. Three cases received intraoperative transfusion of 400 ml red blood cell. Fifty-two of eighty-six cases (60.5%) needed to place the drainage tube in lienalis recess postoperatively, which was removed within three days (1 to 3 days). The total amount of draining fluids was less than 100 ml (range15-100 ml). Recovery of bowel movement occurred within an average of twenty-two (range 18-50) hours after LS. Patients were discharged from hospital in three to six days postoperatively. For patients with ITP, a positive immediate response to splenectomy was defined as a PLT more than 100 × 109/L after surgery, which maintained without therapy. In 39 of the 47 patients with ITP, the effective rate of LS was 82.9% (39/47).
Splenectomy for those patients with hereditary sherocytosis (HS) was initially described by Sutherland and Burghard in 1910. With the advancement of laparoscopic instruments and surgeon’s experience, minimally invasive approach has been used extensively in many surgical procedures including splenectomy. Now LS has been recognized as a safe and effective treatment for hematologic disorders and other splenic diseases[22-25]. However, the spleen is fragile and is located deeply in the left upper quadrant, and the abdominal organs like stomach, omentum, and pancreas tail obscure the splenic hilum. Operators are faced with a great deal of difficulty and risk when dealing with LS.
Since the initial reports, early experience has been gained in patients with immune thrombocytopenic purpura and other splenic disorders in a number of centers. In all these early reports, patients received LS either in the supine or the lithotomic position, and laparoscope was placed through a port near the umbilicus. In our seven early LS cases, the patients were placed in the lithotomic position too. This position, however, may take exposure and dissection suboptimal, or even cumbersome. In the lithotomic position, the laparoscope is usually inserted through the trocar near the umbilicus, when peri-splenic adhesion or splenomegaly, causes trouble to expose and dissect the peri-splenic ligaments, such as lienorenal ligament and lienophrenic ligament. Also, this position is very difficult for surgeons to expose posterior-dorsal vessels of spleen clearly and retract spleen to the medial abdomen against its gravity, when attempted to dissect the superior splenic ligaments. For these reasons, we made the rest LS patients lie in the right recumbent position or the right lateral position. We found that the abdominant organs like stomach, omentum and colon all went to the right by their gravity, dorsal side of spleen was exposed satisfactorily, and the peri-splenic ligaments are dissected easily in these two positions. In our experience, it is easy to dissect ligaments, to mobilize spleen and to place the stapler without any tension when using the right lateral approach. The procedure we used can also reduce operating time and avoid spleen or capsule fractures. In this study, there was no massive intraoperative bleeding, and no injury to great splenic vessels was observed.
Splenomegaly was initially considered as a contraindication of laparoscopic splenectomy[26-31]. With the advancement of laparoscopic technology, LS of enlarged spleen has been performed successfully with laparoscopy[32-37]. However, the difficulty in conducting LS on splenomegaly is certainly greater than that on the spleen with normal size. As operative area is stuffed with enlarged spleen, the peri-splenic ligaments is relative shorter, and the splenic hilum is deeply hidden in the enlarged spleen, the manipulation of LS becomes very difficult. It is hard to dissect the dorsal and upper pole ligaments of spleen in this situation. A tear of splenic capsule and splenic pedicle hemorrhage can often occur. It is a common cause to alter LS to open splenectomy in splenomegaly. In our study, we found that the right lateral approach is particularly suitable for patients with splenomegaly. Surgeons easily manipulate in right lateral position by taking advantage of gravity of spleen to expose the retroperitoneal attachments and to dissection even in the presence of dense diaphragmatic adhesions. The right lateral position offers a better laparoscopic view and space for manipulation than other positions. Moreover, only three trocars are typically required, and splenic pedicle exposition can be performed easily with less risk of capsular disruption. In fact, we have used this position in all LS cases regardless of the size of spleen since 2000[38,39]. However, The disadvantage of the right lateral position is lack of wide visual field, which presents the possibility of missing the accessory spleen not located in the neighborhood of splenic hilum. In addition, the distance between costal margin and iliac crest is rather short in some patients with obesity being placed in the right lateral position, which may cause difficulty for laparoscopic manipulation.
After exploring the abdominal cavity, the lower pole ligament of spleen and splenocolic ligement should be dissected firstly. Then, lienorenal ligament and lienophrenic ligament were dissected in order. The gastosplenic ligament should be dissected after dealing with all peri-splenic ligaments, because these ligaments, especially lienophrenic ligament, create a narrow area between stomach and spleen. When the peri-splenic ligaments are dissected, the spleen will be turned down easily, the space between stomach and spleen will be enlarged, and the gastrosplenic ligament as well as short gastric vessels can be transected by ultrasonic scissors[40,41] or titanium clips. Following this procedure, the injury to stomach or the tear of upper pole of spleen can be avoided when dissecting the upper part of gastrosplenic ligament. At last, the splenic artery and vein are isolated and divided by endoscopic vascular staplers. Individual ligation of splenic vessels requires dissecting the artery and vein of splenic hilum, which may increase the risk of damage to the tail of pancreas and hilum vessels. The high success rate in our group may be related to the operative position we adopted which provides a nice exposure of hilum of the spleen, so that it is certain for endoscopic vascular stapler to cross the entire splenic hilar vessels completely. By the way, the application of stapling instrument is safer than other manners when dealing with the splenic hilum vessels.
Perisplenitis may lead to contraction of ligaments and adhesion of the spleen to the adjacent organs, which increases the difficulty of manipulation and the risk of operation. The adhesion and peri-splenic ligaments should be dissected with ultrasonic scissors carefully in order to avoid possible capsular being torn or great vessels broken, which will result in uncontrollable bleeding. Once the splenic hilum is exposed clearly, transection procedure should be taken before handling the upper pole of spleen. This procedure is very important for the enlarged spleen, which usually has autoinfection leading to inflammatory adhesions to the diaphragm and omentum. To mobilize all the peri-splenic ligaments before transecting the splenic hilum for patients with splenomegaly, it will take the branch for the root and easily lead to uncontrollable bleeding. In one of our cases, the operation took nearly six hours on the patient who suffered from severe perisplenitis and extensive dense adhesion around the spleen. Another two cases received intraoperative transfusion of 400 ml red blood cell, in which the possible causes of bleeding were considered as massively enlarged spleen (more than 20 cm), severe extensive dense adhesion and in the lithotomic position. Although more and more reports defined LS as a safe and easy operation in massive splenomegaly[42-46], we thought the major axis of spleen exceeding 15 cm will surely raise the difficulty and risk in LS.
For patient with hematology disorders, accessory spleen often results in unfavorable therapeutic outcome or recurrence of primary disease[47]. It is reported that the incidence of accessory spleens are 10% to 30% in patients with hematologic diseases[8,48-53]. In this series, we found six patients (12.8%) with accessory spleen. The "cure" rates of the patients with ITP in our group are approximately 83%, showing a good response to LS. However, it is considered that the period of follow-up was short in our study. So far there has been no data available of long-term cure rates of ITP by means of LS. The long-term follow-up is needed to answer this question. Notably, in a comparative study, the rate of discovery of accessory spleens was 3 times higher in open splenectomy than that in laparoscopic splenectomy[54]. The observation showed the need for a systematic search, in various sites such as splenic hilum, tail of pancreas, splenocolic and gastrosplenic ligaments, and the greater omentum, for accessory spleens during laparoscopic splenectomy.
Laparoscopic surgery has more advantages for improving postoperative course. The majority of our patients started to drink water eight hours after the operation. And the hospitalization ranged from three to six days.
In conclusion, laparoscopic splenectomy for patients with hematologic disorders and some other splenic diseases is technically safe and feasible. It is believe that it is easy to conduct laparoscopic splenectomy in the right lateral position. While in case of splenomegaly, the right lateral position provides better visualization than the lithotomic position and the right recumbent position. The lateral position offers many advantages than the conventional supine approach as it provides a more direct view of the splenic hilum by using the gravity of spleen to expose important anatomy. Regardless of the operative position, the major axis of spleen exceeding 15 cm by B-ultrasound in vitro surely increases the difficulty of LS and therefore prolongs the duration of operation.
| 1. | Delaitre B, Maignien B. [Splenectomy by the laparoscopic approach. Report of a case]. Presse Med. 1991;20:2263. [PubMed] |
| 2. | Hamamci EO, Besim H, Bostanoglu S, Sonişik M, Korkmaz A. Use of laparoscopic splenectomy in developing countries: analysis of cost and strategies for reducing cost. J Laparoendosc Adv Surg Tech A. 2002;12:253-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Mostafa G, Matthews BD, Sing RF, Prickett D, Heniford BT. Elective laparoscopic splenectomy for grade III splenic injury in an athlete. Surg Laparosc Endosc Percutan Tech. 2002;12:283-286; discussion 283-286;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Tagaya N, Oda N, Furihata M, Nemoto T, Suzuki N, Kubota K. Experience with laparoscopic management of solitary symptomatic splenic cysts. Surg Laparosc Endosc Percutan Tech. 2002;12:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Tagaya N, Rokkaku K, Kubota K. Splenectomy using a completely needlescopic procedure: report of three cases. J Laparoendosc Adv Surg Tech A. 2002;12:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Chapman WH, Albrecht RJ, Kim VB, Young JA, Chitwood WR. Computer-assisted laparoscopic splenectomy with the da Vinci surgical robot. J Laparoendosc Adv Surg Tech A. 2002;12:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Corcione F, Esposito C, Cuccurullo D, Settembre A, Miranda L, Capasso P, Piccolboni D. Technical standardization of laparoscopic splenectomy: experience with 105 cases. Surg Endosc. 2002;16:972-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Torelli P, Cavaliere D, Casaccia M, Panaro F, Grondona P, Rossi E, Santini G, Truini M, Gobbi M, Bacigalupo A. Laparoscopic splenectomy for hematological diseases. Surg Endosc. 2002;16:965-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Pace DE, Chiasson PM, Schlachta CM, Mamazza J, Poulin EC. Laparoscopic splenectomy does the training of minimally invasive surgical fellows affect outcomes? Surg Endosc. 2002;16:954-956. [PubMed] |
| 10. | Fielding GA. Technical developments and a team approach leads to an improved outcome: lessons learnt implementing laparoscopic splenectomy. ANZ J Surg. 2002;72:459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Rosen M, Ponsky J. Minimally invasive surgery. Endoscopy. 2001;33:358-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Brodsky JA, Brody FJ, Walsh RM, Malm JA, Ponsky JL. Laparoscopic splenectomy. Surg Endosc. 2002;16:851-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Anthony ML, Hardee EM. Laparoscopic splenectomy in children with sickle cell disease. AORN J. 1999;69:567-577, 579-582; quiz 583-584, 587-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Rescorla FJ, Engum SA, West KW, Tres Scherer LR, Rouse TM, Grosfeld JL. Laparoscopic splenectomy has become the gold standard in children. Am Surg. 2002;68:297-301; discussion 301-302. [PubMed] |
| 15. | Ho CM. Splenic cysts: a new approach to partial splenectomy. Surg Endosc. 2002;16:717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Rosen M, Brody F, Walsh RM, Tarnoff M, Malm J, Ponsky J. Outcome of laparoscopic splenectomy based on hematologic indication. Surg Endosc. 2002;16:272-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 78] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Szold A, Kais H, Keidar A, Nadav L, Eldor A, Klausner JM. Chronic idiopathic thrombocytopenic purpura (ITP) is a surgical disease. Surg Endosc. 2002;16:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Katkhouda N, Mavor E. Laparoscopic splenectomy. Surg Clin North Am. 2000;80:1285-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Walsh RM, Heniford BT, Brody F, Ponsky J. The ascendance of laparoscopic splenectomy. Am Surg. 2001;67:48-53. [PubMed] |
| 20. | Fass SM, Hui TT, Lefor A, Maestroni U, Phillips EH. Safety of laparoscopic splenectomy in elderly patients with idiopathic thrombocytopenic purpura. Am Surg. 2000;66:844-847. [PubMed] |
| 21. | Katkhouda N, Manhas S, Umbach TW, Kaiser AM. Laparoscopic splenectomy. J Laparoendosc Adv Surg Tech A. 2001;11:383-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Park AE, Birgisson G, Mastrangelo MJ, Marcaccio MJ, Witzke DB. Laparoscopic splenectomy: outcomes and lessons learned from over 200 cases. Surgery. 2000;128:660-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 81] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 23. | Delaitre B, Champault G, Barrat C, Gossot D, Bresler L, Meyer C, Collet D, Samama G. [Laparoscopic splenectomy for hematologic diseases. Study of 275 cases. French Society of Laparoscopic Surgery]. Ann Chir. 2000;125:522-529. [PubMed] |
| 24. | Jaroszewski DE, Schlinkert RT, Gray RJ. Laparoscopic splenectomy for the treatment of gastric varices secondary to sinistral portal hypertension. Surg Endosc. 2000;14:87. [PubMed] |
| 25. | Budzyński A, Bobrzyński A, Krzywoń J. [Laparoscopic surgery of the spleen]. Przegl Lek. 2001;58:158-161. [PubMed] |
| 26. | Targarona EM, Espert JJ, Cerdán G, Balagué C, Piulachs J, Sugrañes G, Artigas V, Trias M. Effect of spleen size on splenectomy outcome. A comparison of open and laparoscopic surgery. Surg Endosc. 1999;13:559-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 76] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Kobayashi S, Sekimoto M, Tomita N, Monden M. [Laparoscopic splenectomy for a massive splenomegaly using a transcatheter technique]. Nihon Geka Gakkai Zasshi. 1998;99:733-736. [PubMed] |
| 28. | Terrosu G, Donini A, Baccarani U, Vianello V, Anania G, Zala F, Pasqualucci A, Bresadola F. Laparoscopic versus open splenectomy in the management of splenomegaly: our preliminary experience. Surgery. 1998;124:839-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Yuan RH, Chen SB, Lee WJ, Yu SC. Advantages of laparoscopic splenectomy for splenomegaly due to hematologic diseases. J Formos Med Assoc. 1998;97:485-489. [PubMed] |
| 30. | Targarona EM, Espert JJ, Balagué C, Piulachs J, Artigas V, Trias M. Splenomegaly should not be considered a contraindication for laparoscopic splenectomy. Ann Surg. 1998;228:35-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 31. | Nicholson IA, Falk GL, Mulligan SC. Laparoscopically assisted massive splenectomy. A preliminary report of the technique of early hilar devascularization. Surg Endosc. 1998;12:73-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 32. | Glasgow RE, Mulvihill SJ. Laparoscopic splenectomy. World J Surg. 1999;23:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Hebra A, Walker JD, Tagge EP, Johnson JT, Hardee E, Othersen HB. A new technique for laparoscopic splenectomy with massively enlarged spleens. Am Surg. 1998;64:1161-1164. [PubMed] |
| 34. | Rosin D, Brasesco O, Rosenthal RJ. [Laparoscopic splenectomy: new techniques and indications]. Chirurg. 2001;72:368-377. [PubMed] |
| 35. | Stanek A, Gruca Z, Hellmann A, Makarewicz W, Ciepłuch H, Kaska L, Oseka T. [Laparoscopic splenectomy with a postero-lateral approach in patients with idiopathic thrombocytopenic purpura]. Pol Merkur Lekarski. 2000;9:764-766. [PubMed] |
| 36. | Park A, Targarona EM, Trías M. Laparoscopic surgery of the spleen: state of the art. Langenbecks Arch Surg. 2001;386:230-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Esposito C, Schaarschmidt K, Settimi A, Montupet P. Experience with laparoscopic splenectomy. J Pediatr Surg. 2001;36:309-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 38. | de Csepel J, Quinn T, Gagner M. Laparoscopic exclusion of a splenic artery aneurysm using a lateral approach permits preservation of the spleen. Surg Laparosc Endosc Percutan Tech. 2001;11:221-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Tan M, Okada M, Wu Z. [Application of laparoscopic technique in splenectomy]. Zhonghua Waike Zazhi. 2001;39:599-601. [PubMed] |
| 40. | Pampaloni F, Valeri A, Mattei R, Presenti L, Noccioli B, Tozzini S, Di Lollo S, Pampaloni A. Laparoscopic decapsulation of a large epidermoid splenic cyst in a child using the UltraCision LaparoSonic Coagulating Shears. Pediatr Med Chir. 2002;24:59-62. [PubMed] |
| 41. | Schaarschmidt K, Kolberg-Schwerdt A, Lempe M, Saxena A. Ultrasonic shear coagulation of main hilar vessels: A 4-year experience of 23 pediatric laparoscopic splenectomies without staples. J Pediatr Surg. 2002;37:614-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 42. | Terrosu G, Baccarani U, Bresadola V, Sistu MA, Uzzau A, Bresadola F. The impact of splenic weight on laparoscopic splenectomy for splenomegaly. Surg Endosc. 2002;16:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Kercher KW, Matthews BD, Walsh RM, Sing RF, Backus CL, Heniford BT. Laparoscopic splenectomy for massive splenomegaly. Am J Surg. 2002;183:192-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 44. | Heniford BT, Park A, Walsh RM, Kercher KW, Matthews BD, Frenette G, Sing RF. Laparoscopic splenectomy in patients with normal-sized spleens versus splenomegaly: does size matter? Am Surg. 2001;67:854-857. [PubMed] |
| 45. | Hashizume M, Tomikawa M, Akahoshi T, Tanoue K, Gotoh N, Konishi K, Okita K, Tsutsumi N, Shimabukuro R, Yamaguchi S. Laparoscopic splenectomy for portal hypertension. Hepatogastroenterology. 2002;49:847-852. [PubMed] |
| 46. | Greene AK, Hodin RA. Laparoscopic splenectomy for massive splenomegaly using a Lahey bag. Am J Surg. 2001;181:543-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 47. | Ribó JM, García Aparicio L, Morales I. [Laparoscopic splenectomy in the treatment of hematologic diseases]. Cir Pediatr. 2001;14:69-72. [PubMed] |
| 48. | Anglin BV, Rutherford C, Ramus R, Lieser M, Jones DB. Immune thrombocytopenic purpura during pregnancy: laparoscopic treatment. JSLS. 2001;5:63-67. [PubMed] |
| 49. | Reddy VS, Phan HH, O'Neill JA, Neblett WW, Pietsch JB, Morgan WM, Cywes R. Laparoscopic versus open splenectomy in the pediatric population: a contemporary single-center experience. Am Surg. 2001;67:859-63; discussion 863-4. [PubMed] |
| 50. | Cogliandolo A, Berland-Dai B, Pidoto RR, Marc OS. Results of laparoscopic and open splenectomy for nontraumatic diseases. Surg Laparosc Endosc Percutan Tech. 2001;11:256-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 51. | Marcaccio MJ. Laparoscopic splenectomy in chronic idiopathic thrombocytopenic purpura. Semin Hematol. 2000;37:267-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | 54 Bresler L, Guerci A, Brunaud L, Ayav A, Sebbag H, Tortuyaux JM, Lederlin P, Boissel P. Laparoscopic splenectomy for idiopathic thrombocytopenic purpura: outcome and long-term results. World J Surg. 2002;26:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 53. | 55 Tanoue K, Okita K, Akahoshi T, Konishi K, Gotoh N, Tsutsumi N, Tomikawa M, Hashizume M. Laparoscopic splenectomy for hematologic diseases. Surgery. 2002;131:S318-S323. [PubMed] |
| 54. | 56 Tsiotos G, Schlinkert RT. Laparoscopic splenectomy for immune thrombocytopenic purpura. Arch Surg. 1997;132:642-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Edited by Xu XQ