Published online Dec 15, 2003. doi: 10.3748/wjg.v9.i12.2846
Revised: September 26, 2003
Accepted: October 22, 2003
Published online: December 15, 2003
Microvesicular pneumatosis intestinalis, also called “pseudolipomatosis” for resembling fatty infiltration, is characterized by the presence of small gas voids in the gastrointestinal wall, especially in mucosa. These voids are not lined with epithelia. There are few reported cases about colon, duodenum and skin. Because there is only one case report about pseudolipomatosis in the stomach, we re-evaluated 909 endoscopic biopsies taken from gastric corpus to check the presence of pseudolipomatosis. We determined pseudolipomatosis foci in 3 percent (n = 27) of biopsies. In two cases there were pseudolipomatosis foci in endoscopic biopsies having otherwise normal histologic findings, while there were pseudolipomatosis foci in endoscopic biopsies of 25 patients with gastritis. Helicobacter pylori was found in 85% of biopsies having pseudolipomatosis foci. In this study, we presented some histopathologic characteristics of pseudolipomatosis seen in gastric mucosa.
- Citation: Alper M, Akcan Y, Belenli OK, Çukur S, Aksoy KA, Suna M. Gastric pseudolipomatosis, usual or unusual? Re-evaluation of 909 endoscopic gastric biopsies. World J Gastroenterol 2003; 9(12): 2846-2848
- URL: https://www.wjgnet.com/1007-9327/full/v9/i12/2846.htm
- DOI: https://dx.doi.org/10.3748/wjg.v9.i12.2846
Microvesicular pneumatosis intestinalis which is also called “pseudolipomatosis” for resembling fatty infiltration, is characterized by the presence of small gas voids in the gastrointestinal wall, especially in mucosa[1]. These gas voids are not lined with epithelial cells. Since we came across only one letter about gastric mucosa while searching literature for our previous case report, in which we presented a case of pseudolipomatosis in the stomach, duodenum and colon, although recently in gastrointestinal system pseudolipomatosis was defined particularly in the colon, duodenum and skin, we investigated endoscopic biopsies with regard to pseudolipomatosis[1-8].
In this study, 909 endoscopic gastric biopsies were investigated at the Department of Pathology of Düzce Medical Faculty Abant Ýzzet Baysal University, between December 1998 and June 2003. Biopsies taken from the corpus for various reasons other than cancer were included in this study. Biopsies were fixed in 10% formaldehyde and subjected to automatic tissue follow-up procedures. We re-examined the 4-5 micron thick samples stained with hematoxylene eosin and modified Giemsa by a light microscope. When pseudolipomatosis was found, the presence and grade of inflammation, the presence of intestinal metaplasia, and the presence and concentration of Helicobacter pylori were determined. The absence of inflammation was designated as (0), and the presence of inflammation was classified as mild (1), moderate (2) and severe (3). The absence of Helicobacter pylori was designated as (0), and the presence was classified as scarce (1), moderate (2) and diffuse (3). Intestinal metaplasia was evaluated as present or absent, and atrophy as present or absent, if present as mild, moderate or severe. Three hundred and sixty-four (40%) subjects were female and 545 (60%) were male. The ages of patients ranged between 19 and 78 years with a mean of 46 years.
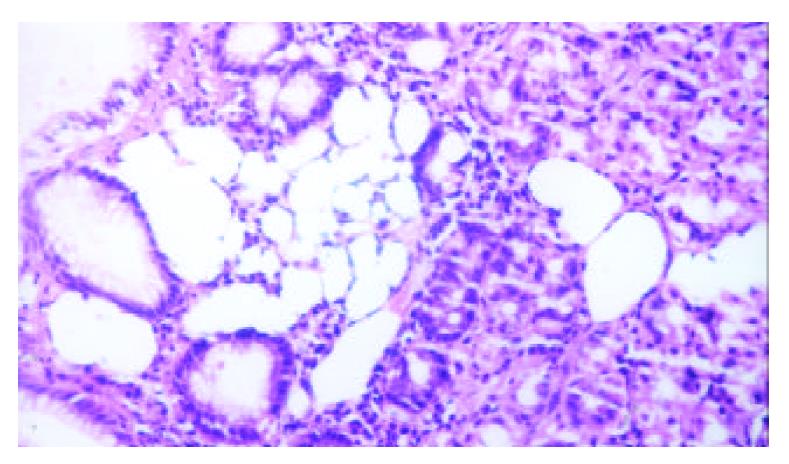
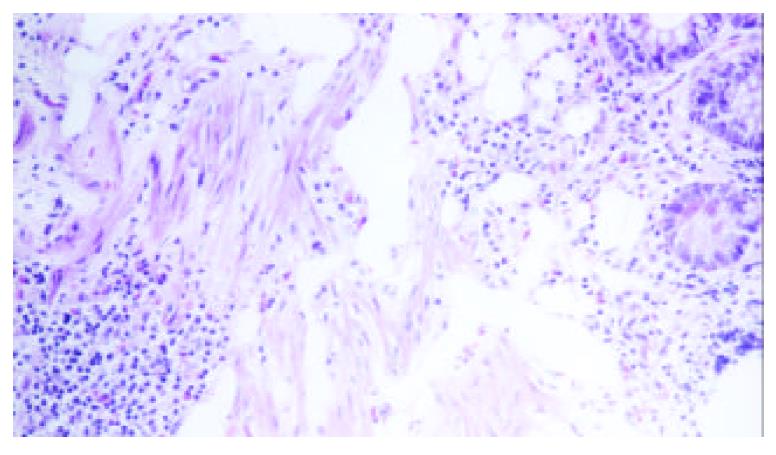
Pseudolipomatosis was found in 27 of 909 re-evaluated cases. Of these 27 patients, 15 were male and 12 were female. Male patients were between 28 and 56 years old, with a mean of 39 years, female patients were aged between 22 and 65 years, with a mean of 41 years. Mucosal vacuolation was characterized by empty spaces, 30-250 micron in diameter, associated with neither fibrosis/sclerosis nor a lymphocytic infiltrate. There was no evidence of true adipocyte differentiation, vascular markers, e.g. S-100 protein, F-VIII and F-XIII were negative. Vacuoles were found in different parts of the mucosa, although they could be seen beneath epithelia, in a few cases they were detected within muscularis mucosa as well (Figure 1 and Figure 2). Twenty five of the patients with pseudolipomatosis had gastritis. Of these patients 23 were Helicobacter pylori positive. Among the Helicobacter pylori positive patients, five had scarce, ten had moderate, and eight had diffuse bacteria. Among the 25 patients with gastritis, 5 had mild, 13 had moderate, and 7 had severe chronic inflammation. In 8 cases with gastritis, intestinal metaplasia was encountered. In all the cases with metaplasia goblet cells and in 4 cases Paneth cells were noticed. Two cases of gastritis had severe atrophy, and one case had mild atrophy. Four patients with gastritis had prior endoscopy for gastric complaints. The previous biopsy results were Helicobacter pylori gastritis with severe inflammatory activity in three cases, and Helicobacter pylori gastritis with moderate inflammatory activity in one case. Pseudolipomatosis was not found in previous endoscopic gastric biopsies of these four patients. However, in one of these patients, pseudolipomatosis was detected in duodenal and colonic biopsies[8]. Two other patients had undergone colonoscopy while being searched for malignancy. In samples taken from the colon pseudolipomatosis was not detected.
The patients who were Helicobacter pylori positive were given a course of treatment for Helicobacter pylori eradication composed of lansoprazol 30 mg daily for 15 days, clarithromycin bid 500 mg and amoxicilin bid 1000 mg for 10 days. One month later control biopsies were performed for 5 patients whose complaints were not fully resolved. We found that in two of them pseudolipomatosis continued while in the other three biopsies pseudolipomatosis was not found. In those cases in which pseudolipomatosis continued, we noticed that although Helicobacter pylori was decreased, it was not completely eradicated, and in the other three patients we saw that Helicobacter pylori was eradicated and the gastritis continued though decreased. Control biopsies were not performed for the remaining patients. In two patients with pseudolipomatosis, a 45-year-old female and a 39-year-old man, biopsies taken for non-specific abdominal pain showed no Helicobacter pylori, inflammation or metaplasia. In these patients no pathologic finding except mild edema could be demonstrated. These patients had no previous endoscopies. Vacuoles were seen in small foci in lamina propria, and were considered as pseudolipomatosis.
Mucosal pseudolipomatosis is a recently described endoscopic finding, most likely caused by intramucosal air. Because of their gross and microscopical similarity to fat, however, the term “pseudolipomatosis” is proposed. Although the etiopathogenesis of pseudolipomatosis is not so clear yet, some probable causes of it in the colon, duodenum and skin have been mentioned[1-8]. We could find only one case-report about gastric pseudolipomatosis except our one[6]. For this reason we searched how often pseudolipomatosis, yet its rate in colon increased contionusly, was found in gastric mucosa.
Pneumatosis coli is a rare condition characterized by multiple gas-filled cysts within the bowel wall. Mechanical, bacterial and biochemical theories have been availabe to explain the pathogenesis of pneumatosis in the colon[5]. Pneumatosis cyctoides intestinalis has been reported to be present together with other conditions such as pseudomembranous enterocolitis, necrotizing enterocolitis, bowel infarction, chronic obstructive pulmonary disease, intestinal obstruction, collagen vascular diseases (scleroderma, dermatomyositis, mixed connective tissue disease), systemic amyloidosis and iatrogenic conditions (after surgery or endoscopy), late-stage AIDS with cryptosporidial diarrhea, and Crohn’s disease[5]. Gagliardi et al[5] detected mucosal pseudolipomatosis foci in colon of 5 cases among 25 pneumatosis coli patients in their study. Micropneumatosis was reported to be caused by disinfectant hydrogen peroxide solution[3]. It might also be a result of colonoscopy application and usually disappeared three weeks after the procedure[4]. Commercially available endoscope disinfecting hydrogen peroxide solution could cause the unique form of colitis referred as pseudolipomatosis[3]. It was also reported in asymptomatic patients as an air pressure- related colonoscopy complication[4]. Mucosal pseudolipomatosis of the colon is an infrequent condition that occurs mainly in elderly males, usually involves the left colon, and is manifested clinically by passage of blood per rectum. Colonoscopy showed solitary or multiple whitish-yellowish plaques, which were localized or involved several segments[1]. Superficial dermal vacuoles resembling fatty infiltration of the skin have also been reported as pseudolipomatosis cutis[2]. Dermal vacuoles likely represent an artifact of tissue fixation or processing and are unrelated to the underlying pathologic process. Trotter et al[2] suggested the name pseudolipomatosis cutis, analogous to insufflation-induced colonic vacuolation, to distinguish this phenomenon from true dermal fatty infiltration and to emphasize its incidental, likely artifactual nature. As in colon and duodenum, histologic studies in the stomach demonstrated microscopic cavities in mucosa, measuring 20 to 300 micron in diameter. Histochemical stains showed that these cavities contained no lipids, suggesting that they were filled with gas. In the study of Gagliardi et al[5] 14 patients were treated with antidiarrhoeals and anti-inflammatory drugs, improvement was detected in 9 cases. There was a high recurrence rate, but with further courses of continued therapy remission was achieved in five patients. According to Gagliardi et al[5] the associations of pneumatosis coli with psychiatric disorders and mucosal pseudolipomatosis were new and of possible pathogenetic.
In our study, 23 out of 27 patients had Helicobacter pylori. In our previous case report, one patient was diagnosed as micropneumatosis on the first and second colonoscopy specimens at a four week interval[8]. After another four weeks during the first half of Helicobacter pylori gastritis treatment of the patient, colonoscopy was repeated for the third time, and micropneumatosis foci were not observed on pathological sections. In the present study, when control biopsy was performed one month later for 5 patients whose complaints were not resolved it was noticed that pseudolipomatosis continued in two of them while pseudolipomatosis was not seen in the other three in control biopsies. In those cases with persistent pseudolipomatosis, it was noticed that although Helicobacter pylori was decreased, it was not completely eradicated, and in the other three patients it was seen that Helicobacter pylori was eradicated and the gastritis findings were decreased. It is also possible that the control endoscopic biopsies may be taken from sites that are free of pseudolipomatosis. Since the conditions of some patients improved after the eradication therapy for Helicobacter pylori, this finding implicates that Helicobacter pylori may be one of the causative factors for micropneumatosis and pneumatosis cyctoides intestinalis. It can also be speculated that micropneumatosis grows with time and may lead to pneumatosis cyctoides intestinalis. The fact that micropneumatosis foci are also reported in most pneumatosis cyctoides intestinalis cases is supportive for this suggestion. The pseudolipomatosis type changes seen in mucosal biopsies should not be ignored by just considering them as artifacts. We think that, in order to determine the etiopathogenesis and significance of gastric mucosal pseudolipomatosis, more case reports are required.
| 1. | Ben Rejeb A, Khedhiri F. [Mucosal pseudo-lipomatosis of the colon. Apropos of a case with a review of the literature]. Arch Anat Cytol Pathol. 1989;37:254-257. [PubMed] |
| 2. | Trotter MJ, Crawford RI. Pseudolipomatosis cutis: superficial dermal vacuoles resembling fatty infiltration of the skin. Am J Dermatopathol. 1998;20:443-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Ryan CK, Potter GD. Disinfectant colitis. Rinse as well as you wash. J Clin Gastroenterol. 1995;21:6-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Waring JP, Manne RK, Wadas DD, Sanowski RA. Mucosal pseudolipomatosis: an air pressure-related colonoscopy complication. Gastrointest Endosc. 1989;35:93-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Gagliardi G, Thompson IW, Hershman MJ, Forbes A, Hawley PR, Talbot IC. Pneumatosis coli: a proposed pathogenesis based on study of 25 cases and review of the literature. Int J Colorectal Dis. 1996;11:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 79] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 6. | Stebbing J, Wyatt JI. Gastric 'pseudolipomatosis'. Histopathology. 1998;32:283-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Cook DS, Williams GT. Duodenal 'pseudolipomatosis'. Histopathology. 1998;33:394-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Belenli OK, Akcan Y, Alper M. Micropneumatosis coexistent with Helicobacter pylori and its improvement.. Indian J Gastroenterol. 2003;22:191-192. [PubMed] |
Edited by Wang XL