Published online Oct 7, 2025. doi: 10.3748/wjg.v31.i37.111081
Revised: July 19, 2025
Accepted: August 28, 2025
Published online: October 7, 2025
Processing time: 94 Days and 19.6 Hours
Endoscopic submucosal dissection (ESD) is considered one of the effective and minimally invasive methods for managing lateral spreading tumors of the intestine. However, with the widespread adoption of this technique, the incidence of complications is expected to increase. The most common complications of ESD are hemorrhage and perforation. Rare cases of obstruction after colorectal ESD have been reported, which are often easily misdiagnosed. Therefore, clinicians should maintain heightened awareness of this complication.
We report the case of a 50-year-old male who developed bowel obstruction following ESD. On the second day after the procedure, the patient presented with fever and a mild left lower abdominal pain. Physical examination revealed tenderness and rebound tenderness in the left lower quadrant. Plain abdominal radiographs demonstrated air-fluid levels and dilatation of the proximal bowel. The patient continued to fast and was treated with intravenous antibiotics. On the third postoperative day, he developed abdominal distension in the lower abdomen and vomited approximately 200 mL of greenish-yellow fluid, with no bowel movement for two days after the procedure. A diagnosis of obstruction after ESD was made. Continuous gastrointestinal decompression was initiated on the fourth day, resulting in symptomatic improvement. Follow-up abdominal radiographs showed marked improvement in the obstruction compared with prior imaging. The patient resumed oral intake and was discharged uneventfully on the eighth postoperative day.
Acute intestinal obstruction after ESD is a rare complication. Delayed diagnosis or misdiagnosis may be life-threatening. Clinicians should be vigilant for this condition following ESD.
Core Tip: Acute intestinal obstruction may occur as a severe complication following endoscopic submucosal dissection (ESD). The prognosis of ESD-related complications depends on the type and severity, as well as the timeliness and appropriateness of management. We report a very rare complication of ESD to enhance clinicians’ awareness of such events and to emphasize important procedural consideration for endoscopists.
- Citation: Zhang Q, Hong D, Zhou YC, He GX, Jiang T. Acute intestinal obstruction caused by endoscopic submucosal dissection: A case report. World J Gastroenterol 2025; 31(37): 111081
- URL: https://www.wjgnet.com/1007-9327/full/v31/i37/111081.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i37.111081
Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are the most common endoscopic techniques for managing precancerous lesions of the bowel and early-stage colorectal cancer. The maximum tumor size that can be reliably resected en bloc by EMR is approximately 2 cm[1]. ESD is more suitable for en bloc resection, with a lower recurrence rate after the procedure and without limitations regarding tumor size or location compared with EMR. Consequently, ESD is frequently performed worldwide, because the colorectal muscularis propria is relatively thin and the mucosa is rich in vessels. ESD carries a higher risk of complications, including hemorrhage and perforation. However, acute obstruction after ESD is an infrequent complication and is seldom reported in the literature. We report a case of a patient who developed acute obstruction less than 24 hours after ESD and was treated successfully with conservative management, including fasting, intravenous fluid therapy, broad-spectrum antibiotics, intestinal decompression, and mucosal clip closure. This approach yielded satisfactory results and avoided the need for surgery. The present report aims to raise clinical awareness of obstruction as a rare complication following ESD. Early recognition and appropriate management are essential to prevent serious consequences and improve patient outcomes.
A 50-year-old man developed abdominal pain after ESD, and bowel obstruction was diagnosed 18 hours later.
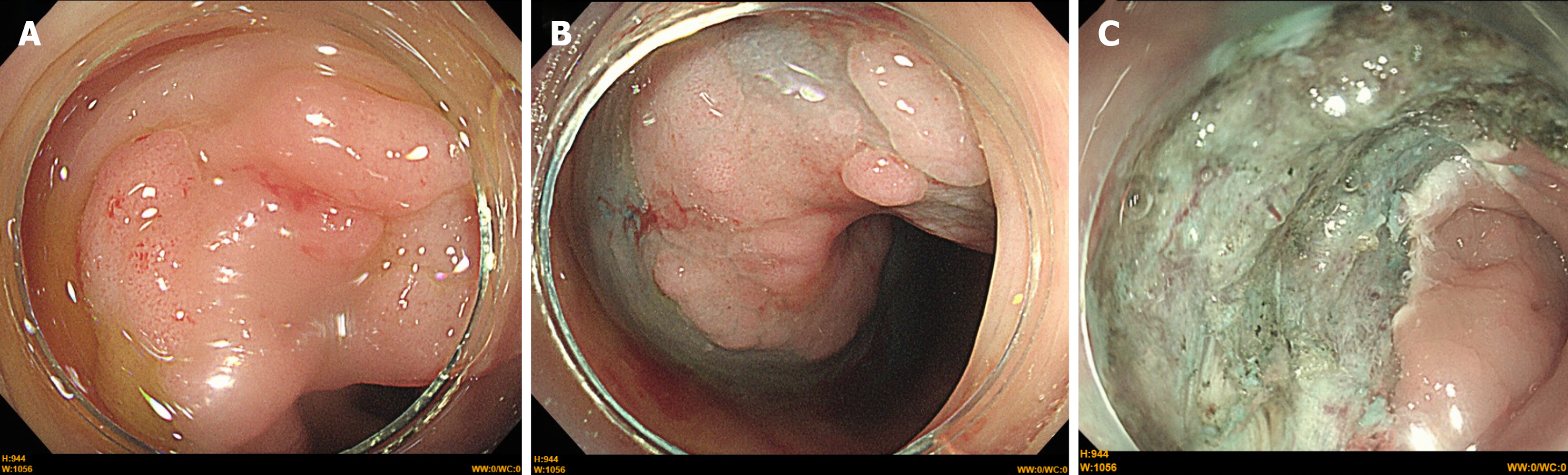
The patient underwent digestive endoscopy as part of a routine health assessment, during which a laterally spreading tumor in the sigmoid colon measuring 30 mm × 15 mm was identified and resected by ESD (Figure 1). Eighteen hours after the procedure, he experienced left lower abdominal pain and fever (39.4 °C). On the third postoperative day, he developed abdominal distension and emesis, with no bowel movement.
The patient reported no significant disorders in his past illness history.
The patient reported no significant personal or family medical history.
Abdominal examination revealed mild tenderness and rebound tenderness in the left-lower quadrant.
Routine laboratory tests demonstrated an elevated white blood cell count of 9.53 × 109/L [reference range (RR), 3.50 × 109-9.50 × 109/L] with a predominance of neutrophils (83.9%, RR, 40.0%-75.0%). Serum C-reactive protein and procalcitonin levels were 81.44 mg/L (RR, 0.00-4.00 mg/L) and 0.55 ng/mL (RR, 0.00-0.05 ng/mL), respectively.
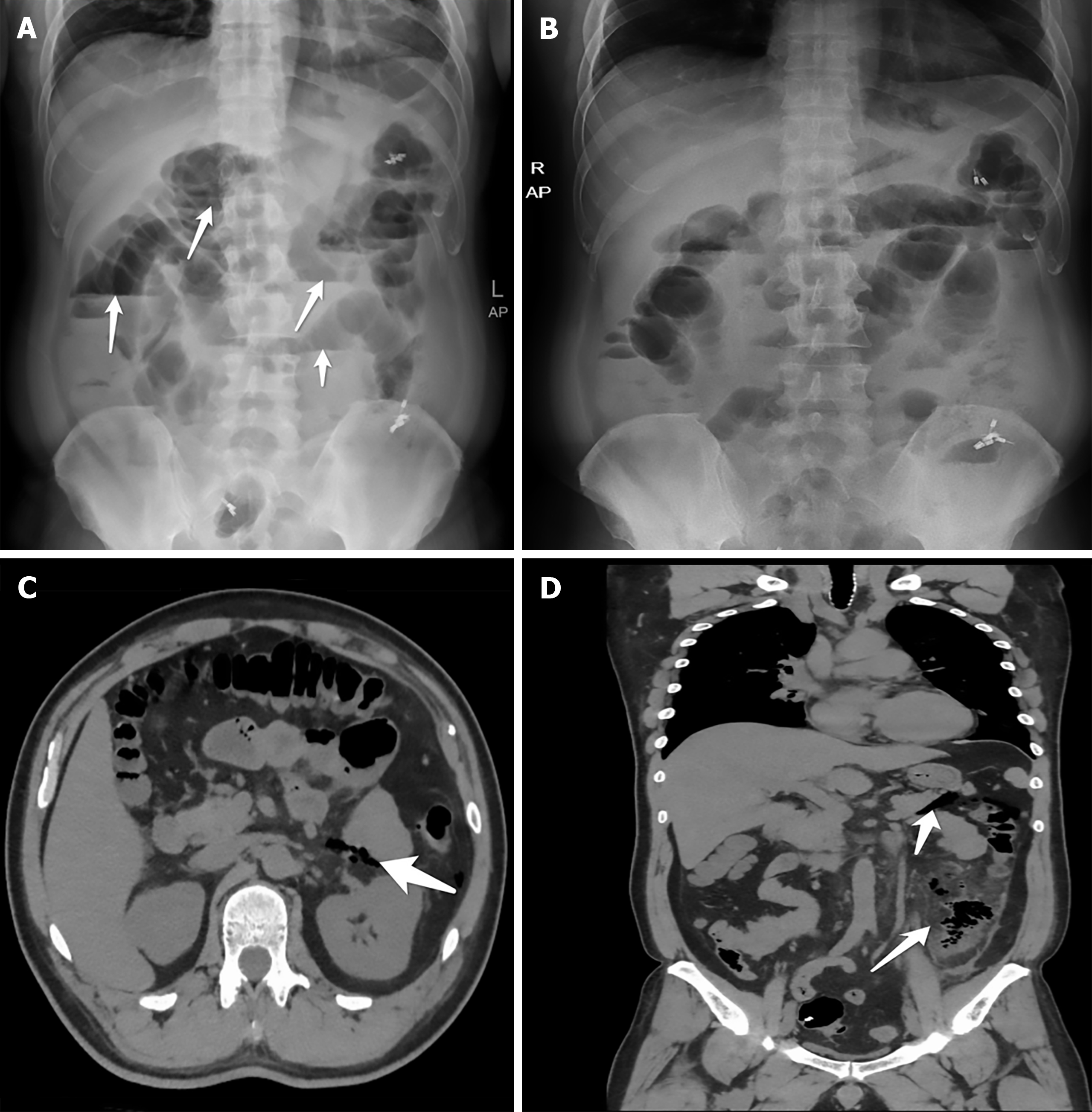
Initial plain radiography on the first postoperative day (Figure 2A) revealed air-fluid levels and dilatation of the proximal bowel. Subsequent plain radiography on second postoperative day (Figure 2B) and computed tomography (CT) on the fourth postoperative day (Figure 2C and D) were performed to further assess the dynamic changes associated with the obstruction.
The patient was diagnosed with acute obstruction following ESD.
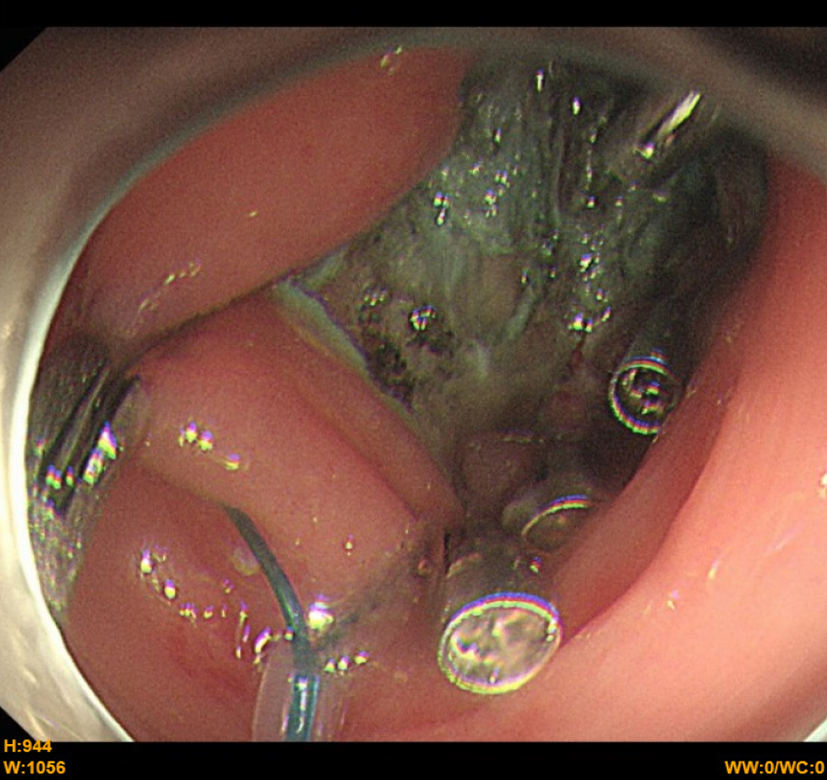
Management included fasting, maintenance of fluid and electrolyte balance, intravenous antibiotic therapy (cefo
During a three-month follow-up period, the patient remained asymptomatic, with no discomfort reported.
Intestinal obstruction is a common complication after abdominal surgery. However, it rarely occurs following gastrointestinal endoscopy. The main clinical manifestations include abdominal pain, abdominal distension, vomiting, and absence of bowel movement. Misdiagnosis can lead to delays in treatment and increased mortality. Compared with EMR, ESD has a relatively higher rate of en bloc resection, thereby reducing the local recurrence rate, particularly for lesions smaller than 2 cm[2]. However, ESD is also associated with a higher complication rate than EMR. Acute intestinal obstruction as a complication of ESD has rarely been reported. To date, only one similar case has been documented[3], indicating the rarity of this event. Comparison of the two reported cases indicates that obstruction onset occurs within 24 hours after ESD and that unnecessary surgery can often be avoided, particularly in the absence of perforation. The etiology of intestinal obstruction after ESD remains uncertain. Possible causes include: (1) Inflammatory mucosal reaction after ESD leading to marked swelling of the intestinal wall and luminal narrowing[3]; (2) Paralytic obstruction caused by sympathetic overstimulation, excessive air insufflation, or adverse reaction to sedative agent[3]; and (3) Obstruction due to fecalith formation[4]. In our patient, the obstruction was likely multifactorial. The three most probable contributing factors were: (1) Inappropriate endoscopic purse-string suture procedure, which may have triggered adhesions between opposing areas of intestinal mucosa; (2) Postoperative perforation detected by abdominal CT potentially leading to paralytic obstruction; and (3) Anatomical characteristics of the sigmoid colon. Analyzing the obstruction onset time may provide clinical insight into its underlying etiology. In this case, the onset occurred within 48 hours, and the duration was relatively short. Combined with the laboratory finds, we speculate that transient adhesion caused by inflammatory changes in the bowel mucosa was the primary mechanism. Resolution of obstruction following potent antibiotic therapy supports this etiologic consideration.
To date, no studies have confirmed the risk factors for post-ESD obstruction. We speculate that the size and depth of bowel lesions may be predictive risk factors for ESD-related complications. Timely diagnosis of complications after ESD remains challenging, as the initial manifestations are often nonspecific. CT scanning offers greater sensitivity and specificity than plain abdominal radiography for detecting ESD-related complications and plays an important role in determining their etiology. Early diagnosis of intestinal obstruction and identification of its underlying cause are essential for implementing an appropriate treatment plan, reducing the risk of disease progression, and improving prognosis. Preventive measures for post-ESD-related complications warrant greater attention. Modified ESD techniques and novel devices[5,6] may represent promising strategies for reducing complication rates of ESD in the future. In most patients with ESD-related complications, conservative management such as fasting, intravenous fluid therapy, potent antibiotics, intestinal decompression, and mucosal clip closure can help avoid surgical intervention. This case illustrates a rare but potentially serious complication after ESD, highlighting the need for clinician vigilance.
Intestinal obstruction is an extremely rare complication following ESD, and can often be effectively managed with conservative treatment.
| 1. | Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K; Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1024] [Cited by in RCA: 1431] [Article Influence: 238.5] [Reference Citation Analysis (3)] |
| 2. | Draganov PV, Aihara H, Karasik MS, Ngamruengphong S, Aadam AA, Othman MO, Sharma N, Grimm IS, Rostom A, Elmunzer BJ, Jawaid SA, Westerveld D, Perbtani YB, Hoffman BJ, Schlachterman A, Siegel A, Coman RM, Wang AY, Yang D. Endoscopic Submucosal Dissection in North America: A Large Prospective Multicenter Study. Gastroenterology. 2021;160:2317-2327.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 144] [Article Influence: 28.8] [Reference Citation Analysis (1)] |
| 3. | Park SY, Jeon SW. Acute intestinal obstruction after endoscopic submucosal dissection: report of a case. Dis Colon Rectum. 2008;51:1295-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Sun Z, Cong Y, Yu J. Evaluation of the Effects of Multiplane Reconstruction Technology with Multi-slice Spiral CT in the Etiological Diagnosis of Acute Intestinal Obstruction. Altern Ther Health Med. 2025;AT8869. [PubMed] |
| 5. | Yoshida N, Hirose R, Dohi O, Inagaki Y, Murakami T, Inada Y, Morimoto Y, Kobayashi R, Inoue K, Ghoneem E, Itoh Y. A novel reopenable clip with sharp claw for complete closure of mucosal defects after colorectal endoscopic submucosal dissection. Endoscopy. 2025;57:354-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 6. | Yamada K, Tajika M, Tanaka T, Ito N, Takagi A, Niwa Y. Modified anchor traction method allows safe colorectal endoscopic submucosal dissection: the T-shaped traction method. Endoscopy. 2025;57:E64-E65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/