Published online Sep 14, 2025. doi: 10.3748/wjg.v31.i34.110548
Revised: July 19, 2025
Accepted: August 7, 2025
Published online: September 14, 2025
Processing time: 87 Days and 0.1 Hours
Single-balloon enteroscopy (SBE) is an established procedure for evaluating small bowel lesions. While its efficacy is well recognized, the incidence of major compli
To investigate the complications and risk factors associated with diagnostic SBE.
This multicenter retrospective study included consecutive patients who under
A total of 2865 SBE procedures were performed in 1840 patients. The mean age was 51 ± 18 years, and 64.5% were male. The most common indication was ob
Acute intestinal perforation is a rare but serious complication. Prior abdominal surgery and abdominal compre
Core Tip: This large multicenter study evaluates the safety of diagnostic single-balloon enteroscopy in 2865 procedures, the largest cohort to date. While the overall major complication rate was low (0.4%), all complications were acute small bowel perforations, primarily in the ileum. Importantly, prior abdominal surgery and the use of abdominal compression significantly increased the risk of perforation. These findings reaffirm the safety profile of single-balloon enteroscopy but highlight the need for careful patient selection and technical vigilance. The study fills a critical gap by identifying key risk factors for complications in a large real-world population.
- Citation: Ullah S, Bai YQ, Wareesawetsuwan N, Cui LL, Danzhu YJ, Wang K, Zhu SS, He X, Cao XG, Guo CQ, Zhang FB. Complications of single-balloon enteroscopy: A nine-year multicenter experience of 2865 procedures. World J Gastroenterol 2025; 31(34): 110548
- URL: https://www.wjgnet.com/1007-9327/full/v31/i34/110548.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i34.110548
Single-balloon enteroscopy (SBE) has emerged as an alternative to double-balloon enteroscopy (DBE) for the evaluation of small bowel diseases[1-3]. SBE employs a single balloon attached to the overtube and is advanced through the small bowel using a push-and-pull technique involving balloon inflation and deflation. It has demonstrated diagnostic and therapeutic yields comparable to DBE, while offering a simplified technique and shorter procedural duration[3-6].
The overall complication rate for both techniques is approximately 1%[7], and systematic reviews directly comparing the two have shown no significant difference in safety profiles[8,9]. The most commonly reported major complications associated with SBE include perforation, bleeding, and pancreatitis. Perforation is believed to result from advancing the scope through areas of weakened or surgically altered small bowel anatomy; bleeding may result from traumatic mucosal injury; and pancreatitis is likely due to traumatic or ischemic injury to the pancreas during the push maneuver[10,11].
Several studies have explored complications associated with SBE[12-15]. However, all studies were single-center, lacked risk factor analysis, and none included more than 500 procedures. Data on SBE-related complications in large populations remain limited compared to DBE. Therefore, this retrospective multicenter study aimed to assess the major complication rate and its associated risk factors in the largest cohort of diagnostic SBE procedures to date.
This multicenter retrospective study was conducted at large endoscopy centers in three tertiary care hospitals in China: The First Affiliated Hospital of Zhengzhou University (914 patients), Henan Provincial People’s Hospital (856 patients), and Qinghai Provincial People’s Hospital (70 patients), between January 2016 and September 2024. Consecutive patients who underwent diagnostic SBE and provided written informed consent were enrolled. Exclusion criteria included significant comorbidities such as unstable cardiac or pulmonary disease, abnormal coagulation study (international normalized ratio > 1.5), and pregnancy.
Data on baseline characteristics, procedural details, indications, enteroscopic findings, and major complications within 30 days post-procedure were collected. All patients were followed for 30 days post-procedure through inpatient records, outpatient visits, and telephone interviews. Each participating center adhered to a standardized protocol for documenting and monitoring adverse events, ensuring consistency in complication reporting. For cases of SBE-associated major complications, clinical data including presenting symptoms, laboratory and radiologic findings, enteroscopy reports, management, length of hospital stay, and clinical outcomes were reviewed. The study was approved by the institutional review boards of all participating hospitals, approval No. 2022-KY-11 36-002.
Eight hours prior to the SBE procedure, patients were instructed to consume 3 Liters of polyethylene glycol solution for routine bowel preparation. All procedures were performed by senior endoscopists with experience of more than 50 SBE cases. Patients underwent general anesthesia, monitored by an anesthesiologist or an anesthesia nurse. The route of SBE, per oral or per anal, was selected based on the patient’s clinical presentation and imaging findings. In the absence of compelling evidence, the per oral route was preferred as the initial approach.
All procedures utilized the SIF-Q260 enteroscope (Olympus, Tokyo, Japan) with the ST-SB1 overtube (Olympus Optical Company Ltd.). Carbon dioxide insufflation was used for bowel distension[7]. Abdominal compression was applied in selected cases to improve the rate of complete enteroscopy, as previously described[16]. The procedure was terminated when a diagnosis was established, a serious complication such as uncontrolled bleeding or perforation occurred, or complete enteroscopy was achieved. In cases where complete enteroscopy could not be achieved due to factors such as residual gas, an endoscopic clip was placed to mark the site, and the procedure was repeated via the alternate route. All three endoscopy centers adhered to the same standardized protocol for performing SBE.
Diagnostic SBE was defined as a procedure primarily performed to visualize the small intestine for diagnostic purposes. It could also include additional procedures such as endoscopic clip placement for site marking and tissue biopsy[17].
Our primary outcome was SBE-associated major complications. A complication was defined as any adverse event occurring within 30 days of SBE that negatively affected the patient’s health. Major complications were defined as those requiring hospitalization for more than 10 days, endoscopic, radiological, or surgical intervention, or resulting in death[13,18]. Acute perforation was defined as the presence of gas or luminal contents outside the gastrointestinal tract, or any clearly visible perforation identified endoscopically during or shortly after the procedure[19]. Acute pancreatitis was diagnosed when at least two of the following criteria were met: Characteristic abdominal pain, serum amylase or lipase levels greater than three times the upper limit of normal, and imaging findings consistent with acute pancreatitis. Bleeding was defined as any gastrointestinal hemorrhage occurring during or after SBE that required emergency department consultation, hospitalization, or therapeutic intervention[20].
The secondary outcomes included procedural time, maximal insertion depth, complete enteroscopy rate, enteroscopic findings and diagnostic yield. Procedural time was recorded by an assisting nurse, starting from the insertion of the endoscope to its removal. Maximal insertion depth was measured according to the method described in the DBE study[21]. Complete enteroscopy was defined as reaching the ileocecal valve via the oral approach, the pylorus via the anal approach, or visualizing the entire small bowel by identifying a clip placed during the initial examination[22]. Diagnostic yield was defined as the identification of a lesion during SBE that explained the patient’s clinical presentation.
Continuous variables were presented as mean ± SD or median (interquartile range), as appropriate. Categorical variables were expressed as numbers and percentages. Differences between continuous variables were assessed using the Student’s t-test or the Mann-Whitney U test, depending on the data distribution, while categorical variables were compared using the χ2 test. Binary logistic regression was employed to identify risk factors associated with complications. All statistical analyses were performed using SPSS version 16.0. A two-tailed P value < 0.05 was considered statistically significant.
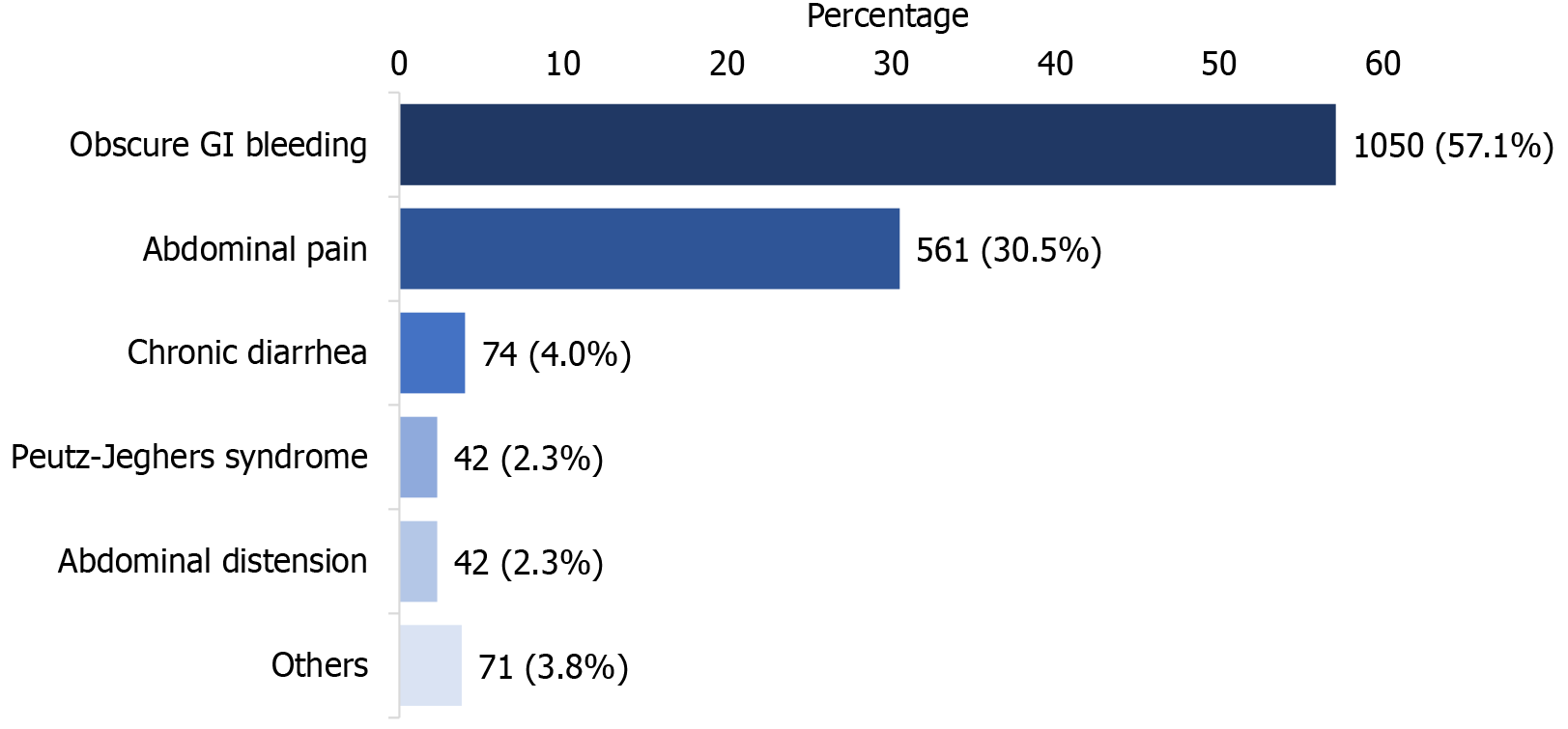
A total of 2865 diagnostic SBE procedures were performed in 1840 patients. The mean age was 51 ± 18 years, and 64.5% were male. Prior abdominal surgery was reported in 15.7% of patients. Most patients (55.7%) underwent SBE via both oral and anal routes. Median procedural times were 61 (42-80) minutes for the oral route and 60 (45-75) minutes for the anal route, with maximal insertion depths of 290 (210-340) cm and 190 (100-270) cm, respectively. Complete enteroscopy was achieved in 12.3% of cases. The most common indication was obscure gastrointestinal bleeding (57.1%), followed by abdominal pain (30.5%). Baseline characteristics and procedural parameters are summarized in Table 1, and indications for SBE are shown in Figure 1.
| Characteristic | Patients (n = 1840) |
| Male | 1187 (64.5) |
| Age (year), mean ± SD | 51 ± 18 |
| History of abdominal surgery | 288 (15.7) |
| Total SBE procedures | 2865 |
| Complete SBE | 231 (12.3) |
| Enteroscopic approach | |
| Per oral route only | 543 (29.5) |
| Per anal route only | 272 (14.8) |
| Both routes | 1025 (55.7) |
| Abdominal compression during SBE | 428 (23.3) |
| Procedural time, minutes, median (IQR) | |
| Per oral route | 61 (42-80) |
| Per anal route | 60 (45-75) |
| Maximal insertion depth (cm), median (IQR) | |
| Per oral route | 290 (210-340) |
| Per anal route | 190 (100-270) |
Pathologic lesions were identified in 1364 patients (74.1%). The positive findings included ulcers (18.0%), diverticula (15.1%), vascular malformations (14.7%), strictures (12.0%), erosions (4.3%), polyps (6.6%), adenocarcinoma (4.5%), gastrointestinal stromal tumors (3.0%), lymphoma (1.3%), Crohn’s disease (1.4%), and other lesions (2.7%), as shown in Table 2. The diagnostic yield was 74.1%, equivalent to the positive findings rate. A total of 476 patients (25.9%) had no identifiable lesions despite undergoing bidirectional SBE.
| Characteristic | n (%) |
| Positive findings | 1364 (74.1) |
| Ulcer | 332 (18.0) |
| Diverticulum | 277 (15.1) |
| Vascular malformation | 270 (14.7) |
| Stricture | 220 (12.0)1 |
| Malignant stricture | 41 (2.2) |
| Benign stricture | 179 (9.7) |
| Erosion | 80 (4.3) |
| Polyp | 122 (6.6) |
| Adenocarcinoma | 83 (4.5) |
| GIST | 56 (3.0) |
| Lymphoma | 23 (1.3) |
| Crohn’s disease | 26 (1.4) |
| Other findings | 50 (2.7) |
| Negative findings | 476 (25.9) |
| Diagnostic yield | 1364 (74.1) |
| Major complication | 7 (0.0) |
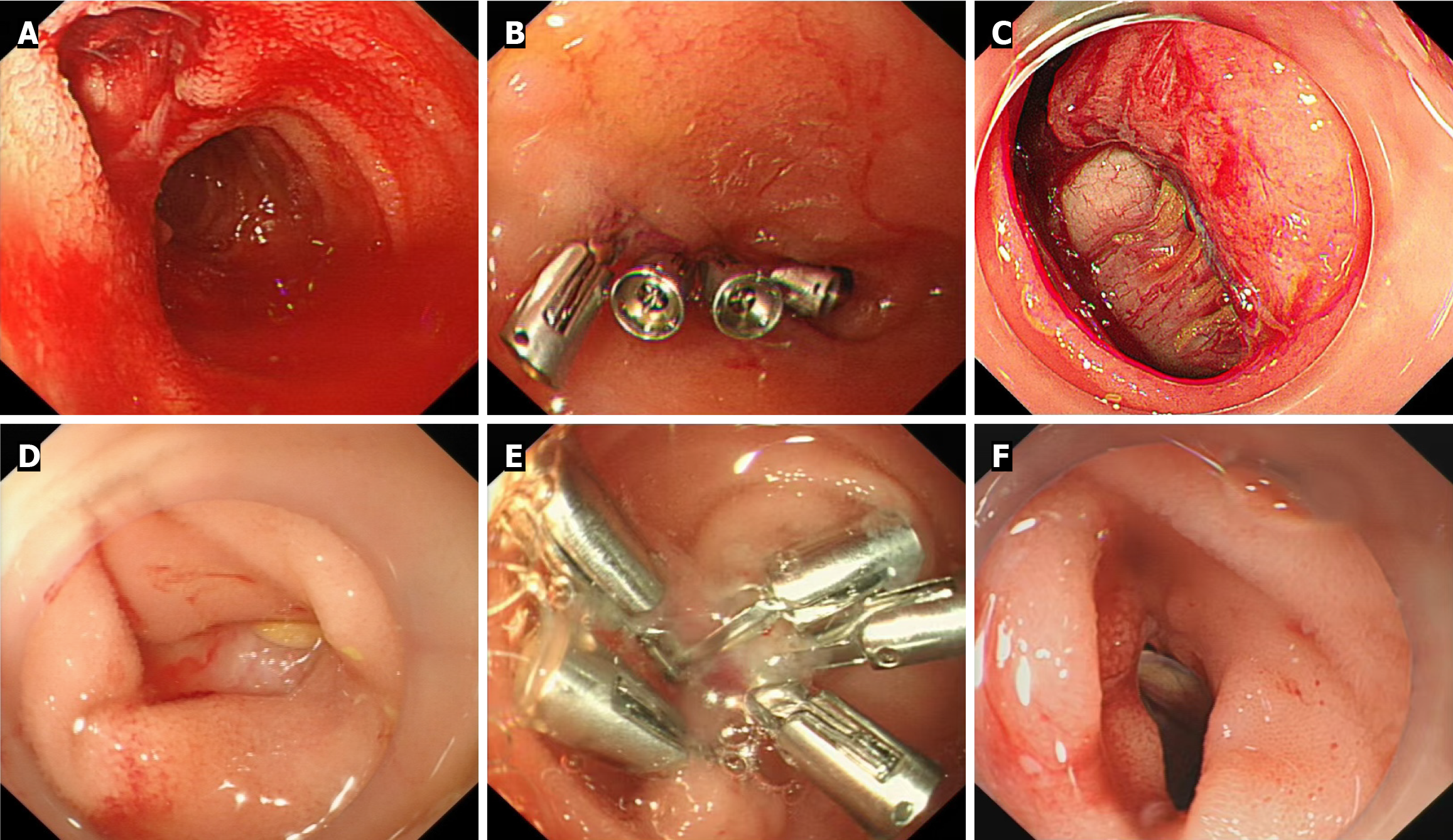
Among the 1840 patients who underwent diagnostic SBE, seven patients met the criteria for major complications, resulting in a major complication rate of 0.4%. All major complications involved acute intestinal perforation, diagnosed endoscopically during the procedure by visualization of intraperitoneal organs. The median time-to-event was estimated at 17 minutes (10-30 minutes) after the start of the procedure. In six of the seven cases, perforation occurred during scope advancement through the distal ileum in the setting of increased resistance or difficult angulation. In one case, perforation occurred during passage through an unrecognized stenotic segment in duodenum. Review of the procedural notes indicated that these cases frequently involved technical difficulty, such as resistance during advancement, challenging scope manipulation, or multiple loops reduction. Maximal insertion depth ranged from 15 cm to 100 cm and was relatively short due to early termination following perforation.
Six perforations occurred in the ileum and one in the duodenum. Through-the-scope clip (TTSC) placement was attempted in four cases with small perforations but was unsuccessful, as all patients developed abdominal pain, fever, or signs of peritonitis within 24 hours and subsequently underwent surgery. The remaining three patients with large perforations proceeded directly to surgical repair. No cases of acute pancreatitis or bleeding were reported.
All patients recovered without further complications. Six of the seven patients had abdominal adhesions, correlating with a history of prior abdominal surgery. Among them, two were diagnosed with small bowel lymphoma during surgery. The remaining patient, who had neither abdominal adhesions nor a history of prior surgery, was found to have small bowel stenosis intraoperatively during surgical repair. Details of the perforation cases are summarized in Table 3 and illustrated in Figure 2.
| No. | Age/sex | Previous abdominal Sx | Indication | SBE procedure | Perforation | Management | HS (day) | Outcome | Definite diagnosis |
| 1 | 73/female | None | Abdominal pain | Approach: Oral | Presentation: Perforation during SBE2 | Surgery | 17 | Recovery | Duodenal stenosis, etiology unknown |
| Sedation: General anesthesia | Site of perforation: Duodenum | ||||||||
| Abdominal compression: Yes | |||||||||
| Time: 10 minutes | Size: 5 cm × 5 cm | ||||||||
| Finding1: Normal | |||||||||
| 2 | 58/female | Caesarean section | Abdominal pain | Approach: Anal | Presentation: Perforation during SBE2 | An endoscopic clip was attempted. 24 hours later, the patient developed fever and signs of peritonitis. Surgery was performed, and the clip was found to have inadequately closed the perforation | 11 | Recovery | Abdominal adhesion |
| Time: 14 minutes | Site of perforation: Ileum | ||||||||
| Sedation: General anesthesia | |||||||||
| Abdominal compression: Yes | Size: 1 cm × 3 cm | ||||||||
| Finding1: Normal | |||||||||
| 3 | 67/female | Abdominal exploration and appendectomy | Abdominal pain | Approach: Anal | Presentation: Perforation during SBE2 | Surgery | 12 | Recovery | Small bowel lymphoma and abdominal adhesion |
| Time: 7 minutes | |||||||||
| Sedation: General anesthesia | |||||||||
| Abdominal compression: Yes | Site of perforation: Ileum | ||||||||
| Finding1: Normal | Size: 1 cm × 2 cm | ||||||||
| 4 | 20/male | Abdominal exploration and appendectomy | Abdominal pain | Approach: Anal | Presentation: Perforation during SBE2 | An endoscopic clip was placed immediately after perforation. During postoperative observation, the patient had persistent abdominal pain, and imaging revealed intraperitoneal free air. Surgery was performed 24 hours later | 19 | Recovery | Abdominal adhesion |
| Time: 30 minutes | Site of perforation: Ileum | ||||||||
| Sedation: General anesthesia | Size: 1 cm × 1 cm | ||||||||
| Abdominal compression: Yes | |||||||||
| Finding1: Normal | |||||||||
| 5 | 53/male | Abdominal exploration and appendectomy | Abdominal pain | Approach: Anal | Presentation: Perforation during SBE2 | An endoscopic clip was applied at the perforation site, but closure was unsuccessful. The patient developed severe abdominal pain and subsequently underwent surgery 24 hours later | 14 | Recovery | Abdominal adhesion |
| Time: 17 minutes | Site of perforation: Ileum | ||||||||
| Sedation: General anesthesia | Size: 1 cm × 1 cm | ||||||||
| Abdominal compression: Yes | |||||||||
| Finding1: Normal | |||||||||
| 6 | 55/male | Abdominal exploration and appendectomy | Abdominal pain | Approach: Anal | Presentation: Perforation during SBE2 | Surgery | 13 | Recovery | Small bowel lymphoma and abdominal adhesion |
| Time: 28 minutes | Site of perforation: Ileum | ||||||||
| Sedation: General anesthesia | Size: 3 cm × 3 cm | ||||||||
| Abdominal compression: Yes | |||||||||
| Finding1: Normal | |||||||||
| 7 | 24/male | Partial small-bowel resection | OGIB | Approach: Anal | Presentation: Perforation during SBE2 | An endoscopic clip was applied after perforation during SBE. 24 hours later, the patient developed generalized abdominal pain and high-grade fever. Surgery was performed, and intraoperative findings confirmed perforation; the clip had failed to close it | 24 | Recovery | Abdominal adhesion |
| Time: 34 minutes | Site of perforation: Ileum | ||||||||
| Sedation: General anesthesia | Size: 0.5 cm × 1.5 cm | ||||||||
| Abdominal compression: Yes | |||||||||
| Finding1: Normal |
Prior abdominal surgery (6/7) and abdominal compression (7/7) were significantly associated with perforation (P < 0.001 for both). Patients with a history of abdominal surgery had a significantly increased risk of perforation, with an odds ratio of 33.00 (95% confidence interval: 3.96-275.15, P = 0.001). In a subgroup analysis, the perforation rate in patients with prior abdominal surgery was 2.1% (6/288). For cases where abdominal compression was used, the perforation rate was 1.6% (7/428). Age and sex were comparable between the perforation and non-perforation groups. There was no association between perforation and completion of SBE. Maximal insertion depth and procedural time were not assessed as risk factors, as all perforations occurred during the procedure, resulting in prematurely terminated procedures and shorter times.
This multicenter retrospective study includes the largest cohort to date evaluating major complications associated with diagnostic SBE over a nine-year period. The overall major complication rate was 0.4%, with all cases involving acute small bowel perforation during the procedure. A history of abdominal surgery and the use of abdominal compression were both significantly associated with an increased risk of perforation.
Given the low complication rate observed, SBE is considered a safe procedure for small bowel examination. Our finding of an overall major complication rate of 0.4% is consistent with previous studies. Aktas et al[13] reported no major complications among 145 patients who underwent diagnostic SBE. Other studies that included both diagnostic and therapeutic SBE reported complication rates ranging from 0% to 3.1%[2,6,9,12,14,15], with small bowel perforation being the most commonly reported serious adverse event.
In the seven cases of acute small bowel perforation in our study, the underlying mechanisms likely involved a combination of contributing factors.
First, direct trauma from the hook-shaped tip of the enteroscope may occur during attempts to fixate the small bowel segment prior to overtube advancement, as suggested by Aktas et al[13]. This differs from the DBE system, which uses an inflated balloon for fixation and may exert less focal pressure on the bowel wall[23].
Second, the small bowel wall is relatively thinner than that of the large bowel, with the ileum being the narrowest and most fragile segment. This anatomical vulnerability supports our finding that six of the seven perforation cases occurred in the ileum during anal-route SBE. In addition, preexisting small bowel pathology, such as ulcerated or friable lesions, may further compromise the integrity of the bowel wall. Two patients in our study were diagnosed with small bowel lymphoma, a condition associated with spontaneous perforation in 9% of biopsy-proven cases, 59% of which occur in the small intestine[24]. Tominaga et al[25] similarly reported a case of perforation following oral-route SBE in a patient with metastatic carcinoma of unknown origin, in which tumor infiltration was suspected to have weakened the bowel wall. Although abdominal computed tomography may be useful for screening patients at higher risk of perforation, in our two lymphoma cases, pre-procedure computed tomography scans showed no significant abnormalities in the bowel wall.
Third, adhesions from previous abdominal surgery can limit bowel mobility and flexibility, making it more susceptible to perforation during scope advancement or withdrawal, especially when force is applied. In our study, the perforation rate among patients with a history of abdominal surgery was 2.1%, compared to the overall rate of 0.4%. Gerson et al[17] identified adhesions as a risk factor for perforation in DBE, reporting a rate of 3% in patients with prior abdominal surgery, compared to 0.4% overall. Most of these cases occurred during the anal approach, which is consistent with our observations.
Fourth, the use of abdominal compression during SBE may elevate intra-abdominal pressure externally, thereby increasing the risk of perforation. In a randomized controlled trial[16], perforation occurred in two of 102 patients who were randomized to the abdominal compression group, both of whom had a history of abdominal surgery. Our findings support this association, particularly when abdominal compression is used in combination with prior surgery. Additionally, in our study, one patient with a duodenal perforation, unlike the others who had ileal perforations, had underlying duodenal stenosis. This condition likely contributed to internal pressure buildup in the duodenum, making it vulnerable to perforation. In such cases, careful loop reduction and gentle advancement are recommended rather than increasing abdominal pressure.
In our study, all seven cases of acute intestinal perforation were identified immediately during the procedure and ultimately required surgical intervention. TTSC were initially applied in four cases with smaller perforations. However, all attempts failed, and the patients underwent surgery within 24 hours. This contrasts with the high success rate of TTSC reported for iatrogenic colonic perforations, which is approximately 90%[26]. The low success rate in our series may be attributed to several contributing factors. The small bowel lumen is narrower than that of the colon, making endoscopic access and clip deployment more difficult. In addition, the enteroscope used in SBE is longer than standard colonoscope, which increases procedural complexity and limits scope control. Active peristalsis of the small intestine may also promote clip dislodgement. Furthermore, the size of the perforations in our study was relatively large, ranging from 1 cm to 3 cm, which may have exceeded the effective closure capacity of TTSC devices. However, newer techniques with higher success rates for larger perforations, such as over-the-scope clips or endoscopic suturing, were not attempted due to unavailability at the time.
The clinical implication of our study is that, while caution is necessary in all SBE procedures, particular attention should be given to patients with known risk factors, such as a history of abdominal surgery. These patients require especially careful technique during the procedure. When endoscopists encounter significant resistance during scope advancement, the use of fluoroscopic guidance or early termination of the procedure should be considered, as perforation is a serious complication. In addition, abdominal compression should be avoided in high-risk patients to reduce the likelihood of perforation.
This study is limited by its retrospective design, lack of long-term follow-up, and potential inter-operator variability, although complications were not confined to a single center. No data on long-term adverse events or outcomes were available due to the limited follow-up period. Additionally, we did not adjust for confounding factors in the logistic regression due to the small number of complication cases. A large prospective study is warranted to validate these findings and provide more robust evidence, and further research focusing on optimizing strategies to reduce complications in high-risk patients is also needed.
In conclusion, this multicenter study presents the largest cohort of patients undergoing diagnostic SBE and demonstrates that acute intestinal perforation is a rare major complication, occurring in 0.4% of cases. Prior abdominal surgery and abdominal compression were significant risk factors. Nonetheless, diagnostic SBE remains a safe and effective technique for small bowel evaluation. However, patients with a history of abdominal surgery should undergo SBE with great caution and avoid the use of abdominal compression. For patients in whom abdominal compression is considered to improve the completion rate, the risk of perforation must be carefully weighed. Careful patient selection is recommended to minimize the risk of complications.
| 1. | Goenka MK, Afzalpurkar S, Rai VK, Agarwal R, Shah BB, Rodge GA, Raj B, Goenka U. Single-balloon enteroscopy in management of small-bowel disorders. Indian J Gastroenterol. 2020;39:550-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Kou GJ, Liu C, Yu YB, Li YQ, Zuo XL. Single-operator single-balloon enteroscopy is safe and effective: A 6-year retrospective study. J Dig Dis. 2024;25:353-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Garg R, Singh A, Mohammed A, Aggarwal M, Stevens T, Vargo J, Jang S. Efficacy and safety of double- versus single-balloon retrograde enteroscopy. Eur J Gastroenterol Hepatol. 2023;35:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 4. | Pinto-Pais T, Pinho R, Rodrigues A, Fernandes C, Ribeiro I, Fraga J, Carvalho J. Emergency single-balloon enteroscopy in overt obscure gastrointestinal bleeding: Efficacy and safety. United European Gastroenterol J. 2014;2:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Lipka S, Rabbanifard R, Kumar A, Brady P. Single versus double balloon enteroscopy for small bowel diagnostics: a systematic review and meta-analysis. J Clin Gastroenterol. 2015;49:177-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Koh JTE, Kim Wei L, Francisco CP, Ravi R, Chan W, Khor C, Asokkumar R. Double balloon enteroscopy versus single balloon enteroscopy: A comparative study. Medicine (Baltimore). 2024;103:e38119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Rondonotti E, Spada C, Adler S, May A, Despott EJ, Koulaouzidis A, Panter S, Domagk D, Fernandez-Urien I, Rahmi G, Riccioni ME, van Hooft JE, Hassan C, Pennazio M. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) Technical Review. Endoscopy. 2018;50:423-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 304] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 8. | Wadhwa V, Sethi S, Tewani S, Garg SK, Pleskow DK, Chuttani R, Berzin TM, Sethi N, Sawhney MS. A meta-analysis on efficacy and safety: single-balloon vs. double-balloon enteroscopy. Gastroenterol Rep (Oxf). 2015;3:148-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Kim TJ, Kim ER, Chang DK, Kim YH, Hong SN. Comparison of the Efficacy and Safety of Single- versus Double-Balloon Enteroscopy Performed by Endoscopist Experts in Single-Balloon Enteroscopy: A Single-Center Experience and Meta-Analysis. Gut Liver. 2017;11:520-527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Chavalitdhamrong D, Adler DG, Draganov PV. Complications of enteroscopy: how to avoid them and manage them when they arise. Gastrointest Endosc Clin N Am. 2015;25:83-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Moeschler O, Mueller MK. Deep enteroscopy - indications, diagnostic yield and complications. World J Gastroenterol. 2015;21:1385-1393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Lin MC, Chen PJ, Shih YL, Huang HH, Chang WK, Hsieh TY, Huang TY. Outcome and Safety of Anterograde and Retrograde Single-Balloon Enteroscopy: Clinical Experience at a Tertiary Medical Center in Taiwan. PLoS One. 2016;11:e0161188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Aktas H, de Ridder L, Haringsma J, Kuipers EJ, Mensink PB. Complications of single-balloon enteroscopy: a prospective evaluation of 166 procedures. Endoscopy. 2010;42:365-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Davis-Yadley AH, Lipka S, Rodriguez AC, Nelson KK, Doraiswamy V, Rabbanifard R, Kumar A, Brady PG. The safety and efficacy of single balloon enteroscopy in the elderly. Therap Adv Gastroenterol. 2016;9:169-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Manno M, Barbera C, Dabizzi E, Mussetto A, Conigliaro R. Safety of single-balloon enteroscopy: our experience of 72 procedures. Endoscopy. 2010;42:773; author reply 774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Zhang FB, Zhang JP, Bai YQ, Zhang DJ, Cao XG, Guo CQ. Effect of Abdominal Compression on Total Single-Balloon Enteroscopy Rate: A Randomized Controlled Trial. Mayo Clin Proc. 2023;98:1660-1669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Gerson LB, Tokar J, Chiorean M, Lo S, Decker GA, Cave D, Bouhaidar D, Mishkin D, Dye C, Haluszka O, Leighton JA, Zfass A, Semrad C. Complications associated with double balloon enteroscopy at nine US centers. Clin Gastroenterol Hepatol. 2009;7:1177-1182, 1182.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (1)] |
| 18. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2084] [Article Influence: 59.5] [Reference Citation Analysis (2)] |
| 19. | Farhat S, Chaussade S, Ponchon T, Coumaros D, Charachon A, Barrioz T, Koch S, Houcke P, Cellier C, Heresbach D, Lepilliez V, Napoleon B, Bauret P, Coron E, Le Rhun M, Bichard P, Vaillant E, Calazel A, Bensoussan E, Bellon S, Mangialavori L, Robin F, Prat F; SFED ESD study group. Endoscopic submucosal dissection in a European setting. A multi-institutional report of a technique in development. Endoscopy. 2011;43:664-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 20. | Rodríguez de Santiago E, Sánchez Aldehuelo R, Riu Pons F, Rodríguez Escaja C, Fernández-Esparrach G, Cañete-Ruiz Á, Ferre Aracil C, Pérez-Corte D, Ríos León R, Marcos-Prieto HM, Delgado-Guillena PG, García-Rodríguez A, Guarner-Argente C, Muriel A, de la Fuente-Briongos E, García García de Paredes A, Parejo-Carbonell S, Téllez L, Senosiaín-Lalastra C, Burgos-Santamaría D, Aicart-Ramos M, Mateos Muñoz B, Peñas-García B, Pagano G, Casals Urquiza G, Urpi Ferreruela M, Ángel de Jorge-Turrión M, Barreiro-Alonso E, Fraile-López M, Gómez-Outomuro A, Altamirano MI, Núñez Esteban M, Ruiz-Andreu M, Arribas-Anta J, de Frutos D, Herreros-de-Tejada A, Arias-Rivera ML, Roldán-Fernández M, Marcos Martín ÁF, Zamora J, Vázquez-Sequeiros E, Albillos A; ENDOHEM research group of the Spanish Society of Gastrointestinal Endoscopy (SEED) and the Spanish Gastroenterology Association (AEG). Endoscopy-Related Bleeding and Thromboembolic Events in Patients on Direct Oral Anticoagulants or Vitamin K Antagonists. Clin Gastroenterol Hepatol. 2022;20:e380-e397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | May A, Nachbar L, Ell C. Double-balloon enteroscopy (push-and-pull enteroscopy) of the small bowel: feasibility and diagnostic and therapeutic yield in patients with suspected small bowel disease. Gastrointest Endosc. 2005;62:62-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 259] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 22. | Li X, Zhao YJ, Dai J, Li XB, Xue HB, Zhang Y, Xiong GS, Ohtsuka K, Gao YJ, Liu Q, Song Y, Fang JY, Ge ZZ. Carbon dioxide insufflation improves the intubation depth and total enteroscopy rate in single-balloon enteroscopy: a randomised, controlled, double-blind trial. Gut. 2014;63:1560-1565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Riccioni ME, Urgesi R, Cianci R, Spada C, Nista EC, Costamagna G. Single-balloon push-and-pull enteroscopy system: does it work? A single-center, 3-year experience. Surg Endosc. 2011;25:3050-3056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Vaidya R, Habermann TM, Donohue JH, Ristow KM, Maurer MJ, Macon WR, Colgan JP, Inwards DJ, Ansell SM, Porrata LF, Micallef IN, Johnston PB, Markovic SN, Thompson CA, Nowakowski GS, Witzig TE. Bowel perforation in intestinal lymphoma: incidence and clinical features. Ann Oncol. 2013;24:2439-2443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 25. | Tominaga K, Iida T, Nakamura Y, Nagao J, Yokouchi Y, Maetani I. Small intestinal perforation of endoscopically unrecognized lesions during peroral single-balloon enteroscopy. Endoscopy. 2008;40 Suppl 2:E213-E214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Verlaan T, Voermans RP, van Berge Henegouwen MI, Bemelman WA, Fockens P. Endoscopic closure of acute perforations of the GI tract: a systematic review of the literature. Gastrointest Endosc. 2015;82:618-28.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/