Published online Feb 21, 2024. doi: 10.3748/wjg.v30.i7.624
Peer-review started: November 3, 2023
First decision: December 14, 2023
Revised: December 21, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 21, 2024
Processing time: 109 Days and 22 Hours
Colonoscopy is an integral part of the lower bowel care and is generally consider
Core Tip: Although colonoscopy is seen as a potentially safe procedure performed as a daycare practice, yet it is associated with a wide range of complications. Emerging evidence in the literature documents injuries to abdominal organs beyond the bowel wall. The most commonly affected organ is the spleen, followed by the pancreas and infrequently the liver, mesentery and urinary bladder. Despite its low frequency, some cases are serious especially the rupture of visceral organs like spleen. In such cases, conservative management may not always work and interventional radiologic procedures and/or surgery may be required.
- Citation: Emara MH, Mazid U, Elshaer YA, Elkerdawy MA, Malik DF, Mahros AM. Trauma to the solid abdominal organs: The missed dark box of colonoscopy. World J Gastroenterol 2024; 30(7): 624-630
- URL: https://www.wjgnet.com/1007-9327/full/v30/i7/624.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i7.624
Colonoscopy is potentially a safe diagnostic and therapeutic procedure performed daily as an outpatient care service. Colonoscopy refers to the examination of colon and terminal ileum using flexible colonoscopes. The introduction of colonoscopy was a paradigm shift in the diagnosis and treatment of lower gastrointestinal (GI) diseases. It is indicated for evaluation of lower GI symptoms including chronic diarrhea, constipation, bleeding per rectum, tenesmus and abdominal pain among others. It is also an integral part of monitoring activity and response to treatment in inflammatory bowel diseases (IBD), follow up of patients with diverticular disease and mucosal tissue acquisition for different purposes. Furthermore, it is now a cornerstone not only in screening but also in the treatment of early stages of colorectal cancer (CRC). In fact, with the advancements achieved in colonoscopy, CRC is now classified as a preventable disease through screening of the high-risk group of the patients and application of different therapeutic interventions. The therapeutic potential extends from simple hot and cold snare polypectomy to advanced endoscopic mucosal resection, and endoscopic submucosal dissection for superficial bowel neoplasia and stenting for both benign and malignant lesions[1-3].
The operator should maintain an acceptable level of competency to clearly identify the indications for the procedure, technical ease with avoidance of looping and excessive force application while advancing the scope, and high experience in handling high risk patients. In addition, early identification and treatment of procedure related complications is very crucial[2].
The common adverse events related to this procedure vary and include abdominal pain, distension, perforation, bleeding, and adverse events related to the bowel preparation solutions used to clean the colon before the endoscopic examination. Furthermore, adverse events due to the used sedation medications have been described also[3].
Severe acute abdominal pain occurring post-colonoscopy usually directs the attention towards bowel perforation, however, extra-luminal adverse events related to colonoscopy presenting with acute abdominal pain are associated with a wide range of manifestations, and are increasingly reported in the literature[3-6].
Post-colonoscopy abdominal pain is a common manifestation, usually benign, and mostly related to the gaseous distension and tractions induced by the procedure[5,6]. However, continuous and steadily increasing pain should alarm the endoscopists and clinicians to the development of complications. Furthermore, development of symptoms not related to the procedure, e.g., nausea, vomiting, marked and progressive abdominal distension, hypotension and hemodynamic instability should raise the possibility of serious complications especially post-procedural perforation, bleeding and injury to other organs. The overall rate of colonoscopy related serious complications is 2.8/1000 procedure[3] and mortality is estimated to be 0.23 to 0.91 per 10000 among FIT-positive and negative participants undergoing screening colonoscopy in a recently published Dutch study respectively[7].
Injury to organs beyond the colonic wall induced by colonoscopy is uncommon. These injuries are sometimes serious and life-threatening, and that is why a high index of suspicion should be raised upon evaluating patients’ post-procedural state. There are no accurate estimates to overall organ injuries induced by colonoscopy, however, many reports are evolving in the literature figuring out these injuries. The first report for organ injury by colonoscopy was reported as early as mid-1970s[8], and thereafter many case reports of different organ injuries were published.
We analyzed many articles across the literature through search of the major databases including PubMed, Embase, and Cochrane. The retrieved articles are mainly case reports, case series and reviews while the observational studies were infrequently found.
Although splenic injury after colonoscopy is a rare complication, yet spleen is the most frequently injured abdominal organ during colonoscopy. There is no accurate estimate for the incidence of post colonoscopy splenic injury. However, a study from a single institution focusing on all colonoscopies done between 1980 and 2008 reported the incidence of splenic injury to be 0.2 per 10000 procedures[9]. Another study documented a rate of 0.72 per 10000 procedures[10]. An intermediate incidence was recently figured out by Laanani et al[11], with figures of 0.20-0.34 per 10000 procedures.
It was first documented by Wherry and Zehner[12], and is a serious complication that can lead to life threatening conditions. Catastrophic complete splenic rupture was reported among 22% of cases, while the majority of cases (63%) experienced other types of splenic injuries such as, spleen laceration, sub-capsular hematoma, and spleen avulsion[13].
Diagnosis of splenic injury may be challenging as post-colonoscopy abdominal discomfort and pain is common and mostly due to trapped air in colon. However, in splenic injury, symptoms develop within 24 h most commonly as persistent abdominal pain without radiographic evidence of perforation, peritoneal irritation, and a drop in hematocrit and hemodynamic instability, depending on the severity of the injury. Contrast enhanced computed tomography (CT) scan is the gold standard method for diagnosis of splenic injuries because it can detect the presence of haemoperitoneum, describe the extent of injury and exclude other organ injuries[14].
Treatment varies according to the type and severity of splenic injury and the associated hemodynamic instability, if any. In hemodynamically stable patients with closed sub-capsular hematoma and no intra-peritoneal blood conservative treatment should be tried. This includes close monitoring, intravenous fluids, bed rest, serial hemoglobin and hematocrit monitoring, and serial imaging. In hemodynamically unstable patients with active bleeding and associated peritonitis, selective splenic artery embolization is an option, however, splenectomy is usually the definitive management[14,15].
Regarding liver, the first report of liver injury following colonoscopy was reported as early as 1979 by Ellis et al[16], who reported combined liver, splenic, and mesenteric injury in a 33-year-old lady with active IBD. Combined hepatic and splenic lacerations due to rupture of tight vascular adhesions between transverse colon and both the spleen and liver was reported 8 years later by Levine et al[17]. Combined hepatic and splenic injuries during colonoscopy are rather common than isolated hepatic injury that is extremely rare. Noreña et al[18], reported a large subcapsular hepatic hematoma, right lobe laceration and hemoperitoneum 4 d after a routine colonoscopy. One more, lone hepatic injury was reported by Jammal et al[19], who described a subcapsular hepatic hematoma 6 h after colonoscopy.
In these cases (Table 1), most patients experienced persistent right side abdominal pain, peritoneal irritation, drop in hematocrit and hemodynamic instability, depending on the degree of hepatic injury. Although abdominal ultrasound has been used to diagnose large sized hepatic hematoma, yet contrast CT scan is the gold standard method for confirming diagnosis, assessing extent, and diagnosing associated other organ injuries. Management options for hepatic injury depend on hemodynamic stability and extent of injury including conservative approach, percutaneous drainage, angiographic embolization, or exploratory laparotomy[17-21].
| Ref. | Type of injury | Age, sex, and risk factors | Presentation | Treatment | Comments |
| Ellis et al[16], 1979 | Combined liver and spleen | 33-year-old female, her manifestations and colonoscopy findings were suggestive of IBD | Left upper quadrant followed by hemodynamic instability | Surgical | The spleen ruptured, laceration to left liver lobe, injury to mesocolon. Ruptured? IBD related adhesions were seen |
| Noreña et al[18], 2013 | Lone liver injury | 73-year-old male, undergoing a screening colonoscopy | Severe right upper abdominal pain radiating to lumbar region with abdominal distension and rigidity | Laparoscopic evaluation and drainage were done with conservative management | A subcapsular hepatic hematoma and a right hepatic; lobe laceration as well as a large hemoperitoneum |
| Jammal et al[19], 2013 | Lone liver injury | 30-year-old woman undergoing screening colonoscopy for polyps | Right upper quadrant pain radiating to the right scapula | Conservative | Abdominal ultrasonography and CT achieved diagnosis of a subcapsular hematoma |
| Hussain et al[20], 2020 | Combined liver and spleen | A 71-year-old woman with many medical co-morbidities had an EGD; and colonoscopy for nonspecific abdominal pain | Brought to emergency room in code blue hours after having colonoscopy | Emergency laparotomy with splenectomy and hepatorrhaphy | Adhesion of omentum to bilateral abdominal wall and pelvis. The patient passed away dye to brain hypoxic events |
Regarding pancreas, there are no accurate estimates for pancreatic injuries induced by colonoscopy. However, the frequency of pancreatic injury following colonoscopy seems low. The literature presents many published cases (Table 2), figuring out this serious complication. Probably the first reported pancreatic injury in relation to colonoscopy reported in English literature was described by Thomas and Mitre[22]. Thereafter, many cases were reported. The reported pancreas related adverse events comprised acute pancreatitis (AP)[5,6,23], pancreatitis with hemorrhage related to tail of pancreas[21] and pancreatic duct leak with development of colo-pancreatic fistula[22]. Diagnosis should be suspected with the development of the symptoms after colonoscopy usually by 2-6 h and these include epigastric pain, nausea, vomiting, haemodynamic instability associated with pancreatic enzymes’ elevation[24]. However, the presentation may be delayed to many hours.
| Ref. | Type of injury | Age, sex, and risk factors | Presentations | Treatment | Comments |
| Sidiqi and Gong[5], 2019 | Acute pancreatitis | 53-yr-old female | Epigastric pain with nausea and vomiting | Conservative | Probably direct trauma to tail of the pancreas by movement of the endoscope |
| Limb et al[6], 2016 | Acute pancreatitis | 69-yr-old female, multiple abdominal surgeries, and previous episode of acute pancreatitis | Epigastric pain | Conservative | Crohn’s disease; controlled under mesalazine therapy |
| Thomas and Mitre[22], 1994 | Acute pancreatitis | A 25-yr-old male, technical difficulties with passage of the scope beyond the splenic flexure after manipulations, position change and external abdominal pressure | Mid-epigastric pain with nausea and vomiting | Conservative | Alpha loop formation. The pancreatic inflammation was limited to the tail (close proximity to splenic flexure) |
| Khashram and Frizelle[24], 2011 | Hemorrhage around tail of pancreas | Trauma of insufflation transmitted to the pancreas | Epigastric pain | Conservative | |
| Ahmed et al[32], 2019 | Pancreatic duct leak | 62-yr-old female, prior left nephrectomy | Worsening left sided abdominal pain, nausea and vomiting | ERCP with PD stenting | A collection involving pancreatic tail and splenic flexure (possible following adhesions of the prior surgery) was seen in the CT |
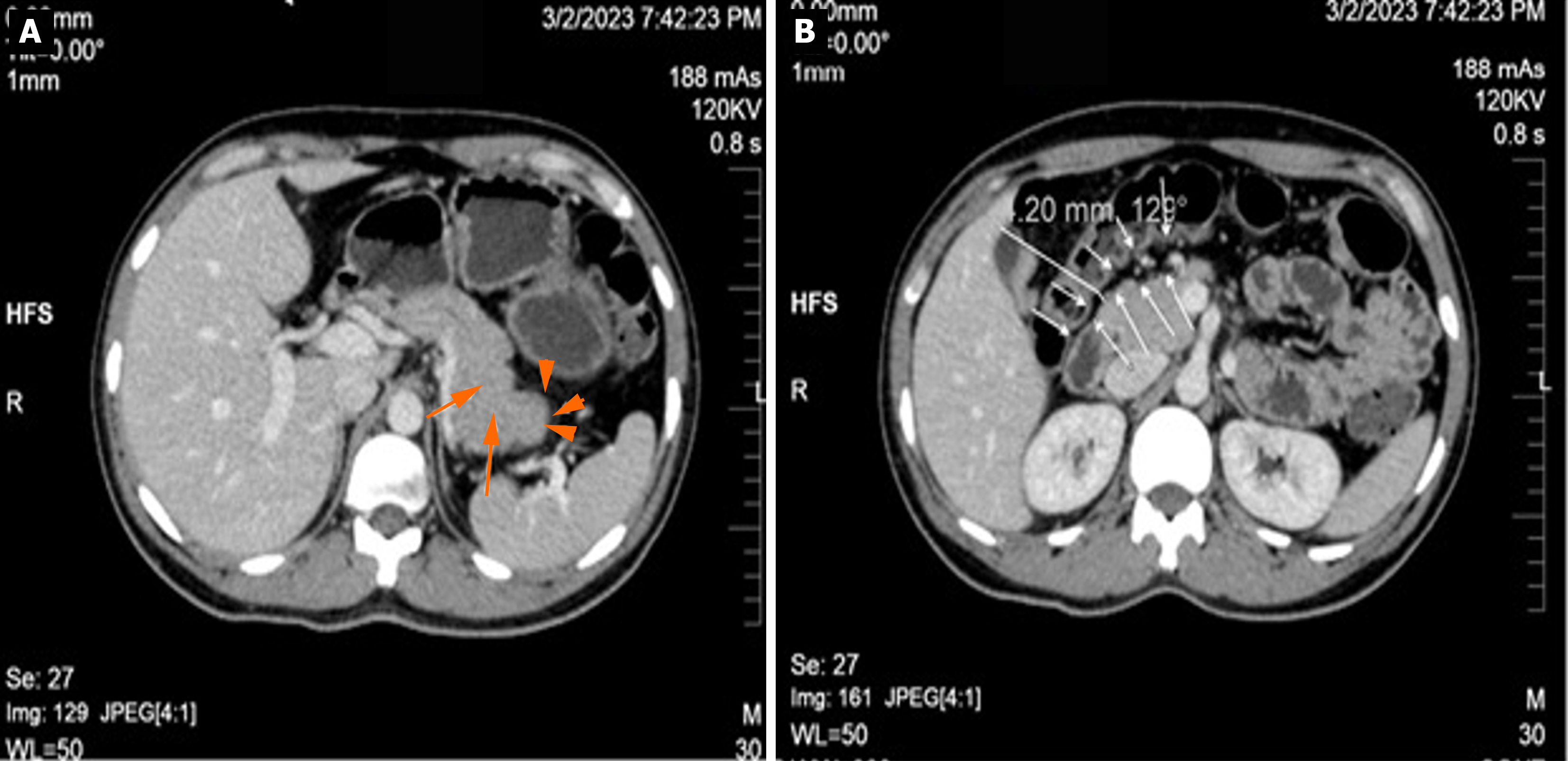
Diagnosis usually combines clinical manifestations of epigastric pain and vomiting, with elevated pancreatic enzymes[22-24], and CT scan (Figure 1) not only confirms the diagnosis but also assesses the severity of the injury.
The risk factors for pancreatic injuries include direct mechanical trauma to the pancreas due to procedural difficulties particularly around the splenic flexure, cautery induced transmural colonic burns, over-insufflation of colon, direct abdominal pressure exerted to facilitate endoscope advancement[5,22-24] and prior abdominal surgeries with pre-existing adhesions[24].
Treatment varies based on severity and etiology. For uncomplicated AP, conservative treatment with fluids, analgesics with or without prophylactic antibiotics is usually sufficient[5,22]. The duration of conservative treatment is usually few days[5,24], and may be prolonged to 1-2 wk in complicated cases[5]. Complicated cases may require further inter
Apart from acute kidney injury due to bowel preparation solutions[25], direct physical injuries to the kidney(s) or supra-renal gland(s) by colonoscopy was not reported.
Other uncommon abdominal organ injuries during colonoscopy that have been reported involve the mesentery with a tear[26], and urinary bladder with multiple perforations[27]. Small bowel injury has been reported also-these injuries are mostly perforations and encountered in ileum following electrocautery within colon[28] or pneumatic distension[29], or proximal jejunum due to rupture of jejunal diverticulum in elderly people[30]. These uncommon injuries and perforations are related to previous abdominal surgeries with presence of adhesions[27,29,31], weak bowel wall due to age[26], and excessive air insufflation during colonoscopy[28,31]. It may be a single[30] or multiple perforations[27,31].
The mechanism of intra-abdominal organ injures during colonoscopy is not fully understood. However, many risk factors have been identified and it can be categorized into organ related, procedure related, and local abdominal factors. Organomegaly either due to infiltrative, hematologic, or intrinsic diseases predispose the organ to trauma during colonoscopy; this was evident in many injuries involving spleen[14]. Previous episodes of inflammation also increase the likelihood of organ affection and was described in many cases of post colonoscopy pancreatitis[6]. Furthermore, the procedure of colonoscopy itself plays a pivotal role in occurrence of such injuries, where looping or hooking to straighten the left colon[23], marked inflation with air[24,29,32,33], use of electrical current[28], supine position, external abdominal pressure have been proposed as possible precipitants of colonoscopy related injuries. Local abdominal factors have been verified as potential precipitants for colonoscopy related injuries. The close proximity of splenic flexure to spleen and the tail of pancreas (Figure 1) explain why injuries are more frequently reported in this anatomical site (pancreatitis and splenic injuries). Intra-abdominal adhesions due to prior abdominal surgeries have been focused as the most important predisposing factor for colonoscopy related injuries[16,17] reported to the spleen, pancreas, liver, mesentery, and urinary bladder due to the transmitted traction exerted through the adhesion bands from the colon to these organs, e.g., spleen, liver, and urinary bladder or to the ligaments fixing these organs in their anatomical positions, e.g., rupture of spleno-colic ligament due to manipulations in the splenic flexure predispose to extensive splenic injuries[8]. The underlying bowel diseases especially IBD[16], bowel polyposis, diverticulae[30] were described as possible predisposing factors for these injuries[14], especially in elderly[30].
There are no published guidelines to guard against the abdominal organ injuries during colonoscopy. However, certain precautions and preventive strategies can be extrapolated from the colonoscopy practice guidelines and from the case reports focusing on these injuries. The prevention strategies should focus not only on preventing organ injuries but also should prevent the delay in diagnosis of such potentially fatal injuries.
Preventive measures include good colonoscopy technique[8], to avoid loop formation and to avoid the use of excessive force[34]; and it is probably that emerging endoscopic technologies and artificial intelligence will lead to a reduced risk of these organ injuries.
The left lateral position of the patient may reduce the risk of splenic injury after colonoscopy. It is postulated that if the patient assumed a supine position, the forces exerted on the spleen due to gravity and traction during colonoscopy oppose each other. This factor will increase the chance of splenic capsular avulsion, especially if there are other predisposing factors, such as previous abdominal surgery. The adhesions in supine position will be tightened while in left lateral position the spleen will fall beside the colon and any fibrotic band will be loose. Consequently, it is recommended that, patients belonging to the high-risk group should be placed in the left lateral position, and the supine position needs to be avoided during colonoscopy[34]. Manual abdominal counter-pressure applied correctly and safely during colonoscopy can reduce the risk of tears during the procedure[26].
Abdominal organ injuries may remain asymptomatic post-colonoscopy for a variable period of time that extends from hours to days and hence patients should be informed about the possible complications and the leading manifestations and they should be instructed to access the ER for suggestive complaints especially abdominal pain, distension, and hemodynamic instability[35]. High risk patients should be monitored before discharge and clinicians should raise the high level of suspicion when evaluating those patients[34].
In conclusion, colonoscopy related abdominal organ injuries are uncommon, however serious, that should not be overlooked by clinicians and endoscopists. Severe abdominal pain, distension, hypotension and hemodynamic instability in absence or rectal bleeding should raise the possibility of severe organ injury. Splenic and hepatic injury following colonoscopy is serious and may be life threatening and usually needs interventional radiology or surgical intervention. AP following colonoscopy is usually mild and usually managed conservatively. Other abdominal organs are less frequently injured during colonoscopy. Left lateral position, avoidance of looping and excessive force during the procedure would probably reduce the risk of such injuries.
| 1. | Gangwani MK, Aziz A, Dahiya DS, Nawras M, Aziz M, Inamdar S. History of colonoscopy and technological advances: a narrative review. Transl Gastroenterol Hepatol. 2023;8:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 2. | Lee SH, Park YK, Lee DJ, Kim KM. Colonoscopy procedural skills and training for new beginners. World J Gastroenterol. 2014;20:16984-16995. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (2)] |
| 3. | ASGE Standards of Practice Committee; Fisher DA, Maple JT, Ben-Menachem T, Cash BD, Decker GA, Early DS, Evans JA, Fanelli RD, Fukami N, Hwang JH, Jain R, Jue TL, Khan KM, Malpas PM, Sharaf RN, Shergill AK, Dominitz JA. Complications of colonoscopy. Gastrointest Endosc. 2011;74:745-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 239] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 4. | Ha JF, Minchin D. Splenic injury in colonoscopy: a review. Int J Surg. 2009;7:424-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Sidiqi MM, Gong B. Acute pancreatitis as a complication of routine colonoscopy-A rare case report. Int J Surg Case Rep. 2019;57:81-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Limb C, Ibrahim IA, Fitzsimmons S, Harper AJ. Recurrent pancreatitis after unremarkable colonoscopy, temporalised by CT imaging: an unusual case. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Kooyker AI, Toes-Zoutendijk E, Opstal-van Winden AWJ, Buskermolen M, van Vuuren HJ, Kuipers EJ, van Kemenade FJ, Ramakers C, Dekker E, Nagtegaal ID, de Koning HJ, Spaander MCW, Lansdorp-Vogelaar I, van Leerdam ME. Colonoscopy-Related Mortality in a Fecal Immunochemical Test-Based Colorectal Cancer Screening Program. Clin Gastroenterol Hepatol. 2021;19:1418-1425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Sarhan M, Ramcharan A, Ponnapalli S. Splenic injury after elective colonoscopy. JSLS. 2009;13:616-619. [PubMed] |
| 9. | Kamath AS, Iqbal CW, Sarr MG, Cullinane DC, Zietlow SP, Farley DR, Sawyer MD. Colonoscopic splenic injuries: incidence and management. J Gastrointest Surg. 2009;13:2136-2140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 10. | Cooper GS, Kou TD, Rex DK. Complications following colonoscopy with anesthesia assistance: a population-based analysis. JAMA Intern Med. 2013;173:551-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 194] [Article Influence: 14.9] [Reference Citation Analysis (1)] |
| 11. | Laanani M, Coste J, Blotière PO, Carbonnel F, Weill A. Patient, Procedure, and Endoscopist Risk Factors for Perforation, Bleeding, and Splenic Injury After Colonoscopies. Clin Gastroenterol Hepatol. 2019;17:719-727.e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 12. | Wherry DC, Zehner H Jr. Colonoscopy-fiberoptic endoscopic approach to the colon and polypectomy. Med Ann Dist Columbia. 1974;43:189-192. [PubMed] |
| 13. | Ullah W, Rashid MU, Mehmood A, Zafar Y, Hussain I, Sarvepalli D, Hasan MK. Splenic injuries secondary to colonoscopy: Rare but serious complication. World J Gastrointest Surg. 2020;12:55-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 14. | Piccolo G, Di Vita M, Cavallaro A, Zanghì A, Lo Menzo E, Cardì F, Cappellani A. Presentation and management of splenic injury after colonoscopy: a systematic review. Surg Laparosc Endosc Percutan Tech. 2014;24:95-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 15. | Prowda JC, Trevisan SG, Lev-Toaff AS. Splenic injury after colonoscopy: conservative management using CT. AJR Am J Roentgenol. 2005;185:708-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Ellis WR, Harrison JM, Williams RS. Rupture of spleen at colonoscopy. Br Med J. 1979;1:307-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Levine E, Wetzel LH. Splenic trauma during colonoscopy. AJR Am J Roentgenol. 1987;149:939-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Noreña I, Varón A, Dennis C, Dennis R. Hepatic injury following colonoscopy. Endoscopy. 2013;45 Suppl 2:E247. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Jammal M, Valesky W, Das D, Brown C, Kapoor M. Subcapsular liver hematoma after colonoscopy diagnosed by emergency department bedside ultrasonography. J Emerg Med. 2013;45:598-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Hussain S, McCaskey E, Loschner A, Ie S. Hepatic and Splenic Injury: A Rare Iatrogenic Post ColonoscopyComplication. ARC J Clin Case Rep. 2020;6:22-25. [DOI] [Full Text] |
| 21. | Shankar S, Rowe S. Splenic injury after colonoscopy: case report and review of literature. Ochsner J. 2011;11:276-281. [PubMed] |
| 22. | Thomas AW, Mitre RJ. Acute pancreatitis as a complication of colonoscopy. J Clin Gastroenterol. 1994;19:177-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Williams CB, Lane RH, Sakai Y. Colonoscopy: an air-pressure hazard. Lancet. 1973;2:729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Khashram M, Frizelle FA. Colonoscopy--a rare cause of pancreatitis. N Z Med J. 2011;124:74-76. [PubMed] |
| 25. | Ivanovic LF, Silva BC, Lichtenstein A, Paiva EF, Bueno-Garcia ML. Kidney injury and other complications related to colonoscopy in inpatients at a tertiary teaching hospital. Clinics (Sao Paulo). 2018;73:e456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Shacket RA, Gillis BJ, Guthrie CS. Mesenteric Tear Can Be Caused by Abdominal Counter-Pressure Applied During Colonoscopy. Am J Case Rep. 2021;22:e928889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 27. | Suh JW, Min JW, Namgung H, Park DG. Urinary Bladder Injury During Colonoscopy Without Colon Perforation. Ann Coloproctol. 2017;33:112-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 28. | Erdman LH, Boggs HW Jr, Slagle GW. Electrical ileal perforation: an unusual complication of colonoscopy. Dis Colon Rectum. 1979;22:501-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Razzak IA, Millan J, Schuster MM. Pneumatic ileal perforation: an unusual complication of colonoscopy. Gastroenterology. 1976;70:268-271. [PubMed] [DOI] [Full Text] |
| 30. | Pasumarthy L, Srour J, Johnson D. Jejunal Perforation following Screening Colonoscopy. Case Rep Gastroenterol. 2008;2:187-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 31. | Nemeh HW, Ranzinger MR, Dutro JA. Mid-ileal perforation secondary to colonoscopy. Am Surg. 1994;60:228-229. [PubMed] |
| 32. | Ahmed D, Nabiha S, Martin F, Guru T. 1452 Unusual Complication Following Screening Colonoscopy. American J Gastroenterol. 2019;114:S805-S806. [DOI] [Full Text] |
| 33. | Frühmorgen P, Demling L. Complications of diagnostic and therapeutic colonoscopy in the Federal Republic of Germany. Results of an inquiry. Endoscopy. 1979;11:146-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 93] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 34. | Tse CC, Chung KM, Hwang JS. Splenic injury following colonoscopy. Hong Kong Med J. 1999;5:202-203. [PubMed] |
| 35. | Petersen CR, Adamsen S, Gocht-Jensen P, Arnesen RB, Hart-Hansen O. Splenic injury after colonoscopy. Endoscopy. 2008;40:76-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shinozaki M, Japan; Zhang J, China; Zhang Z, China S-Editor: Chen YL L-Editor: A P-Editor: Cai YX