Published online Jan 21, 2024. doi: 10.3748/wjg.v30.i3.199
Peer-review started: November 28, 2023
First decision: December 8, 2023
Revised: December 12, 2023
Accepted: January 5, 2024
Article in press: January 5, 2024
Published online: January 21, 2024
Processing time: 50 Days and 17.9 Hours
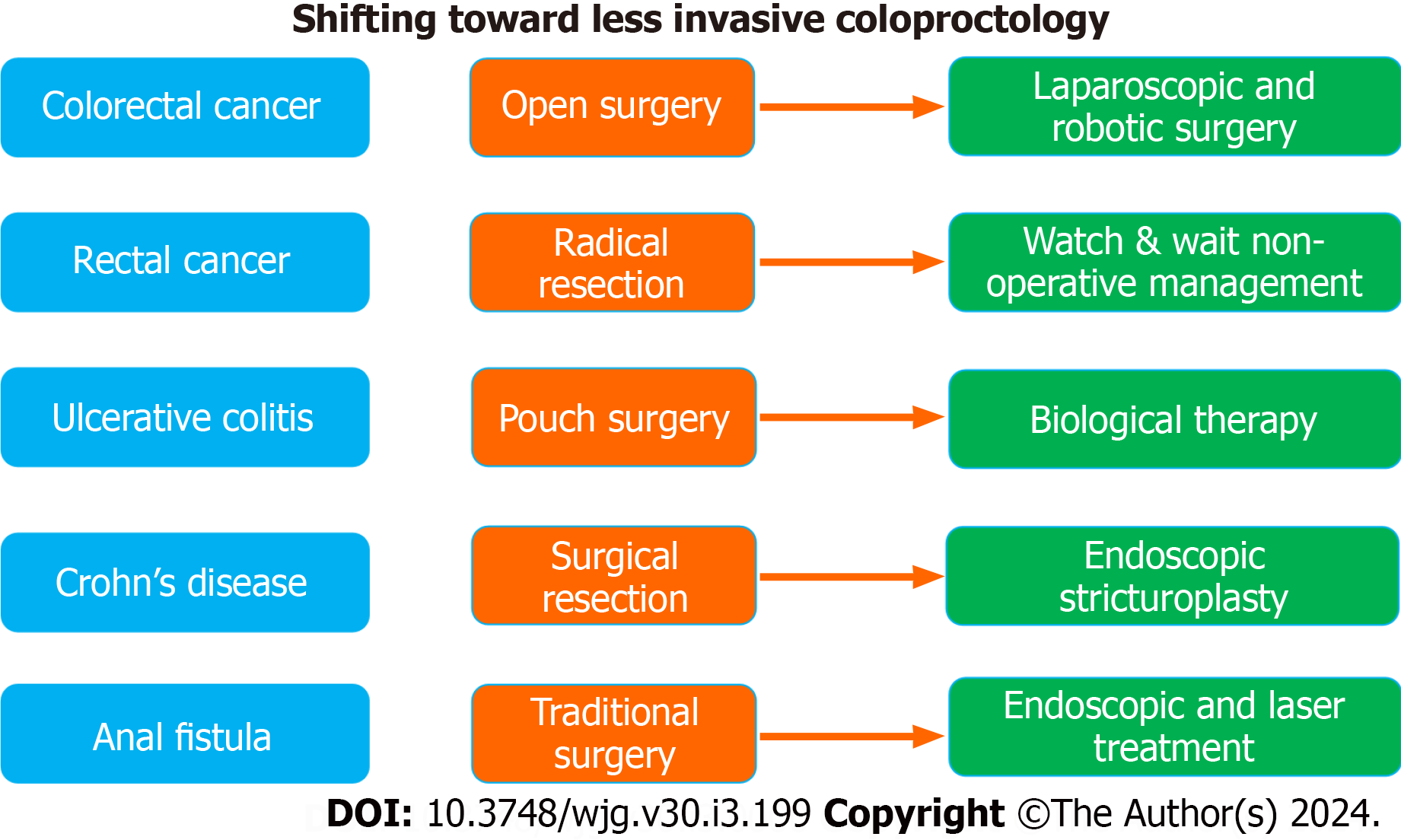
Medical care has undergone remarkable improvements over the past few decades. One of the most important innovative breakthroughs in modern medicine is the advent of minimally and less invasive treatments. The trend towards employing less invasive treatment has been vividly shown in the field of gastroenterology, particularly coloproctology. Parallel to foregut interventions, colorectal surgery has shifted towards a minimally invasive approach. Coloproctology, including both medical and surgical management of colorectal diseases, has undergone a remarkable paradigm shift. The treatment of both benign and malignant colorectal conditions has gradually transitioned towards more conservative and less inva
Core Tip: One of the most important innovative breakthroughs in modern medicine is the advent of minimally and less invasive treatments. Coloproctology has undergone a remarkable paradigm shift as the treatment of benign and malignant colorectal conditions has gradually transitioned towards less invasive approaches. An important paradigm shift was the trend to avoid the need for radical resection of rectal cancer altogether in patients who showed complete response to neoadjuvant treatment. Another example is the trend toward non-operative management of inflammatory bowel disease and benign anorectal disorders.
- Citation: Emile SH, Ragheb J. Toward less invasive coloproctology: The future is out there. World J Gastroenterol 2024; 30(3): 199-203
- URL: https://www.wjgnet.com/1007-9327/full/v30/i3/199.htm
- DOI: https://dx.doi.org/10.3748/wjg.v30.i3.199
Medical care has undergone remarkable improvements over the past few decades. One of the most important innovative breakthroughs in modern medicine is the advent of minimally and less invasive treatments. The notion that sometimes “less is more” has made clinical researchers across the world contemplate that adequate treatment of a medical or surgical condition should not necessarily be invasive. The concept of ”Less is More medicine” was introduced more than a decade ago to address the unfounded presumption that providing more care is always better, as the overuse of medical care may indeed be associated with risks and harm[1].
The trend towards employing less invasive treatment has been vividly shown in the field of Gastroenterology. Since the first days of rigid gastrointestinal endoscopy in the 1800’s until the present time, gastroenterology has evolved into a minimally invasive specialty of its own. Early gastroenterology began as a primarily diagnostic field to support surgical decision-making, which changed with the advent of Adolf Kussmaul’s rigid endoscope in 1868[2]. For the first time, endoscopic tools such as biopsy forceps could be used for tissue diagnosis as well as therapeutically for relieving food impactions. Decades later, surgeries like Heller’s myotomy or sleeve gastrectomy would meet their endoscopic coun
One of the famous examples of treatment paradigm shift is the management of peptic ulcers. For several decades, selective and highly selective vagotomy was the standard of care for peptic ulcers. While effective in healing peptic ulcers, vagotomy was recognized to be a technically demanding and challenging procedure with potentially significant morbidity, particularly when it is combined with anterectomy[3]. These limitations motivated researchers to search for other equally effective yet less invasive treatments and thus proton pump inhibitors (PPIs) were developed. PPIs proved effective in the treatment of peptic ulcers with a well-tolerated safety profile[4], becoming the standard of care for peptic ulcers and replacing vagotomy which is now indicated in a select group of patients with refractory disease[3].
Parallel to foregut interventions, colorectal surgery has shifted towards a minimally invasive approach. Coloproctology, including both medical and surgical management of colorectal diseases, has undergone a remarkable paradigm shift. The treatment of both benign and malignant colorectal conditions has gradually transitioned towards more conservative and less invasive approaches. In particular, patients with major colorectal diseases, including colorectal cancer and inflammatory bowel disease (IBD), have benefited from the “less is more” treatment concept.
Crohn’s disease is one of the most challenging conditions to treat. Nonetheless, collective evidence has shown that early medical treatment with biological agents may reduce the need for surgery by 37%[5]. In fact, advances in medical mana
Treatment of colorectal cancer has exhibited an important shift toward less invasive management overall and specifically less invasive surgery. Surgical resection of colorectal neoplasms using a laparoscopic or robotic-assisted approach has been increasingly adopted in many hospitals in the world[10]. Minimally invasive surgery for colorectal cancer has provided tangible short-term benefits, including smaller incisions, less pain, faster recovery, and less wound-related complications, yet without compromising the oncologic outcomes[11]. Moreover, rather than doing partial colectomies for low-grade malignant polyps, endoscopic submucosal dissection or full-thickness resection can be alternatively and safely performed[12].
An even more interesting paradigm shift was the trend to avoid the need for radical resection of rectal cancer alto
Akin to colorectal cancer and IBD, coloproctologists have started to adopt less invasive approaches for benign and frequently diagnosed colorectal conditions such as hemorrhoids, anal fistulas, and pilonidal sinus disease. Although excisional hemorrhoidectomy is considered the standard of care for grade III-IV hemorrhoidal disease owing to its effectiveness, adverse effects namely severe postoperative pain are challenging and sometimes dissuade patients from re
The impact of less invasive treatment approaches on the quality of life of the patients with colorectal diseases has been explored in the literature. Compared to the more invasive open surgery, minimally invasive colorectal resections are associated with better cosmetic outcomes and greater patient satisfaction[21]. Laparoscopic resection of colorectal cancer is also associated with shorter hospital stays and higher quality of life scores than open resection on the short term[22]. Similarly, the adoption of a non-operative management approach may confer better quality of life. In a matched-controlled study, Hupkens et al[23] found that watch-and-wait strategy for rectal cancer conferred better quality of life than did radical resection in terms of physical and cognitive function, physical and emotional roles, and global health status. Non-operative treatment was also associated with fewer defecation, sexual, and urinary functional adverse events. Also, minimally invasive treatment of benign anal conditions may confer better quality of life than conventional treat
The trend of adopting less invasive approaches to treat various colorectal conditions does not seem to be stopping soon as further research on novel, more effective, and safer methods is ongoing. Perhaps this could be considered an overly optimistic prediction, but the authors of this article anticipate that in the near future, most cases of colorectal cancer and IBD will be subject to non-operative, minimally invasive treatment. However, only time will tell if this prediction proves valid.
| 1. | Kherad O, Peiffer-Smadja N, Karlafti L, Lember M, Aerde NV, Gunnarsson O, Baicus C, Vieira MB, Vaz-Carneiro A, Brucato A, Lazurova I, Leśniak W, Hanslik T, Hewitt S, Papanicolaou E, Boeva O, Dicker D, Ivanovska B, Yldiz P, Lacor P, Cranston M, Weidanz F, Costantino G, Montano N. The challenge of implementing Less is More medicine: A European perspective. Eur J Intern Med. 2020;76:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Kravetz R. A Look Back: Reflections on Medical History & Artifacts from the Pages of the American Journal of Gastroenterology. Flagstaff: Rudy Ramos Design Studio, 2020. |
| 3. | Lagoo J, Pappas TN, Perez A. A relic or still relevant: the narrowing role for vagotomy in the treatment of peptic ulcer disease. Am J Surg. 2014;207:120-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Scally B, Emberson JR, Spata E, Reith C, Davies K, Halls H, Holland L, Wilson K, Bhala N, Hawkey C, Hochberg M, Hunt R, Laine L, Lanas A, Patrono C, Baigent C. Effects of gastroprotectant drugs for the prevention and treatment of peptic ulcer disease and its complications: a meta-analysis of randomised trials. Lancet Gastroenterol Hepatol. 2018;3:231-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 175] [Article Influence: 21.9] [Reference Citation Analysis (17)] |
| 5. | Law CCY, Tkachuk B, Lieto S, Narula N, Walsh S, Colombel JF, Ungaro RC. Early Biologic Treatment Decreases Risk of Surgery in Crohn's Disease but not in Ulcerative Colitis: Systematic Review and Meta-Analysis. Inflamm Bowel Dis. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 39] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 6. | Kalman TD, Everhov ÅH, Nordenvall C, Sachs MC, Halfvarson J, Ekbom A, Ludvigsson JF, Myrelid P, Olén O. Decrease in primary but not in secondary abdominal surgery for Crohn's disease: nationwide cohort study, 1990-2014. Br J Surg. 2020;107:1529-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Kuehn F, Hodin RA. Impact of Modern Drug Therapy on Surgery: Ulcerative Colitis. Visc Med. 2018;34:426-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Abou Khalil M, Boutros M, Nedjar H, Morin N, Ghitulescu G, Vasilevsky CA, Gordon P, Rahme E. Incidence Rates and Predictors of Colectomy for Ulcerative Colitis in the Era of Biologics: Results from a Provincial Database. J Gastrointest Surg. 2018;22:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Navaneethan U, Lourdusamy D. Endoscopic Stricturotomy and Strictureplasty. Gastrointest Endosc Clin N Am. 2022;32:687-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 10. | Stănciulea O, Eftimie M, Moşteanu I, Tivadar B, Blăniţă D, Popescu I. Minimally Invasive Colorectal Surgery - Present and Future Trends. Chirurgia (Bucur). 2019;114:167-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Imaizumi K, Homma S, Miyaoka Y, Matsui H, Ichikawa N, Yoshida T, Takahashi N, Taketomi A. Exploration of the advantages of minimally invasive surgery for clinical T4 colorectal cancer compared with open surgery: A matched-pair analysis. Medicine (Baltimore). 2022;101:e29869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 12. | Andrisani G, Hassan C, Pizzicannella M, Pugliese F, Mutignani M, Campanale C, Valerii G, Barbera C, Antonelli G, Di Matteo FM. Endoscopic full-thickness resection vs endoscopic submucosal dissection for challenging colorectal lesions: a randomized trial. Gastrointest Endosc. 2023;98:987-997.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Habr-Gama A, São Julião GP, Perez RO. Nonoperative management of rectal cancer: identifying the ideal patients. Hematol Oncol Clin North Am. 2015;29:135-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 14. | Kasi A, Abbasi S, Handa S, Al-Rajabi R, Saeed A, Baranda J, Sun W. Total Neoadjuvant Therapy vs Standard Therapy in Locally Advanced Rectal Cancer: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020;3:e2030097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 286] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 15. | Emile SH. Evidence-based review of methods used to reduce pain after excisional hemorrhoidectomy. J of Coloproctology. 2019;39:081-089. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Hoyuela C, Carvajal F, Juvany M, Troyano D, Trias M, Martrat A, Ardid J, Obiols J. HAL-RAR (Doppler guided haemorrhoid artery ligation with recto-anal repair) is a safe and effective procedure for haemorrhoids. Results of a prospective study after two-years follow-up. Int J Surg. 2016;28:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | De Nardi P, Maggi G, Pagnanelli M, Vlasakov I, Corbetta D. Hemorrhoid laser dearterialization: systematic review and meta-analysis. Lasers Med Sci. 2023;38:54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Emile SH, Elfeki H, Shalaby M, Sakr A. A Systematic review and meta-analysis of the efficacy and safety of video-assisted anal fistula treatment (VAAFT). Surg Endosc. 2018;32:2084-2093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 97] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 19. | Elfeki H, Shalaby M, Emile SH, Sakr A, Mikael M, Lundby L. A systematic review and meta-analysis of the safety and efficacy of fistula laser closure. Tech Coloproctol. 2020;24:265-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 20. | Wang H, Jiang HY, Zhang YX, Jin HY, Fei BY, Jiang JL. Mesenchymal stem cells transplantation for perianal fistulas: a systematic review and meta-analysis of clinical trials. Stem Cell Res Ther. 2023;14:103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 21. | Scarpa M, Erroi F, Ruffolo C, Mollica E, Polese L, Pozza G, Norberto L, D'Amico DF, Angriman I. Minimally invasive surgery for colorectal cancer: quality of life, body image, cosmesis, and functional results. Surg Endosc. 2009;23:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Ihnát P, Martínek L, Mitták M, Vávra P, Ihnát Rudinská L, Zonča P. Quality of life after laparoscopic and open resection of colorectal cancer. Dig Surg. 2014;31:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Hupkens BJP, Martens MH, Stoot JH, Berbee M, Melenhorst J, Beets-Tan RG, Beets GL, Breukink SO. Quality of Life in Rectal Cancer Patients After Chemoradiation: Watch-and-Wait Policy Versus Standard Resection - A Matched-Controlled Study. Dis Colon Rectum. 2017;60:1032-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 199] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 24. | Shabahang H, Maddah G, Mofidi A, Nooghabi MJ, Khaniki SH. A Randomized Clinical Trial of Laser Hemorrhoidoplasty vs Milligan and Morgan Hemorrhoidectomy. World J Lap Surg. 2019;12:59-63. [DOI] [Full Text] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fu L, China S-Editor: Lin C L-Editor: A P-Editor: Xu ZH